Hypertension is a common chronic cardiovascular disease, with persistently high blood pressure, causes damage to the heart, cerebral blood vessels, kidneys, and other organs, and can increase the risk of heart disease, stroke, and other diseases (1). By category, hypertension can typically be divided into essential hypertension, secondary hypertension, and pregnancy-induced hypertension (2). Hypertension has been identified as an essential risk factor for death, with an estimated 9.4 million premature deaths and 92 million disabilities attributable to hypertension each year (3–5). Based on available surveys, more than 1 billion people worldwide with hypertension in 2019, the number has doubled since 1990 (6). The largest global study of hypertension trends to date, led by Imperial College London and the World Health Organization in 2021 and involving more than 1,100 doctors and scientists, found the number of adults aged 30–79 with hypertension has increased from 650 million to 1.28 billion in the last 30 years and more than 700 million of these don't know they have (7). By 2019, China managed about 109 million registered hypertensive patients, the standardized management rate of hypertensive patients has increased by 29.28%, and the blood pressure control rate in the population managed for hypertension has increased by 16.84% in the past decade, with an average annual growth rate of 3.28% (8). In addition to the high prevalence of hypertension, the financial burden of this disease is also significant. The global healthcare costs due to hypertension exceed $500 billion per year, and only the United States incurs more than $300 billion per year, with Europe being the region with the highest healthcare costs for hypertension (9, 10). China's direct medical costs due to hypertension from 1993 to 2003 grew from RMB 4.531 billion to RMB 30.030 billion, with an average annual growth rate as high as 20.82%, which is faster than the GDP, and even faster than the growth rate of the total health costs and the total medical costs in the same period (11). The annual per capita cost of hypertension among Chinese residents in the period of 2006–2011 was RMB 6,271.80, accounting for 45.58% of the annual per capita income (12), and the medical cost of hypertension in China in 2019 was as high as RMB 74.06 billion, accounting for 5.1% of the total national medical cost (13, 14). With the aging of China's population, China's hypertensive population is bound to increase continually, and the hypertensive disease burden will continue to increase. Hypertension has become a worldwide public health problem bringing a heavy economic burden of disease to the world (15–17), and hypertensive patients with other comorbidities and complications will consume more medical resources and incur more healthcare costs (18, 19), so the need for research on hypertension cost control is particularly urgent (20–22).
As an essential part of China's healthcare system, TCM hospitals make comprehensive use of the correlation of all four examinations as well as traditional resources and therapeutic means, such as traditional Chinese medicine, acupuncture and moxibustion, and tuina, to carry out diagnosis and treatment for diseases. The TCM hospitals' therapy process emphasizes mutually the overall concept and individualized diagnosis, which focuses on regulating the balance and coordination of the systems within the human body while formulating targeted treatment plans according to the patient's specific condition and physical characteristics. Meanwhile, TCM hospitals inherit and carry forward the essence of TCM, as well as actively introduce modern medical technology, and promote the development of integrated Chinese medicine and Western medicine diagnosis and treatment modes, to satisfy the demand for patients' all-around diagnosis and treatment service. In recent years, the Chinese government has paid more and more attention to the inheritance and innovation of Chinese medicine and focused on the dominant therapy of TCM in the treatment of chronic diseases, such as cupping, scraping, acupuncture, and tuina (23–25). In particular, the publication of “Expert Consensus on the Diagnosis and Treatment of Hypertension with Traditional Chinese Medicine” (26, 27) has further improved the system of diagnostic and therapeutic protocols for the treatment of hypertension with Chinese medicine in China. Undeniably, TCM tonics, oral CPMs (Chinese patent medicines, CPMs), and TCM injections have been widely used in the treatment of hypertension and have achieved remarkable efficacy (28–30), which reflects unique TCM advantages in improving clinical efficacy, reducing BP levels, and improving the quality of life. In a word, TCM provides an excellent alternative for hypertensive patients who cannot tolerate conventional Western medications.
The Global Report on Hypertension released by WHO in September 2023, estimates the economic benefits of improved hypertension treatment options are ~18 times greater than the costs. As an important treatment method for hypertension in China, Chinese medicine, including herbal formulas, acupuncture, acupoints, footbaths, and other Chinese medical treatments, as well as the combination of Chinese medicine and Western medicine, not only achieve effective clinical results in the treatment of hypertension but also have an absolute advantage in terms of cost. In this regard, the overall cost of treating hypertension in TCM hospitals is much lower than Western medicine due to the vast area of cultivation of Chinese herbal medicine in China and the high availability and circulation of Chinese medicine resources. Therefore, this paper reviewed and analyzed the relevant information of 3,595 patients with hypertension who were hospitalized in Tianshui Hospital of TCM in Gansu Province, China from January 2017 to June 2022, to explore the influencing factors of hospitalization cost of patients. In this study, targeted countermeasures and suggestions were also proposed to control hospitalization cost and give full play to the price advantages of chronic diseases in TCM, to effectively alleviate the economic pressure brought by hypertension to the national economy.
2 Materials and methods 2.1 Study design and populationThe data for this study came from the National Health Big Data Platform (a governmental non-full public database) of the Health Commission of Gansu Province, China, and the data content mainly involved information on the front page of TCM hospital cases, with detailed on hypertensive hospitalized patients in Tianshui City TCM Hospital, Gansu Province, for January 2017–June 2022. Inclusion criteria: patients with a primary diagnosis of tertiary hypertension I10.x05 (in accordance with ICD-10). Exclusion criteria: the length of stay is < 1 day, logically inconsistent in medical information, and diagnostic information with incomplete and could not be effectively supplemented. Following the above inclusion and exclusion criteria, 3,595 valid cases were finally included. As the research data need to be treated confidentially and should not be made public, the corresponding author can be contacted if necessary.
2.2 Data processingSince the key indicator of hospitalization cost in this study is economic data, to eliminate the bias effect of inflation and other factors on the study of hospitalization cost in hypertension, the cost adjustment was made based on the Consumer Price Index (CPI) for healthcare in Gansu Province from 2017 to 2022, with 2016 as the base period for statistical correlation analysis.
According to the existing research, hospitalization cost is affected by factors such as length of stay (31–34). In this study, the length of stay and hospitalization cost were endogenous variables, while gender, ethnicity, age, marital status, visit times, payment methods of medical insurance, occupations, admission pathways, treatment categories, clinical pathways, use of TCM preparations, use of TCM diagnosis and treatment equipment, use of TCM diagnosis and treatment techniques, disease severity, and surgery and procedures were exogenous variables. In addition, relevant variables should be classified or integrated according to the actual analysis. The specific variable assignment processing was shown in Table 1.
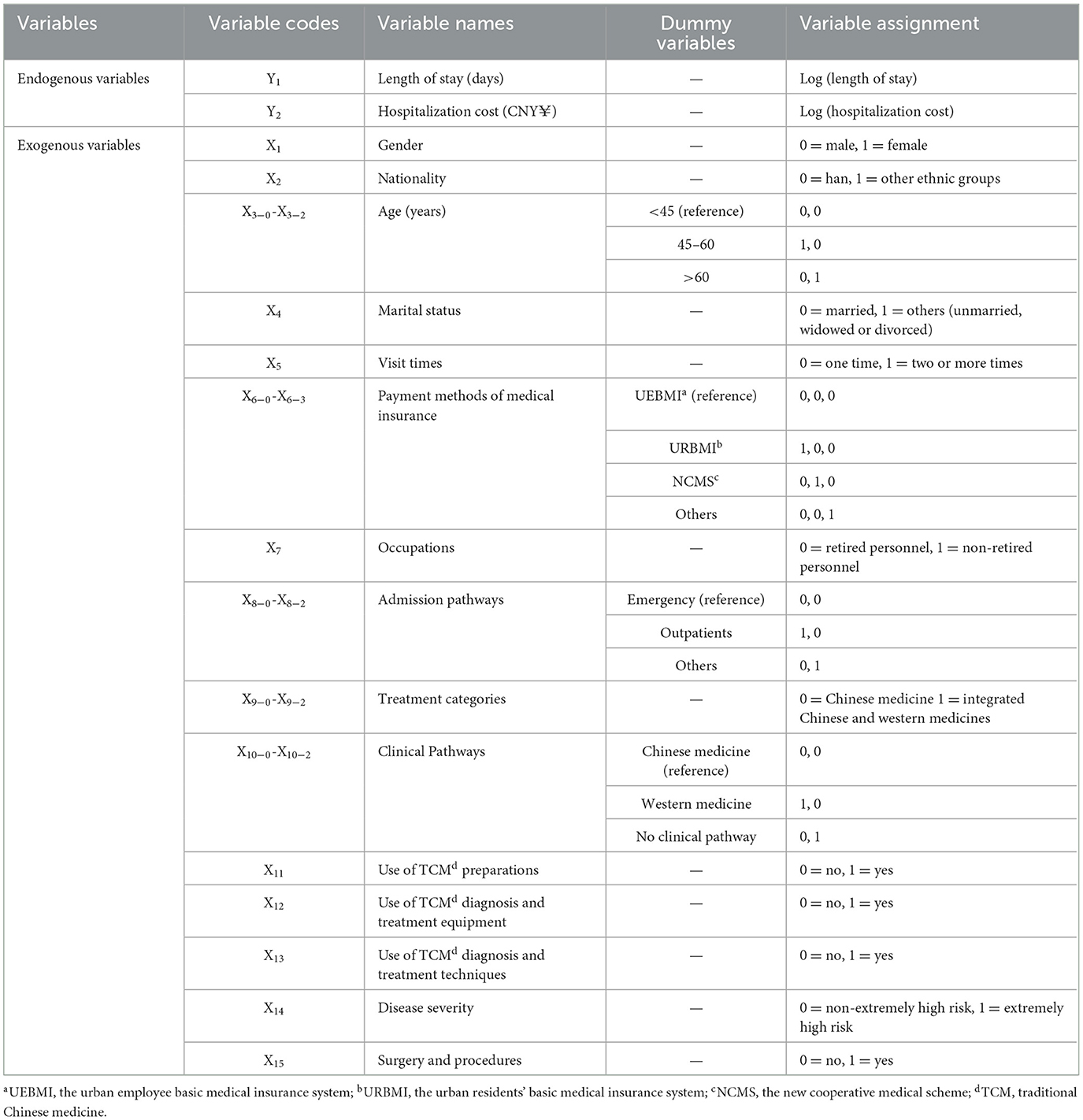
Table 1. Variable assignment processing case.
2.3 Statistical analysisFirstly, univariate analysis of length of stay and hospitalization cost was performed using SPSS 26.0. Since the original data of hospitalization cost and length of stay did not follow the normal distribution, the Mann-Whitney U-test and Kruskal-Wallis H-test were used to process and analyze according to the data types, and the length of stay and hospitalization cost were expressed in the median and quartile. Secondly, variables that were statistically significant in the univariate analysis selected as independent variables, and the dependent variables length of stay and hospitalization cost, which did not obey normal distribution, were logarithmically transformed into Log (Length of stay) and Log (Hospitalization cost) to approximate the requirement of obeying normality, to establish multiple linear regression models. Based on multiple linear regression analysis model, Amos 24.0 software was used to establish a path model with statistically significant variables in multiple linear regression results as independent variables, Log (Length of stay) as mediator variables, and Log (Hospitalization cost) as dependent variables, to explore the influencing factors and its rank relationship of hospitalization cost in patients with hypertension comprehensively. The test level of the above analysis was α = 0.05.
3 Results 3.1 Univariate analysis results of length of stay and hospitalization costAs can be seen from Table 2, there were significant differences (p < 0.05) in the length of stay among hypertensive patients with different ages, visit times, payment methods of medical insurance, occupations, admission pathways, treatment categories, clinical pathways, use of TCM diagnosis and treatment equipment, disease severity, and whether surgery and procedures were performed, and more comparison of differences can be seen in Figure 1. Furthermore, there were also statistical differences (p < 0.05) in the hospitalization cost of hypertensive patients by different ages, marital status, visit times, payment methods of medical insurance, admission pathways, length of stay, use of TCM diagnosis and treatment equipment, disease severity, and whether surgery and procedures were performed, and more comparison of differences can be seen in Figure 2.
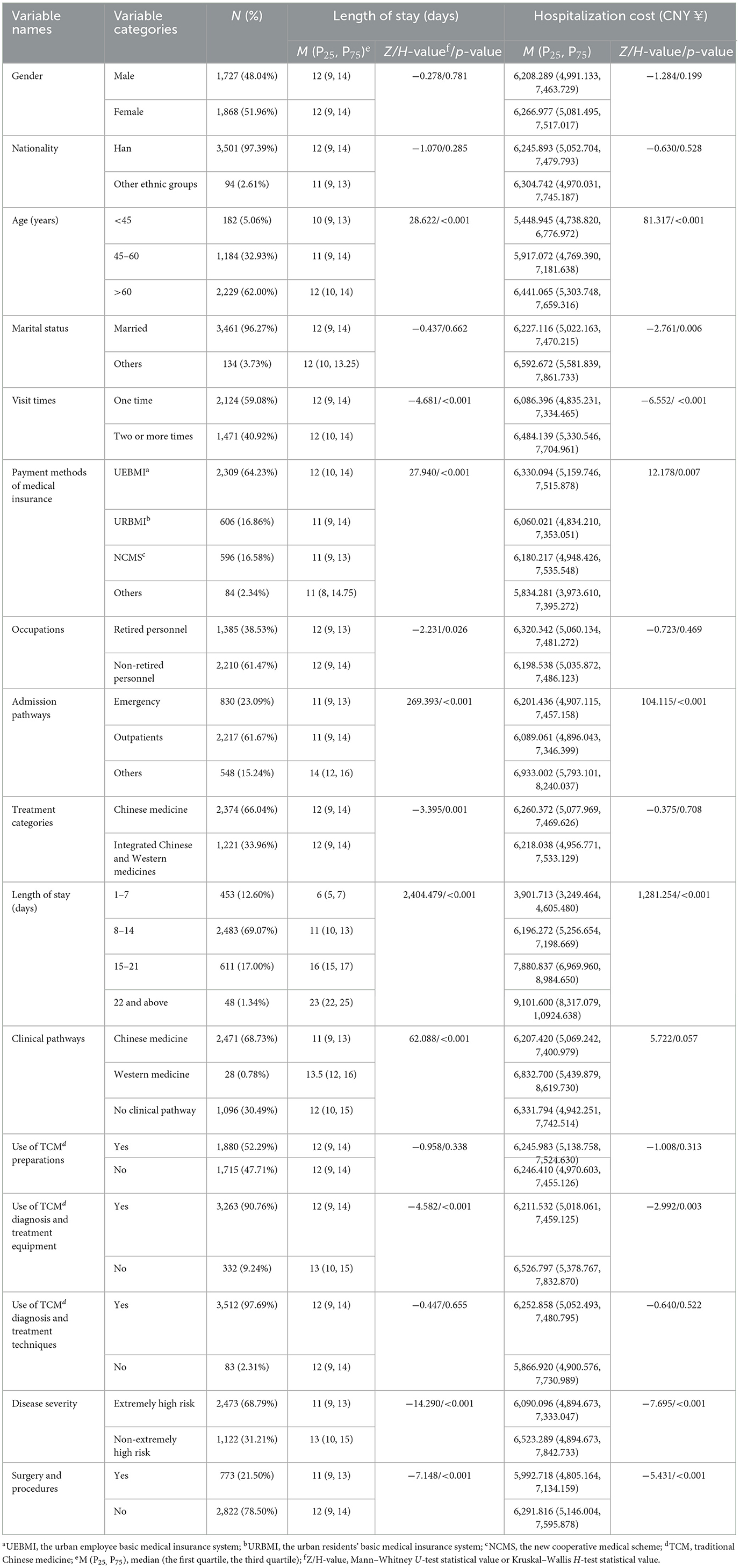
Table 2. Description of the study sample (length of stay and hospitalization cost).
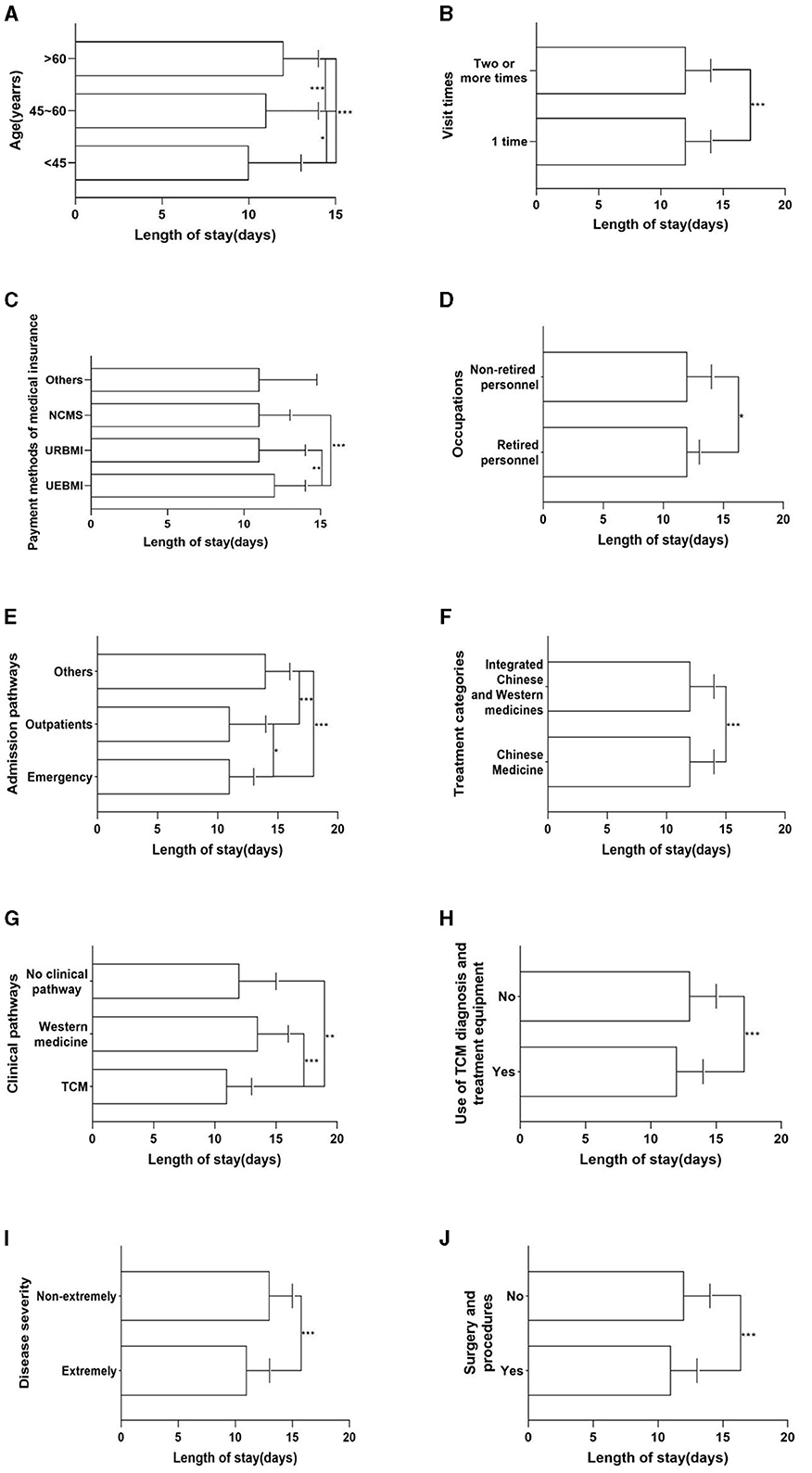
Figure 1. Univariate analysis results of length of stay. (A) Age. (B) Visit times. (C) Payment methods of medical insurance. (D) Occupations. (E) Admission pathways. (F) Treatment categories. (G) Clinical pathways. (H) Use of TCM diagnosis and treatment equipment. (I) Disease severity. (J) Surgery and procedures. *p < 0.05; **p < 0.01; ***p < 0.001.

Figure 2. Univariate analysis results of hospitalization cost. (A) Age. (B) Marital status. (C) Visit times. (D) Payment methods of medical insurance. (E) Admission pathways. (F) Length of stay. (G) Use of TCM diagnosis and treatment equipment. (H) Disease severity. (I) Surgery and procedures. *p < 0.05; **p < 0.01; ***p < 0.001.
3.2 Multivariate linear regression results of length of stay and hospitalization costResults of multivariate linear regression showed that the length of stay of hypertensive patients was affected by age, visit times, payment methods of medical insurance, other ways of admission pathways, and disease severity (p < 0.05), and the regression equation of length of stay (F = 20.322, p < 0.001, R2 = 0.078) was as follows:
Y1 = 0.953 + 0.037*X3 − 1 + 0.042*X3 − 2 + 0.032*X5 – 0.020*X6 − 1 – 0.027*X6 − 2 + 0.015*X8 − 1 + 0.098*X8 − 2 – 0.028*X14.
Hospitalization cost was affected by age, marital status, payment methods of medical insurance, admission pathways, surgery and procedures, and length of stay (p < 0.05), and the regression equation of hospitalization cost (F = 327.863, p < 0.001, R2 = 0.543) was as follows:
Y2 = 3.103 + 0.038*X3 − 2 + 0.019*MX4 + 0.015*X6 − 2 – 0.012*X8 − 1 – 0.010*X15 + 0.610*Y1.
The results are summarized in Table 3. Further calculation based on analysis results showed that the residual path coefficient was 0.676 (Pe = 1-R2 = 0.676), which is lower than the standardized coefficient of Y1, indicating that there are other influencing factors existing as well. Path models can be developed based on the results of multiple linear regressions to explore other influences on hospitalization cost comprehensively.
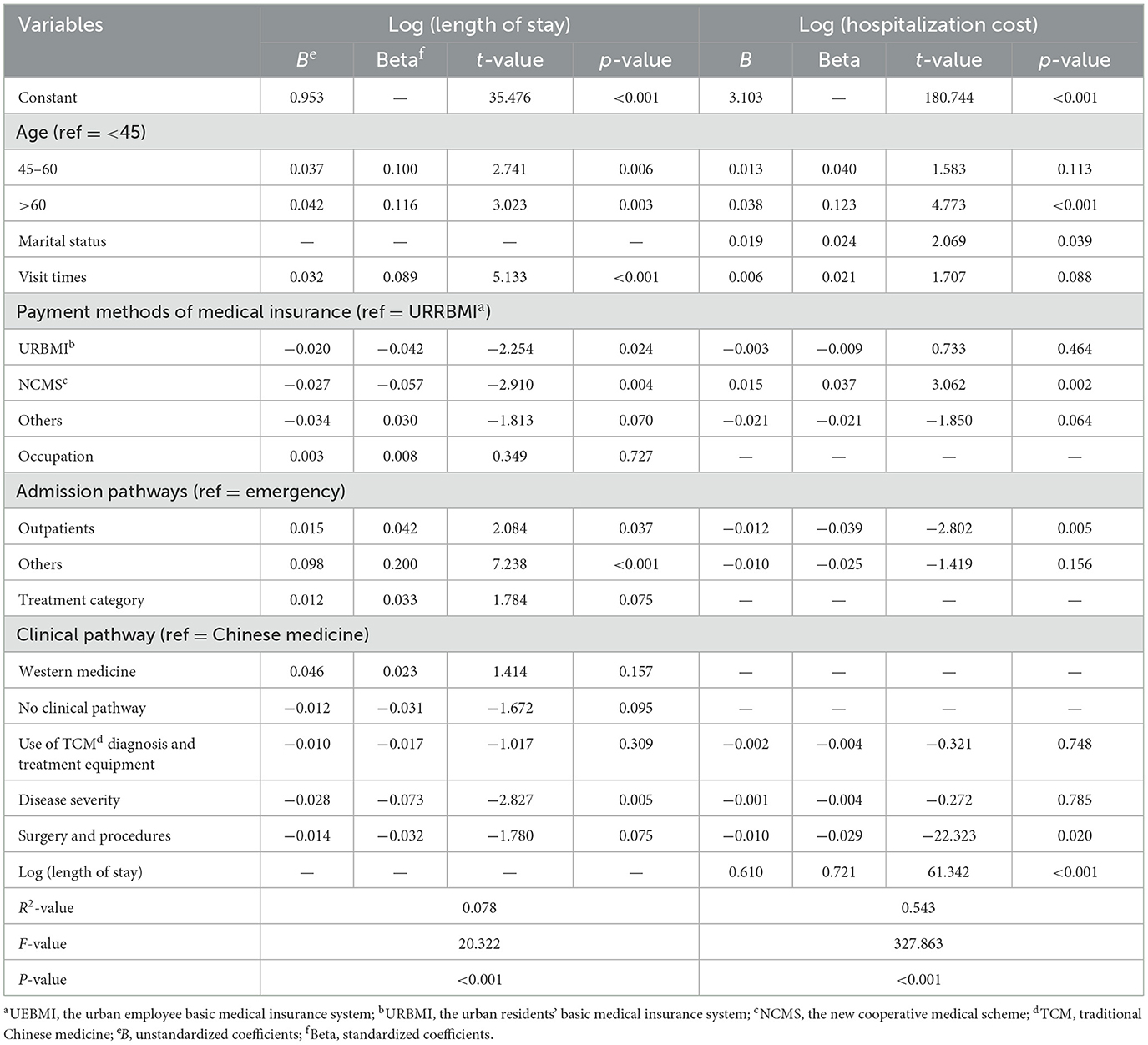
Table 3. Multiple linear regression results of the length of stay and hospitalization cost of hypertension patients.
3.3 Path analysis results of hospitalization costAs shown in Figure 3, visit times, age (45–60), admission pathways (Outpatient, Others), disease severity, and payment methods of medical insurance could indirectly affect the hospitalization cost through the length of stay. In addition, age (>60), admission pathways (Outpatients), marital status, payment methods of medical insurance (NCMS), and surgery and procedures could also affect the hospitalization cost directly.
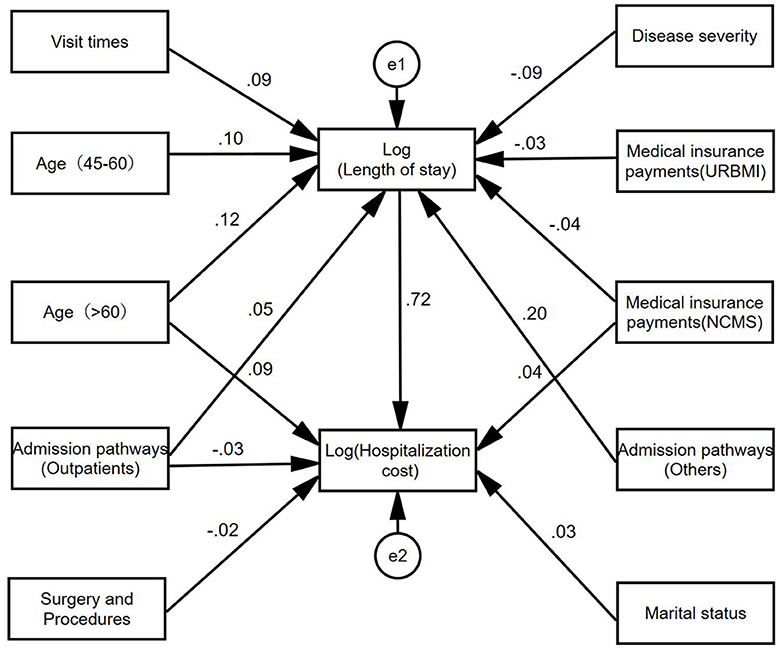
Figure 3. Path diagram of influencing factors of hospitalization cost of hypertension patients.
Based on the path model, the effects decomposition of the influencing factors of hospitalization cost could be derived, and the specific results were summarized in Table 4. The effect of each factor on hospitalization cost ranked as follows: length of stay, age (>60), admission pathways (Others), payment methods of medical insurance (NCMS), visit times, disease severity, admission pathways (Outpatients), marital status, payment methods of medical insurance (URBMI), surgery and procedures.
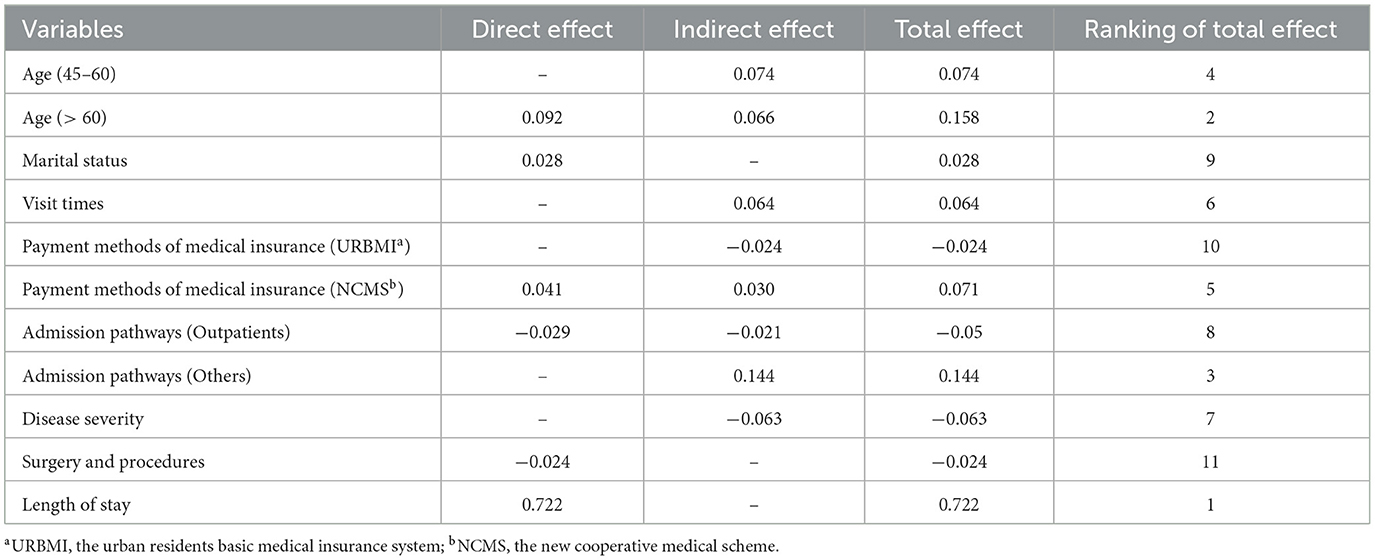
Table 4. Effect decomposition table of influencing factors of hospitalization cost of hypertension patients (tertiary).
4 DiscussionCurrent research on the cost of hypertension mainly focuses on comprehensive (Western medicine) hospitals, while our study is based on the TCM hospitals' official database from local governments in China, with rigorous and appropriate statistical methods to analyze the influence factors on hospitalization cost of hypertensive patients. As a result, this study will powerfully enrich and expand the content of the current research on cost control of hypertension, promote the development of health economics with Chinese characteristics, and be of great practical significance in giving full play to the advantages of traditional Chinese medicine in the treatment of chronic diseases such as hypertension and the reduction of the economic burden of disease in China.
Through the research, we found the length of stay of male patients with hypertension in TCM hospitals is basically equal to female patients, while the hospitalization cost of male patients is slightly higher than female patients. What's more, the age of patients is a stronger factor on hospitalization cost, which increases with growing age. What made this possible is that the older adult due to the continuous aging of the patient's organism and decreasing resistance, have a higher risk of disease and are prone to repeat and prolonged hospitalization, which consumes more healthcare resources (35, 36). Additionally, patients admitted by other pathways, such as medical referral and cross-province medical treatment, will significantly increase hospitalization cost (37). The fact that medical insurance policies of some insured places have set up differential treatment for medical referral and cross-provincial medical treatment so that their reimbursement ratio is lower than other groups, is the main reason for the current Chinese government's continuous implementation of medical insurance reform. In terms of visit times, patients with repeat visit may have relatively complex and severe conditions that show a tendency toward poorer outcomes, of which hospitalization cost will also be relatively high. As the condition progressed to critical, the risk of increased hospitalization cost rose dramatically, implying a greater possibility of resuscitation, and further increasing the risk of higher hospitalization cost.
In complete harmonization with existing studies, hospitalization cost is higher for older patients, the greater the number of visit times, and longer length of stay (38–40). Meanwhile, we found the length of stay and hospitalization cost are higher among non-retired personnel patients (41–43), which may be due to the fact that higher work pressure induces more serious hypertensive disorders with more hospitalization cost (44–46). This result coincided with multiple existing studies (47, 48), which indicate that young and middle-aged working hypertension patients tend to have a predominantly cerebral workload, older retired hypertension patients are mostly engaged in physical work, as well as working mental work face more pressure, whose prevalence of hypertension and severity of the disease also increase continuously. In addition, patients with hypertension admitted through other pathways have longer length of stay and higher hospitalization cost, mainly because patients' conditions are more complex or severe with more special investigations and treatments. At the same time, the referral pathway may result in poor transfer of information between multiple providers, which increases duplication of tests and treatments and further increases hospitalization cost (49, 50).
Confusingly, hypertensive patients with more critical diseases and undergoing surgeries and procedures had fewer length of stay and lower hospitalization cost than patients with non-critical diseases and without surgeries and procedures. Combined with the characteristics of TCM syndrome differentiation and treatment, the explanations conjecture are as follows: Firstly, the more critical the disease, the more standardized the treatment, surgical operation, and medical service process are performed. Subsidiary, surgery and procedures in the sense of TCM, such as acupuncture, moxibustion, cupping therapy, tuina, qigong, and other external treatment methods, have always been safer, more convenient, and less costly than Western surgeries (51–53), which reduces the length of stay and hospitalization cost with excellent therapeutic results. Moreover, according to the relevant policies of Chinese medical insurance, and surgery and procedures will receive greater reimbursement support from medical insurance, so the actual hospitalization cost is relatively low.
In general, in addition to the length of stay and age, the hospitalization cost of hypertension patients in TCM hospitals is also affected by the admission pathways, payment methods of medical insurance, and visit times, among which the length of stay has the greatest impact on the hospitalization cost of patients with hypertension (5, 54, 55). The longer the length of stay, the greater the medical-economic pressure the patients face. Notably, the health literacy level of hypertensive patients also affects hospitalization cost (56). Health literacy affects patients' lifestyle, medication adherence treatment behavior, etc., which in turn affects the disease management and prognosis of patients with chronic diseases (57–59). Some studies have shown that the proportion of hypertension patients with health literacy was 10.10%, which was lower than 16.13% of the general population (60), indicating that improving health literacy is an important strategy to prevent and control hypertension and other chronic diseases.
5 ConclusionsIn this study, 3,595 inpatients with a primary diagnosis of tertiary hypertension in Tianshui Hospital of Traditional Chinese Medicine, Gansu Province, China from January 2017 to June 2022 were selected as the research objects, to explore the influencing factors of hospitalization cost of hypertension patients. From our analysis results, the hospitalization cost of hypertensive patients is mainly affected by length of stay, age, admission pathways, payment methods of medical insurance, and visit times, and the length of stay is the most important and core influencing factor. As chronic diseases such as hypertension intensify and threaten the quality of life and health of all human beings, the Chinese government should continue to optimize the methods of diagnosis and treatment of TCM, incorporate the “combining disease and syndrome” into the process of treating illnesses to classify and define treatments, and actively exert the characteristics and advantages of TCM in the treatment of chronic diseases such as hypertension. Meanwhile, the China government should continue to deepen the reform of medical insurance policies, enhance the strength of outpatient medical insurance for chronic diseases, and optimize the structure of medical insurance treatment for patients with chronic diseases. More importantly, the China government should innovate a compensation mechanism for TCM to incentivize patients to actively use TCM to improve their health literacy, thereby reducing the length of stay, relieving their pain, and lowering the burden of medical costs.
Data availability statementThe raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Author contributionsH-jH: Conceptualization, Data curation, Formal analysis, Methodology, Project administration, Software, Writing – original draft, Writing – review & editing. T-zC: Investigation, Validation, Writing – review & editing. YC: Formal analysis, Validation, Writing – review & editing. Y-hB: Validation, Writing – original draft. M-eC: Software, Writing – original draft. J-yY: Resources, Supervision, Writing – review & editing. Z-hL: Conceptualization, Funding acquisition, Resources, Supervision, Writing – review & editing.
FundingThe author (s) declare financial support was received for the research, authorship, and/or publication of this article. This research was funded by the National Social Science Foundation of China, grant number 19BZX082.
AcknowledgmentsThanks for the financial support from the National Social Science Foundation and the support from the Key Discipline Construction Program of Marxism in Gansu University of Traditional Chinese Medicine.
Conflict of interestThe authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's noteAll claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References1. Tschanz MP, Cushman WC, Harrell TE, Berlowitz DR, Sall JL. Synopsis of the 2020 U.S. Department of Veterans Affairs/U.S. Department of Defense Clinical Practice Guideline: The Diagnosis and Management of Hypertension in the Primary Care Setting. Ann Int Med. (2020) 173:904–13. doi: 10.7326/M20-3798
PubMed Abstract | Crossref Full Text | Google Scholar
2. Yin R, Yin L, Li L, Silva-Nash J, Tan J, Pan Z, et al. Hypertension in China: burdens, guidelines, and policy responses: a state-of-the-art review. J Hum Hypertens. (2022) 36:126–34. doi: 10.1038/s41371-021-00570-z
PubMed Abstract | Crossref Full Text | Google Scholar
3. Lim SS, Vos T, Flaxman AD, Danaei G, Shibuya K, Adair-Rohani H, et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990-2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. (2012) 380:2224–60. doi: 10.1016/s0140-6736(12)61766-8
PubMed Abstract | Crossref Full Text | Google Scholar
4. GBD 2017 Diet Collaborators. Health effects of dietary risks in 195 countries, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. (2019) 393:1958–72. doi: 10.1016/S0140-6736(19)30041-8
PubMed Abstract | Crossref Full Text | Google Scholar
7. NCD Risk Factor Collaboration (NCD-RisC). Worldwide trends in hypertension prevalence and progress in treatment and control from 1990 to 2019: a pooled analysis of 1201 population-representative studies with 104 million participants. Lancet. (2021) 398:957−80. doi: 10.1016/S0140-6736(21)01330-1
PubMed Abstract | Crossref Full Text | Google Scholar
8. You L, Zhao J, Chen X, Yang L, Liu M, Pan Y, et al. National essential public health services programs over the past decade research report two: progress and achievements of the lmplementation of national essential public health services programs over the past decade. Chin General Pract. (2022) 25:3209–20. doi: 10.12114/j.issn.1007-9572.2022.0407
Crossref Full Text | Google Scholar
9. Mills KT, Bundy JD, Kelly TN, Reed JE, Kearney PM, Reynolds K, et al. Global disparities of hypertension prevalence and control: a systematic analysis of population-based studies from 90 countries. Circulation. (2016) 134:441–50. doi: 10.1161/CIRCULATIONAHA.115.018912
PubMed Abstract | Crossref Full Text | Google Scholar
10. Feng YJ, Wang HC Li YC, Zhao WH. Hypertension screening and follow-up management by primary health care system among Chinese population aged 35 years and above. Biomed Environ Sci. (2015) 28:330–40. doi: 10.3967/bes2015.047
PubMed Abstract | Crossref Full Text | Google Scholar
11. Kejun L, Mei W. Economic burden of main chronic non-infectious diseases in China. Chin Health Econ. (2005) 77–80. doi: 10.3969/j.issn.1003-0743.2005.10.031
Crossref Full Text | Google Scholar
12. Liu M, Sun L, Liu G. Economic burden and economic risk of five major chronic diseases among Chinese urban residents. J Peking Univ. (2014) 46:782–9. doi: 10.3969/j.issn.1003-0743.2005.10.03
PubMed Abstract | Crossref Full Text | Google Scholar
13. Zhang Y, Chai P, Zhai T, Wan Q. Study on accounting and analysis of curative expenditure on cardio-cerebrovascular diseases in China. Chin Circ J. (2020) 35:859–65. doi: 10.3969/j.issn.1000-3614.2020.09.003
PubMed Abstract | Crossref Full Text | Google Scholar
14. Zhou P, Cheng J, Gu S, Liu C. Analysis on the treatment cost and influencing factors of hypertension patients in Hainan province. Chin Health Econ. (2020) 39:62–4. doi: 10.7664/CHE20200416
Crossref Full Text | Google Scholar
15. GBD 2016 Causes of Death Collaborators. Global, regional, and national age-sex specific mortality for 264 causes of death, 1980-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet. (2017) 390:1151–210. doi: 10.1016/S0140-6736(17)32152-9
PubMed Abstract | Crossref Full Text | Google Scholar
16. Yang G, Wang Y, Zeng Y, Gao GF, Liang X, Zhou M, et al. Rapid health transition in China, 1990-2010: findings from the Global Burden of Disease Study 2010. Lancet. (2013) 381:1987–2015. doi: 10.1016/S0140-6736(13)61097-1
PubMed Abstract | Crossref Full Text | Google Scholar
17. GBD 2016 Mortality Collaborators. Global, regional, and national under-5 mortality, adult mortality, age-specific mortality, and life expectancy, 1970-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet. (2017) 390:1084–150. doi: 10.1016/s0140-6736(17)31833-0
PubMed Abstract | Crossref Full Text | Google Scholar
18. Gregory AN, Anastasia U, Anouk D-L, Maureen O-R, Kimberly GB. Health care costs by type of expenditure across eGFR stages among patients with and without diabetes, cardiovascular disease, and heart failure. J Am Soc Nephrol. 31:1594–601. doi: 10.1681/asn.2019121308
PubMed Abstract | Crossref Full Text | Google Scholar
19. Blakely T, Kvizhinadze G, Atkinson J, Dieleman J, Clarke P. Health system costs for individual and comorbid noncommunicable diseases: an analysis of publicly funded health events from New Zealand. PLoS Med. (2019) 16:1002716. doi: 10.1371/journal.pmed.1002716
PubMed Abstract | Crossref Full Text | Google Scholar
20. Wierzejska E, Giernaś B, Lipiak A, Karasiewicz M, Cofta M, Staszewski R. A global perspective on the costs of hypertension: a systematic review. Arch Med Sci. (2020) 16:92689. doi: 10.5114/aoms.2020.92689
PubMed Abstract | Crossref Full Text | Google Scholar
21. Gheorghe A, Griffiths U, Murphy A, Legido-Quigley H, Lamptey P, Perel P, et al. The economic burden of cardiovascular disease and hypertension in low- and middle-income countries: a systematic review. BMC Public Health. (2018) 18:975. doi: 10.1186/s12889-018-5806-x
PubMed Abstract | Crossref Full Text | Google Scholar
22. Muka T, Imo D, Jaspers L, Colpani V, Chaker L, van der Lee JS, et al. The global impact of non-communicable diseases on healthcare spending and national income: a systematic review. Eur J Epidemiol. (2015) 30:25177. doi: 10.1007/s10654-014-9984-2
PubMed Abstract | Crossref Full Text | Google Scholar
23. Li L, Yang M, Song J, Yu Y, Huang H. Network meta-analysis of the antihypertensive effect of traditional Chinese exercises on patients with essential hypertension. J Healthc Eng. (2022) 2022:9419037. doi: 10.1155/2022/9419037
PubMed Abstract | Crossref Full Text | Google Scholar
24. Zhong D, Li J, Yang H, Li Y, Huang Y, Xiao Q, et al. Tai Chi for essential hypertension: a systematic review of randomized controlled trials. Curr Hypertens Rep. (2020) 3:25. doi: 10.1007/s11906-020-1031-y
PubMed Abstract | Crossref Full Text | Google Scholar
25. Dai L, Jiang Y, Wang P, Chen K. Effects of three traditional Chinese fitness exercises combined with essential hypertension: a systematic review and network meta-analysis of randomized controlled trials. Evid Based Comp Altern Med. (2021) 22:70472. doi: 10.1155/2021/2570472
PubMed Abstract | Crossref Full Text | Google Scholar
26. Expert Consensus on Diagnosis and Treatment of Hypertension with Traditional Chinese Medicine. Chin J Exp Trad Med Form. (2019) 25:217–21.
27. Xing M, Xiong X. Interpretation of expert consensus on diagnosis and treatment of hypertension with traditional Chinese medicine. Chin J Exp Trad Med Form. (2022) 28:192–205. doi: 10.13422/j.cnki.syfjx.20221191
PubMed Abstract | Crossref Full Text | Google Scholar
28. Wu S, Jiang N, Shi Y, Zhao X, Guo Z, Liu J, et al. Observation on the therapeutic effect of Xiaochaihu decoction on hypertension vertigo with liver heat and phlegm dampness syndrome. Chin Arch Trad Chin Med. (2022) 40:169–72. doi: 10.13193/j.issn.1673-7717.2022.01.040
Crossref Full Text | Google Scholar
29. Cui S, Li R, Zhou Y. Clinical effect of Xinkeshu tablets combined with irbesartan on abdominal obesity complicated with essential hypertension and hyperlipidemia. Chin Jo Clin Ration Drug Use. (2022) 15:103–5. doi: 10.15887/j.cnki.13-1389/r.2022.16.032
Crossref Full Text | Google Scholar
30. Zhang J, Wei W. Clinical study on Puerarin injection combined with irbesartan for primary hypertension of type of static blood obstructing the internal. New China Med. (2022) 54:94–6. doi: 10.13457/j.cnki.jncm.2022.12.020
Crossref Full Text | Google Scholar
31. He J, Sun N, Yang Z, Shu T, Huang W, Fang Q. Analysis of hospitalization costs and their influencing factors in patients with primary diagnosis of pulmonary arterial hypertension. Chongqing Med. (2023) 52:2685–9. doi: 10.3969/j.issn.1671-8348.2023.17.024
PubMed Abstract | Crossref Full Text | Google Scholar
32. Chen M, Kong F, Su B, Wei X, Yang J. Factors influencing hospitalization cost for diabetic patients in traditional Chinese medicine hospitals in Qingyang City, China. Int J Environ Res Public Health. (2022) 19:13859. doi: 10.3390/ijerph192113859
留言 (0)