Atrial fibrillation (AF) is the most common type of arrhythmia worldwide, and its prevalence in middle—to low-income countries is underestimated (1). AF in the developed world is well studied. Still, there is little data on AF management and demographics in the Middle East, with only four data registries (2). AF-related research in Arab countries contributes only 0.7% of AF research worldwide (3).
Syria has been suffering from a conflict since 2011. It has been deprived of healthcare funding and resources, particularly exacerbated during the cholera and COVID-19 outbreaks (4, 5). Therefore, less than 50% of its hospitals operate as usual, with more than half its healthcare workforce forced to leave the country due to conflict (6). AF management in hospitals during the current economic and political turmoil is unclear, with a scarcity of published inpatient figures and outcomes originating from Syrian healthcare (7–10). Although late advances in AF management have enhanced the AF burden and symptom control, readmission rates continue to increase and have been one of the primary sources of AF-related financial constraints on healthcare economies around the world. One crucial problem is the fact that up to around one-third of AF may be asymptomatic (11), and this may account for a large proportion of the 20% of patients who suffer a stroke without any apparent underlying cause. In a previous study, subclinical atrial tachyarrhythmia detected by implanted devices (defibrillators or pacemakers) was associated with a more than two-fold increase in thromboembolic events (12). In the developed world, opportunistic screening for AF has been explored in pharmacy settings and primary care (13, 14). However, this has proven challenging in a conflict setting such as Syria, where the main patient pool is inside hospitals admitted through the emergency department (ED). Therefore, we aimed to explore the feasibility of opportunistic AF screening in a tertiary Syrian ED department to assess the prevalence of undiagnosed AF.
Methods Study design and data collectionThis single-centre cross-sectional observational study was conducted at Tishreen's University Hospital, Latakia, Syria. It is a large teaching hospital and tertiary care centre with around 860 beds. On average, the hospital provides free healthcare to approximately 50,000–60,000 inpatients yearly, with an even more significant number of outpatients seeking care in various medical departments. The ED has around 50 beds across different units, including triage, critical care, and observation. The study included patients over 40 years old reporting the ED between the 1st of July 2024 and the 1st of September 2024. A 12-lead ECG was conducted routinely regardless of the presenting complaint. Two general cardiology consultants blindly reviewed ECGs. We excluded patients with a critical condition or hemodynamic instability, and patients with discrepancies in ECG diagnosis between the two cardiology consultants. ED and medical clinical charts were examined for patients’ demographics. The research reported in this article adhered to the Declaration of Helsinki. The project was conducted as part of an audit approved by the hospital board and involved prospective analysis of anonymised collected data (reference: 277/C). The reporting of this observational study followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines (15).
Study outcomesThe study's primary outcomes included the prevalence of AF in patients presenting to ED. A secondary analysis explored the correlation between demographics and the presence of AF.
Statistical analysisContinuous variables are expressed as median and interquartile range (IRQ). Categorical variables are expressed as counts and percentages (%). Pearson's χ 2 or Fisher's exact test was used for categorical variables between groups. Students’ t-tests and Kruskal–Wallis tests were used to compare continuous variables between the groups depending on the normality of the distribution. We used logistic regression to examine the relationship between demographics and AF presence. Our multivariable model was constructed a priori and included demographics that are statistically significant in the univariable model. A 2-sided p-value <0.05 was considered statistically significant. Statistical analysis was performed using GraphPad Prism V10.3 for Mac (San Diego, California, USA).
Results Patients characteristics and primary outcomesAfter applying the selection criteria in Figure 1, 694 patients were included in the final analysis, of which 101 had unknown AF proven on the 12-lead ECG (15%). Demographics are demonstrated in Table 1. Males comprised 57% of the cohort, with a median age of 61 (IQR: 52–68 years). Compared to the rest of the patients, AF patients were older (66 vs. 59 years; p < 0.001), had a lower proportion of males (39% vs. 54%; p = 0.01), a higher prevalence of diabetes mellitus (49% vs. 21%; p = 0.01), and more cases of congestive cardiac failure (CCF) (38% vs. 17%; p < 0.001). This resulted in a higher CHA₂DS₂-VASc score in AF patients [3 [2–4] vs. 2 [1–3]; p < 0.001]. Other ECG findings and patients’ presenting complaints are shown in Figure 2. ECG was normal in 247 (36%). The most common ECG abnormality was sinus tachycardia in 115 patients (17%), and the most common presenting complaints were trauma (44%), followed by respiratory complaints (12%) and chest pain/syncope (7%).
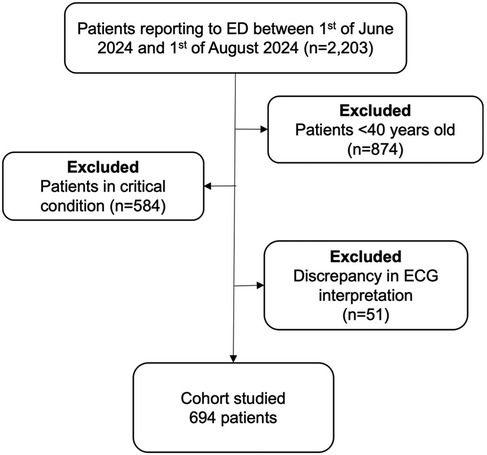
Figure 1. Flow chart of the patient selection criteria. AF, atrial fibrillation; ED, emergency department.
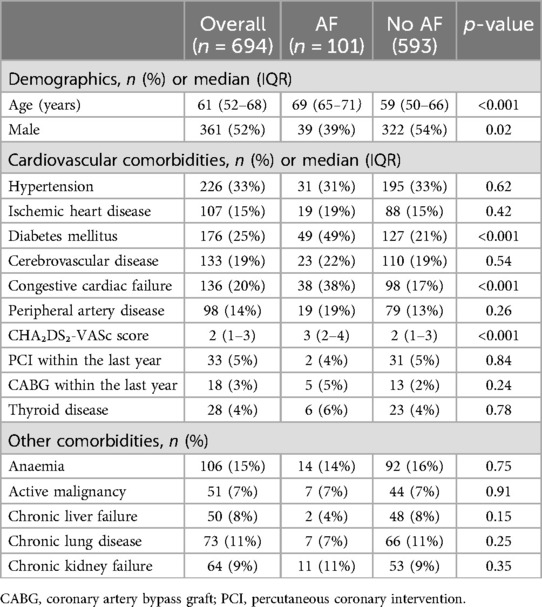
Table 1. Demographics and characteristics of patients stratified by 12-lead electrocardiogram results.
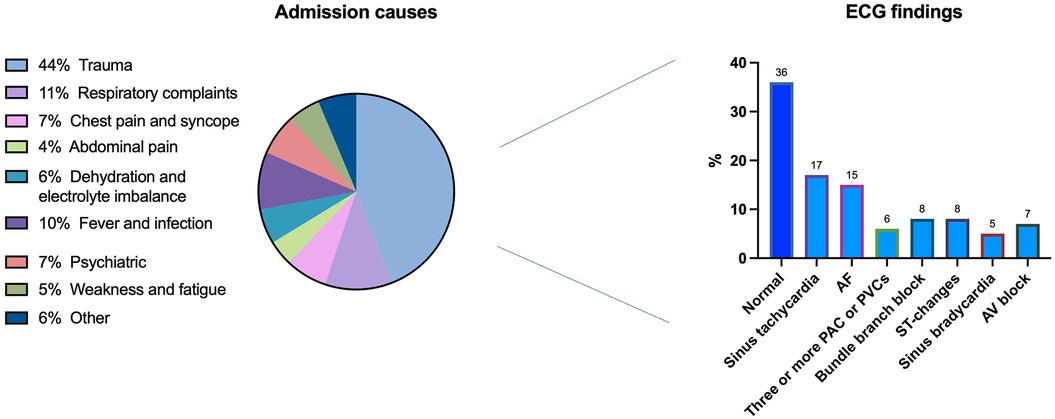
Figure 2. Admissions aetiology and electrocardiogram results. ECG, electrocardiogram; AF, atrial fibrillation; PAC, premature atrial contraction; PVC, premature ventricular contraction.
Secondary outcomesLogistic regression models are demonstrated in Table 2. Univariable regression showed that older age [odds ratio [OR]: 2, 95% confidence interval [CI]: 1.2–3.8, p = 0.02], females (OR: 2.2, 95% CI: 1.2–4.1, p = 0.01), DM (OR: 2.3, 95% CI: 1.2–4.2, p = 0.004), CCF (OR: 3.1, 95% CI: 1.5–5.7, p = 0.01) and a higher CHA₂DS₂-VASc score (OR: 2, 95% CI: 1.6–2.5, p < 0.001) were associated with positive AF screening. The multivariable logistic regression model demonstrated that CCF (OR: 3.3, 95% CI: 1.5–6.4, p < 0.001) and a CHA₂DS₂-VASc score (OR: 4, 95% CI: 1.6–7.7, p < 0.001) were independently associated with positive AF screening.
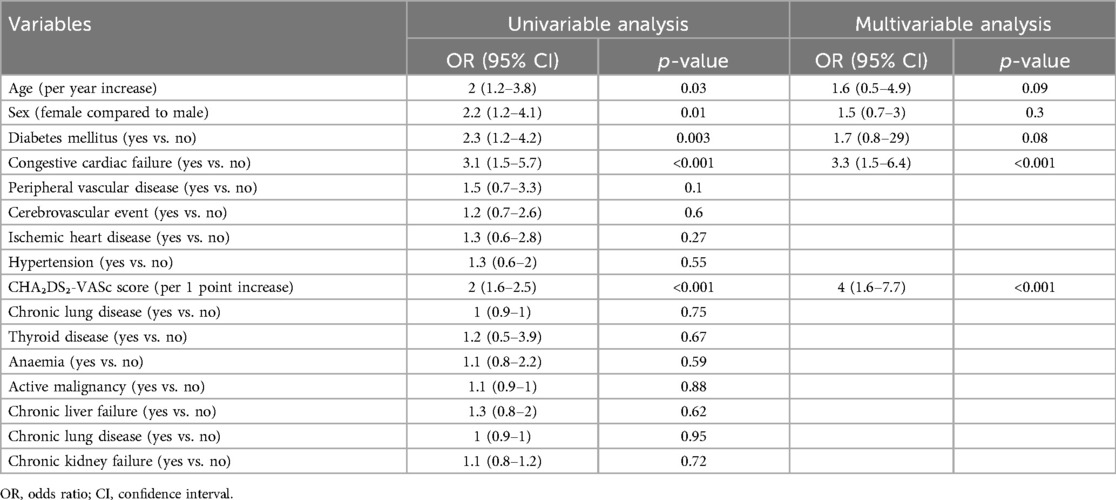
Table 2. Logistic regression model regarding predictors of atrial fibrillation in the study.
DiscussionThis is the first study describing the utility of opportunistic ED-based screening for AF in Syria and the Middle East. It highlights two significant novel findings for the Syrian-Arabic population: 15% had a positive screening for AF, and the CHA2DS2-VASc score and CCF were independently associated with positive AF screening.
As AF is known to have enormous implications on economies worldwide (16), recent studies have focused on many aspects of AF, including hospitalisation and readmission rates (17, 18). AF screening can identify more cases, but there is limited evidence on how it affects health outcomes. Anticoagulation treatment was associated with a reduced risk of mortality and first stroke, but it also increased the risk of significant bleeding. Therefore, the exact extent of this risk is uncertain, and no trials have assessed the benefits and risks of anticoagulation specifically for screen-detected populations (19).
Previous studies have reported conflicting results on the role of ECG screening for AF detection. For example, Fitzmaurice et al. demonstrated that both systematic and opportunistic screening in primary care increased AF detection rates compared to routine practice, with no significant difference between the two approaches (20). However, this study highlighted that systematic screening required more resource allocation without significantly improving detection rates, raising questions about cost-effectiveness. On the other hand, Morgan et al. showed that systematic nurse-led screening achieved significantly higher detection rates than opportunistic screening (4.5% vs. 1.3%) (21). This finding underscores the role of healthcare professionals in enhancing AF detection, though variability in results across practices and concerns about scalability in low-resource settings remain.
Lowres et al. further demonstrated the utility of modern technology such as iECGs, which yielded a fourfold increase in AF detection compared to routine care. However, despite improved AF diagnosis, no significant reduction in clinical events (e.g., stroke) was observed, and the high cost of $10,780 per diagnosis limits its applicability, especially in resource-limited or conflict-affected settings (22). The US Preventive Services Task Force statement 2018 concluded that evidence was insufficient to assess the benefits and harms of AF screening with routine ECGs (23). However, these data were pulled from countries without conflict and with fully functional healthcare. In a conflict country, including Syria, an ED visit is an opportunity to screen for common conditions in adults and the elderly population, including AF.
Our positive AF detection of 15% far exceeds rates reported in the developed world. For example, a multicentral US-based study showed an AF prevalence of 1.1% in the ED-based screening (24). There was no previous data from a developing world country undergoing conflict for comparison. Our results can be compared to findings from various studies conducted in developing countries. This comparison is essential to understand AF's prevalence and detection rates in different healthcare settings, particularly in low-resource environments. AF prevalence in the developing world was proposed to be between 1% and 7.4% in the general population and between 1% and 56% in hospital settings, keeping with our rate (25, 26). In rural India, a community-based screening program revealed a high burden of unrecognized AF, with detection rates significantly influenced by the methodology employed. Soni et al. reported that their innovative approach, which involved randomised home-based serial screening of individuals aged 50 years and older, yielded a higher AF detection rate than previous studies that utilised a single rhythm check (27). This suggests that the detection rate can vary significantly based on the screening strategy, which may also apply to the Syrian context. Moreover, a study conducted in Sweden found a total AF prevalence of 12.3% in a screened population, indicating that similar screening efforts in different geographical locations can yield comparable detection rates (28). In another study focusing on low-resource settings, Evans et al. emphasised the feasibility of using mobile ECG technology for AF screening, which detected a significant proportion of AF cases that would otherwise remain undiagnosed (29). This suggests that the integration of technology in screening processes can enhance detection rates, potentially leading to a higher prevalence being reported in similar settings. This comparison underscores the importance of addressing resource limitations and the compounded impact of conflict on healthcare delivery, highlighting the need for tailored strategies to improve AF screening in such settings.
Our higher AF rates may partially be attributed to the Syrian conflict, which has been ongoing since 2011 and has massively affected health infrastructure. It resulted in a high turnover of skilled staff and inadequate nurses and allied health professionals (30). Only half of the country's hospitals and primary healthcare centres are fully functional (30). Although there was no data before the conflict for comparison, the current data is likely to reflect the current state of play throughout this war-torn country. This included reduced access to preventive healthcare and a higher burden of cardiovascular risk factors and disruptions in healthcare infrastructure, which likely contributed to our high AF pickup rate.
Furthermore, socioeconomic disparities may affect the ability of patients to adhere to management plans and to attend follow-up appointments. Financial constraints may also limit access to necessary interventions and medications, leading to patients developing complications from the patient's cardiac conditions (31). Furthermore, the high AF prevalence observed in this study may also be influenced by conflict-specific factors, such as psychological stress and trauma, which are known contributors to cardiovascular disease. However, due to logistical constraints in the ED, data on these variables could not be collected. Future studies should address this gap by integrating psychosocial and conflict-related stressors assessments into the study design. CCF and CHA₂DS₂-VASc scores are known predictors of AF (32, 33), and our study's findings align with those. CCF contributes to changes in the atria, increasing the prevalence of AF due to mechanical stress, activation of certain hormones, and inflammation (33). The components of the CHA₂DS₂-VASc score, particularly CCF, indicate the shared risk factors for stroke and the development of AF. The more risk factors a patient has (as noted in the CHA₂DS₂-VASc score), the greater the likelihood of developing AF. Therefore, policymakers should put a strategy to screen these patients for AF as they appear to be at a higher risk in our Syrian cohort. Our study was limited to three months due to logistical constraints and the reliance on real-time prospective data collection to ensure accuracy. However, extending the study period to a full year could provide more comprehensive data, accounting for seasonal variations in ED presentations. Future studies should consider longer data collection durations to capture a broader spectrum of AF cases and patient demographics.
This study offers new insights into the prevalence and predictors of AF in a conflict-affected environment, emphasising the feasibility of opportunistic AF screening in EDs. It highlights the necessity for further research to examine the broader impact of conflict-specific factors, such as psychological stress, on cardiovascular health. Furthermore, the findings pave the way for larger, multi-centre studies investigating AF prevalence and management in other conflict- or low-resource settings, thereby contributing to the global understanding of AF in underrepresented populations. From a clinical standpoint, this study demonstrates that routine ECG screening in the ED can effectively identify undiagnosed AF, even in resource-limited and conflict-affected environments. Identifying CHA2DS2-VASc score and CCF as independent predictors of AF can help clinicians stratify high-risk patients for targeted screening and early intervention. This approach has the potential to reduce stroke risk and improve outcomes in underserved populations by facilitating timely anticoagulation therapy and other appropriate management strategies.
LimitationsData collection was limited to a single tertiary care centre in Latakia. This city was relatively less affected by the Syrian conflict than the other northern and eastern regions of Syria. Therefore, our results might not be generalisable to other centres/regions, given the significant heterogeneity in the quality and level of hospital supplies and staffing. Additionally, our analysis included only routinely collected data within the medical records and by the number of patients who presented to the hospital. Therefore, other variables potentially impacting AF prevalence may have yet to be identified. Our ECG screening might have missed paroxysmal AF and subclinical AF patients. Thus, AF prevalence might have been underestimated. This study's duration was limited to three months, which may have introduced seasonal biases in patient presentations. Additionally, expanding the study retrospectively or prospectively for a full year could yield more representative data on AF prevalence and its associated risk factors. This remains a key area for future research.
ConclusionOpportunistic AF screening in Syrian EDs could play a crucial role in identifying AF and initiating appropriate treatment, particularly in a conflict setting where access to routine medical care is significantly limited. A higher CHA₂DS₂-VASc score and the presence of CCF were independently associated with the presence of AF.
Data availability statementThe raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statementThe studies involving humans were approved by Tishreen's University Hospital, Latakia. The studies were conducted in accordance with the local legislation and institutional requirements. The ethics committee/institutional review board waived the requirement of written informed consent for participation from the participants or the participants’ legal guardians/next of kin because data was collected anonymously and as a part of an audit approved by the institution.
Author contributionsIA: Writing – original draft, Writing – review & editing. AlkA: Data curation, Methodology, Validation, Writing – review & editing. AJ: Methodology, Writing – review & editing. AlaA: Data curation, Methodology, Writing – review & editing. IS: Writing – review & editing. KY: Writing – review & editing. RS: Writing – review & editing. GN: Writing – review & editing. MZ: Writing – review & editing.
FundingThe author(s) declare financial support was received for the research, authorship, and/or publication of this article. GAN is supported by British Heart Foundation Research Excellence Award (RE/24/130031), British Heart Foundation Programme Grant (RG/17/3/32774), Medical Research Council Biomedical Catalyst Developmental Pathway Funding Scheme (MR/S037306/1) and NIHR i4i grant (NIHR204553). MZ is supported by the British Heart Foundation (CH/12/1/29419) to the University of Leicester, which provides funding matched to this BHF award to; and the Leicester NIHR Biomedical Research Centre (NIHR203327).
Conflict of interestThe authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The author(s) declared that they were an editorial board member of Frontiers, at the time of submission. This had no impact on the peer review process and the final decision.
Generative AI statementThe author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher's noteAll claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References1. Joseph PG, Healey JS, Raina P, Connolly SJ, Ibrahim Q, Gupta R, et al. Global variations in the prevalence, treatment, and impact of atrial fibrillation in a multi-national cohort of 153 152 middle-aged individuals. Cardiovasc Res. (2020) 117(6):1523–31. doi: 10.1093/cvr/cvaa241
Crossref Full Text | Google Scholar
2. Al-Shamkhani W, Ayetey H, Lip GY. Atrial fibrillation in the Middle East: unmapped, underdiagnosed, undertreated. Expert Rev Cardiovasc Ther. (2018) 16(5):341–8. doi: 10.1080/14779072.2018.1457953
PubMed Abstract | Crossref Full Text | Google Scholar
3. Akiki D, El Hage S, Wakim E, Safi S, Assouad E, Salameh P. Atrial fibrillation in the Arab world: a bibliometric analysis of research activity from 2004 to 2019. Journal of Cardiac Arrhythmias. (2021) 34(1):12–22. doi: 10.24207/jca.v34i1.3430
Crossref Full Text | Google Scholar
4. Antoun I, Alkhayer A, Aboud Y, Alkhayer H, Kotb A, Alkhayer A, et al. COVID-19 inpatient treatments and outcomes during the conflict in Syria: an observational cohort study. IJID Regions. (2023) 7:72–6. doi: 10.1016/j.ijregi.2022.12.009
PubMed Abstract | Crossref Full Text | Google Scholar
5. Antoun I, Alkhayer A, Kotb A, Barker J, Alkhayer A, Mahfoud Y, et al. The prevalence and prognostic value of diabetes and hypertension in patients treated for cholera during the ongoing Syrian conflict. Clin Infect Pract. (2024) 23:100362. doi: 10.1016/j.clinpr.2024.100362
PubMed Abstract | Crossref Full Text | Google Scholar
7. Antoun I, Aljabal M, Alkhayer A, Mahfoud Y, Alkhayer A, Simon P, et al. Atrial fibrillation inpatient management patterns and clinical outcomes during the conflict in Syria: an observational cohort study. Perfusion. (2024) 17:2676591241259140. doi: 10.1177/02676591241259140
Crossref Full Text | Google Scholar
8. Antoun I, Alkhayer A, Aljabal M, Mahfoud Y, Alkhayer A, Simon P, et al. Thirty-day unplanned readmissions following hospitalization for atrial fibrillation in a tertiary Syrian center: a real-world observational cohort study. Heart Rhythm O2. (2024) 5(12):854–9. doi: 10.1016/j.hroo.2024.05.010
PubMed Abstract | Crossref Full Text | Google Scholar
9. Antoun I, Alkhayer A, Aljabal M, Mahfoud Y, Alkhayer A, Kotb AI, et al. Incidence, outcomes, and predictors of new heart failure in Syrian conflict-affected population following hospitalization for atrial fibrillation: a retrospective cohort study. Perfusion. (2024):02676591241283883. doi: 10.1177/02676591241283883
Crossref Full Text | Google Scholar
10. Antoun I, Alkhayer A, Eldin AJ, Alkhayer A, Yazji K, Somani R, et al. Gender disparity in quality of life in atrial fibrillation patients during the Syrian conflict: an observational cohort study. Heart Rhythm O2. (2025). In press. doi: 10.1016/j.hroo.2024.12.010
Crossref Full Text | Google Scholar
11. Savelieva I, Camm AJ. Clinical relevance of silent atrial fibrillation: prevalence, prognosis, quality of life, and management. J Interv Card Electrophysiol. (2000) 4(2):369–82. doi: 10.1023/A:1009823001707
PubMed Abstract | Crossref Full Text | Google Scholar
12. Healey JS, Connolly SJ, Gold MR, Israel CW, Van Gelder IC, Capucci A, et al. Subclinical atrial fibrillation and the risk of stroke. N Engl J Med. (2012) 366(2):120–9. doi: 10.1056/NEJMoa1105575
PubMed Abstract | Crossref Full Text | Google Scholar
13. Godin R, Yeung C, Baranchuk A, Guerra P, Healey JS. Screening for atrial fibrillation using a mobile, single-lead electrocardiogram in Canadian primary care clinics. Can J Cardiol. (2019) 35(7):840–5. doi: 10.1016/j.cjca.2019.03.024
PubMed Abstract | Crossref Full Text | Google Scholar
14. Lowres N, Neubeck L, Salkeld G, Krass I, McLachlan AJ, Redfern J, et al. Feasibility and cost-effectiveness of stroke prevention through community screening for atrial fibrillation using iPhone ECG in pharmacies. Thromb Haemostasis. (2014) 111(06):1167–76. doi: 10.1160/TH14-03-0231
Crossref Full Text | Google Scholar
15. Vandenbroucke JP, Von Elm E, Altman DG, Gøtzsche PC, Mulrow CD, Pocock SJ, et al. Strengthening the reporting of observational studies in epidemiology (STROBE): explanation and elaboration. PLoS Med. (2007) 4(10):e297. doi: 10.1371/journal.pmed.0040297
PubMed Abstract | Crossref Full Text | Google Scholar
16. Arora S, Patel P, Lahewala S, Patel N, Patel NJ, Thakore K, et al. Etiologies, trends, and predictors of 30-day readmission in patients with heart failure. Am J Cardiol. (2017) 119(5):760–9. doi: 10.1016/j.amjcard.2016.11.022
PubMed Abstract | Crossref Full Text | Google Scholar
17. Freeman JV, Wang Y, Akar J, Desai N, Krumholz H. National trends in atrial fibrillation hospitalization, readmission, and mortality for medicare beneficiaries, 1999–2013. Circulation. (2017) 135(13):1227–39. doi: 10.1161/CIRCULATIONAHA.116.022388
PubMed Abstract | Crossref Full Text | Google Scholar
18. Lahewala S, Arora S, Patel P, Kumar V, Patel N, Tripathi B, et al. Atrial fibrillation: utility of CHADS2 and CHA2DS2-VASc scores as predictors of readmission, mortality and resource utilization. Int J Cardiol. (2017) 245:162–7. doi: 10.1016/j.ijcard.2017.06.090
PubMed Abstract | Crossref Full Text | Google Scholar
19. Kahwati LC, Asher GN, Kadro ZO, Keen S, Ali R, Coker-Schwimmer E, et al. Screening for atrial fibrillation: updated evidence report and systematic review for the US preventive services task force. JAMA. (2022) 327(4):368–83. doi: 10.1001/jama.2021.21811
PubMed Abstract | Crossref Full Text | Google Scholar
20. Fitzmaurice DA, Hobbs FR, Jowett S, Mant J, Murray ET, Holder R, et al. Screening versus routine practice in detection of atrial fibrillation in patients aged 65 or over: cluster randomised controlled trial. Br Med J. (2007) 335(7616):383. doi: 10.1136/bmj.39280.660567.55
Crossref Full Text | Google Scholar
21. Morgan S, Mant D. Randomised trial of two approaches to screening for atrial fibrillation in UK general practice. British Journal of General Practice. (2002) 52(478):373–80.
22. Halcox JP, Wareham K, Cardew A, Gilmore M, Barry JP, Phillips C, et al. Assessment of remote heart rhythm sampling using the AliveCor heart monitor to screen for atrial fibrillation: the REHEARSE-AF study. Circulation. (2017) 136(19):1784–94. doi: 10.1161/CIRCULATIONAHA.117.030583
PubMed Abstract | Crossref Full Text | Google Scholar
23. Curry SJ, Krist AH, Owens DK, Barry MJ, Caughey AB, Davidson KW, et al. Screening for atrial fibrillation with electrocardiography: US preventive services task force recommendation statement. JAMA. (2018) 320(5):478–84. doi: 10.1001/jama.2018.10321
PubMed Abstract | Crossref Full Text | Google Scholar
24. Scott PA, Pancioli AM, Davis LA, Frederiksen SM, Eckman J. Prevalence of atrial fibrillation and antithrombotic prophylaxis in emergency department patients. Stroke. (2002) 33(11):2664–9. doi: 10.1161/01.STR.0000035260.70403.88
PubMed Abstract | Crossref Full Text | Google Scholar
25. Nguyen TN, Hilmer SN, Cumming RG. Review of epidemiology and management of atrial fibrillation in developing countries. Int J Cardiol. (2013) 167(6):2412–20. doi: 10.1016/j.ijcard.2013.01.184
PubMed Abstract | Crossref Full Text | Google Scholar
26. Santos IS, Goulart AC, Olmos RD, Thomas GN, Lip GYH, Lotufo PA, et al. Atrial fibrillation in low- and middle-income countries: a narrative review. Eur Heart J Suppl. (2020) 22(Supplement_O):O61–77. doi: 10.1093/eurheartj/suaa181
PubMed Abstract | Crossref Full Text | Google Scholar
27. Soni A, Earon A, Handorf A, Fahey N, Talati K, Bostrom J, et al. High burden of unrecognized atrial fibrillation in rural India: an innovative community-based cross-sectional screening program. Jmir Public Health and Surveillance. (2016) 2(2):e159. doi: 10.2196/publichealth.6517
PubMed Abstract | Crossref Full Text | Google Scholar
28. Svennberg E, Engdahl J, Al-Khalili F, Friberg L, Frykman V, Rosenqvist M. Mass screening for untreated atrial fibrillation: the STROKESTOP study. Circulation. (2015) 131(25):2176–84. doi: 10.1161/CIRCULATIONAHA.114.014343
PubMed Abstract | Crossref Full Text | Google Scholar
29. Evans GF, Shirk A, Muturi P, Soliman EZ. Feasibility of using mobile ECG recording technology to detect atrial fibrillation in low-resource settings. Glob Heart. (2017) 12(4):285. doi: 10.1016/j.gheart.2016.12.003
PubMed Abstract | Crossref Full Text | Google Scholar
31. Leyh BM, Gispen ME. Access to medicines in times of conflict: overlapping compliance and accountability frameworks for Syria. Health Hum Rights. (2018) 20(1):237.30008566
PubMed Abstract | Google Scholar
32. Saliba W, Gronich N, Barnett-Griness O, Rennert G. Usefulness of CHADS2 and CHA2DS2-VASc scores in the prediction of new-onset atrial fibrillation: a population-based study. Am J Med. (2016) 129(8):843–9. doi: 10.1016/j.amjmed.2016.02.029
PubMed Abstract | Crossref Full Text | Google Scholar
33. Martín-Pérez M, Ruigómez A, Michel A, Rodríguez LAG. Incidence and risk factors for atrial fibrillation in patients with newly diagnosed heart failure. J Cardiovasc Med (Hagerstown). (2016) 17(8):608–15. doi: 10.2459/JCM.0000000000000403
留言 (0)