The prevalence of cardiometabolic diseases, such as cardiovascular diseases, diabetes, and stroke, is an important threat to human health (1), especially among middle-aged and older populations. In recent years, the rate of cardiometabolic multimorbidity (defined herein as the presence of two or more the following cardiometabolic diseases: diabetes, heart disease, and stroke) has increased due to rising global obesity rates (2, 3). A previous large survey of nearly 40,000 people in sub-Saharan Africa showed that the prevalence of cardiometabolic multimorbidity among respondents aged 15-69 years was 4.8% (4), with a prevalence of 14.1% in the 55-69 age group (4). In China, results from a population-based survey of 500,000 people aged 30-79 years showed that the prevalence of cardiometabolic multimorbidity was 6.0% (5). Moreover, multiple studies have confirmed that cardiometabolic multimorbidity is associated with the risk of cognitive decline and dementia (6), higher mortality (7, 8), higher depressive symptoms (9), and lower quality of life (10) compared to single cardiometabolic diseases. Given these health hazards and high prevalence trends, it is important to elucidate the potential risk factors for cardiometabolic multimorbidity and target these factors for early prevention and intervention, which may help reduce the incidence of cardiometabolic multimorbidity.
Evidences from basic biological research and observational studies have identified poor socioeconomic factors (e.g., low income, low education, and a single civil status), unhealthy lifestyles (e.g., smoking, alcohol consumption, and unhealthy diet), and gut metabolite as important factors related to cardiometabolic multimorbidity (11–16). Additionally, studies have explored the association between body measures, such as grip strength (17). Obesity is now widely recognized as the most relevant risk factor for cardiometabolic multimorbidity. A review of 16 cohort studies involving 0.12 million adults in Europe and the United States found that elevated BMI was associated with an increased risk of cardiometabolic multimorbidity (18). Obesity was an important risk factor for cardiometabolic multimorbidity in middle-aged and older people (19). Furthermore, visceral adipose tissue distribution, but not overall obesity, is an independent predictor of cardiometabolic disease (20). Previous Chinese scholars constructed a Chinese visceral adiposity index (CVAI) based on a sample of Chinese people using age, BMI, waist circumference, total triglycerides (TG), and high-density lipoprotein cholesterol (HDL-C) (21). The CVAI is a superior predictor of cardiometabolic diseases, such as stroke, diabetes, and cardiovascular disease, compared with BMI (22–24). However, it is unclear whether the CVAI predicts the development of cardiometabolic multimorbidity.
To fill the aforementioned gap in the literature and provide new biomarkers for the prevention of cardiometabolic multimorbidity, our study aimed to explore the association between CVAI and cardiometabolic multimorbidity based on a national cohort.
2 Materials and methods2.1 ParticipantsThe data used in this study were obtained from a national cohort, the China Health and Retirement Longitudinal Study (CHARLS, 2011-2018 wave). The CHARLS is a nationally representative survey of middle-aged and older adults aged 45 years and older in China. Specific sampling and design details have been reported in the literature (25). We used 17708 participants from the 2011 CHARLS as potential study participants; a total of 9540 participants were included at baseline after excluding participants aged <45 years and those with missing data on CVAI, cardiometabolic multimorbidity, and covariates. We selected the 2013, 2015, and 2018 CHARLS as a follow-up survey, and 9028 participants were included in the cohort analysis after excluding participants with cardiometabolic multimorbidity at baseline, those lost to follow-up, and those with missing cardiometabolic multimorbidity data. CHARLS was approved by the Biomedical Ethics Review Committee of Peking University. Figure 1 shows the selection of participants from the CHARLS cohort.
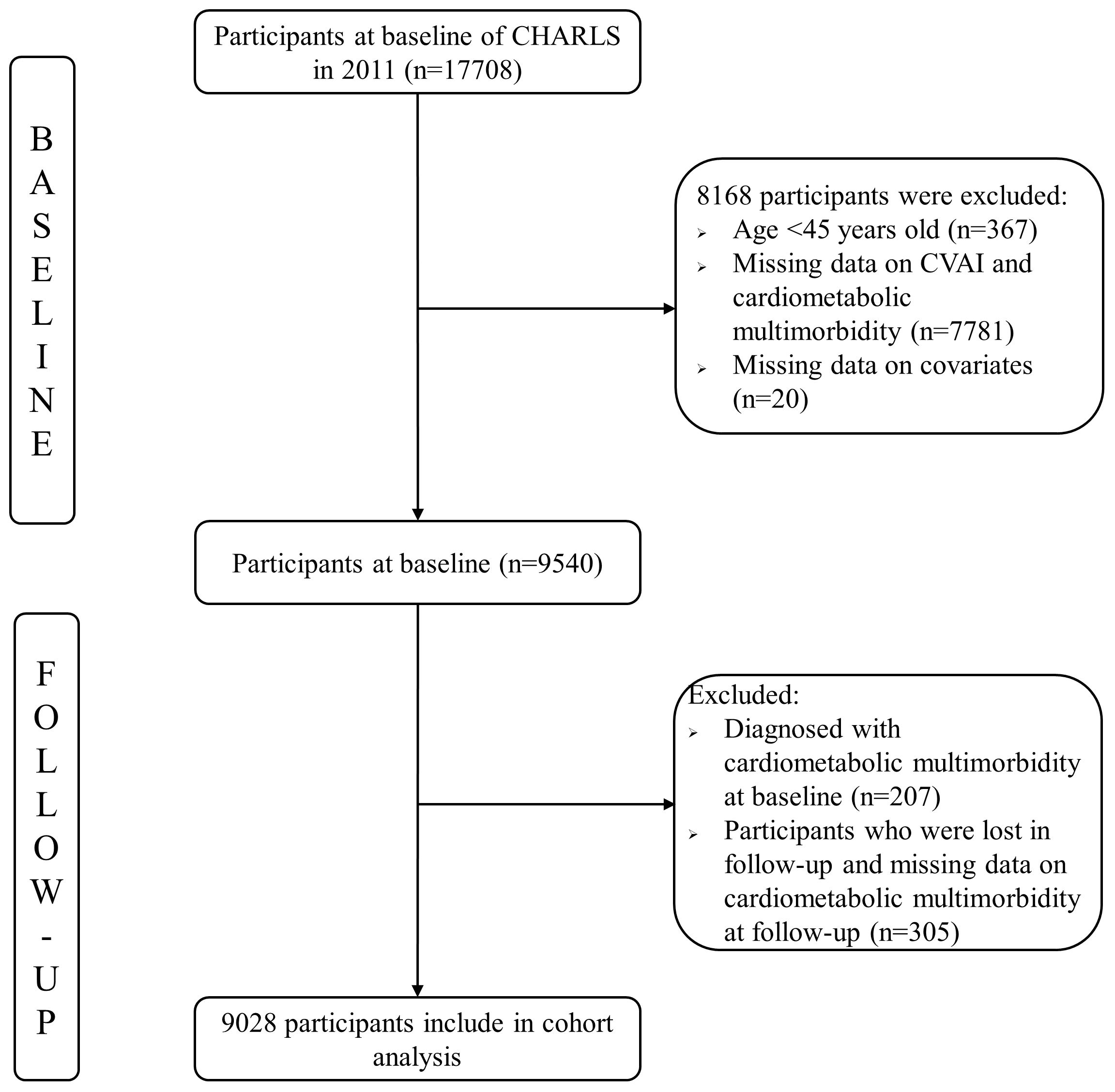
Figure 1 The selection process of the participants.
2.2 Measures2.2.1 CVAICVAI was measured using previously validated biomarker estimation formulas (21).
Males: CVAI = −267.93 + 0.68 * age + 0.03 * BMI(kg/m2) + 4.00 * WC(cm) + 22.00 * Log10TG(mmol/L) − 16.32 * HDL-C(mmol/L);
Females: CVAI = −187.32 + 1.71 * age + 4.23 * BMI(kg/m2) + 1.12 * WC(cm) + 39.76 * Log10TG(mmol/L) − 11.66 * HDL-C(mmol/L).
2.2.2 Cardiometabolic multimorbidityIn alignment with previous studies (26), we focused on three cardiometabolic diseases: diabetes, heart disease, and stroke, excluding hypertension. Participants were asked ‘Have you been diagnosed with diabetes by a doctor?’, ‘Have you been diagnosed with heart attack, coronary heart disease, angina, congestive heart failure, or other heart problems by a doctor?’ and ‘Have you been diagnosed with stroke by a doctor?’, respectively. If the participants’ answer were yes, they were considered as having the disease. The presence of two or more of these three diseases is considered as cardiometabolic multimorbidity.
2.2.3 CovariatesSocio-demographic characteristics, lifestyle, health status, and blood biomarkers were included as potential covariates. Socio-demographic characteristics included age, sex, residence, marital status, educational level, and family income (truncated by the median into low and high). Lifestyle included smoking, drinking, exercise, and participation in social activities. Health status included pain, self-rated health, health insurance, hypertension, respiratory disease, kidney disease, digestive disease, mental illness, current use of antihypertensive drugs, current use of antidiabetic drugs, and current use of antidyslipidemia drugs. Blood biomarkers included low-density lipoprotein cholesterol (LDL-C, unit: mg/dL), total cholesterol (unit: mg/dL), and fasting blood glucose (unit: mg/dL).
2.3 Statistical methodsIn this study, we used the mean ± standard deviation (SD) to describe the distribution status of continuous variables, such as BMI and frequency (composition ratio), to characterize the distribution status of categorical variables, such as sex. To clearly distinguish the association between CVAI values and cardiometabolic multimorbidity, we divided the CVAI into four equal parts according to quartiles: Q1, Q2, Q3, and Q4. We used the Cox proportional hazard regression model to explore the association between CVAI quartiles and cardiometabolic multimorbidity, adjusting for covariates. Hazard ratios (HRs) and 95% confidence intervals (CIs) were used to show the strength of the associations. To demonstrate this association, after controlling for different covariates, we constructed three Cox models. Model 1 is not adjusted for any of the variables. Model 2 was adjusted for socio-demographic characteristics. Model 3 was adjusted for lifestyles, health status, and blood biomarkers, which was initially based on Model 2. We conducted subgroup analysis to explore sex and age heterogeneity in the association between CVAI and cardiometabolic multimorbidity. Additionally, two sensitivity analyses were conducted to further assess the robustness of the association. We first excluded participants with hypertension, respiratory disease, kidney disease, digestive disease, mental illness and reran the Cox regression analyses since the CVAIs of these participants may be extremely high or low. Second, we included the CVAI as a continuous variable in the model to determine whether the association between the specific value of the CVAI and cardiometabolic multimorbidity remained statistically significant to exclude artificial loss of information due to the classifications. Finally, we also conducted the receiver operating characteristic curve (ROC) analysis and calculated area under ROC (AUC) to assess the predictive capabilities of the CVAI for cardiometabolic multimorbidity. We used the maximal Youden index to determine ideal cutoff values for CVAI prediction of cardiometabolic multimorbidity by overall, age and sex. All statistical analyses were conducted using STATA 16.0, and the test level for statistical significance was set at P < 0.05.
3 Results3.1 Descriptive statisticsThe mean age of the 9028 participants included in the final analysis was 59.3 years (SD: 9.3), with a range of 45–96 years. Of these, 4183 (46.3%) were male, and 4845 (53.7%) were female. The mean CVAI was 98.39 (SD: 50.30). The chi-square test showed statistically significant differences in the distribution of CVAI according to age, sex, residence, marital status, educational level, smoking, drinking, social activity participation, hypertension, kidney disease, digestive disease, cardiometabolic multimorbidity, body mass index, waist circumference, triglyceride level, and high-density lipoprotein cholesterol level. The participants’ characteristics are shown in Table 1.
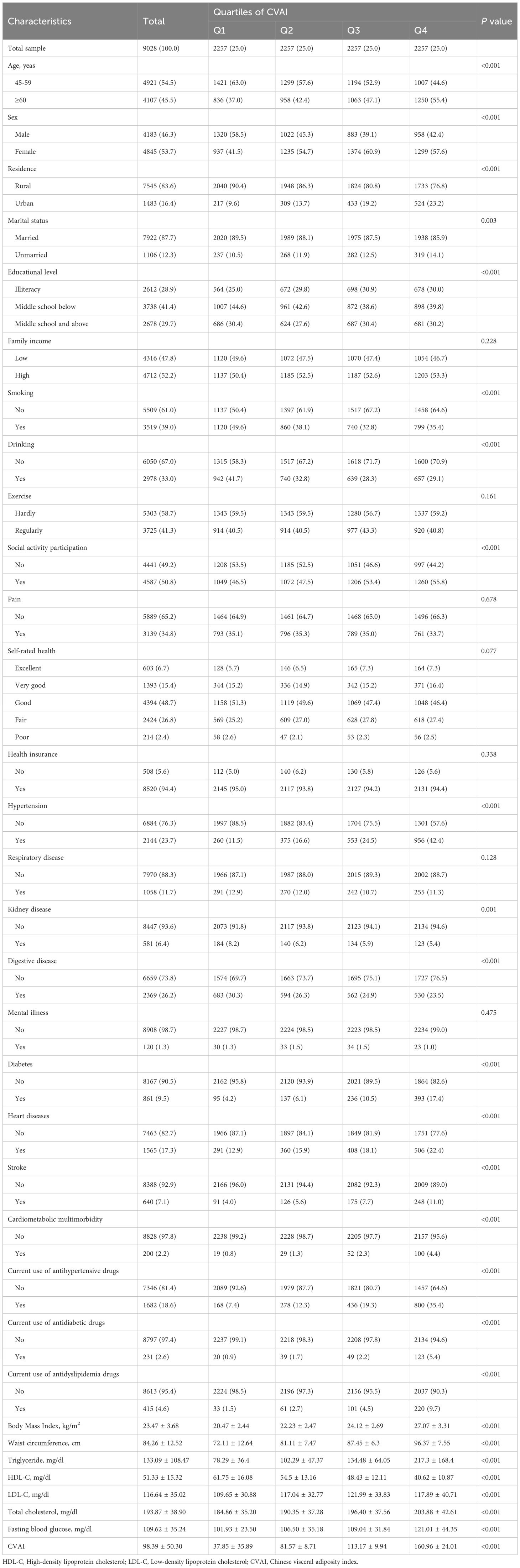
Table 1 Characteristics of participants according to CVAI.
3.2 Cox hazard modelTable 2 displays the associations between CVAI quartiles and cardiometabolic multimorbidity. In the unadjusted model, compared with the Q1 of CVAI, the Q3 and Q4 of CVAI were all significantly associated with a high incidence of cardiometabolic multimorbidity. After adjusting for age, sex, residence, marital status, educational level, and family income, the association between CVAI quartiles and cardiometabolic multimorbidity remained significant. In the fully-adjusted model, compared with participants in the Q1 of CVAI, the HRs (95% CIs) of participants in Q2, Q3, and Q4 of the CVAI for the risk of cardiometabolic multimorbidity were 1.358 (0.758 – 2.433), 2.203 (1.286 – 3.774), and 3.547 (2.100 – 5.992), respectively. Additionally, a linear association was observed between the CVAI quartiles and the incidence of cardiometabolic multimorbidity in all Cox models (P <0.001).
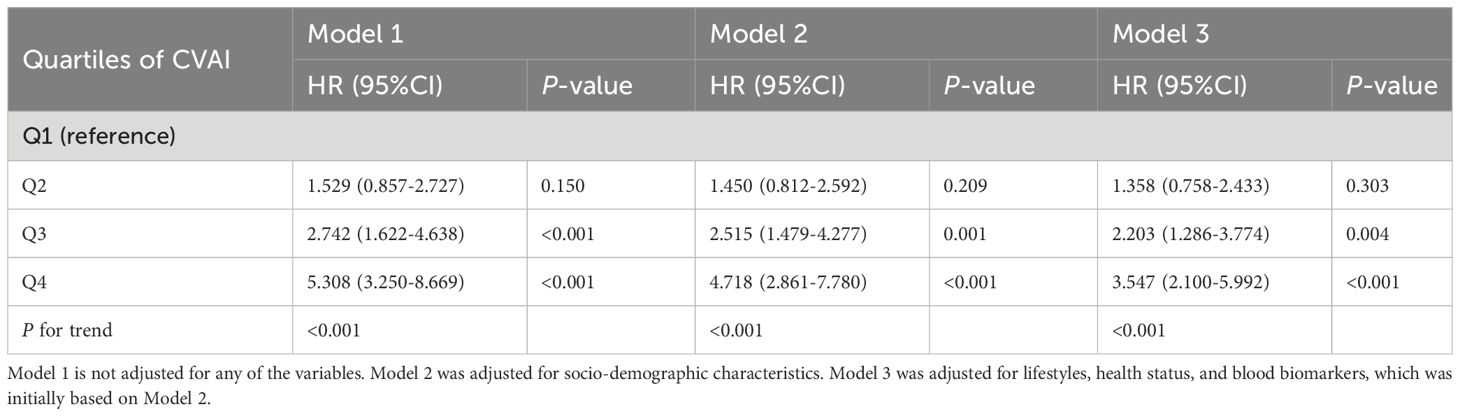
Table 2 Associations between CVAI and cardiometabolic multimorbidity.
3.3 Subgroup analysesThe results of the subgroup analyses for sex and age are presented in Table 3. The association found between the CVAI quartiles and cardiometabolic multimorbidity remained statistically significant (P<0.05) in males and middle-aged adults aged 45-59 years. Meanwhile, only the Q4 of CVAI was associated with an increased risk of cardiometabolic multimorbidity in females and older adults aged 60 years or more. Additionally, there was no evidence of an interaction between the CVAI quartiles and sex or age in association with cardiometabolic multimorbidity (P for interaction >0.05).

Table 3 Subgroup analyses of CVAI and cardiometabolic multimorbidity.
3.4 Sensitivity analysisIn the first sensitivity analysis, we excluded participants with hypertension, respiratory disease, kidney disease, digestive disease, and mental illness, and performed a fully-adjusted Cox model. The results showed no substantial change in the association between CVAI quartiles and cardiometabolic multimorbidity (compared with Q1, the HRs of the participants in Q3 and Q4 were 2.708 [95%CI= 1.039-7.055], 3.966 [95%CI= 1.505-10.450]). Additionally, we conducted a second sensitivity analysis using CVAI as a continuous variable. The results suggested that the elevated CVAI values were associated with an increased risk of cardiometabolic multimorbidity (HR= 1.011, 95%CI= 1.007-1.014). The results of both sensitivity analyses suggested that the association between CVAI and cardiometabolic multimorbidity was robust.
3.5 Predictive capability of the CVAI for cardiometabolic multimorbidityThe results of predictive capability of the CVAI for cardiometabolic multimorbidity are presented in Table 4. The AUC of overall, male group, female group, the aged <60 years, and the aged ≥60 was 0.685 (95% CI = 0.649-0.722), 0.702 (95% CI = 0.649-0.759), 0.668 (95% CI = 0.618-0.728), 0.701 (95% CI = 0.647-0.756), and 0.660 (95% CI = 0.610-0.711), respectively. The ideal cutoff value for CVAI prediction of cardiometabolic multimorbidity was 121.388 in total sample. For each group, the following cutoff values were 102.378 in male, 136.554 in female, 101.927 in the aged <60 years group, and 132.568 in the aged ≥60 years group. More details are displayed in Table 4.

Table 4 Predictive capability of the CVAI for cardiometabolic multimorbidity.
4 DiscussionOur study explored the association between CVAI and cardiometabolic multimorbidity among middle-aged and older Chinese adults based on a national cohort. We found a linear association between the CVAI quartiles and the risk of cardiometabolic multimorbidity. Compared with the participants in Q1 of the CVAI, those in Q3 and Q4 had a 135% and 278% higher risk of future cardiometabolic multimorbidity, respectively. The results of ROC analyses indicate that CVAI has good predictive capability for cardiometabolic multimorbidity. This study suggests that the CVAI may be a reliable biomarker for predicting the occurrence of cardiometabolic multimorbidities in clinical settings.
The association between CVAI and cardiometabolic diseases has been confirmed in several previous studies. For example, a recent study based on the CHARLS found that an increase in the CVAI predicted the risk of developing future strokes among middle-aged and older adults (23). A U-shaped relationship was also found between CVAI and type 2 diabetes mellitus (27). Additionally, evidence suggests that the CVAI is associated with cardiometabolic multimorbidity. In a cohort study involving more than 2,000 patients with type 2 diabetes, elevated CVAI was found to increase the risk of cardiovascular events (28). Additionally, the risk of stroke in patients with metabolic syndrome increased with increased CVAI (29). A cross-sectional study of Chinese older adults showed a linear association between CVAI and the prevalence of hypertension and diabetes mellitus (30). This observational study provides strong support for our findings. According to the capacity–load model, the risk of cardiometabolic diseases is a combination of the interaction between the metabolic capacity and the load of the body (2). Obesity is thought to increase the metabolic load, leading to impaired metabolic capacity of the body and imbalances in metabolic homeostasis, leading to an increased risk of cardiometabolic diseases (31, 32). Visceral fat is mainly located in the abdominal cavity, and its increase can cause fat cells to spill over into the surrounding organs (liver, kidneys, and heart), resulting in insulin resistance, which impairs the metabolic function of these organs (20). Furthermore, elevated CVAI produces insulin resistance, leading to renal cytokine imbalance and damage to the glomerular basement membrane, initiating metabolic dysfunction in the kidneys (33–35). Additionally, a UK Biobank-based study found that pericardial adipose tissue objectively measured using cardiovascular magnetic resonance imaging significantly and positively correlated with abnormal cardiovascular structure and function (36). It has also been found that increased abdominal adipose tissue induces the production of inflammatory cytokines, leading to an inflammatory response and oxidative stress that impairs vascular endothelial function (37).
The results of the subgroup analysis revealed interesting findings. First, this study found that the association between the CVAI quartiles and cardiometabolic multimorbidity was stronger in males than in females, wherein both the Q3 and Q4 of the CVAI were associated with an increased risk of cardiometabolic multimorbidity, whereas in females only Q4 showed an association. A previous animal study based on obese mice found a stronger pro-inflammatory state in the adipose endothelial cells of male mice than in female mice, indicating that male mice are put at higher risk due to obesity (38). Additionally, animal experiments have shown that obese female mice have a higher glucose tolerance than male mice due to the anti-inflammatory properties of estrogen, which reduces immune cell infiltration and oxidative stress in the adipose tissue of female mice (39). Evidence from animal studies may partially explain our findings, but more population-based studies are needed to further elucidate the causes of these differences due to sex. Another interesting finding was that the association between CVAI quartiles and cardiometabolic multimorbidity was stronger in the middle-aged group aged 45-59 years, compared to that of older adults aged ≥ 60 years. Two previous studies reported similar findings in that the CVAI was more strongly associated with new-onset diabetes (27) and stroke (40) in the middle-aged adults compared to older adults. There exists the persistence of the “obesity paradox” in older adults, wherein the all-cause mortality is lower in the overweight BMI group compared with the normal BMI group (41). It has also been found that overweight and mildly obese individuals have a lower prevalence of cardiovascular disease and a better prognosis (42, 43). This may partially support our finding that the Q4 of the CVAI is associated with a higher risk of cardiometabolic multimorbidity in the older adult group, but not Q3. Given that only a few studies have directly explored the associations and biological mechanisms of CVAI with health outcomes in older adults, future in-depth animal experiments or long-term cohort studies are required to validate our findings.
This study has strengths in terms of its research design and analytical strategy. First, it used population-representative data from a large national epidemiological survey, which may allow our findings to be extrapolated to the entire Chinese middle-aged and elderly population. The findings of this study have a high practical value in guiding the early warning and prevention of cardiometabolic morbidity in middle-aged and elderly people, such as the incorporation of CVAI as a biomarker for cardiometabolic morbidity in primary health care. Additionally, several confounders in our statistical analyses were controlled, and subgroup analyses for age and sex were also performed, which allowed us to detect possible differences in different groups and to estimate more accurately the association between CVAI and cardiometabolic multimorbidity. A sensitivity analysis was also conducted to test the robustness of the findings. Finally, we also analyzed the predictive capability and optimal cutoff value of CVAI for cardiometabolic multimorbidity, which can be used by healthcare professionals. However, this study has some limitations. First, although we used a cohort study with a high level of evidence to explore the association between CVAI and cardiometabolic multimorbidity, observational studies were limited since these could not infer causality. In the future, causal inference methods, such as Mendelian randomization or experimental study designs, should be used to elucidate the causal relationship between the two. Second, due to database limitations, the CHARLS did not have records on the dietary, precise physical activity, specific drug usage (such as statins and antiplatelet drugs) from the participants at the time of the survey, which may lead to the omission of covariates in our study, resulting in confounding bias. Third, we excluded participants with missing variables in the baseline survey and those lost to follow-up, which created a selection bias. Finally, cardiometabolic multimorbidity was self-reported. Since the participants were tasked to report their physician-diagnosed disease, this may have been subject to recall bias.
5 ConclusionsElevated CVAI was significantly associated with a higher risk of cardiometabolic multimorbidity in middle-aged and older Chinese adults. The CVAI was found to be a valid biomarker with good predictive capability for cardiometabolic multimorbidity and can be used by primary healthcare organizations in the future for early warning, prevention, and intervention in cardiometabolic multimorbidity.
Data availability statementThe datasets presented in this article are not readily available because the data of this study can be obtained on the official website of CHARLS. Requests to access the datasets should be directed to http://charls.pku.edu.cn/.
Ethics statementThe studies involving humans were approved by Biomedical Ethics Review Committee of Peking University. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributionsXY: Conceptualization, Formal Analysis, Methodology, Software, Writing – original draft. GZ: Formal Analysis, Methodology, Writing – original draft. CH: Validation, Writing – review & editing. PW: Validation, Writing – review & editing. JL: Supervision, Writing – review & editing. MZ: Supervision, Writing – review & editing, Funding acquisition, Project administration.
FundingThe author(s) declare that financial support was received for the research, authorship, and/or publication of this article. The work was supported by Shanghai Municipal Commission of Science and Technology (No.17DZ1910605 and No.15411970200), Shanghai Municipal Health Commission (No.201540140), Shanghai Qingpu District Science and Technology Association (No.QPXHB 23-05) and Shanghai Qingpu District Health Commission (No.QWJ2022-01, No.W2019-41, No.MY2023-6, No.LX2023-4 and No.YY2023-8).
AcknowledgmentsThank all the participants and investigators for the China Health and Retirement Longitudinal Study (CHARLS).
Conflict of interestThe authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s noteAll claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References2. Miranda JJ, Barrientos-Gutiérrez T, Corvalan C, Hyder AA, Lazo-Porras M, Oni T, et al. Understanding the rise of cardiometabolic diseases in low- and middle-income countries. Nat Med. (2019) 25:1667–79. doi: 10.1038/s41591-019-0644-7
PubMed Abstract | CrossRef Full Text | Google Scholar
3. Cheng X, Ma T, Ouyang F, Zhang G, Bai Y. Trends in the prevalence of cardiometabolic multimorbidity in the United States, 1999-2018. Int J Environ Res Public Health. (2022) 19:4726. doi: 10.3390/ijerph19084726
PubMed Abstract | CrossRef Full Text | Google Scholar
4. Otieno P, Asiki G, Wekesah F, Wilunda C, Sanya RE, Wami W, et al. Multimorbidity of cardiometabolic diseases: a cross-sectional study of patterns, clusters and associated risk factors in sub-Saharan Africa. BMJ Open. (2023) 13:e064275. doi: 10.1136/bmjopen-2022-064275
PubMed Abstract | CrossRef Full Text | Google Scholar
5. Fan J, Sun Z, Yu C, Guo Y, Pei P, Yang L, et al. Multimorbidity patterns and association with mortality in 0.5 million Chinese adults. Chin Med J. (2022) 135:648–57. doi: 10.1097/cm9.0000000000001985
PubMed Abstract | CrossRef Full Text | Google Scholar
6. Dove A, Marseglia A, Shang Y, Grande G, Vetrano DL, Laukka EJ, et al. Cardiometabolic multimorbidity accelerates cognitive decline and dementia progression. Alzheimer's Dementia. (2022) 19:821–830. doi: 10.1002/alz.12708
CrossRef Full Text | Google Scholar
7. Zhang D, Tang X, Shen P, Si Y, Liu X, Xu Z, et al. Multimorbidity of cardiometabolic diseases: prevalence and risk for mortality from one million Chinese adults in a longitudinal cohort study. BMJ Open. (2019) 9:e024476. doi: 10.1136/bmjopen-2018-024476
PubMed Abstract | CrossRef Full Text | Google Scholar
8. Di Angelantonio E, Kaptoge S, Wormser D, Willeit P, Butterworth AS, Bansal N, et al. Association of cardiometabolic multimorbidity with mortality. JAMA - J Am Med Assoc. (2015) 314:52–60. doi: 10.1001/jama.2015.7008
CrossRef Full Text | Google Scholar
9. Huang ZT, Luo Y, Han L, Wang K, Yao SS, Su HX, et al. Patterns of cardiometabolic multimorbidity and the risk of depressive symptoms in a longitudinal cohort of middle-aged and older Chinese. J Affect Disord. (2022) 301:1–7. doi: 10.1016/j.jad.2022.01.030
PubMed Abstract | CrossRef Full Text | Google Scholar
10. Otieno P, Asiki G, Wilunda C, Wami W, Agyemang C. Cardiometabolic multimorbidity and associated patterns of healthcare utilization and quality of life: Results from the Study on Global AGEing and Adult Health (SAGE) Wave 2 in Ghana. PloS Global Public Health. (2023) 3:e0002215. doi: 10.1371/journal.pgph.0002215
PubMed Abstract | CrossRef Full Text | Google Scholar
11. Li D, Wang L, Zhou Z, Song L, Chen S, Yang Y, et al. Role of socioeconomic, lifestyle, and clinical factors in the progression of cardiometabolic multimorbidity in China: A 10-year prospective cohort study. Nutrition metabolism Cardiovasc Dis NMCD. (2022) 32:2383–91. doi: 10.1016/j.numecd.2022.06.016
CrossRef Full Text | Google Scholar
12. Singh-Manoux A, Fayosse A, Sabia S, Tabak A, Shipley M, Dugravot A, et al. Clinical, socioeconomic, and behavioural factors at age 50 years and risk of cardiometabolic multimorbidity and mortality: A cohort study. PloS Med. (2018) 15:e1002571. doi: 10.1371/journal.pmed.1002571
PubMed Abstract | CrossRef Full Text | Google Scholar
13. Freisling H, Viallon V, Lennon H, Bagnardi V, Ricci C, Butterworth AS, et al. Lifestyle factors and risk of multimorbidity of cancer and cardiometabolic diseases: a multinational cohort study. BMC Med. (2020) 18:5. doi: 10.1186/s12916-019-1474-7
PubMed Abstract | CrossRef Full Text | Google Scholar
14. Ouyang L, Yu C, Xie Z, Su X, Xu Z, Song P, et al. Indoleamine 2,3-dioxygenase 1 deletion-mediated kynurenine insufficiency in vascular smooth muscle cells exacerbates arterial calcification. Circulation. (2022) 145:1784–98. doi: 10.1161/circulationaha.121.057868
PubMed Abstract | CrossRef Full Text | Google Scholar
15. An J, Ouyang L, Yu C, Carr SM, Ramprasath T, Liu Z, et al. Nicotine exacerbates atherosclerosis and plaque instability via NLRP3 inflammasome activation in vascular smooth muscle cells. Theranostics. (2023) 13:2825–42. doi: 10.7150/thno.81388
PubMed Abstract | CrossRef Full Text | Google Scholar
16. Jin Z, Meng W, Xiao T, Deng J, Wang J, Wen J, et al. Vertical sleeve gastrectomy-derived gut metabolite licoricidin activates beige fat thermogenesis to combat obesity. Theranostics. (2023) 13:3103–16. doi: 10.7150/thno.81893
PubMed Abstract | CrossRef Full Text | Google Scholar
17. Lu Y, Li G, Ferrari P, Freisling H, Qiao Y, Wu L, et al. Associations of handgrip strength with morbidity and all-cause mortality of cardiometabolic multimorbidity. BMC Med. (2022) 20:191. doi: 10.1186/s12916-022-02389-y
PubMed Abstract | CrossRef Full Text | Google Scholar
18. Kivimäki M, Kuosma E, Ferrie JE, Luukkonen R, Nyberg ST, Alfredsson L, et al. Overweight, obesity, and risk of cardiometabolic multimorbidity: pooled analysis of individual-level data for 120 813 adults from 16 cohort studies from the USA and Europe. Lancet Public Health. (2017) 2:e277–85. doi: 10.1016/s2468-2667(17)30074-9
PubMed Abstract | CrossRef Full Text | Google Scholar
19. Qin K, Bai S, Chen W, Li J, Guo VY. Association of comorbid depression and obesity with cardiometabolic multimorbidity among middle-aged and older Chinese adults: A cohort study. Arch Gerontol Geriatr. (2023) 107:104912. doi: 10.1016/j.archger.2022.104912
PubMed Abstract | CrossRef Full Text | Google Scholar
20. Valenzuela PL, Carrera-Bastos P, Castillo-García A, Lieberman DE, Santos-Lozano A, Lucia A. Obesity and the risk of cardiometabolic diseases. Nat Rev Cardiol. (2023) 20:475–94. doi: 10.1038/s41569-023-00847-5
PubMed Abstract | CrossRef Full Text | Google Scholar
21. Xia MF, Chen Y, Lin HD, Ma H, Li XM, Aleteng Q, et al. A indicator of visceral adipose dysfunction to evaluate metabolic health in adult Chinese. Sci Rep. (2016) 6:38214. doi: 10.1038/srep38214
PubMed Abstract | CrossRef Full Text | Google Scholar
22. Han M, Qin P, Li Q, Qie R, Liu L, Zhao Y, et al. Chinese visceral adiposity index: A reliable indicator of visceral fat function associated with risk of type 2 diabetes. Diabetes/metabolism Res Rev. (2021) 37:e3370. doi: 10.1002/dmrr.3370
CrossRef Full Text | Google Scholar
23. Zhang Z, Zhao L, Lu Y, Meng X, Zhou X. Association between Chinese visceral adiposity index and risk of stroke incidence in middle-aged and elderly Chinese population: evidence from a large national cohort study. J Trans Med. (2023) 21:518. doi: 10.1186/s12967-023-04309-x
CrossRef Full Text | Google Scholar
24. Wang Y, Zhao X, Chen Y, Yao Y, Zhang Y, Wang N, et al. Visceral adiposity measures are strongly associated with cardiovascular disease among female participants in Southwest China: A population-based prospective study. Front Endocrinol. (2022) 13:969753. doi: 10.3389/fendo.2022.969753
CrossRef Full Text | Google Scholar
25. Zhao YH, Hu YS, Smith JP, Strauss J, Yang GH. Cohort profile: the China health and retirement longitudinal study (CHARLS). Int J Epidemiol. (2014) 43:61–8. doi: 10.1093/ije/dys203
PubMed Abstract | CrossRef Full Text | Google Scholar
26. Di Angelantonio E, Kaptoge S, Wormser D, Willeit P, Butterworth AS, Bansal N, et al. Association of cardiometabolic multimorbidity with mortality. JAMA. (2015) 314:52–60. doi: 10.1001/jama.2015.7008
PubMed Abstract | CrossRef Full Text | Google Scholar
27. Pan L, Xu Q, Liu J, Gao Y, Li J, Peng H, et al. Dose-response relationship between Chinese visceral adiposity index and type 2 diabetes mellitus among middle-aged and elderly Chinese. Front Endocrinol. (2022) 13:959860. doi: 10.3389/fendo.2022.959860
CrossRef Full Text | Google Scholar
28. Qiao T, Luo T, Pei H, Yimingniyazi B, Aili D, Aimudula A, et al. Association between abdominal obesity indices and risk of cardiovascular events in Chinese populations with type 2 diabetes: a prospective cohort study. Cardiovasc Diabetology. (2022) 21:225. doi: 10.1186/s12933-022-01670-x
CrossRef Full Text | Google Scholar
29. Liu Z, Huang Q, Deng B, Wei M, Feng X, Yu F, et al. Elevated Chinese visceral adiposity index increases the risk of stroke in Chinese patients with metabolic syndrome. Front Endocrinol. (2023) 14:1218905. doi: 10.3389/fendo.2023.1218905
CrossRef Full Text | Google Scholar
30. Ren Y, Cheng L, Qie R, Han M, Kong L, Yan W, et al. Dose-response association of Chinese visceral adiposity index with comorbidity of hypertension and diabetes mellitus among elderly people. Front Endocrinol. (2023) 14:1187381. doi: 10.3389/fendo.2023.1187381
CrossRef Full Text | Google Scholar
31. Wells JC. Ethnic variability in adiposity, thrifty phenotypes and cardiometabolic risk: addressing the full range of ethnicity, including those of mixed ethnicity. Obes Rev. (2012) 13:14–29. doi: 10.1111/j.1467-789X.2012.01034.x
PubMed Abstract | CrossRef Full Text | Google Scholar
32. Bosy-Westphal A, Braun W, Geisler C, Norman K, Müller MJ. Body composition and cardiometabolic health: the need for novel concepts. Eur J Clin Nutr. (2018) 72:638–44. doi: 10.1038/s41430-018-0158-2
PubMed Abstract | CrossRef Full Text | Google Scholar
36. Ardissino M, McCracken C, Bard A, Antoniades C, Neubauer S, Harvey NC, et al. Pericardial adiposity is independently linked to adverse cardiovascular phenotypes: a CMR study of 42 598 UK Biobank participants. Eur Heart J Cardiovasc Imaging. (2022) 23:1471–81. doi: 10.1093/ehjci/jeac101
PubMed Abstract | CrossRef Full Text | Google Scholar
38. Rudnicki M, Pislaru A, Rezvan O, Rullman E, Fawzy A, Nwadozi E, et al. Transcriptomic profiling reveals sex-specific molecular signatures of adipose endothelial cells under obesogenic conditions. iScience. (2023) 26:105811. doi: 10.1016/j.isci.2022.105811
PubMed Abstract | CrossRef Full Text | Google Scholar
39. Nickelson KJ, Stromsdorfer KL, Pickering RT, Liu TW, Ortinau LC, Keating AF, et al. A comparison of inflammatory and oxidative stress markers in adipose tissue from weight-matched obese male and female mice. Exp Diabetes Res. (2012) 2012:859395. doi: 10.1155/2012/859395
留言 (0)