Stigma and discrimination are human rights and global public health problems which constitute serious impediments to optimal HIV treatment outcomes (1–10). Stigma is a damaging social phenomenon which demeans and devalues individuals or a group of people portraying them as undesirable due to attributes or characteristics that are societally adjudged unacceptable (1, 2, 7, 10–18). HIV-related stigma is often expressed as irrational behaviors, negative attitudes, and unfavorable judgments toward people living with or at risk of HIV which remains very common in low and middle income countries including Nigeria. This can negatively affect the health and wellbeing of people living with HIV (PLWH) by acting as an impediment to optimization of HIV prevention, treatment and support services (19–21). This most often become internalized and leads to undesirable affective, cognitive, and mental health outcomes (2). Internalized HIV-related stigma is the conditional acceptance of negative societal perceptions, characterizations, and labeling of PLWH which can be expressed with self-depreciating feelings such as shame, self-blame, low self-esteem, and self-worth (2, 3). Men who have sex with men (MSM) are disproportionately affected by HIV infection which continues to expand worldwide in both developed and developing countries (7, 21). This group is often stigmatized due to their peculiarities, positions, gender identity and sexual orientation which drives discrimination across sectors of society, including in health care, education, workplace as well as within families and in communities (3, 13, 18). Young men who have sex with men (YMSM) living with HIV face a life-long illness associated with numerous health and social challenges that evolve with time thereby impacting on different areas of their lives. They have to cope with the shock, fear, anger, guilt and shame of having HIV infection as well as the attendant stigmatizing responses associated with their sexual identity which impact on their mental health (22). Studies of HIV-related stigma among YLWHA is of relevance since youth are highly vulnerable to stigma and their numbers are on the rise in society. Youth's vulnerability to HIV-related stigma is exacerbated by social and economic marginalization, as well as the rapid physical and psychosocial transitions (8, 12, 15, 19). However, there is still relatively little empirical evidence on HIV-stigma among people living with HIV particularly for the YMSM in HIV care (20). It was against this backdrop that this study was conducted to assess the level of HIV related stigma and its associated factors among YMSM in HIV care in Plateau State, North central Nigeria as a way of generating geo-specific information and evidence for advocacy and policy change.
Methodology Study areaThis study was conducted in Jos, Plateau state, North central Nigeria, which has a population of about 3.2 million people (23). There is a viable MSM networks in the state with functional internal systems and coordination structures including HIV support groups. Additionally, The Society for Family Health (SFH) currently operates One Stop Shop (OSS) for HIV services attending to the HIV care needs of the Key Affected Population in the state (KAP) while the APIN (AIDS Prevention Initiatives in Nigeria) Public Health Initiative is the lead implementing partner supporting PEPFAR funded HIV prevention and care programs in the state.
Study populationThe study population comprised of all YMSM in HIV care in the state affiliated to the HIV support group or within the MSM network in the state who were between 18–24 years of age.
Study designThis was a cross-sectional study to assess the level of HIV-related stigma and its associated factors among YMSM in HIV care conducted between July 2023 and April 2024 using quantitative method of data collection.
Sample size estimationThe sample size for this study was determined using the sample size estimation formula for a cross-sectional study (24). Where n was the minimum sample size, Z is the standard normal deviate at 95% confidence interval (1.96), q is the complementary probability (1 – p), d is the precision of the study set at 0.05 and p is the prevalence of severe HIV-related stigma among PLHIV from a previous study (6.7%) (6). This gave a minimum sample size of 96.
Criteria for inclusion in the studyAll YMSM in HIV care affiliated to the HIV support group or within the MSM network in the state who were 18–24 years were eligible to participate in the study while those who declined to consent for participation in the study were excluded.
Sampling techniqueRespondent Driven Sampling (RDS) technique was used in this study to recruit consenting eligible YMSM members of MSM community into the study (18, 23, 25). The Respondent-driven sampling (RDS) is a modified form of snowball sampling which offers several advantages for hard to reach groups. A total of 122 YMSM aged 18–24 years currently in HIV care were identified and recruited for the study following informed consent for participation in the study. The facility appointment diary and the HIV case management registers were used to identify the eligible participants in the one- stop shop (OSS) clinic for the key population while the testing peer navigators, some respected YMSM and the key population MSM coordinator facilitated the recruitment of the YMSM accessing HIV care for the state. The recruitment process ended following a 4-week period of saturation when no eligible participants was found.
Data collectionAn interviewer's administration approach to data collection was employed using the Berger's HIV-stigma scale for assessment of HIV related stigma and an adapted tool for demographics as well as social and sexual behaviors of the participants (26, 27). Berger's HIV stigma scale (BHSS) was used for the assessment of perceived HIV stigma among the YMSM in HIV care. Eight trained research assistants who were members of the MSM network carried out the data collection after the completion of the recruitment of the participants into the study. The questionnaires were pretested among MSM in a neighboring state. Prior to the administration of the questionnaire, written informed consent was obtained and documented from all the respondents with the assurance of confidentiality and anonymity of their responses provided.
Grading of responseThe HIV stigma scale consisted of 40 items in four different subscales using a 4-point rating scale of strongly disagree = 1, disagree = 2, agree = 3 and strongly agree = 4 giving a maximum attainable overall score of 160 and minimum attainable score of 40. This scale was further subdivided into four subscales namely; Personalized Stigma subscale (PS) having a total of 18 items with a maximum attainable score of 72 using a 4-point rating scale of strongly disagree = 1, disagree = 2, agree = 3 and strongly agree = 4. The Disclosure Concerns (DC) having 10 items with a maximum attainable score of 40 using a 4-point rating scale of strongly disagree = 1, disagree = 2, agree = 3 and strongly agree = 4. Negative Self-Image (NSI) subscale with a total of 13 items and a maximum attainable score of 52 using a 4 point rating scale also and the Public Attitudes (PA) subscale having 20 items with a maximum attainable score of 80. Furthermore, all 40-items on the scale were cumulatively computed to give the Total HIV Stigma Score (TSS). The scores emanating from the elicited responses are scaled in the positive direction indicating that the higher the scores, the higher the level of HIV-related stigma (6, 8, 10, 28). The Total HIV related stigma score was further categorized into low-level stigma, middle-level stigma and High-level stigma using the percentile graph. Scores between 25th percentile and 50th percentile (40–80) was adjudged to be low-level stigma while scores between 50th percentile and 75th percentile (81–120) as middle-level stigma and those >75th percentile (121–160) categorized as high-level stigma (6, 10, 28).
The explanatory variables in this study were classified as demographic characteristics and sexual behaviors of the respondents. The socio-demographic characteristics included age as at last birthday, religion, highest level of education, sexual orientation categorized as bisexual and homosexual, family type assessed as monogamous and polygamous, family history of same sex orientation assessed as present if the respondents had seen or known any family member engaging in sex with another man, engagement in a paid job assessed as engaged and not engaged, disclosure of HIV status as yes or no, duration on HIV treatment in years and disclosure of sexual orientation as yes or no. The sexual behaviors assessment included type of MSM categorized as penetrative, receptive or both, engagement in anal sex within the last 7days as yes or no, use of condoms in the last anal sex assessed as yes or no. Furthermore, number of male sexual partners within the last 3 months was categorized as 1, 2–5, and 6 or more, self-reported lifetime history of STIs as positive or negative and self-reported engagement in transactional sexual practice within the last 6 months prior to the study which wase assessed as engaged or not engaged. Transactional sex was defined as non-marital, non-commercial sexual relationships motivated by an implicit assumption that sex will be exchanged for material support or other benefits e.g. money (29). The primary outcome variable was total HIV-related stigma score while the secondary outcome variables were the HIV-related stigma subscales scores.
Data analysisAll filled questionnaires were reviewed for completeness and thereafter serialized. Data analysis was carried out using SPSSS statistical software version 23. Descriptive statistical analysis was carried out on quantitative variables such age of the respondent, age at same sex sexual debut, total HIV-related stigma scores and the scores of stigma subscales. These quantitative variables were expressed with mean and standard deviation as their summary indices after fulfilling the assumptions of normality while duration on HIV treatment was found to be skewed and median and interquartile range were employed as its summary indices. Other explanatory variables such as age group, marital status, sexual orientation, family history of same sex orientation, and grading of the HIV stigma etc were presented in frequency table expressed in frequencies and percentages. Correlation between the Total HIV-related stigma scores and the scores of the subscales was established using Pearson's correlation. The correlation coefficient (r) for PS subscale was 0.91, DC subscale was 0.75, NSI subscale 0.90 and PA subscale 0.98. The variation in mean total HIV-related stigma score was tested using unpaired students T-test for explanatory variables expressed in two categories while one way analysis of variance was used for those expressed in three or more categories. Mean difference and 95% confidence interval were used as point and interval estimates of the difference in mean scores in the student T-test with a probability value of < 0.05 was considered statistically significant.
ResultsThe mean age of the study participants was 22.2 ± 2.0 years with 56 (45.6%) being 22 years and below. Fifty-two (42.6%) of the respondents identified as bisexual and 66 (54.1%) debuted sex with a male partner below 16 years of age. Fifty-one (41.8%) of the study participants had completed tertiary education while 73 (59.3%) of them had disclosed their HIV status to at least one person in the past (Table 1).
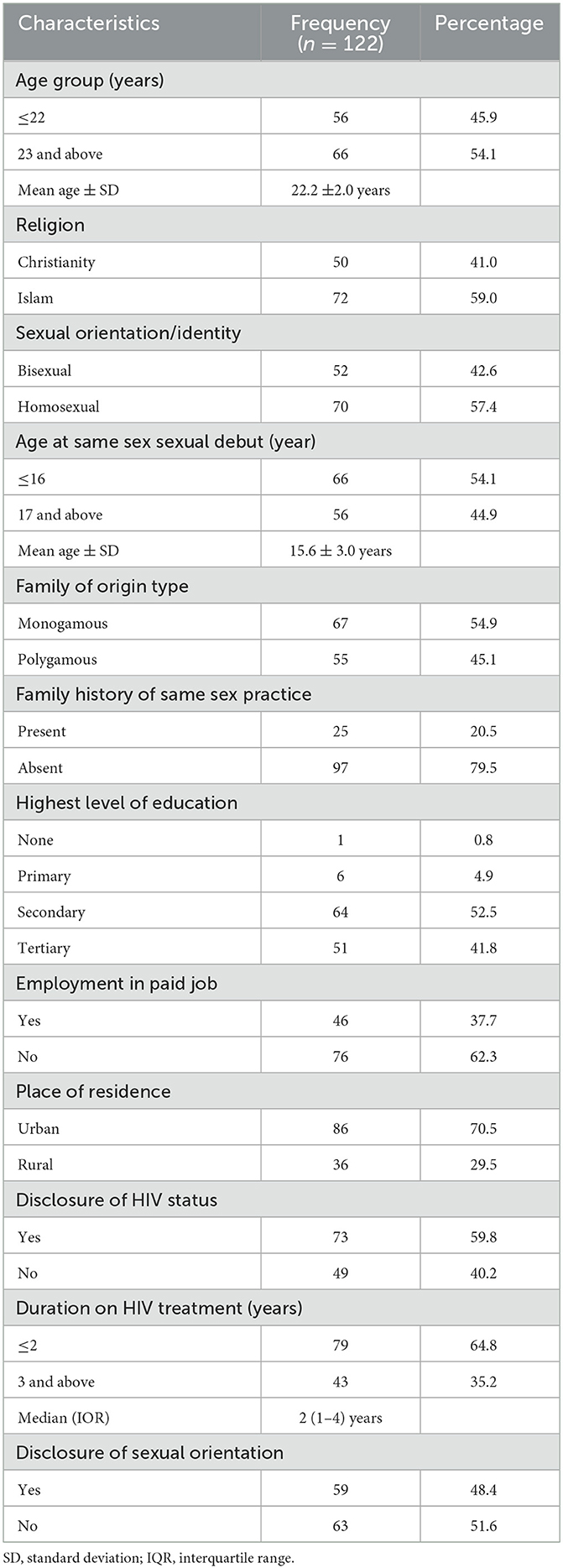
Table 1. Sociodemographic characteristics of the participants.
With regards to the sexual behaviors of the participants, 31 (25.4%) were penetrative MSM, 18 (14.8%) receptive and 73 (59.8%) both receptive and penetrative in their anal sex sexual preferences. Engagement in transactional sex was self-reported by 41 (33.6%) with 71 (58.2%) reported engagement in anal sex within the last 7 days of the assessment and 33 (46.5%) of those who had engaged in anal sex did not use condoms (Table 2).
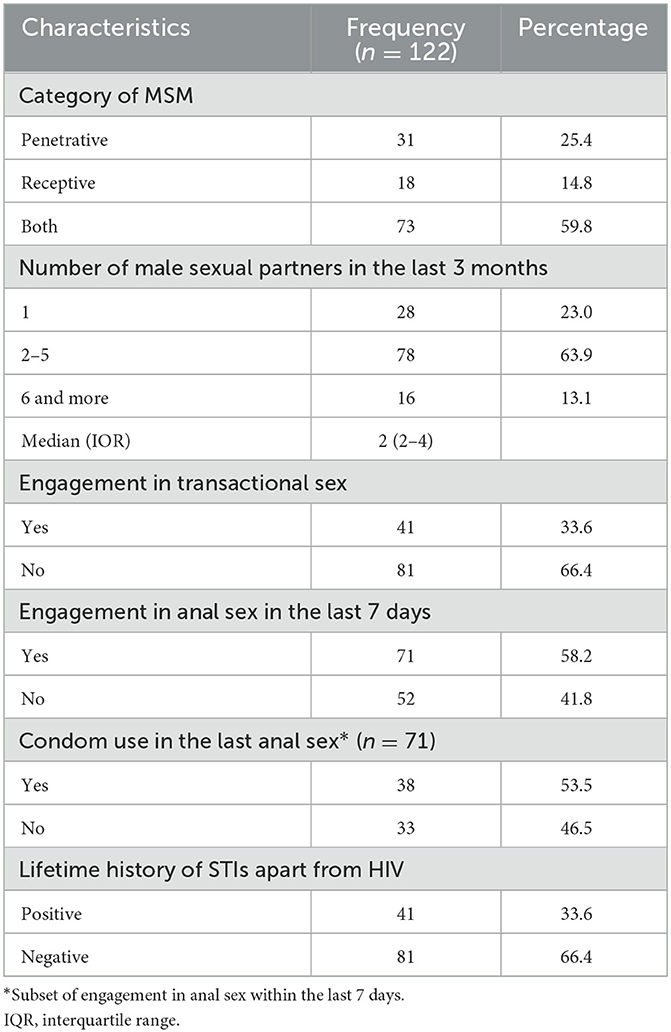
Table 2. Sexual behaviors of the participants.
In the assessment of the HIV related stigma, the total HIV-related stigma score for the participants was 121.9 ± 18.8 with 40 (32.8%) being classified as high-level stigma and 75 (61.5%) with middle-level stigma. The mean personalized stigma subscale score of 48.3 ± 11.7 was reported among the participants while average score for stigma associated with disclosure subscale was found to be 30.9 ± 4.2. Mean scores for negative self-image and public attitude stigma subscales were 35.8 ± 6.6 and 57.2 ± 10.4 respectively (Table 3).
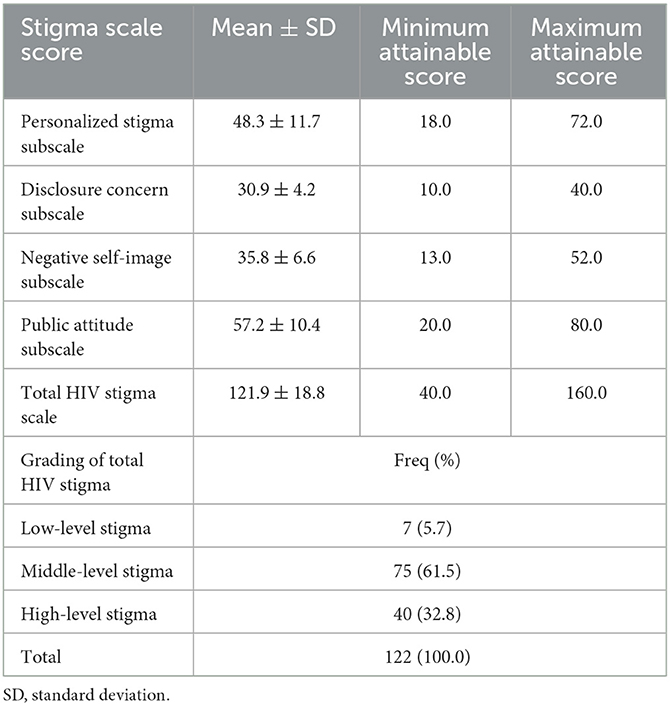
Table 3. HIV related stigma assessment scores of the participants.
The variation in the mean overall HIV-related stigma scores across the demographic characteristics and the sexual behaviors of the respondents is shown in Table 4. In this study, age, sexual orientation, age at same sex debut, level of education, employment status, disclosure of sexual orientation and engagement in transactional sex among others did not show any statistically significant variation in the mean total HIV-related sigma scores. However, significant variation in mean total HIV-related stigma score was found with duration on HIV treatment as those who had been on treatment for 3 years and more having a mean score of 117.8 ± 15.2 compared to 110.3 ± 20.1 among those who had been on treatment for 2 years of less (mean difference: −7.50; 95% Confidence interval: −14.45, −5.51; p = 0.035; Table 4). Furthermore, no statistically significant variation was found in the assessment of the mean scores of the personalized stigma and public attitudes subscales across the demographic characteristics and sexual behaviors of the respondents. However, duration on HIV treatment showed statistically significant difference on the disclosure concern subscale with those who had been on treatment for 3 years and more having a mean score of 32.4 ± 3.5 compared to 30.2 ± 4.3 of those who had been on treatment for 2 years of less (mean difference: −2.22; 95% Confidence interval: −3.74, −0.70; p = 0.004). Similarly, respondents who had been on treatment for 3 years and more had a higher mean score of 37.5 ± 4.9 compared to 34.9 ± 7.2 for those who had been on treatment for 2 years of less (mean difference: −2.64; 95% Confidence interval: −5.08, −0.19; p = 0.035) on the negative self-image subscale (Tables 5–8).
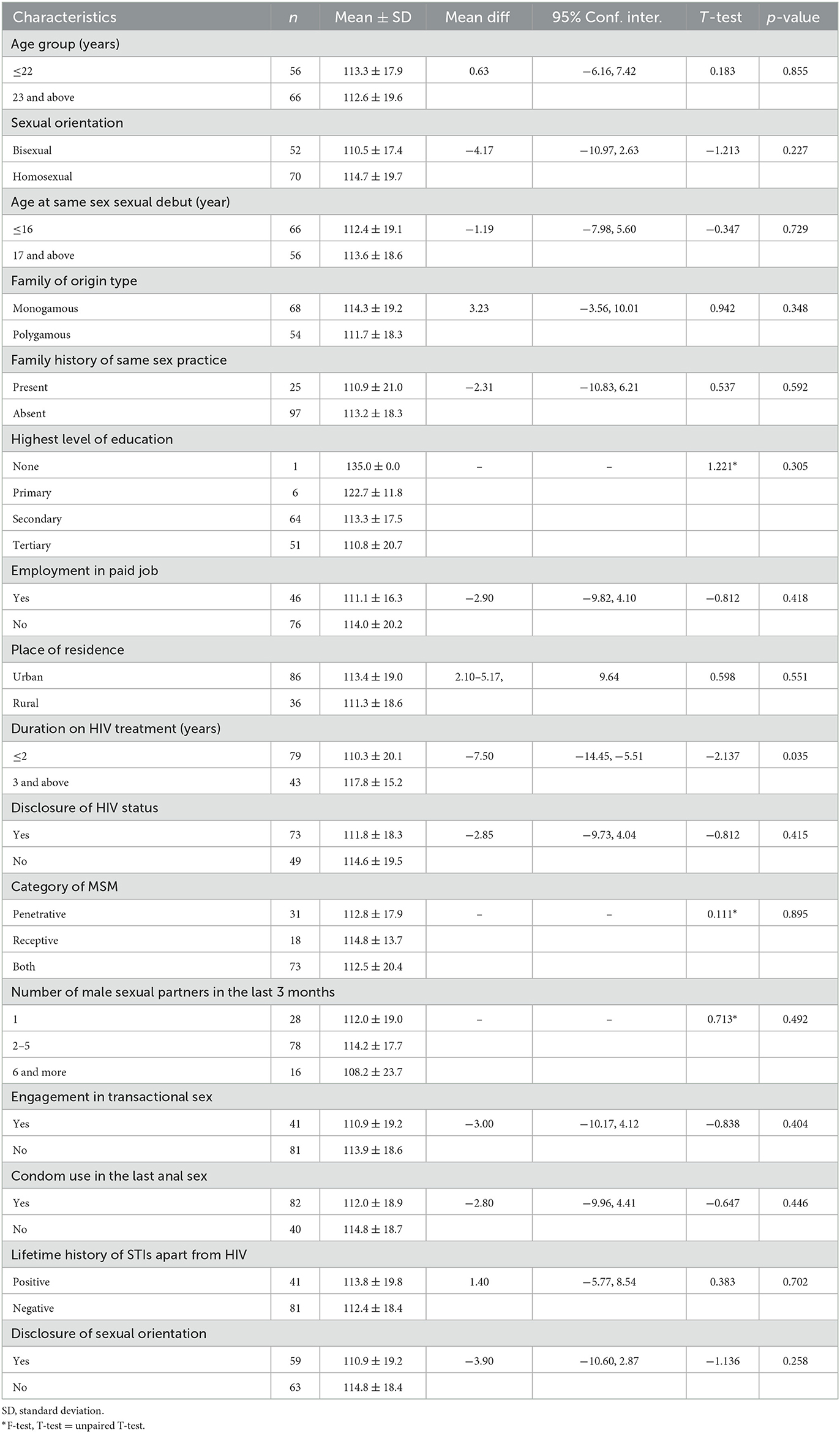
Table 4. Variation in mean Total HIV stigma score by characteristics of the participants.
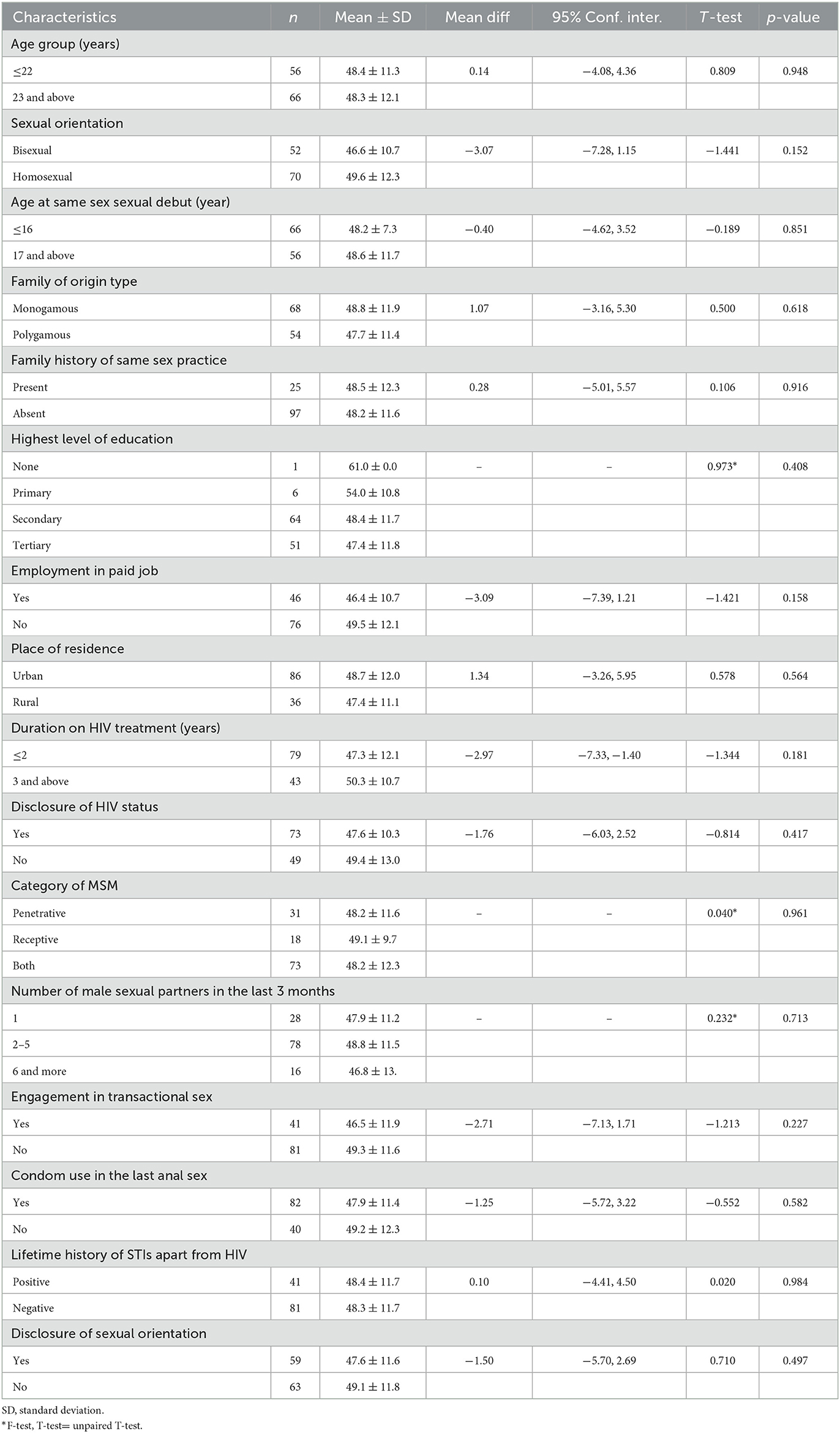
Table 5. Variation in mean personalized stigma subscale score by characteristics of the participants.
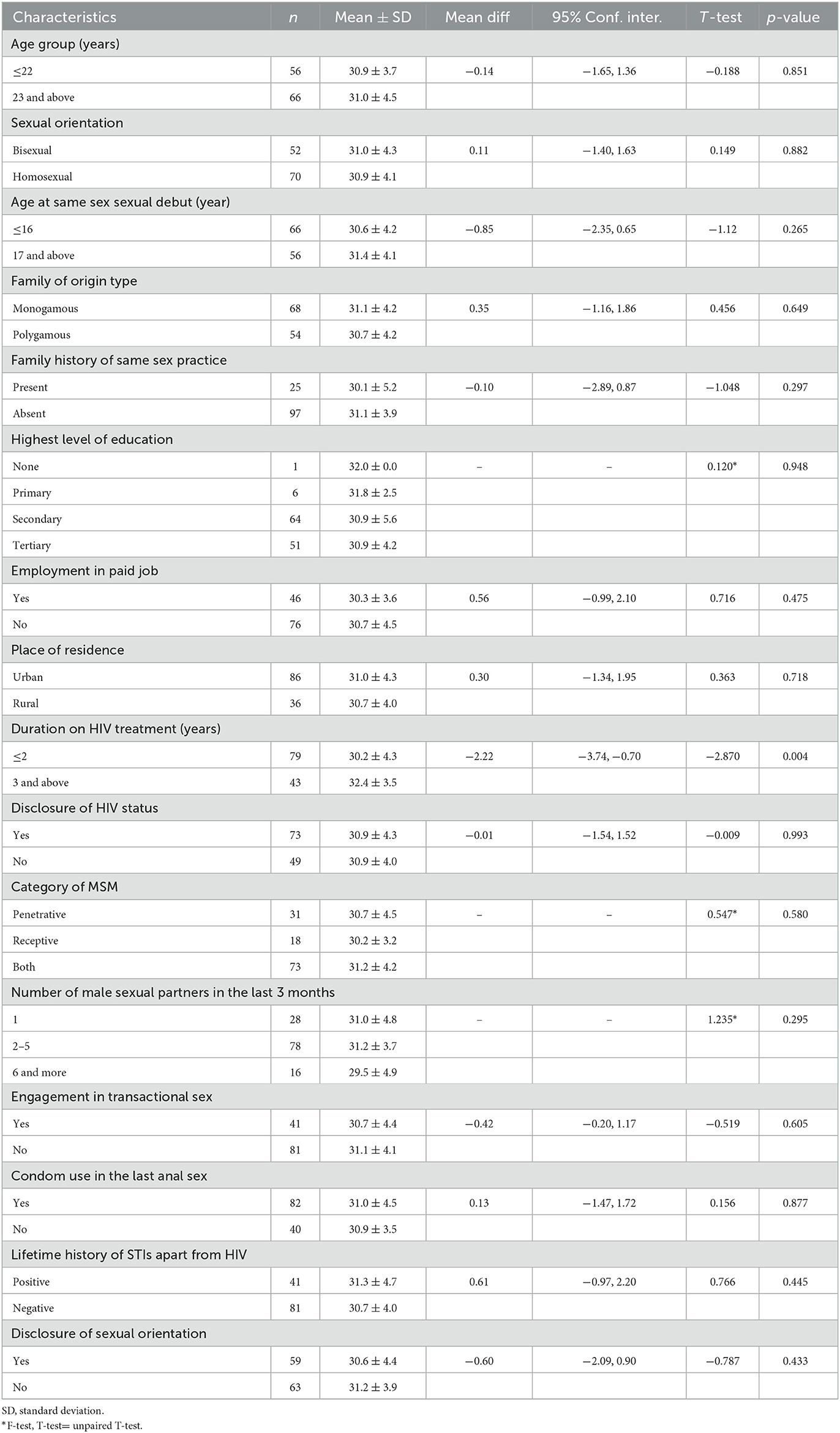
Table 6. Variation in mean disclosure concern subscale score by characteristics of the participants.
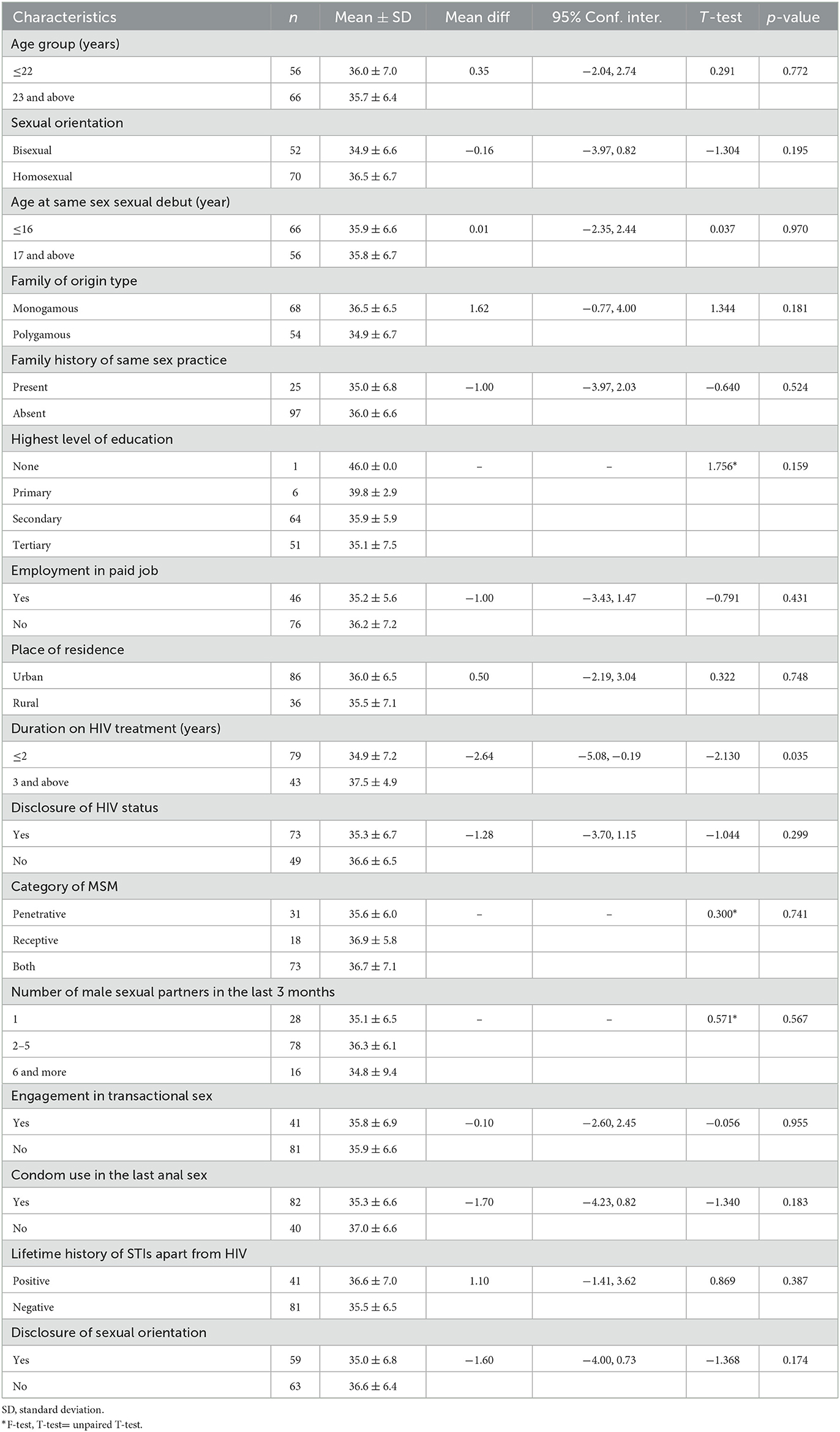
Table 7. Variation in mean negative self-image subscale score by characteristics of the participants.
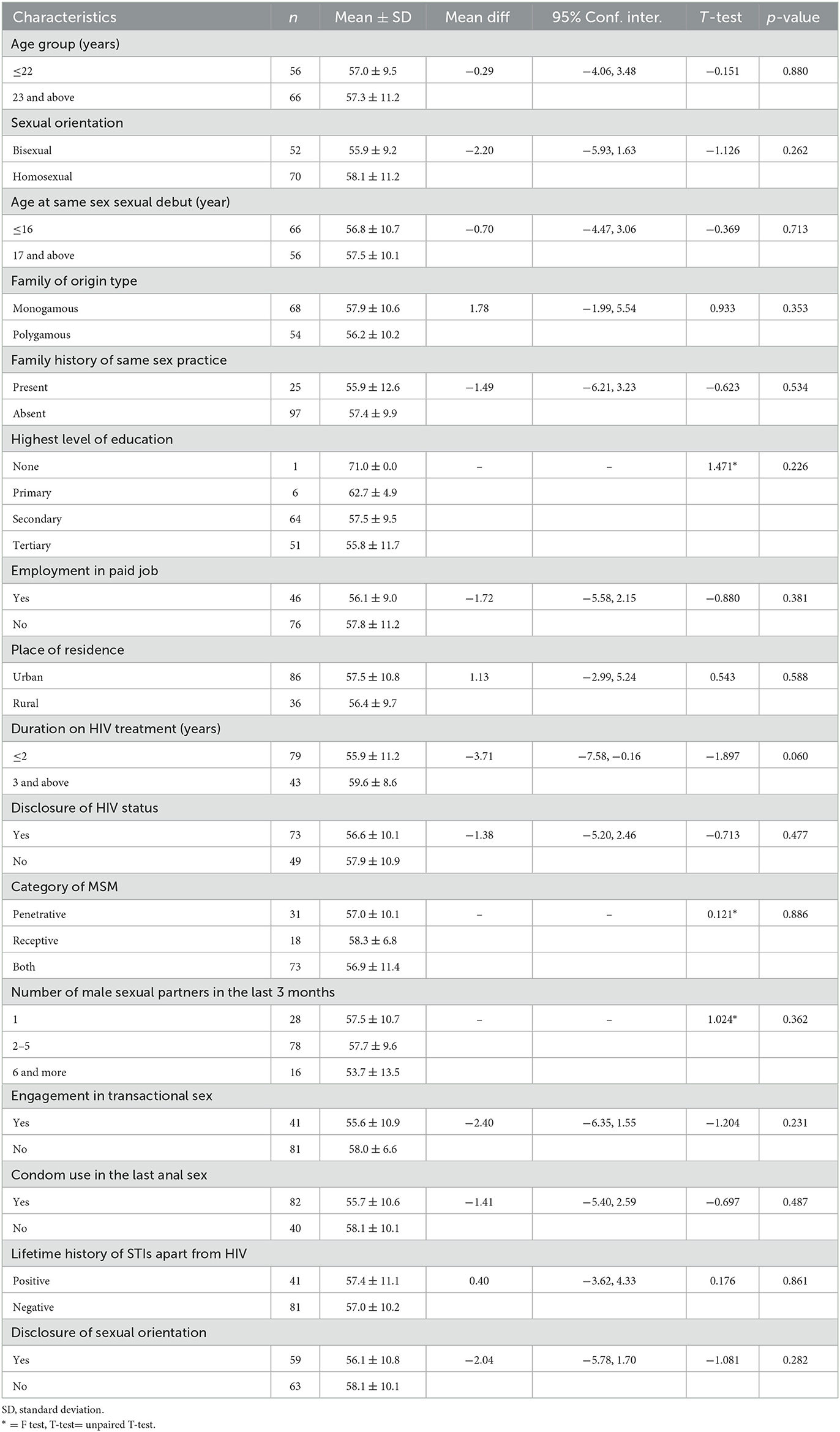
Table 8. Variation in mean Public attitude subscale score by characteristics of the participants.
DiscussionHIV-related stigma poses to be an imminent clog in the cascade of HIV treatment and continuum of care thereby potentiating poor adherence, disclosure refusal, self-blame, depression, isolation and treatment failure (6, 30–32). In this study, high level of HIV-related stigma was reported among the YMSM in HIV care as demonstrated by high total HIV stigma scores and also across all the subscales of personalized stigma, disclosure, negative self-image and public attitude. The high total HIV-related stigma scores found in this study are consistent with findings of other studies conducted in India, China and United States of America (7, 18, 20, 33, 34). However, other studies conducted in United States of America reported slightly lower levels of HIV-related stigma in comparison to this study (1, 19). The similarities observed with the findings of this study and others cited ones could be attributable to the use of similar stigma assessment tools, study design and MSM in HIV care as the study participants. However, adults in HIV care who were not members of the MSM community were assessed for HIV related stigma in some of the other referenced studies. It is important to state that the MSM population and particularly YMSM are a vulnerable group perceived to be exhibiting behaviors and sexual identities that contradict social norms, cultures and traditions in most climes (18). This in itself has been the foremost driver of HIV-related stigma among the MSM population and significant contributor to the relegation of this group to the closet. The combination stigmatization and repressive legislations pose serious challenges to HIV care and if not addressed, it will continue to negatively impact the desired HIV/AIDS treatment outcomes and possibly contribute to reversing the gains already achieved in the HIV treatment landscape.
Total HIV-related stigma score was found to increase with duration in HIV care in this study, however, other studies reported abandonment by spouse, isolation by family, exclusion from social activities, bisexual identity, bartering sex, injection drug use, disclosure and depression as factors driving HIV-related stigma (6, 18, 20). It is therefore imperative that development or deployment of innovative and context specify strategies for stigma reduction in HIV care is essential but more importantly such strategies should target the peculiarities of the YMSM in HIV care. The cross-sectional design of this study will not support the establishment of temporal relationship particularly between duration in HIV care and the total HIV-related stigma score which was found to be statistically significant. Additionally, the tool used for the assessment of HIV related stigma focused on perceived stigma making it important that further studies be conducted to examine the lived experience of stigma in this population and its potential environmental drivers as nexus for generating empirical evidence in providing the needed psychological, psychosocial and social support necessary to mitigate the impact of stigma on the YMSM living with HIV.
ConclusionThis study found a high level of HIV- related stigma among the Young Men who Have Sex with Men in HIV care which is significantly influenced by the duration of time in HIV care. The study also found high levels of sub-scales of stigma such as Personalized Stigma, Disclosure Concerns, Negative Self-Image and Public Attitudes.
Data availability statementThe raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statementThis study involving humans was approved by Jos University Teaching Hospital Human Research Ethics Committee. This study was conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributionsTA: Conceptualization, Formal analysis, Methodology, Writing – original draft, Writing – review & editing. BC: Formal analysis, Writing – original draft, Writing – review & editing. AZ: Conceptualization, Supervision, Writing – original draft, Writing – review & editing. PK: Conceptualization, Supervision, Writing – original draft, Writing – review & editing.
FundingThe author(s) declare financial support was received for the research, authorship, and/or publication of this article. Research reported in this publication was supported by the Fogarty International Center and National Institute of Mental Health, of the National Institutes of Health under Award Number D43 TW010543. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Conflict of interestThe authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's noteAll claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References1. Kalichman SC, Katner H, Banas E, Hill M, Kalichman MO. Cumulative effects of stigma experiences on retention in HIV care among men and women in the rural Southeastern United States. AIDS Patient Care STDS. (2020) 34:484–90. doi: 10.1089/apc.2020.0144
PubMed Abstract | Crossref Full Text | Google Scholar
2. Budhwani H, Robles G, Starks TJ, MacDonell KK, Dinaj V, Naar S. Healthy choices intervention is associated with reductions in stigma among youth living with HIV in the United States (ATN 129). AIDS Behav. (2021) 25:1094–102. doi: 10.1007/s10461-020-03071-1
PubMed Abstract | Crossref Full Text | Google Scholar
3. Greenwood GL, Wilson A, Bansal GP, Barnhart C, Barr E, Berzon R, et al. HIV-related stigma research as a priority at the National Institutes of Health. AIDS Behav. (2022) 26:5–26. doi: 10.1007/s10461-021-03260-6
PubMed Abstract | Crossref Full Text | Google Scholar
4. Babel RA, Wang P, Alessi EJ, Raymond HF, Wei C. Stigma, HIV risk, and access to HIV prevention and treatment services among men who have sex with men (MSM) in the United States: a scoping review. AIDS Behav. (2021) 25:3574–604. doi: 10.1007/s10461-021-03262-4
PubMed Abstract | Crossref Full Text | Google Scholar
5. Bharat S. A systematic review of HIV/AIDS-related stigma and discrimination in India: current understanding and future needs. SAHARA J. (2011) 8:138–49. doi: 10.1080/17290376.2011.9724996
PubMed Abstract | Crossref Full Text | Google Scholar
6. Oke OO, Akinboro AO, Olanrewaju FO, Oke OA, Omololu AS. Assessment of HIV-related stigma and determinants among people living with HIV/AIDS in Abeokuta, Nigeria: a cross-sectional study. SAGE Open Med. (2019) 7:2050312119869109. doi: 10.1177/2050312119869109
PubMed Abstract | Crossref Full Text | Google Scholar
8. Smit PJ, Brady M, Carter M, Fernandes R, Lamore L, Meulbroek M, et al. HIV-related stigma within communities of gay men: a literature review. AIDS Care. (2012) 24:405–12. doi: 10.1080/09540121.2011.613910
PubMed Abstract | Crossref Full Text | Google Scholar
9. Baugher AR, Beer L, Fagan JL, Mattson CL, Freedman M, Skarbinski J, et al. Prevalence of internalized HIV-related stigma among HIV-infected adults in care, United States, 2011-2013. AIDS Behav. (2017) 21:2600–08. doi: 10.1007/s10461-017-1712-y
PubMed Abstract | Crossref Full Text | Google Scholar
10. Nworuh OB, Ogbalu AI. Experience of HIV-related stigma by people living with HIV/AIDS (PLWHA), based on gender: a case of PLWHA attending clinic in the Federal Medical Center, Owerri, Imo states, Nigeria. J Public Health Epidemiol. (2013) 5:435–39. doi: 10.5897/JPHE2013.0496
PubMed Abstract | Crossref Full Text | Google Scholar
11. Turan B, Budhwani H, Fazeli PL, Browning WR, Raper JL, Mugavero MJ, et al. How does stigma affect people living with HIV? The mediating roles of internalized and anticipated HIV stigma in the effects of perceived community stigma on health and psychosocial outcomes. AIDS Behav. (2017) 21:283–91. doi: 10.1007/s10461-016-1451-5
PubMed Abstract | Crossref Full Text | Google Scholar
12. Kimera E, Vindevogel S, Reynaert D, Justice KM, Rubaihayo J, De Maeyer J, et al. Experiences and effects of HIV-related stigma among youth living with HIV/AIDS in Western Uganda: a photovoice study. PLoS ONE. (2020) 15:e0232359. doi: 10.1371/journal.pone.0232359
PubMed Abstract | Crossref Full Text | Google Scholar
13. Schuster MA, Collins R, Cunningham WE, Morton SC, Zierler S, Wong M, et al. Perceived discrimination in clinical care in a nationally representative sample of HIV-infected adults receiving health care. J Gen Intern Med. (2005) 20:807–13. doi: 10.1111/j.1525-1497.2005.05049.x
PubMed Abstract | Crossref Full Text | Google Scholar
14. Kinsler JJ, Wong MD, Sayles JN, Davis C, Cunningham WE. The effect of perceived stigma from a health care provider on access to care among a low-income HIV-positive population. AIDS Patient Care STDS. (2007) 21:584–92. doi: 10.1089/apc.2006.0202
PubMed Abstract | Crossref Full Text | Google Scholar
15. Rueda S, Mitra S, Chen S, Gogolishvili D, Globerman J, Chambers L, et al. Examining the associations between HIV-related stigma and health outcomes in people living with HIV/AIDS: a series of meta-analyses. BMJ Open. (2016) 6:e011453. doi: 10.1136/bmjopen-2016-011453
PubMed Abstract | Crossref Full Text | Google Scholar
16. Anderson AM, Ross MW, Nyoni JE, McCurdy SA. High prevalence of stigma-related abuse among a sample of men who have sex with men in Tanzania: implications for HIV prevention. AIDS Care. (2015) 27:63–70. doi: 10.1080/09540121.2014.951597
PubMed Abstract | Crossref Full Text | Google Scholar
17. Knight R, Small W, Shoveller JA. HIV stigma and the experiences of young men with voluntary and routine HIV testing. Sociol Health Illn. (2016) 38:153–67. doi: 10.1111/1467-9566.12345
PubMed Abstract | Crossref Full Text | Google Scholar
18. Li Z, Hsieh E, Morano JP, Sheng Y. Exploring HIV-related stigma among HIV-infected men who have sex with men in Beijing, China: a correlation study. AIDS Care. (2016) 28:1394–401. doi: 10.1080/09540121.2016.1179713
PubMed Abstract | Crossref Full Text | Google Scholar
19. Harper GW, Lemos D, Hosek SG. Stigma reduction in adolescents and young adults newly diagnosed with HIV: findings from the Project ACCEPT intervention. AIDS Patient Care STDS. (2014) 28:543–54. doi: 10.1089/apc.2013.0331
PubMed Abstract | Crossref Full Text | Google Scholar
20. Swendeman D, Rotheram-Borus MJ, Comulada S, Weiss R, Ramos ME. Predictors of HIV-related stigma among young people living with HIV. Health Psychol. (2006) 25:501–9. doi: 10.1037/0278-6133.25.4.501
PubMed Abstract | Crossref Full Text | Google Scholar
21. Azucar D, Rusow JA, Slay L, Taiwo M, Rodriguez A, Johnson A, et al. Combining the HYM (Healthy Young Men's) cohort study and the TRUTH (A Trans Youth of Color Study): protocol for an expanded mixed methods study renewal. JMIR Res Protoc. (2022) 11:e39232. doi: 10.2196/39232
PubMed Abstract | Crossref Full Text | Google Scholar
22. Bhana A, Abas MA, Kelly J, van Pinxteren M, Mudekunye LA, Pantelic M. Mental health interventions for adolescents living with HIV or affected by HIV in low- and middle-income countries: systematic review. BJPsych Open. (2020) 6:e104. doi: 10.1192/bjo.2020.67
PubMed Abstract | Crossref Full Text | Google Scholar
23. Afolaranmi TO, Hassan ZI, Ugwu OJ, Ofakunrin AOD, Bello KK, Chingle MP, et al. Retention in HIV care and its predictors among HIV-infected men who have sex with men in Plateau state, North Central Nigeria. J Family Med Prim Care. (2021) 10:1596–601. doi: 10.4103/jfmpc.jfmpc_1748_20
PubMed Abstract | Crossref Full Text | Google Scholar
24. Ibrahim T. Sample size determination. In: Research Methodology and Dissertation Writing for Health and Allied Health Professionals, 1st Edn. Abuja: Cress Global Link Limited (2009), p. 75.
25. Bamgboye EA, Badru T, Bamgboye A. Transactional sex between men and its implications on HIV and sexually transmitted infections in Nigeria. J Sex Transm Dis. (2017) 2017:1810346. doi: 10.1155/2017/1810346
PubMed Abstract | Crossref Full Text | Google Scholar
26. Berger BE, Ferrans CE, Lashley FR. Measuring stigma in people with HIV: psychometric assessment of the HIV stigma scale. Res Nurs Health. (2001) 24:518–29. doi: 10.1002/nur.10011
PubMed Abstract | Crossref Full Text | Google Scholar
27. Nugroho A, Erasmus V, Coulter RWS, Koirala S, Nampaisan O, Pamungkas W, et al. Driving factors of retention in care among HIV-positive MSM and transwomen in Indonesia: a cross-sectional study. PLoS ONE. (2018) 13:e0191255. doi: 10.1371/journal.pone.0191255
PubMed Abstract | Crossref Full Text | Google Scholar
28. Li Z, Sheng Y. Investigation of perceived stigma among people living with human immunodeficiency virus/acquired immune deficiency syndrome in Henan Province, China. Int J Nurs Sci. (2014) 1:385–8. doi: 10.1016/j.ijnss.2014.10.019
PubMed Abstract | Crossref Full Text | Google Scholar
29. Oldenburg CE, Perez-Brumer AG, Biello KB, Landers SJ, Rosenberger JG, Novak DS, et al. Transactional sex among men who have sex with men in Latin America: economic, sociodemographic, and psychosocial factors. Am J Public Health. (2015) 105:e95–102. doi: 10.2105/AJPH.2014.302402
PubMed Abstract | Crossref Full Text | Google Scholar
30. Sengupta S, Banks B, Jonas D, Miles MS, Smith GC. HIV interventions to reduce HIV/AIDS stigma: a systematic review. AIDS Behav. (2011) 15:1075–87. doi: 10.1007/s10461-010-9847-0
PubMed Abstract | Crossref Full Text | Google Scholar
31. Stangl AL, Lloyd JK, Brady LM, Holland CE, Baral S. A systematic review of interventions to reduce HIV-related stigma and discrimination from 2002 to 2013: how far have we come? J Int AIDS Soc. (2013) 16(3 Suppl 2):18734. doi: 10.7448/IAS.16.3.18734
PubMed Abstract | Crossref Full Text | Google Scholar
32. Fife BL, Wright ER. The dimensionality of stigma: a comparison of its impact on the self of persons with HIV/AIDS and cancer. J Health Soc Behav. (2000) 41:50–67. doi: 10.2307/2676360
PubMed Abstract | Crossref Full Text | Google Scholar
33. Charles B, Jeyaseelan L, Pandian AK, Sam AE, Thenmozhi M, Jayaseelan V. Association between stigma, depression and quality of life of people living with HIV/AIDS (PLHA) in South India – a community based cross sectional study. BMC Public Health. (2012) 12:463. doi: 10.1186/1471-2458-12-463
留言 (0)