Mental health, including emotional, psychological, and social well-being, is important at every stage of our life (1, 2). It enables people to realize their full potential, work productively and make meaningful contributions to their communities (2–4). Furthermore, proper psycho-emotional health involves a normal emotional, behavioral, and social maturity to a person (5). Work place violence derails such mental health of healthcare workers. Work place violence against healthcare workers is a problem of growing interest in research and has been poorly prioritized in healthcare systems (6). Violence against healthcare workers are varied and a complex phenomenon (7).
Psycho-emotional abuse (Verbal abuse, sexual and racial harassment, bullying/mobbing and other threats) was the most reported worked place violence in many countries (7, 8). Psycho-emotional abuse is any non-physical pattern of behavior that intentionally harms an individual’s mental state and undermines their ability to reach their full potential (5, 9). It results from a person’s dislike towards a person or object, especially when they feel like that person or object did something wrong (10–12). Psycho-emotional abuse may be overt or covert and can be tricky to spot – even by the person experiencing it (11). The abuser’s behaviors are deliberate and intentional and often rooted in envy, fragility, and aggression. It may manifest in forms of harassment, intimidation, or other threatening disruptive behavior that may occurs at the work site (5, 9).
Verbal abuse leaves no visible scars, but the emotional damage can be devastating (6). Today, doctors pay more attention to a person’s emotions and behaviors as indicators of potential health issues than ever before. Acts of violence and other injuries is currently the third-leading cause of fatal occupational injuries in the United States. Psycho-emotional violence at work has many negative impacts both at the organizational and individual level, such as the erosion of individual’s self-esteem, debases their sense of achievement, diminishes their sense of belonging, prevents their healthy and vigorous development, and takes away the individual’s well-being (11, 13). Some of the specific consequences include: decreased job performance and job satisfaction, confusion, self-blame, depression, inability to concentrate, lack of motivation, procrastination, low self-esteem, fear of failure, hopelessness, worthlessness, and self-sabotage (11).
The prevalence of psycho-emotional violence varies between countries and across different professions. In countries like Egypt (7) and Jordan (14) verbal abuse was reported to be 69.5% among nurses and (63.5%) among physicians, respectively. In Barbados, psycho-emotional abuse (60% verbal abuse, 19% bullying, 7% sexual harassment and 3% racial harassment) were found to be high among medical staffs (8). The prevalence of verbal abuse and sexual harassment was found to be a little bit higher in Riyadh (79.5 and 76.5% respectively) (15) and Saudi Arabia (75.6%) (16). Similarly, verbal abuse was found to be high among nurses working in psychiatry hospital in Jordan (71.9%) (17).
Being female (8); age, being nurse and night work (18); working when understaffed, working directly with volatile people, drug and alcohol abuse, inadequate security, long waits for service (19); working in psychiatry hospitals or psychiatry department (17) were identified as major factors for such violence.
Cases of severe psycho-emotional trauma, if left unmanaged, may lead to retaliatory violence, chronic illness, or even suicide and fear of future events. Although there have been numerous studies on psycho-emotional, there is no consensus regarding the current status of psychological violence directed at health care workers in in low income counties like Ethiopia. This study aimed to identify service providers’ experience of psycho-emotional violence and its associated factors in eastern Ethiopia.
Methods Study design, setting and periodA cross-sectional study was conducted among health professionals working at public hospitals in eastern Ethiopia, including Harar and Dire Dawa, located 525 km and 515 km from the capital of Ethiopia (Addis Ababa), respectively. Harari region has one general and one comprehensive and specialized university hospital, whereas the Dire Dawa city administration has one general and one referral hospital that serves millions of people located in the eastern part of Ethiopia. According to the Harari National Region Health Bureau report/evidence, approximately 560 healthcare workers were working in these health institutions. Similarly, the two public hospitals in Dawa had approximately 400 healthcare providers at the time of the study. This study was conducted from January 18 to February 10, 2022.
Study population and sampling procedureMulti-stage sampling was used to randomly select health professionals working in selected public hospitals in eastern Ethiopia based on their institutional identification number. All health professionals who had been in these public hospitals for more than 6 months were included in this study. All healthcare professionals on annual leave, or maternity leave, and those who were critically ill during data collection were excluded from the study. The sample size is calculated using the single population proportion formula by taking the prevalence of psycho-emotional trauma among health professionals from previous studies (prevalence in % 95 confidence level and 5% margin of error using a study conducted in Gonder Referral Hospital) (20). The final sample size was proportionally allocated to each health facility based on the actual number of healthcare workers. The health professionals were then stratified by professional category as doctors/health officers, nurses/midwives (nurses, midwives, nursing assistants, and theatre attendants), laboratory technicians, and pharmacists. The sample size in each hospital was proportionally allocated to each healthcare professional category according to their number. Finally, simple random sampling was used to select the required sample.
Data collection and quality control proceduresData were collected by health professionals (BSc Public Health officers) using a structured questionnaire prepared by the World Health Organization (21) which contains both open- and closed-ended questions as well as other workplace violence assessment tools from other similar studies (7, 22–24) that were adopted and modified in such a way that could meet the objectives of this study. The questionnaire contained questions on psycho-emotional violence, individual factors, work-related factors, and organizational factors that directly met the objectives of the study. Data quality was ensured through the training of data collectors, pre-testing of questionnaires, electronic data collection (Kobo collect), and supervision of the data collection process. In addition, respondents were encouraged to respond to all items in the questionnaire within the time they devoted to minimizing a large non-response rate. The completeness and consistency of the data were checked by the data collectors immediately after receiving the questionnaire from each participant. The questionnaire was pretested at Haramaya Hospital in 5% of the sample.
Variables and measurementsThe main outcome variable was psycho-emotional violence (verbal abuse, bullying/mobbing, harassment, and threats) experienced by study participants in the last 12 months, answered with yes or no questions.
Workplace violenceIncidents when staff members are abused, threatened, or assaulted in circumstances related to their work, including commuting to and from work, involving an explicit or implicit challenge to their safety, well-being, or health.
Psychological violence (emotional abuse)The intentional use of power, including the threat of physical force, against another person or group that can harm physical, mental, spiritual, moral, or social development. These include verbal abuse, bullying/mobbing, harassment, and threats. This was measured with a yes or no answer if the health professional experienced one of these violence.
AbuseBehavior that humiliates degrades or otherwise indicates a lack of respect for the dignity and worth of an individual. This was measured with a yes or no answer if the health professional experienced one of the violence.
Bullying/MobbingRepeated and overtime offensive behavior through vindictive, cruel, or malicious attempts to humiliate or undermine an individual or group of employees. This was measured with a yes or no answer if the health professional experienced one of this violence.
HarassmentAny conduct based on age, disability, HIV status, domestic circumstances, sex, sexual orientation, gender reassignment, race, color, language, religion, politics, trade union or other opinion or belief, national or social origin, association with a minority, property, birth, or another status that is unreciprocated or unwanted, which affects the dignity of men and women at work.
Sexual harassmentAny unwanted, unreciprocated, and unwelcome behavior of a sexual nature that is offensive to the person involved, and causes that person to be threatened, humiliated, or embarrassed. This was measured with a yes or no answer if the health professional experienced one of this violence.
Racial harassmentAny threatening conduct based on race, color, language, national origin, association with a minority, birth, or another status that is unreciprocated or unwanted, which affects the dignity of women and men at work. This was measured with a yes or no answer if the health professional experienced one of these violence.
ThreatPromised use of physical force or power (i.e., psychological force) results in fear of physical, sexual, psychological harm, or other negative consequences to the targeted individuals or groups. This was measured with a yes or no answer if the health professional experienced one of these violence.
Emotional healthRefers to the emotional quality experienced by an individual. The emotional health outcomes of WPV include emotional exhaustion, detachment, sadness, frustration, and anger.
Data processing and analysisData from the Kobo collection were downloaded into Excel and exported to Stata 16. Data were cleaned and analyzed using descriptive summary measures, such as percentage, frequencies, and mean/median and standard deviation (SD), as appropriate, and presented using tables and graphs. Logistic analysis with a 95% confidence interval was used to determine the factors associated with psycho-emotional violence and its determinants. Variables with p-values less than or equal to 0.25 were entered into a multivariable logistic regression model. Hosmer-Lemeshow’s goodness-of-fit tests were used to determine the goodness of fit for the final model. In multivariate analysis, variables with a p-value less than 0.05 were considered to be significantly associated with psycho-emotional violence.
Results Health workers characteristicsA total of 744 healthcare providers were interviewed. More than half of the study participants 53.76 and 58.84% were males and married, respectively. The median age of the study participants was 31(+7) years, and the median work experience was 6 (+7.30SD) years. A total of 17 (2.28%) were senior managers (Table 1).
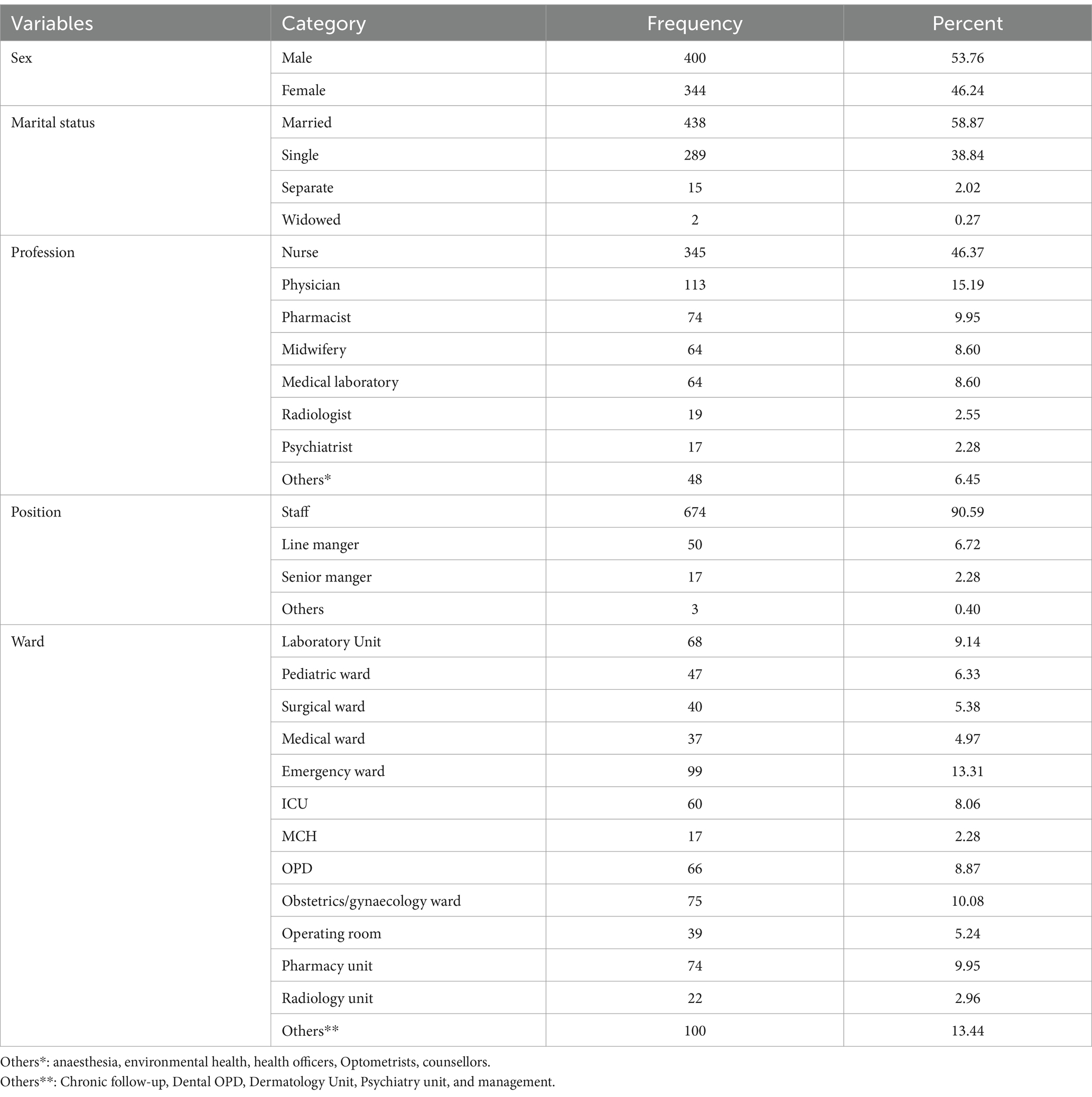
Table 1. Socio-demographic characteristics of the study participants, eastern Ethiopia, 2022.
Prevalence of psycho-emotional violencePsycho-emotional violence was reported by 57.39% of the HCWs. Verbal violence was reported by 71.37% (531/744) of participants. In contrast, bullying/mobbing was reported by 13.71% (102/744) of participants. Sexual and racial harassment was reported by 0.94% (7/744) and 9% (65/744) of health professionals, respectively.
Sources of psycho-emotional violence against health professionalsAccording to the findings of this study, patient families accounted for 61.6% (434) of verbal violence cases, while patients themselves accounted for 40% (282) of verbal violence cases. Regarding the main source of bullying/mobbing, patients’ relatives accounted for 5.8% (41) of the main sources and patients themselves accounted for 3.1% (22). Similarly, the main sources of racial harassment were relatives of relatives, 38 (5.4%), followed by staff members (3.5%, 25). Furthermore, the main source of sexual harassment was staff members (0.42%) (3), followed by patients themselves (0.29%) (2) (Table 2).
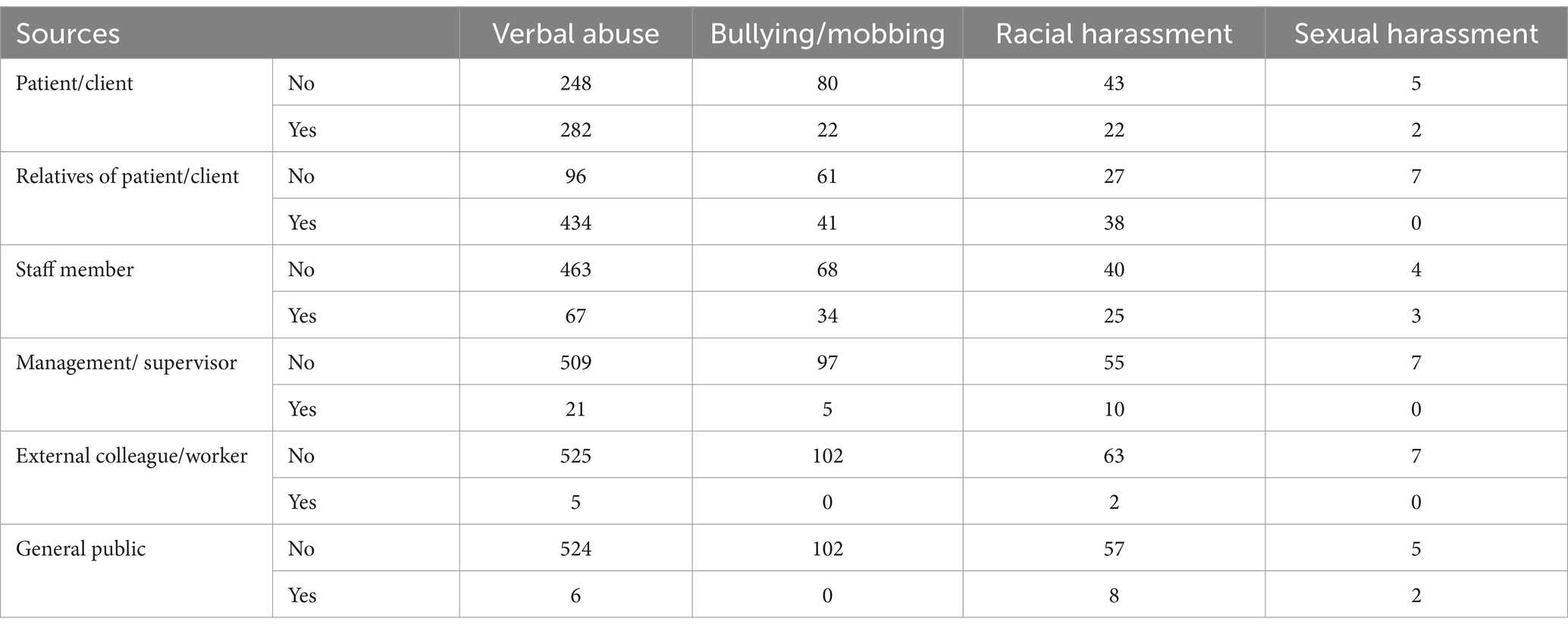
Table 2. Sources of psycho-emotional violence against healthcare providers, eastern Ethiopia, 2022.
Actions taken after psycho-emotional violence incidentThe majority of study participants (57.5%, 404) said they did not take any action following psycho-emotional violence against them, of which 69.3% (280) took no action following verbal abuse against them. Similarly, about 25.5% (179) of the study participants told the person to stop psycho-emotional violence, of which 83.2% (149) said to person following verbal abuse against them (Additional file 1).
Knowledge of workplace violence policies in their health facilitiesThe majority of study participants said they did not know whether their employer had developed specific policies on health safety (55.65%), physical workplace violence (62.37%), verbal abuse (63.17%), bullying/mobbing (63.84%), sexual harassment (62.10%), racial harassment (63.58%), and other threats (62.23%) (Figure 1).
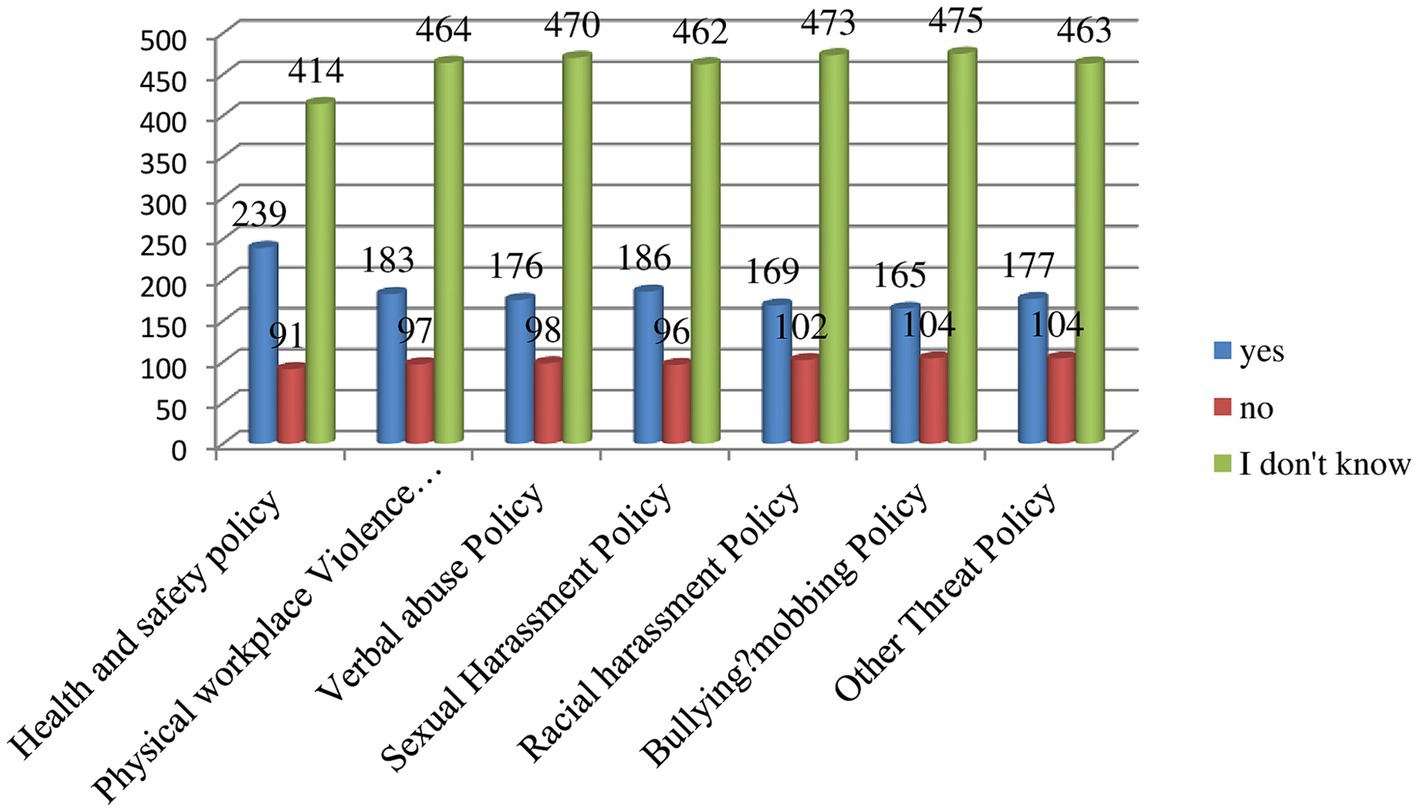
Figure 1. Knowledge of study participants whether their employer developed workplace violence policies in their health facilities, eastern Ethiopia, 2022.
Available measures to deal with psycho-emotional workplace violenceThe majority of the study participants (64.47%; 502/744) said that there was a security structure to deal with such psycho-emotional workplace violence (Figure 2).
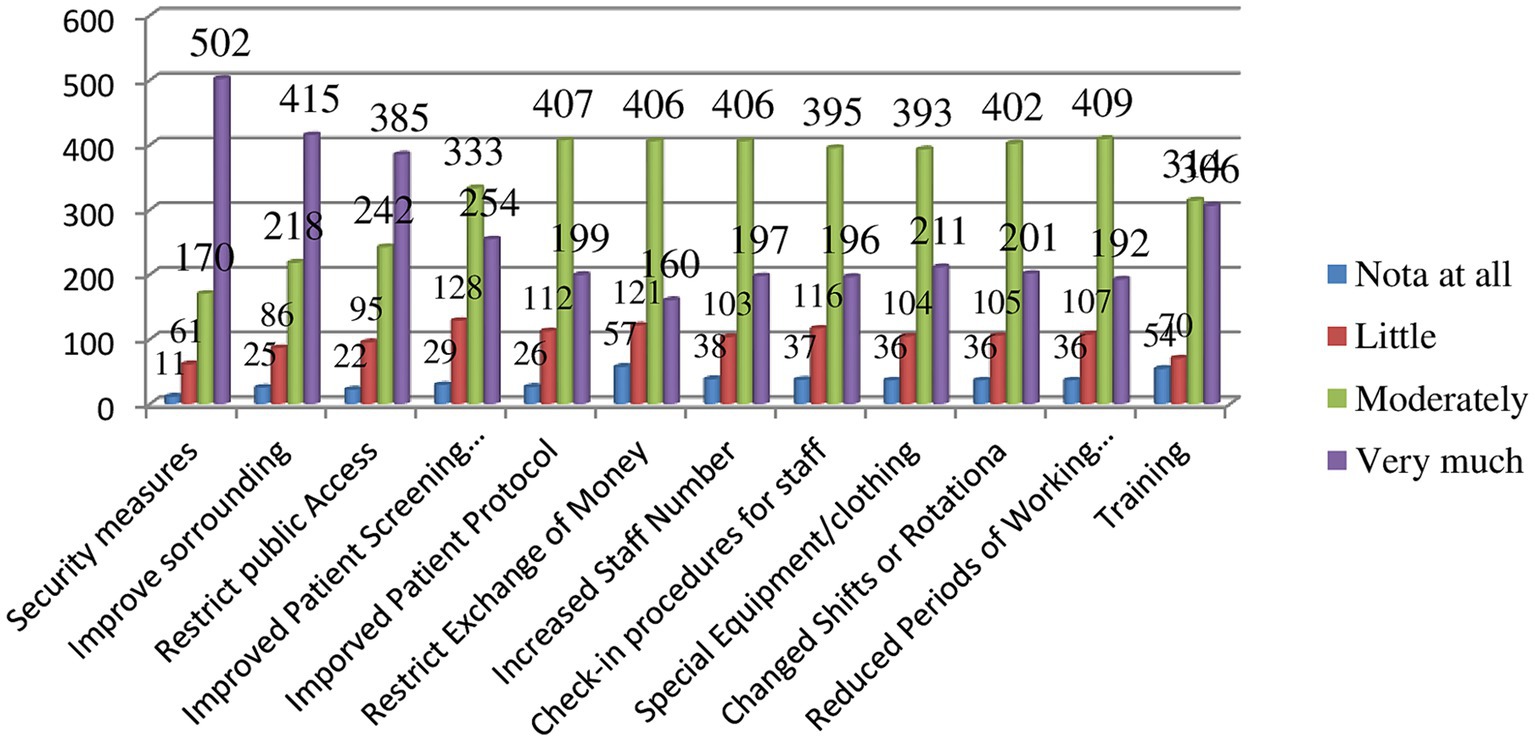
Figure 2. Available measures to deal with psycho-emotional workplace violence, eastern Ethiopia, 2022.
Factors associated with psycho-emotional violenceMultivariable logistic regression analysis showed that the absence of guidelines for gender-based abuse [AOR = 35.62, 95% CI (17.47, 72.64)], presence of measures that improve surroundings (class lighting and privacy) [AOR = 0.58, 95% CI (0.35, 0.98)], training on WPV coping mechanism [AOR = 0.16, 95%CI (0.26, 0.98)], spending more than 50% of their time with HIV/AIDS patients (AOR = 1.96, 95%CI [1.05, 3.72]), and spending more than 50% of their time with psychiatric patients [AOR = 1.92, 95%CI (1.08, 3.43)] were factors significantly associated with WPV against health professionals.
Accordingly, the odds of WPV were 35.62 times higher among health professionals in settings that had guidelines for gender-based abuse as compared to those in settings that had no guidelines [AOR = 35.62, 95% CI (17.47, 72.64)].
The odds of experiencing WPV decreased by 42% for health professionals in settings where measures that improve surroundings (class lighting and privacy) were taken as compared to in settings where such measures were not implemented [AOR = 0.58, 95% CI (0.35, 0.98)].
The odds of experiencing WPV decreased by 84% for health professionals who took training on violence coping mechanisms compared to those who did not receive training, keeping other variables in the model constant (AOR = 0.16, 95%CI [0.26, 0.98]).
The odds of WPV increased by 98% among health professionals spending most of their working time with HIV/AIDS patients compared to their counterparts while adjusting for other variables in the model (AOR = 1.98, 95%CI [1.05, 3.72]).
The odds of WPV were increased by 92% among health professionals who spend more than 50% of their time with psychiatric patients as compared to their counterparts holding other variables in the model constant [AOR = 1.92, 95%CI (1.08, 3.43)] (Table 3).
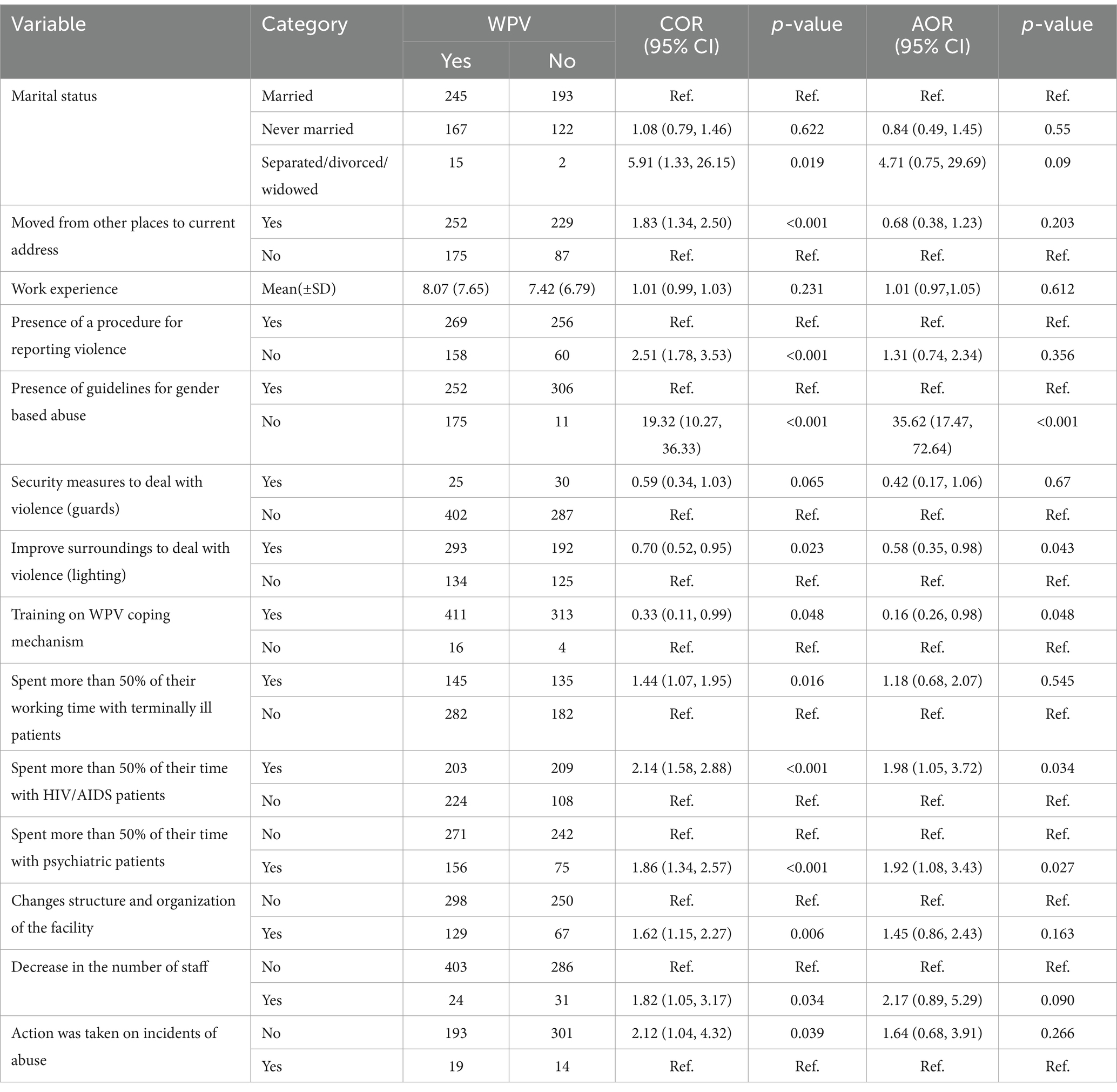
Table 3. Factors associated with psycho-emotional workplace violence against health professionals working in Public Health Facilities of eastern Ethiopia, 2022.
DiscussionThis study assessed the magnitude of WPV and its associated factors among health professionals in eastern Ethiopia. Accordingly, the finding showed 57.39% (95% CI: 53.75–60.98%) experienced WPV. This finding is in line with the prevalence reported in Brazil (25), Saudi Arabia (16), Egypt, South Africa, Thailand, and Portugal (26) and 5 European countries (Poland, the Czech Republic, the Slovak Republic, Turkey, and Spain) (23) but higher than findings from studies in southern Ethiopia (27, 28). The higher prevalence of WPV in the current study might be due to the differences in the study population. A previous study from Southern Ethiopia assessed violence against nurses, whereas the current study assessed violence against all categories of health professionals. Evidently, stress and violence are widespread in health sector where doctors, nurses and social workers experience repeated violence (25).
Most health professionals had experienced verbal abuse (71%). This is in agreement with previous studies (23–25), and might be because it is easily committed in the form of shouting, belittling, and offensive or obscene language, harassing remarks.
Similar to previous studies (29, 30), patients and patient relatives were the main sources of violence. This could be explained by the fact that patients and patient relatives might have frequent contact with health workers, which may increase the risk of health workers experiencing violence. This study also identified horizontal violence from fellow coworkers. This can be attributed to line of authority and nightshift work as stated by female healthcare workers. Female healthcare workers reported they were sexually abused by their coworkers during night shift.
This study also identified factors that were significantly associated with WPV among health workers. Improving surroundings (lighting, noise, and privacy) decreases workplace violence against health workers. This could be explained by the fact that those measures help to stop behavior that may develop into future violence and limit public access to restricted areas, which in turn reduces unnecessary contact between physicians and patients as well as patient relatives. In addition, such measures reduce the entrance of perpetrators into potential working rooms without the permission of health workers.
The absence of guidelines for gender-based abuse makes WPV against healthcare professionals 35 times more likely. This might be because the policy will inform perpetrators and victims about the kind of behavior (violence, intimidation, bullying, and harassment) considered inappropriate and unacceptable in the workplace and what to do when incidents occur. Therefore, if such guidelines are not implemented, health workers become confused about reporting incidents and the procedure that will be followed when an incident is reported, which raises the probability that violence is repeated.
The odds of experiencing WPV were lowered by 84% among health professionals who received training on violence coping mechanisms compared to those who did not receive training. This finding is in agreement with that of a previous study (31), which stated that training is a key component of reducing workplace aggression. This is because training increases the confidence and ability of health workers to recognize signs of aggression and practice evidence-based interventions to de-escalate agitated patients. In addition, training familiarizes health professionals with their legal responsibilities, risk assessment, effective communication, conflict management, and self-defence.
Working in the psychiatry department was significantly associated with WPV. The odds of experiencing WPV were higher among health professionals who spent more than 50% of their time with psychiatric patients (32) with psychiatric patients. This finding is supported by previous studies (33, 34), and this could be due to the verbal and physical aggression shown by most psychiatric patients. In addition, psychiatric patients are addicted to alcohol and illicit drugs, which might increase their aggressive behavior that makes them commit violence against health workers. This can contributes to deterioration of health care workers’ work life and health, impacts patient care delivery and hinders recruitment and retention of healthcare workers (35).
Caring for HIV/AIDS patients was another variable that was significantly associated with WPV among health professionals. Health workers who spend much of their working time with patients with HIV/AIDS are more likely to develop WPV. This finding is supported by evidence from previous studies (25, 36) where healthcare providers engaged in chronic patient care experience unprecedented psycho-emotional violence such as harassment and verbal abuse. This might be explained by comorbidities and complex medical conditions that lead to the deterioration of physical and psychological health among HIV/AIDS patients. These situations put healthcare professionals caring for HIV/AIDS patients under stressful work conditions.
The main drawback of the current study is the possibility of recall bias, as it requires participants to remember their previous experience with WPV.
ConclusionThe prevalence of Psycho-emotional violence among health professionals in eastern Ethiopia was relatively high. Measures that improve surroundings (class lighting and privacy) decrease the magnitude of WPV, whereas the absence of guidelines for gender-based abuse, lack of training on WPV coping mechanisms, and spending more than 50% of their time with psychiatric and HIV/AIDS patients increases with WPV against health professionals. We recommend that health institutions develop gender abuse mitigation guidelines and provide special training on the coping mechanisms of WPV. In addition, special protection measures are needed for workers in the psychiatry and HIV/AIDS departments.
Data availability statementThe raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statementThe studies involving humans were approved by Ethical clearance was obtained from the institutional Health Research Ethics Review Committee (IHRERC/262/2020) of the College of Health and Medical Sciences, Haramaya University. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants' legal guardians/next of kin.
Author contributionsAT: Conceptualization, Data curation, Formal analysis, Funding acquisition, Methodology, Resources, Writing – original draft, Writing – review & editing. AW: Conceptualization, Data curation, Formal analysis, Funding acquisition, Methodology, Software, Writing – original draft, Writing – review & editing. LR: Conceptualization, Data curation, Formal analysis, Funding acquisition, Methodology, Resources, Software, Validation, Writing – original draft, Writing – review & editing. BT: Conceptualization, Formal analysis, Funding acquisition, Methodology, Writing – original draft, Writing – review & editing. BM: Conceptualization, Data curation, Formal analysis, Methodology, Writing – original draft, Writing – review & editing. MT: Conceptualization, Data curation, Formal analysis, Methodology, Writing – original draft, Writing – review & editing. AC: Conceptualization, Data curation, Formal analysis, Methodology, Writing – original draft, Writing – review & editing. DE: Conceptualization, Data curation, Formal analysis, Funding acquisition, Methodology, Writing – original draft, Writing – review & editing. AG: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Visualization, Writing – original draft, Writing – review & editing.
FundingThe author(s) declare financial support was received for the research, authorship, and/or publication of this article. This work was funded by Haramaya University.
AcknowledgmentsThe authors would like to acknowledge Haramaya University for funding this study in a 2020/2021 HU Special Research Grant. The authors are thankful to the regional, zonal, Woreda health offices, health facilities, data collectors, and study participants.
Conflict of interestThe authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s noteAll claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary materialThe Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2024.1361243/full#supplementary-material
References1. Prince, M, Patel, V, Saxena, S, Maj, M, Maselko, J, Phillips, MR, et al. No health without mental health. Lancet. (2007) 370:859–77. doi: 10.1016/S0140-6736(07)61238-0
Crossref Full Text | Google Scholar
2. Goetzel, RZ, Roemer, EC, Holingue, C, Fallin, MD, McCleary, K, Eaton, W, et al. Mental health in the workplace: a call to action proceedings from the mental health in the workplace: public health summit. J Occup Environ Med. (2018) 60:322–30. doi: 10.1097/JOM.0000000000001271
PubMed Abstract | Crossref Full Text | Google Scholar
3. Keyes, CL, and Lopez, SJ. Toward a science of mental health In: Oxford handbook of positive psychology, Eds. C.R. Snyder and Shane J. Lopez. (New York: Oxford university press) (2009). 89:89–95.
6. National Observatory of Aggressions to Physicians (ONAM) WorkgroupGarrote-Díaz, JM, Becerra-Becerra, A, Bendaña-Jácome, J, Casero-Cuevas, L, Garrote-Cuevas, G, et al. National report on aggressions to physicians in Spain 2010–2015: violence in the workplace-ecological study. BMC Res Notes. (2018) 11:347. doi: 10.1186/s13104-018-3393-7,
Crossref Full Text | Google Scholar
7. Abdellah, RF, and Salama, KM. Prevalence and risk factors of workplace violence against health care workers in emergency department in Ismailia, Egypt. Pan Afr Med J. (2017) 26:21. doi: 10.11604/pamj.2017.26.21.10837
Crossref Full Text | Google Scholar
8. Abed, M, Morris, E, and Sobers-Grannum, N. Workplace violence against medical staff in healthcare facilities in Barbados. Occup Med (Oxford, England). (2016) 66:580–3. doi: 10.1093/occmed/kqw073
PubMed Abstract | Crossref Full Text | Google Scholar
9. Kumari, A, Kaur, T, Ranjan, P, Chopra, S, Sarkar, S, and Baitha, U. Workplace violence against doctors: characteristics, risk factors, and mitigation strategies. J Postgrad Med. (2020) 66:149–54. doi: 10.4103/jpgm.JPGM_96_20
PubMed Abstract | Crossref Full Text | Google Scholar
10. Strecker, PJ. I wish that he hit me: The experiences of people who have been Psychoemotionally abused and have Psychoemotionally abused others Melbourne, Australia: Victoria University Research Repository (VURR), (2012).
11. Iwaniec, D. The emotionally abused and neglected child: Identification, assessment and intervention: a practice handbook. England: John Wiley & Sons (2006).
12. Paat, Y-F, Markham, C, and Peskin, M. Psycho-emotional violence, its association, co-occurrence, and Bidirectionality with cyber, physical and sexual violence. J Child Adolesc Trauma. (2020) 13:365–80. doi: 10.1007/s40653-019-00283-z
PubMed Abstract | Crossref Full Text | Google Scholar
13. Loring, MT. Emotional abuse, © 2024 American Psychological Association. 750 first street NE. Washington, DC 20002–4242: Lexington Books/Macmillan (1994).
14. Alhamad, R, Suleiman, A, Bsisu, I, Santarisi, A, Al Owaidat, A, Sabri, A, et al. Violence against physicians in Jordan: an analytical cross-sectional study. PLoS One. (2021) 16:e0245192. doi: 10.1371/journal.pone.0245192
PubMed Abstract | Crossref Full Text | Google Scholar
15. Alharbi, FF, Alzneidi, NA, Aljbli, GH, Morad, SA, Alsubaie, EG, Mahmoud, MA, et al. Workplace violence among healthcare Workers in a Tertiary Medical City in Riyadh: a cross-sectional study. Cureus. (2021) 13:e14836. doi: 10.7759/cureus.14836
PubMed Abstract | Crossref Full Text | Google Scholar
16. Alshahrani, M, Alfaisal, R, Alshahrani, K, Alotaibi, L, Alghoraibi, H, Alghamdi, E, et al. Incidence and prevalence of violence toward health care workers in emergency departments: a multicenter cross-sectional survey. Int J Emerg Med. (2021) 14:71. doi: 10.1186/s12245-021-00394-1
PubMed Abstract | Crossref Full Text | Google Scholar
17. Al-Omari, H, Abu Khait, A, Al-Modallal, H, Al-Awabdeh, E, and Hamaideh, S. Workplace violence against nurses working in psychiatric hospitals in Jordan. Arch Psychiatr Nurs. (2019) 33:58–62. doi: 10.1016/j.apnu.2019.08.002
PubMed Abstract | Crossref Full Text | Google Scholar
18. Alsaleem, SA, Alsabaani, A, Alamri, RS, Hadi, RA, Alkhayri, MH, Badawi, KK, et al. Violence towards healthcare workers: a study conducted in Abha City, Saudi Arabia. J Fam Community Med. (2018) 25:188–93. doi: 10.4103/jfcm.JFCM_170_17
Crossref Full Text | Google Scholar
20. Yenealem, DG, Woldegebriel, MK, Olana, AT, and Mekonnen, TH. Violence at work: determinants & prevalence among health care workers, Northwest Ethiopia: an institutional based cross sectional study. Ann Occup Environ Med. (2019) 31:8. doi: 10.1186/s40557-019-0288-6
PubMed Abstract | Crossref Full Text | Google Scholar
22. Pinar, T, Acikel, C, Pinar, G, Karabulut, E, Saygun, M, Bariskin, E, et al. Workplace violence in the health sector in Turkey: a national study. J Interpers Violence. (2017) 32:2345–65. doi: 10.1177/0886260515591976
PubMed Abstract | Crossref Full Text | Google Scholar
23. Babiarczyk, B, Turbiarz, A, Tomagová, M, Zeleníková, R, Önler, E, and Sancho, CD. Reporting of workplace violence towards nurses in 5 European countries–a cross-sectional study. Int J Occup Med Environ Health. (2020) 33:325–38. doi: 10.13075/ijomeh.1896.01475
PubMed Abstract | Crossref Full Text | Google Scholar
24. d'Ettorre, G, and Pellicani, V. Workplace violence toward mental healthcare workers employed in psychiatric wards. Saf Health Work. (2017) 8:337–42. doi: 10.1016/j.shaw.2017.01.004
PubMed Abstract | Crossref Full Text | Google Scholar
25. Santos, JD, Meira, KC, Coelho, JC, Dantas, ESO, Oliveira, LVE, Oliveira, JSA, et al. Work-related violences and associated variables in oncology nursing professionals. Ciênc Saúde Colet. (2021) 26:5955–66. doi: 10.1590/1413-812320212612.14942021
PubMed Abstract | Crossref Full Text | Google Scholar
26. Di Martino, V. Workplace violence in the health sector. Country case studies Brazil, Bulgaria, Lebanon, Portugal, South Africa, Thailand and an additional Australian study. Ginebra: Organización Internacional del Trabajo. (2002):3–42.
27. Weldehawaryat, HN, Weldehawariat, FG, and Negash, FG. Prevalence of workplace violence and associated factors against nurses working in public health facilities in southern Ethiopia. Risk Manag Healthc Policy. (2020) 13:1869–77. doi: 10.2147/RMHP.S264178
PubMed Abstract | Crossref Full Text | Google Scholar
28. Fute, M, Mengesha, ZB, Wakgari, N, and Tessema, GA. High prevalence of workplace violence among nurses working at public health facilities in southern Ethiopia. BMC Nurs. (2015) 14:1–5. doi: 10.1186/s12912-015-0062-1
Crossref Full Text | Google Scholar
29. Likassa, T, Gudissa, T, and Mariam, C. Assessment of factors associated with workplace violence against nurses among referral hospitals of Oromia regional state. Ethiop J Health Med Nurs. (2017) 35:22–31.
30. Fehler-Cabral, G, Campbell, R, and Patterson, D. Adult sexual assault survivors’ experiences with sexual assault nurse examiners (SANEs). J Interpers Violence. (2011) 26:3618–39. doi: 10.1177/0886260511403761
PubMed Abstract | Crossref Full Text | Google Scholar
31. Anderson, L, FitzGerald, M, and Luck, L. An integrative literature review of interventions to reduce violence against emergency department nurses. J Clin Nurs. (2010) 19:2520–30. doi: 10.1111/j.1365-2702.2009.03144.x
PubMed Abstract | Crossref Full Text | Google Scholar
32. Lehmann, LS, McCormick, RA, and Kizer, KW. A survey of assaultive behavior in veterans health administration facilities. Psychiatr Serv. (1999) 50:384–9. doi: 10.1176/ps.50.3.384
PubMed Abstract | Crossref Full Text | Google Scholar
33. Ferri, P, Silvestri, M, Artoni, C, and Di Lorenzo, R. Workplace violence in different settings and among various health professionals in an Italian general hospital: a cross-sectional study. Psychol Res Behav Manag. (2016) 9:263–75. doi: 10.2147/PRBM.S114870
PubMed Abstract | Crossref Full Text | Google Scholar
34. Su-hsing, SL, Gerberich, SG, Waller, LA, Anderson, A, and McGovern, P. Work-related assault injuries among nurses. Epidemiology. (1999) 10:685–91. doi: 10.1097/00001648-199911000-00007
Crossref Full Text | Google Scholar
35. Needham, I, Kingma, M, O’Brien-Pallas, L, McKenna, K, Tucker, R, and Oud, N, editors. Workplace violence in the health sector. The Netherlands: KAVANAH, (2008).
36. Musengamana, V, Adejumo, O, Banamwana, G, Mukagendaneza, MJ, Twahirwa, TS, Munyaneza, E, et al. Workplace violence experience among nurses at a selected university teaching hospital in Rwanda. Pan Afr Med J. (2022) 41:64. doi: 10.11604/pamj.2022.41.64.30865
留言 (0)