Pressure injury/injuries (PI/PIs), also referred to as bedsores, decubitus, pressure ulcers, and pressure sores. It is described as localized damage caused by pressure or pressure combined with shear to the skin and/or underlying tissue (1). PIs are one of the most frequently occurring and costly, yet preventable adverse events in institutions and are of particular concern for older adults (2), which are a well-recognized complication of nursing homes (3). In China, the aging population is rapidly increasing, leading to a growing demand for long-term care facilities. By 2020, more than 254 million Chinese people were 60 years of age or older, making up 18.1% of the total population (4). This demographic shift underscores the urgent need for effective pressure injury prevention and management (PIPM) strategies in nursing homes (5). Studies showed that the prevalence of PIs in nursing homes varied from 3.4 to 32.4% globally (6), and the incidence of PIs in nursing homes varied from various countries being reported to range from 3.6 to 39.4% (7). It was reported 1.91–10.4% and 28.9% for PI prevalence and incidence in Chinese nursing homes (8, 9). PIs could trigger a tremendous burden not only on individuals but also on the healthcare systems (10).
Nursing assistants are the primary workforce and caregivers in nursing homes and are essential members of the frontline team who devote a lot of time observing and tracking the outcomes of long-term care residents (11). Therefore, nursing assistants play a crucial role in PIPM. Nursing homes are placing demands on qualified nursing assistants with positive attitudes, enhanced knowledge, and the requisite skills to deliver high-quality care services, ultimately improving the quality of life for residents (12). Bangova pointed out that insufficient knowledge or improper care behavior of nursing assistants will increase the incidence of PIs to a certain extent (13). Due to their likely insufficient knowledge and skills, a large number of nursing assistants initiated preventive care after PI was discovered, inappropriately used PI prevention materials, or performed inappropriate PIPM practices (14). Although guidelines have been provided over the years, of which this information is key when assessing skin breakdown or precursors to skin breakdown, studies showed it is rarely taught to the nursing assistants who are the personnel most likely to assess the beginning signs of skin breakdown (14). Lavallée et al. (15) conducted interviews with nursing home staff, and they identified knowledge as one barrier to PI prevention (15).
To ensure nursing assistants are competent in their work, they need to undergo an innovative education or training program to bridge the knowledge-to-action gap in nursing practice (16). International evidence has consistently identified that training can improve nursing assistants’ competencies in PIPM, strengthen the cognition toward diseases and attitude toward work, as well as promote better care and outcomes for the older adult in nursing homes (17). The Chinese Health Commission launched an advocacy on strengthening the training and standardized management of nursing assistants in 2019, which mentioned that institutions should use trained and qualified nursing assistants to engage in corresponding work, and require active training based on the training outline (18). However, currently, the limited PI-specific training programs mainly target nurses, patients, or family caregivers, and the training curriculum quality varies greatly between these programs worldwide (19, 20). There is a lack of high-quality PI training programs focused on nursing assistants working in nursing homes, especially targeted at enhancing nursing assistants’ competencies around the world. In the UK, there is no national education program for nursing assistants designed to improve skills related to skin assessment and PI prevention (21). In the USA, Wogamon (14) developed a PI training program for nursing assistants in a nursing home, but the program just included some simple content, such as PI causes, risk factors, stages, positioning, documentation, and reporting of pertinent data which were based on the outdated guideline NPUAP/EPUAP 2011. Besides, the training hours were only 2 h with lectures. In Sweden, Hultin et al. (22) trained the nursing assistants from the older adult care facility to improve their PIPM competencies mainly targeting the use of a pressure mapping system based on the outdated guideline NPUAP/EPUAP 2014. The training methods included 15 min training and 1 week of self-practice. All of these programs were not designed based on a theoretical framework. Moreover, in a review of 24 previous studies of comprehensive PI prevention programs (23), 20 of which were of programs in acute care settings and four in long-term care facilities, and most participants were nursing staff not just focused on nursing assistants. Therefore, it is very imperative and urgent to develop a comprehensive, evidence-based, theory-based, innovative training methods-based effective PI training program for nursing assistants.
Social Learning Theory (SLT) was developed by Albert Bandura (1977), and it was widely applied to various training programs in the public health field as the theoretical framework to enhance healthcare providers’ competencies (24). Applying SLT in medical education can strengthen learning behavior and solve common clinical teaching problems through learners’ observation and demonstration (25). Traditional educational models often fail to provide the necessary interactive and observational learning experiences that are essential for nursing assistants to retain and apply critical knowledge in PIPM (26). The SLT-informed model offers a practical framework to bridge this gap. The SLT is a theory of learning that takes into account how individuals learn from each other as well as how learning takes place in social contexts (27). Central to SLT are self-efficacy, knowledge, and skills. By integrating SLT into nursing training, educators can create a dynamic and effective learning environment that prepares future healthcare providers to excel in their profession (28). According to the SLT, the learning process of nursing assistants can take place through observation, imitation, and modeling from experts, which are regulated by four processes namely attention (e.g., paying attention to the online and offline learning), retention (e.g., knowledge quizzes, rehearsal practice, etc.), motor reproduction (e.g., practice feedback), and motivation (e.g., giving positive feedback, reduced workload, improved income, improved working conditions, etc.) process (29). SLT is consistent with the traditional behaviorists’ opinions that they insist upon the importance of practice and repetition in learning and positive or negative reinforcement can be used to encourage the repetition of the behavior (30). The modified Delphi method, an organized and iterative procedure that experts use to come to an agreement, provides a robust framework for developing a training program tailored to the needs of nursing assistants. This method involves multiple rounds of surveys or questionnaires, allowing experts to refine their opinions and achieve consensus on specific topics (31).
This study aims to develop a comprehensive PI training program based on SLT for nursing assistants in Chinese nursing homes using the modified Delphi method. This study can contribute to the broader goal of enhancing geriatric care and promoting the health and wellbeing of the aging population in China. In addition, This study is not only valuable for improving the quality of nursing care in Chinese nursing homes, but also has far-reaching implications for nursing practice and health policy making worldwide.
2 Materials and methods 2.1 Study designA modified two-round Delphi technique was employed to reach a consensus among a panel of experts with extensive PIPM experience. The basic idea behind the Delphi method is to use the qualitative evaluation of the evidence to derive quantitative estimates (32, 33). The development process of the SLT-based training (SLTbT) program of PI was divided into two stages: the stage of the initial draft construction of the SLTbT program by systematic reviews and qualitative study; the stage of content validity of expert panel review (Delphi Method) to form the final version of the SLTbT program. All stages were conducted between July and August 2024. The specific development process is shown in Figure 1. After identifying the research issue, the research team compiled the initial version draft of the SLTbT program of PI informed by the information acquired from the systematic reviews, focus group, and in-depth interviews. The content validation of the initial program was validated by the expert panel review approach (Delphi technique) to finalize the components of the SLTbT program by achieving a consensus from several designated experts. Based on the experts’ opinions or comments received from the content validation, the training program was revised as a final version of SLTbT program. Delphi method does not need researcher to convene the panel experts to meet face-to-face rather communication with the researcher through email, to ensure anonymity and privacy and allow each freedom of expression without outside pressure or influence (33, 34). It involved in using questionnaires to obtain the collective opinion of experts until a consensus is reached (35).
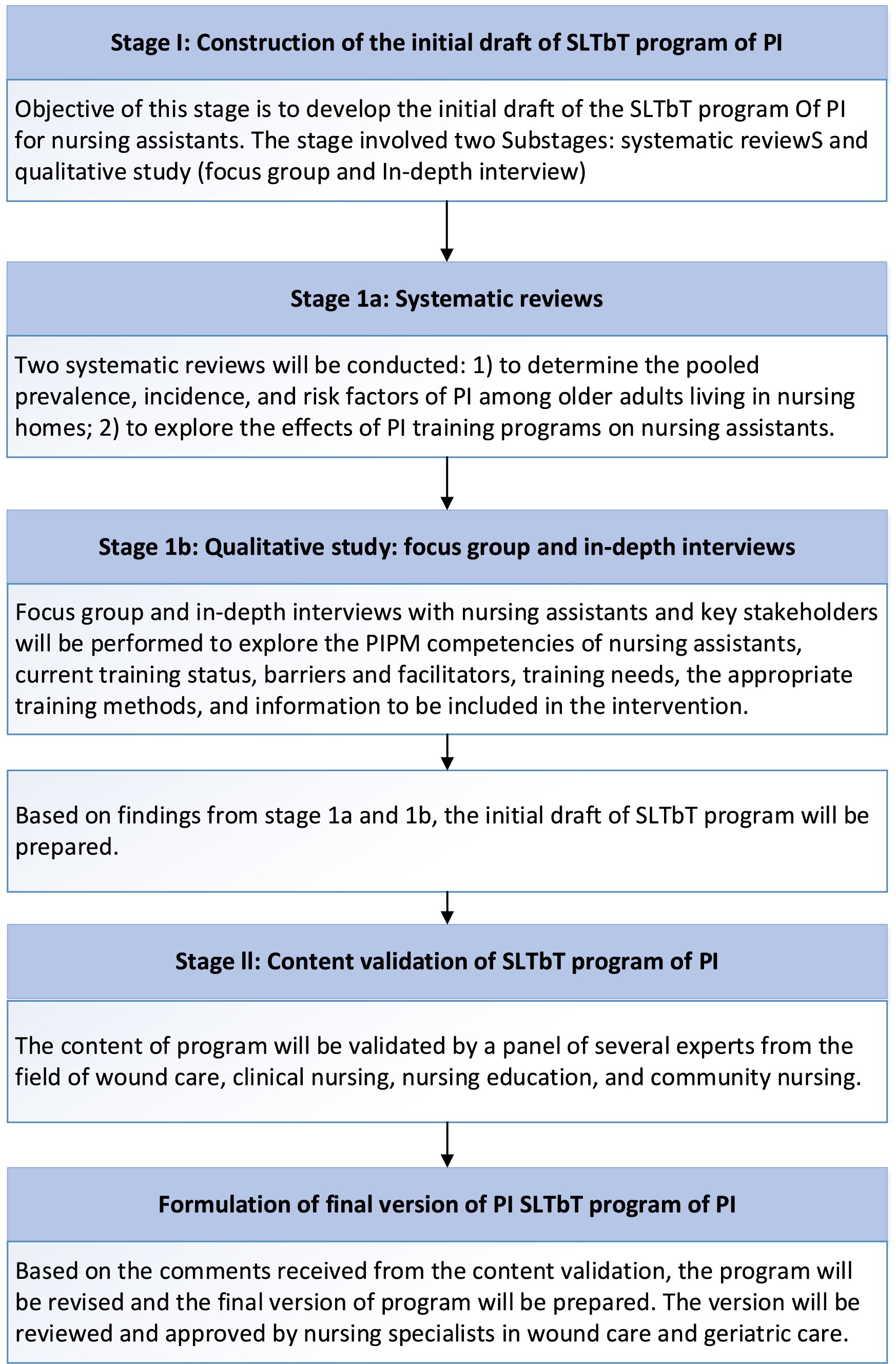
Figure 1. Process of program development.
2.2 Delphi method processThe research team confirmed the initial draft of the SLTbT program including 78 indicator items based on the systematic review, and qualitative study, and entered into the modified Delphi process.
2.2.1 Panel member recruitment and data collectionAn expert panel consisting of several content experts was invited to evaluate the appropriateness, and feasibility of the SLTbT program components using the Delphi technique with two rounds. Between July and August 2024, 15 experts were invited to participate in this study via email or WeChat. Each questionnaire was required to be completed by experts within 2 weeks and returned to the researcher. The experts were selected through purposeful sampling. The inclusion criteria for participants were: (1) come from the hospitals, community healthcare centers, or nursing educational institutions, with much expertise in PIPM; (2) have at least 5 years of wound care experience or at least 5 years of nursing teaching experience; (3) have an associate senior title or higher; (4) have rich research experience in PI field and geriatric care; (5) have a bachelor’s degree or higher. Experts who satisfied the inclusion requirements were invited to join the expert panel by sending emails or using WeChat (34). The participants who are not willing to participate in this study or those who are not interested in the study are excluded. The size of the Delphi expert panel is usually 10–15 members (36).
2.2.2 Consultation questionnaireThe SLTbT program was presented in the form of a consultation questionnaire, including three parts: introduction, expert characteristics, and appropriateness assessment of the PI training program. The initial draft of SLTbT program included 78 indicator items: 4 first-level indicators involving 4 domains (training objectives, training contents, training methods, training evaluation), 13 s-level indicators (three indicators for training objectives domain, two indicators for training contents domain, three indicators for training methods domain, five indicators for training evaluation domain), and 61 third-level indicators (27 indicators for training objectives domain, 21 indicators for training contents domain, eight indicators for training methods domain, five indicators for training evaluation domain). The appropriateness assessment used a 5-point Likert scale to rate responses for each indicator, where 1 means “not at all appropriate” and 5 means “very appropriate.” Furthermore, a column of modification opinions has been attached for experts to add, delete, and revise. The mean value and the coefficient of variation (CV) of appropriateness assignment can be evaluated to assess the experts’ agreement degree of each indicator (37).
2.2.3 Delphi round 1The researcher sent the initial consultation questionnaires to all experts’ emails or WeChat and received their response within 2 weeks. Then the researcher summarized and analyzed the experts’ opinions. Every item that satisfied the consensus filtering criteria was kept in the program. All the consensus items and the revised items based on experts’ opinions were entered into Delphi round 2.
2.2.4 Delphi round 2Experts rated their degree of agreement with each item statement once more in the Delphi round 2. The consultation was terminated when the expert panel came to a consensus following two rounds of the Delphi study.
2.3 Data analysisWe used Microsoft Excel 2010 and IBM SPSS 20.0 software to extract and analyze data. Descriptive analysis was used for the basic information of experts. The scientific soundness and rationality of the Delphi method are reflected by three indicators: experts’ positive coefficient, authority coefficient, and coordination coefficient (33).
1. The experts’ positive coefficient indicates the level of experts’ interest in the study and is represented by the response rate of the expert consultation (38). It demonstrated the experts’ strong enthusiasm for the research when it was >70%.
2. Experts’ authority coefficient (Cr) represents the reliability of the consultation results (37). Expert judgment (Ca) and expert familiarity with the research topic (Cs) were used to calculate the Cr. The formula is (Ca + Cs)/2, and a value of Cr ≥0.70 is deemed acceptable reliability (39, 40). Theoretical analysis, practical experience, knowledge from domestic and foreign literatures, and intuition served as the foundation for Ca, and the high, middle, and low levels were used to reflect the influence degree of judgment basis. The details are as follows: theoretical analysis (0.3, 0.2, 0.1), practical experience (0.5, 0.4, 0.3), knowledge from domestic and foreign counterparts (0.1, 0.1, 0.05), and intuition (0.1, 0.1, 0.05) (See Table 1). The levels of Cs were categorized ranging from “very familiar” to “very unfamiliar,” with corresponding values of 1.0, 0.8, 0.6, 0.4, and 0.2, respectively (40, 41).
3. The coefficient of variation (CV) is used to reflect the degree of consensus among experts’ ratings of each indicator. The smaller the CV value, the better the consensus among experts’ evaluations (37). The value is 0–1. The calculation formula of CV for each indicator item is SD/mean, and the mean value >4.0 or CV <0.25 is the consensus criteria for filtering items (37).
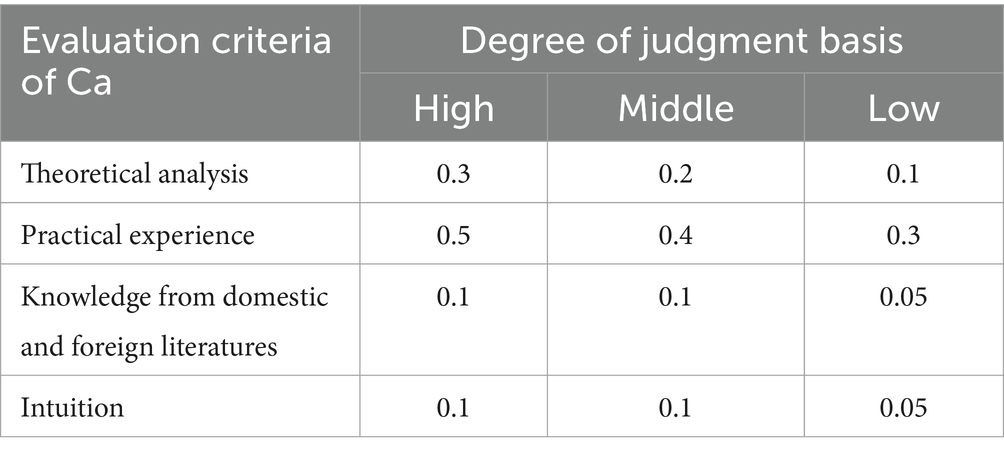
Table 1. Judgment basis with the topics for consultation from experts.
2.4 Ethical considerationThis study was reviewed by the institutional review board at Mahidol University in Thailand (IRB number: MUPH 2024–066) and Jiangsu College of Nursing in China (IRB number: JSCN-ME-2024071801). All participants voluntarily participated in this study.
3 Results 3.1 Expert informationThe study recruited 15 experts in each Delphi round including 13 women and 2 men. The age range was 35–52 (39.87 ± 5.514) years old. These experts came from tertiary hospitals (n = 8, 6 wound care specialists, and 2 geriatric care specialists), community healthcare centers (n = 4), and nursing educational institutions (n = 3). The working experience range was 9–30 (15.47 ± 7.53) years. Five experts held bachelor’s degrees, eight held master’s degrees, and two held doctoral degrees. Eleven experts had associate senior titles, and four had senior titles. All the experts were experienced in the PI field; of them, four worked in community nursing, three in nursing education, and eight in clinical nursing (6 as wound care specialists and 2 as geriatric care specialists).
3.2 Experts’ positive coefficientConsultation questionnaires were issued to 15 experts in each round, and the effective response rate was 100.00%. The positive coefficient was higher than 70%, indicating that the experts had a high level of enthusiasm in this study.
3.3 Experts’ authority coefficientIn this study, Expert judgment (Ca) = 0.98, expert familiarity (Cs) = 0.87, and Cr = 0.93, so the results are highly reliable.
3.4 Experts’ coordination coefficientKendall’s W represents the experts’ coordination coefficient. In the first round, the Kendall’s W was 0.372 (p < 0.001, χ2 = 429.489). In the second round was 0.177 (p < 0.001, χ2 = 207.472). The results showed that there is a high degree of agreement between the experts’ opinions.
3.5 Selection of indicators in the first roundThe mean, standard deviation, and coefficient of variation (CV) of each indicator’s expert ratings were calculated based on the results of the first Delphi round. In this round, the CV range for each indicator was 0.05–0.53, and the mean range was 2.00–4.93. Three indicators (A117, A123, A124) had CV > 0.25 and means <4.0, so these three indicators were deleted. Detailed statistical results of the indicators are shown in Table 2. In the first round, 6 experts proposed modifications to 14 indicators. Nine indicators were modified, three indicators were added and two indicators were merged. The specific modifications are shown in Table 3.
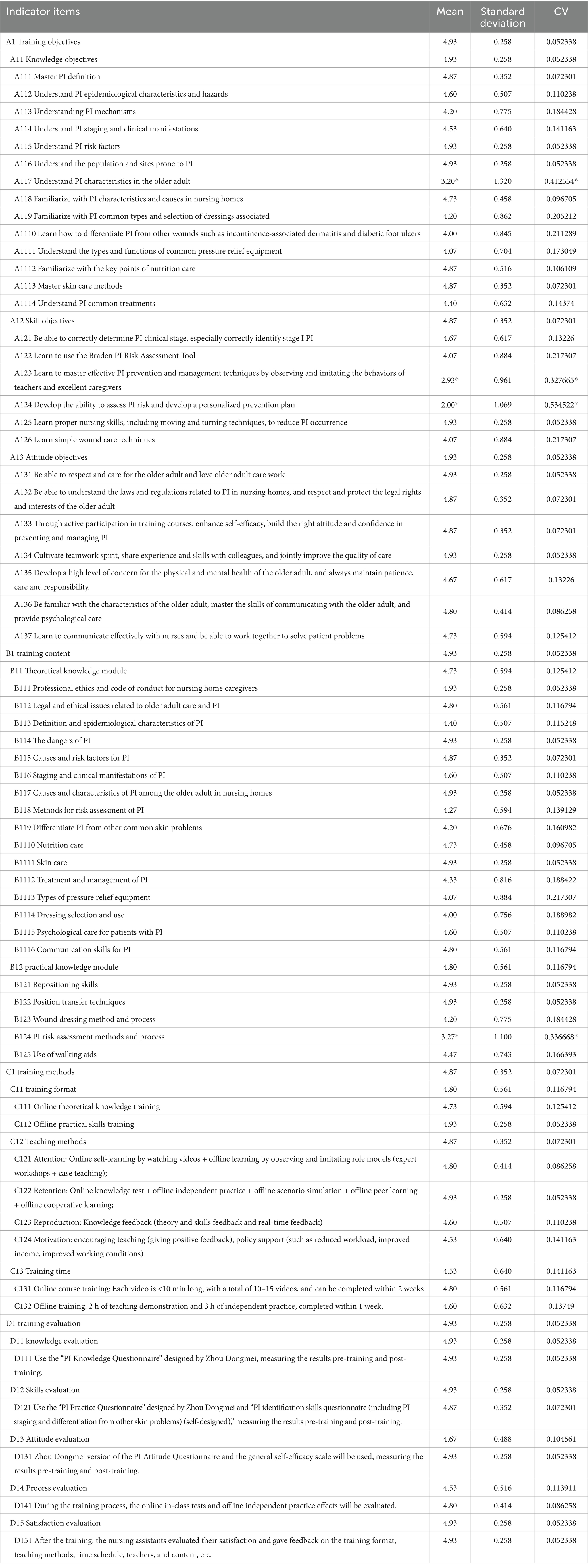
Table 2. Statistical results of expert consultation for the first round indicators.
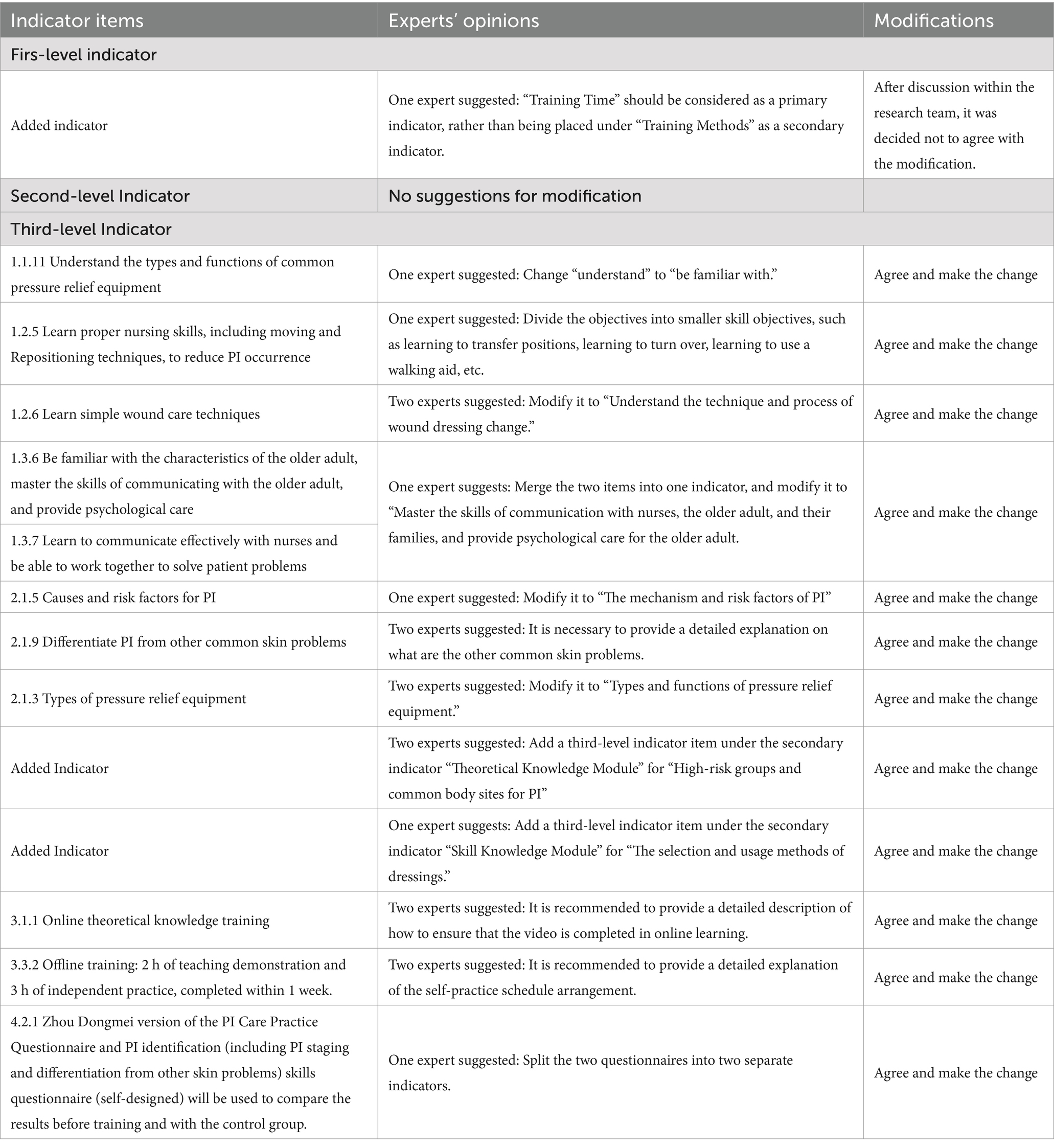
Table 3. Summary of modifications from expert consultation in the first round.
3.6 Selection of indicators in the second roundThe research team made revisions and formed a second round of expert consultation questionnaires based on the results of the first round. The experts’ opinions tended to be consistent after the second round. The appropriateness scores of each indicator reached the inclusion criteria, the CV range of each indicator was 0.05–0.20, and the mean for each indicator was >4. The detailed statistical results of the indicators are shown in Table 4. What is more, the experts did not add, delete, or modify any indicators, nor did they make any other specific suggestions. The SLTbT program of PI included 79 indicator items ultimately: 4 first-level indicators involving 4 domains (training objectives, training contents, training methods, training evaluation), 13 second-level indicators (three indicators for training objectives domain, two indicators for training contents domain, three indicators for training methods domain, five indicators for training evaluation domain), and 62 third-level indicators (25 indicators for training objectives domain, 22 indicators for training contents domain, eight indicators for training methods domain, seven indicators for training evaluation domain).
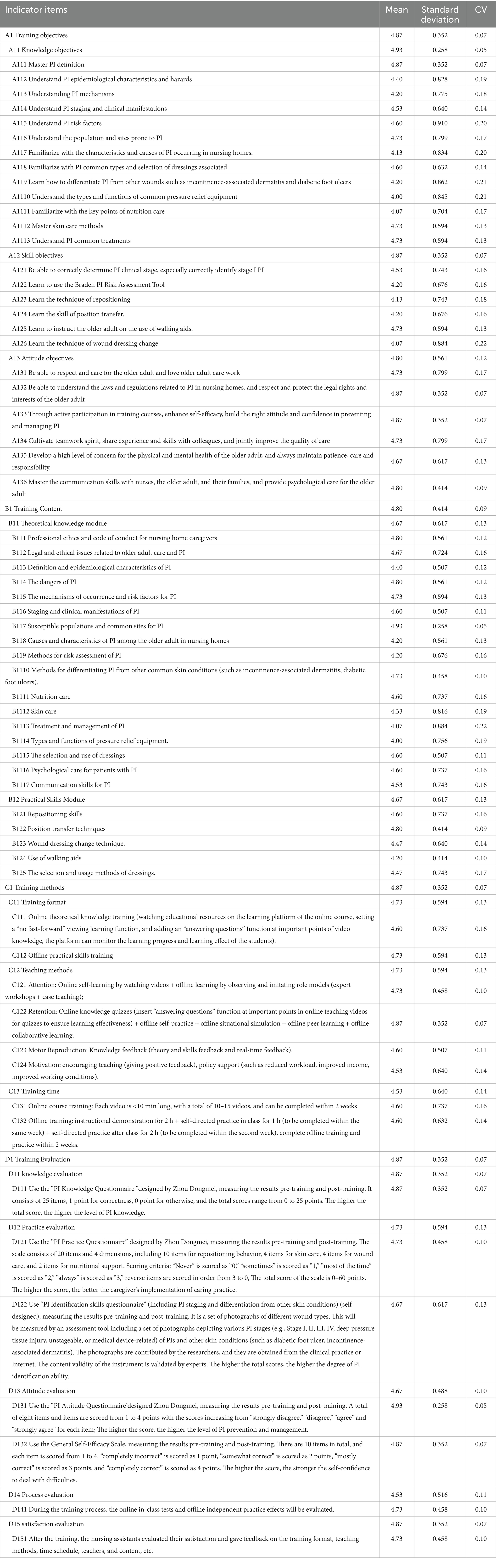
Table 4. Statistical results of expert consultation for the second round indicators.
We demonstrated how the SLT integrated into the PI training program intervention in Figure 2.
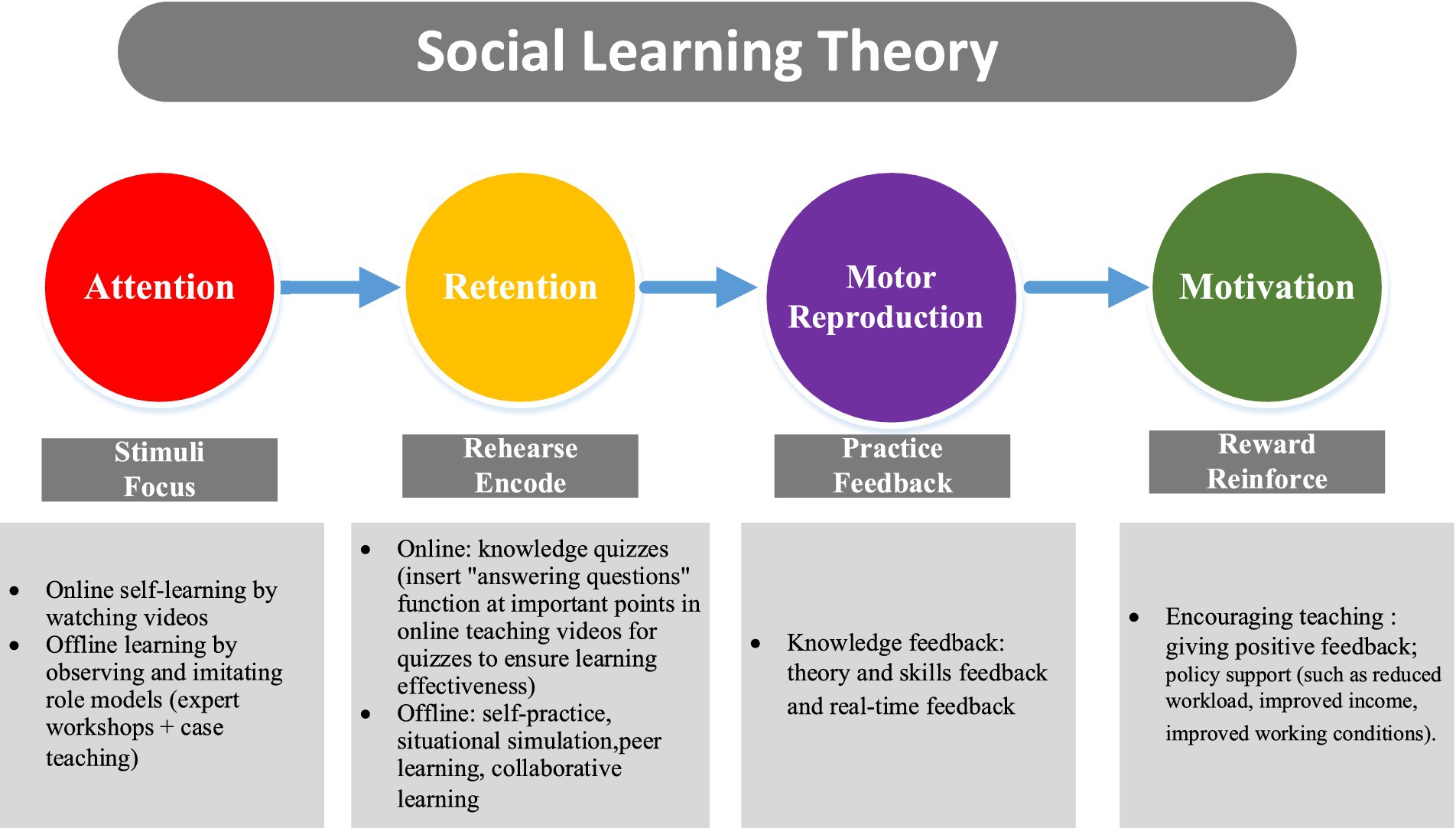
Figure 2. The process of SLT integrating into the PI training program intervention.
4 DiscussionThis study aimed to develop a comprehensive PI program for nursing assistants in Chinese nursing homes by leveraging SLT and refining the program through the modified Delphi method. The study highlights the significance of a methodical and theoretically based approach to training, which can significantly enhance the competencies of PIPM. The significance of PIPM in nursing homes is widely recognized by consumers and other stakeholders, assuming that the incidence and prevalence of PIs are indicators of poor nursing care quality (5). International multiple studies have shown that inappropriate care by caregivers contributes to the development and progression of PIs among patients. As the primary caregivers, nursing assistants normally face the following problems: low education level, lack of entry standard, non-professional, shortage, over workload, and low salaries, which can lead to problems including lack of basic nursing knowledge and skills, lack of regulation, unclear responsibilities, and heavy workloads, and impact nursing care service quality negatively (42–44). Therefore, the PI competency improvement training is very imperative and urgent. At present, the PI training for nursing assistants in nursing homes is not complete in China and even the global scope. The established SLTbT training program regarding PI provides a theoretical framework for global future study.
Expert opinions were gathered and a consensus was reached on the indicators of an effective SLTbT program through the modified Delphi method in this study. This method is particularly useful in situations where there is a need for structured communication among a group of experts to reach an agreement on complex issues (31, 45). The modified Delphi method was instrumental in achieving consensus among experts from various fields, including wound care, community nursing, geriatric nursing, and nursing education. The Kendall’s W of each round were 0.372 (p < 0.001, χ2 = 429.489), and 0.177 (p < 0.00 1, χ2 = 207.472) respectively. Based on the preset consensus criteria, all indicators reached a high degree of consensus (mean > 4.0; CV <0.25). The two-round Delphi process allowed for the systematic collection and refinement of expert opinions. The final PI training program for nursing assistants included 79 indicator items: 4 first-level indicators involving four domains (training objectives, training contents, training methods, training evaluation), 13 second-level indicators (three indicators for training objectives domain, two indicators for training contents domain, three indicators for training methods domain, five indicators for training evaluation domain), and 62 third-level indicators (25 indicators for training objectives domain, 22 indicators for training contents domain, eight indicators for training methods domain, seven indicators for training evaluation domain).
The developed PI training program for nursing assistants in Chinese nursing homes is underpinned by SLT, which posits that learning occurs through observation, imitation, and reinforcement of behaviors (29). SLT points out that combining the demonstration observation of real “role models” with individual autonomy and subjectivity can achieve individual self-learning and education (24). The integrated theory application was consistent with previous studies. Abdullah et al. (46) applied SLT to nursing trainees, effectively improving their professional abilities. This theoretical grounding is crucial as it provides a framework for understanding how nursing assistants can acquire the necessary knowledge and skills for PIPM through the training program. By incorporating SLT principles such as attention, retention, motor reproduction, and motivation, the training program ensures that nursing assistants not only acquire theoretical knowledge but also develop practical skills through observation and modeling. The proposed PIPM education model featured blended modules, interactive modules, simulation-based learning, peer-based learning, and case-based discussions. By observing and imitating the behavior of expert “role models” online and offline, the nursing assistants’ learning attention is aroused. In the form of peer learning and group cooperative learning, the nursing assistants can indirectly reflect on their learning behavior while observing the learning behavior of others, thus realizing alternative reinforcement of learning behavior (47). By using highly practical teaching methods such as case study discussions, scenario simulations, and repeated independent practice, learning behaviors are replicated, ensuring the effectiveness of the training. Combined with real-time feedback and absorption of knowledge and skills, this approach motivates learning and facilitates deep learning. Furthermore, this study innovates new strategies for nursing education by developing a training program to enhance nursing assistants’ competencies in PIPM based on SLT. This program is designed based on the actual training needs of nursing assistants in nursing homes and the need for policy support. It not only provides theoretical and skills-based support tailored to their training time or schedules, teaching methods, and evaluation methods but also addresses the challenges they face in terms of working conditions, workload, and income by offering policy support. This developed training program or education model may make a big difference in future nursing assistants’ training, education and cultivation in China, especially in the aspects of policy support such as improved working conditions, reduced workload, and improved income. These problems were also highlighted in previous studies in which nursing assistants complained they had poor working conditions, heavy workload, and low income (43, 44). In addition, this study may contribute to great implications for international clinical practice. The study advocates for policy incentives and emphasizes the synchronized development of nursing assistants’ knowledge, skills, and career development needs. In addition, it also strengthens nursing assistants’ vocational ethics and understanding of the vocational role, fostering the right professional values to cultivate high-competent nursing assistants. The content of the PI training program is different from previous studies globally. For example, Howe et al. (48) developed a PI educational program that focused on patient skin care through the following common training methods: PowerPoint slides, hands-on demonstrations, and group discussions (48). In demonstration skills, the nursing assistants practiced appropriate positioning, use of specialty beds, and off-loading pressure points (48). Cross et al. (49) designed a PI education program for residential care homes’ nursing assistants, and that just highlighted the basic knowledge and skills with the training method of a clinical nurse specialist’s 2 h lectures and did not give the competency evaluation finally. What is more, all previous studies constructed the program content based on outdated guidelines, and normally they did not measure the training effects toward competency improvement. Additionally, there is a scarcity of research that emphasizes training programs specifically addressing PI management or care, mostly focusing on PI prevention (50, 51). However, in the present study, the program content was designed based on the latest international guideline which involves basic concepts, risk factors, causes and mechanism, clinical stages, risk assessment methods, basic management and treatment methods, skin care, nutrition care, prevention skills, communication skills, psychological care, Legal and ethical issues, and so on.
In China, there is no national-level training program for nursing assistants in nursing homes (52). Nursing assistants’ careers start relatively late in China. While some LTC facilities implement occupational competency-strengthening programs, there is insufficient evidence to support the training effectiveness as it is not a standard, systemic approach and has little effect on PI knowledge and skills (43). Different nursing home has various training programs based on the Nursing Assistant Training Syllabus launched by the National Civil Bureau (53). The training syllabus includes daily care, basic care, rehabilitation services, psychological support, hospice care, care assessment, quality management and training guidance, and other related knowledge and skills (53). However, the training sessions on PI are very limited and sometimes account for only 1 h during the whole training program. Therefore, the current effects of PI training cannot be guaranteed. In addition, the limited PI training programs worldwide mainly target nurses, patients, family caregivers, or nursing assistants in hospitals, and the training curriculum quality, training content, training methods, and training evaluation varied greatly between these programs (43, 52, 54). Furthermore, these programs are often too broad and lack a specific focus on PIPM competencies, which are essential for providing high-quality care in nursing homes. There is a paucity of systemic and comprehensive PI-specific training programs focused on nursing assistants’ competencies in nursing homes worldwide. Therefore, this study has the potential to significantly enhance the care quality of residents in nursing homes by implementing the SLTbT program. It also has a broad and deep influence on international public health and clinical practice such as nursing assistant cultivation, policy-making, nursing management, public awareness improvement, aging population challenges, and so forth.
5 LimitationsIt has several limitations in this study. Firstly, the study employed a modified Delphi method to achieve an agreement among an expert panel. Though it is effective for collective opinions, the limited number of experts may fail to represent the different ideas of all stakeholders, which might affect the generalizability of the findings. Secondly, the Delphi method based on experts’ opinions could cause subjective interpretation which may influence response accuracy. Thirdly, the study did not pilot test the training intervention with real-world situations that could have offered valuable feedback on program’s feasibility and efficacy.
6 ConclusionThis study successfully developed a theoretically grounded PI training program for nursing assistants in Chinese nursing homes. By integrating SLT and utilizing the modified Delphi method, the program addresses the critical need for effective PI training and represents a significant contribution to the field of geriatric care. The comprehensive training indicators provide a solid foundation for improving PIPM practices, ultimately enhancing the wellbeing of older adult residents. The program’s effectiveness has yet to be empirically tested in a real-world setting. Future research should focus on the program’s implementation and its impact on nursing assistants’ performance and older adult residents’ health outcomes.
Data availability statementThe original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding authors.
Ethics statementThe studies involving humans were approved by the Mahidol University in Thailand, Jiangsu College of Nursing in China. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributionsYG: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing, Funding acquisition. SY: Conceptualization, Resources, Software, Writing – review & editing. PB: Conceptualization, Funding acquisition, Methodology, Project administration, Resources, Supervision, Validation, Writing – review & editing. AP: Conceptualization, Methodology, Supervision, Writing – review & editing. WZ: Methodology, Writing – review & editing. LX: Data curation, Resources, Writing – review & editing.
FundingThe author(s) declare that financial support was received for the research, authorship, and/or publication of this article. The research was funded by Mahidol University and Huaian Natural Science Research Plan Project (Joint Special Project) HABL202113, China and the 2024 Jiangsu Provincial Education Science Planning Project (C/2024/01/93), China.
Conflict of interestThe authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s noteAll claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References2. Jaul, E, Barron, J, Rosenzweig, JP, and Menczel, J. An overview of co-morbidities and the development of pressure ulcers among older adults. BMC Geriatr. (2018) 18:305. doi: 10.1186/s12877-018-0997-7
PubMed Abstract | Crossref Full Text | Google Scholar
3. White-Chu, E, Flock, P, and Struck, B. Pressure ulcers in long-term care. Clin Geriatr Med. (2011) 27:241–58. doi: 10.1016/j.cger.2011.02.001
Crossref Full Text | Google Scholar
4. National Bureau of Statistics of China. National Bureau of Statistics of China. China statistical yearbook 2021. Beijing: China Statistics Press (2021).
5. Dellefield, ME, and Magnabosco, JL. Pressure ulcer prevention in nursing homes: nurse descriptions of individual and organization level factors. Geriatr Nurs. (2014) 35:97–104. doi: 10.1016/j.gerinurse.2013.10.010
PubMed Abstract | Crossref Full Text | Google Scholar
7. Souza, D, and Gouveia, SV. Incidence of pressure ulcers in the institutionalized elderly. J Wound Ostomy Continence Nurs. (2010) 37:272–6. doi: 10.1097/WON.0b013e3181d8c25c
Crossref Full Text | Google Scholar
8. Kwong, EWY, Chen, LY, Kwan, RY-C, and Lee, PH. The effectiveness of a pressure injury prevention program for nursing assistants in private for-profit nursing homes: a cluster randomized controlled trial. J Adv Nurs. (2020) 76:1780–93. doi: 10.1111/jan.14391
PubMed Abstract | Crossref Full Text | Google Scholar
9. Shao, Y, Chen, Y, and Lu, X. Prevalence of pressure injuries in institutionalized residents. J Nurs Sci. (2019) 34:19–21. doi: 10.3870/i.issn.1001-4152.2019.18.019
Crossref Full Text | Google Scholar
10. Elli, C, Novella, A, Nobili, A, Ianes, A, and Pasina, L. Factors associated with a high-risk profile for developing pressure injuries in long-term residents of nursing homes. Med Princ Pract. (2022) 31:433–8. doi: 10.1159/000527063
PubMed Abstract | Crossref Full Text | Google Scholar
11. Rummel, E, Evans, EM, and O’Neal, PV. Educating certified nursing assistants to communicate skin changes to reduce pressure injuries. J Gerontol Nurs. (2021) 47:21–8. doi: 10.3928/00989134-20210624-04
PubMed Abstract | Crossref Full Text | Google Scholar
12. Lee, Y-N, Kwon, D-Y, and Chang, S-O. Bridging the knowledge gap for pressure injury Management in Nursing Homes. Int J Environ Res Public Health. (2022) 19:1400. doi: 10.3390/ijerph19031400
PubMed Abstract | Crossref Full Text | Google Scholar
13. Bangova, A. Prevention of pressure ulcers in nursing home residents. Nurs Stand. (2013) 27:54–61. doi: 10.7748/ns2013.02.27.24.54.e7243
Crossref Full Text | Google Scholar
14. Wogamon, C. Exploring the effect of educating certified nursing assistants on pressure ulcer knowledge and incidence in a nursing home setting. Ostomy Wound Manage. (2016) 62:42–50.
PubMed Abstract | Google Scholar
15. Lavallée, JF, Gray, TA, Dumville, J, and Cullum, N. Barriers and facilitators to preventing pressure ulcers in nursing home residents: a qualitative analysis informed by the theoretical domains framework. Int J Nurs Stud. (2018) 82:79–89. doi: 10.1016/j.ijnurstu.2017.12.015
PubMed Abstract | Crossref Full Text | Google Scholar
16. Van Herck, P, Sermeus, W, Jylha, V, Michiels, D, and Van den Heede, K. Using hospital administrative data to evaluate the knowledge-to-action gap in pressure ulcer preventive care. J Eval Clin Pract. (2009) 15:375–82. doi: 10.1111/j.1365-2753.2008.01019.x
PubMed Abstract | Crossref Full Text | Google Scholar
17. Wang, H, Wang, Y, and Sun, Y. Influence of targeted skill training in improving daily nursing skill of nursing workers in retirement organization. China Med. Pharm. (2017) 7:192–4. doi: 10.3969/j.issn.2095-0616.2017.16.059
Crossref Full Text | Google Scholar
19. Chong, CKW, and Lee, JSW. A home-based education programme in pressure injury prevention and management for caregivers of elderly patients: a pilot study. Asian J. Gerontol. Geriatr. (2017) 12:53–9.
21. Ousey, K, Kaye, V, McCormick, K, and Stephenson, J. Investigating staff knowledge of safeguarding and pressure ulcers in care homes. J Wound Care. (2016) 25:5–11. doi: 10.12968/jowc.2016.25.1.5
PubMed Abstract | Crossref Full Text | Google Scholar
22. Hultin, L, Olsson, E, Carli, C, and Gunningberg, L. Pressure mapping in elderly care: a tool to increase pressure injury knowledge and awareness among staff. J Wound Ostomy Continence Nurs. (2017) 44:142–7. doi: 10.1097/WON.0000000000000301
PubMed Abstract | Crossref Full Text | Google Scholar
23. Niederhauser, A, VanDeusen, LC, Parker, V, Ayello, EA, Zulkowski, K, and Berlowitz, D. Comprehensive programs for preventing pressure ulcers: a review of the literature. Adv Skin Wound Care. (2012) 25:167–88. doi: 10.1097/01.ASW.0000413598.97566.d7
PubMed Abstract | Crossref Full Text | Google Scholar
24. Blezer, S, Abujidi, N, and Sap, H. Urban living labs as innovation infrastructure for local urban intervention acceleration and student social learning: the impacts on community wellbeing in Heerlen. Front Public Health. (2023) 11:1242151. doi: 10.3389/fpubh.2023.1242151
PubMed Abstract | Crossref Full Text | Google Scholar
25. Shaughnessy, AF, and Erlich, DR. The science of education: using learning theory to solve teaching problems in medical education. Educ Prim Care. (2022) 33:194–8. doi: 10.1080/14739879.2022.2053344
Crossref Full Text | Google Scholar
27. Bahn, D. Social learning theory: its application in the context of nurse education. Nurse Educ Today. (2001) 21:110–7. doi: 10.1054/nedt.2000.0522
Crossref Full Text | Google Scholar
28. Hill, JR, Song, L, and West, RE. Social learning theory and web-based learning environments: a review of research and discussion of implications. Am J Dist Educ. (2009) 23:88–103. doi: 10.1080/08923640902857713
Crossref Full Text | Google Scholar
29. Bandura, A. Social learning theory. Oxford, England: Prentice-Hall (1977). 247 p.
31. Keeney, S, Hasson, F, and McKenna, H. The Delphi technique in nursing and health research 2011. Oxford: Wiley Blackwell (2011).
32. Avella, J. Delphi panels: research design, procedures, advantages, and challenges. Int J Dr Stud. (2016) 11:305–21. doi: 10.28945/3561
留言 (0)