A. Caranti¹, A. Cimatti²
1 Medicine student at Otorhinolaringoiatric department at San Pier Damiano Hospital, Faenza (Ravenna), Italy
2 Head of Otorhinolaringoiatric dept. at San Pier Damiano Hospital, via Portisano 1, 48018 Faenza (Ravenna), Italy
ABSTRACT
Inflammatory pseudotumor of the parotid gland is a benign clinical finding of unknown origin, rarely reporter in literature, with only about twelve cases reported. Clinique and radiograph profiles are similar, and often confuse, with the ones of malign tumors, and only histological investigation can discriminate it. In our report, we describe a case of inflammatory pseudotumor of parotid gland in a 53 years old man, HIV and HCV positive, who accessed to our department for surgical excision of a right parotid mass. Ultrasound, CT scan and preoperatory examination showed a nodularity with regular edge propending for Warthin tumor diagnosis. Histologic examination of surgical excision concluded for a proliferative fibrous lesion with inflammatory components and positive for Actine compatible with diagnosis of Inflammatory Pseudotumor. Keywords: Inflammatory pseudotumor (IPS) – parotid gland – head and neck pseudotumor.
CASE REPORT
A 53 years old male patient, was admitted to our Clinic in november 2015 due to tumefaction of right parotid gland. The lesion was not related to any relevant systemic symptoms like fever, asthenia, or weight loss. Clinical examination revealed a nodular hard lesion, with regular border and without pain, spontaneous or evocated. In anamnesis, the patient result positive for HIV and chronic carrier for HCV. He has also an history of HBV and HAV positivity in the past. Heavy smoker (20 cigarettes/day) and work exposed to asbestos, he has an history of BPCO with sporadic acute events due to right lug. Hypercholesterolemia and BMI of 27.3 Kg/m2 was also reported. In the past, recurrent tumefactions of thyroid gland with diagnosis of thyroid cist not associated with TSH value alteration. He has been already operated for adeno-tonsilectomy, appendectomy, reparation of Achilles’ tendon and bilateral turbinoplasty. Blood tests was not significates (RBC and WBC was normal, PCR < 0,1 mg/dl, Fibrinogen 441, Creatinine 0,70 mg/dl and non disionemya). Ultrasound examination showed a moderated volume augmentation of the right parotid gland and inside its parenchyma a hypo-anechoic nodularity of 20×32 mm, characterized by regular edge and low augmentation of vascular flow. CT scan, due with and without contrast medium, concluded for a neoformation of 30x20x25 mm, with regular edge compatible with diagnosis of Warthin tumor. There was not evidence of later cervical lymphadenopathies. In accord with patient, was programmed a surgical excision of parotid lateral lobe that included the neoformation. After two day of convalescence, patient was resigned without complications. Histologic examination of excision relived a proliferative sclerotic lesion of parotid parenchyma and lymph node. On the other hands, foam macrophages were also relived. Successive immunohistochemistry examination was positive to Actin and negative for Keratina, S-100, Caldesmone, P-63, Desmine and CD-34. Research for alcolacid resistant mycobacterial was negative. The conclusive diagnosis lead to Inflammatory Pseudotumor, probably due to reactive event. After two month of follow-up, patient has not reported compliances due to surgical intervention.
DISCUSSION
Inflammatory pseudotumor can be defined as a localized mass made up of a fibrous stroma and chronic inflammatory infiltrates with a predominance of plasma cells or histiocytes and an absence of anaplasia and mitotic figures (1). It was first described in 1939 by Brunn. It affects more often childhood or early adulthood than adult, with a preference for female and more frequent in non-European population. IPSs can appear in many different parts of the human body, most often reported are lung, liver, spleen and orbit (2,3). It is also known as an inflammatory myofibroblastic tumor, plasma cell granuloma, xanthomatous pseudotumor or inflammatory fibrosarcoma (4). Someren, in 1978, classified IPTs into 3 category based on histological finding:
1) Xanthogranuloma type (or Histiocytic type) pseudotumors,
2) Plasma cell granuloma type pseudotumors,
3) Sclerotic (or sclerosing granulomatous type) pseudotumors (3,4).
Microscopically, lesions are characterized by four typical components: histiocytes, myofibroblasts, plasma cells and lymphocytes. Also, this cellular types are positive for actin, vimentin and CD3. Stromal it’s often edematous and with vascularization augmentation. Macroscopically, pseudotumors could emulate a malignancy, manifesting itself as an isolated or multiply lesions, with dimensions starting under 1 cm to 25 cm as top size (4). Ultrasound finding evidence a spherical mass with net edge and without calcification (2). Etio-pathogenesis is actually unknown and the main theories about it including inflammatory reaction due to infectious agent, traumatism, ischemia or autoimmune disease (2,4). In particular, Arber et al claim the hypothesis of a parenchymal infection by EpsteinBarr virus leading to IPS (5). On the other hand, Kamisawa et al reported that autoimmune diseases like IgG4 sclerosing cholangitis, could also lead to pseudotumor (6). At head and neck level IPSs have been described involving the orbits, larghiando
ynx, rhinopharynx, Maxillary sinus, thyroid gland and salivary glands, in particular parotid, with only a case in literature about submandibular gland (3,7). In parotid gland, pseudotumor manifests itself like a parotid swelling. At palpation, it’s a hard and nodular lesion that could be associated to later cervical lymphadenopathies, dolor, and systemic symptoms like fever, asthenia and weight loss. On the other hand, facial nerve involvement has never been reported (2,3). In literature, there are not report about positive tumor markers (like ? fetoproteins, carcinoembryonic antigens, etc.) even in blood analysis also in lesion histologic. Other laboratory finding may be negative, or may show elevated erythrocyte sedimentation rate, C-reactive protein levels elevation and, sometimes, an augmentation of white blood cell count. Clinical finding and CT scan are not usually not conclusive, and differential diagnosis should include other inflammatory disease and malignance. FCNA is not always conclusive so, biopsy is necessary to confirm the diagnosis (1). Therapy with corticosteroids has an effectiveness unrecognized, with the exception of retro-orbit IPS. The surgical excision is the only curative therapy, with a rarely cases of recidivism (2).
REFERENCES
1) Thirumaran N.S. et al. – “Inflammatory pseudotumor of Parotid Gland – a case report” – Journal of Evolution of Medical and Dental Sciences/ Volume 2/ Issue 42/ October 21, 2013;
2) Oudidi A. et al. – “Inflammatory pseudotumors of parotid gland. One case study” – La Lettre d’Oto-rhino-laryngologie et de chirurgie cervico-faciale – no 302 – janvier-février – 2006;
3) Barrios Sánchez G.M. et al. – “Inflammatory pseudotumor of the parotid gland” – Med Oral Patol Oral Cir Bucal 2005;10:371-5;
4) Zhang Y. et al. – “Inflammatory pseudotumor of the liver: A case report and literature review” – Intractable Rare Dis Res. 2015 Aug; 4(3): 155–158;
5) Arber D. et al. – “Frequent presence of the EpsteinBarr virus in inflammatory pseudotumor” – Hum Pathol 1995;26:1093-8;
6) Kamisawa T. et al. – “IgG4-related sclerosing disease” – World J Gastroenterol. 2008 Jul 7; 14(25):3948-55.;
7) Williams S.B. et al. – “Inflammatory Pseudotumors of the Major Salivary Glands. Clinicopathologic and immunohistochemical analysis of six cases.” – Am J Surg Pathol 1992;16:896902.
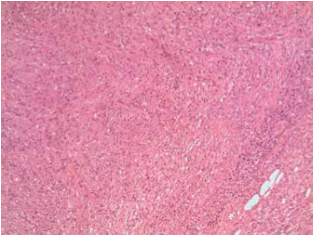 Fig. 1
Fig. 1
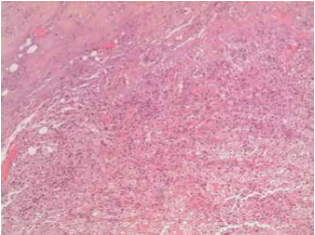 Fig. 2
Fig. 2
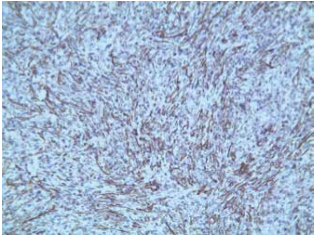 Fig. 3
Fig. 3
留言 (0)