Intertrochanteric fractures of the femur are associated with high mortality rates and a significant incidence of postoperative complications. In older adults, these fractures are often referred to as “the last fracture of life” due to their severe impact on health and mobility. Globally, the number of hip fractures in individuals aged more than 50 years is projected to reach 4.5 million by 2025 (1). In China alone, with the rapid pace of economic and social development and an aging population, approximately 500,000 hip fractures occur annually (2). These fractures impose substantial individual medical costs and socioeconomic burdens. The relationship between preoperative waiting time and improved surgical outcomes, reduced postoperative complications, but a better prognosis remains controversial (3, 4). However, evidence suggests that reducing the preoperative waiting period leads to better patient outcomes (5). Reduced preoperative waiting time has been shown to be beneficial in reducing the incidence of postoperative complications in elderly hip fracture patients and in facilitating postoperative functional recovery (6, 7). Previous studies have demonstrated that comorbidities are responsible for prolonged preoperative waiting times (8). Despite this, no predictive models exist to anticipate the extension of preoperative waiting time in cases of intertrochanteric femur fractures. A model that predicts prolonged waiting times based on information collected at admission is crucial to help clinicians make informed decisions and develop more effective treatment strategies. Nomogram models have proven useful for predicting diagnoses and prognoses in various diseases. To our knowledge, no nomogram model has been developed to predict prolonged preoperative waiting times in patients with intertrochanteric femur fractures. Therefore, this study aimed create an accurate and reliable nomogram model to assist clinicians in predicting delays in surgical treatment and optimizing patient care.
Methods PatientsIn this study, we collected basic information, clinical data, and laboratory findings at the time of admission from 1,129 patients with intertrochanteric fractures who were hospitalized in the Department of Orthopedics at the Affiliated Hospital of Shandong University of Traditional Chinese Medicine. All cases were collected by searching the database within our hospital. These patients underwent surgical treatment from January 2017 to January 2024. The study was approved by the Ethics Committee of the Affiliated Hospital of Shandong University of Traditional Chinese Medicine. The inclusion criteria for the study were as follows: (1) age ≥ 18 years; (2) confirmed diagnosis of unilateral intertrochanteric femur fracture based on X-ray or CT examination; (3) hospitalization and subsequent surgical treatment with internal fixation; (4) length of stay <2 weeks. The exclusion criteria were as follows: (1) bilateral intertrochanteric femoral fractures; (2) multiple fractures; (3) pathologic fractures (4) undergoing two or more surgeries; (5) incomplete data. Exclusion criteria were developed based on our previous studies (9). And we excluded cases of selection bias from interfering with the outcome. A total of 13 patients were excluded based on these criteria, leaving 1,116 patients for inclusion in the study. Out of all enrolled patients, 70% were randomly allocated to the training set and the remaining 30% were assigned to the validation set. The data was split performed using stratification. The training set was utilized to develop the nomogram model, whereas the validation set was used to assess the model’s performance.
Data collectionTwo clinical orthopedic surgeons reviewed all cases independently in accordance with the inclusion criteria and collected the relevant demographic variables, clinical data, and laboratory findings at the time of admission. When the two physicians disagreed on the inclusion criteria, a third senior orthopedic surgeon intervened to determine and ultimately resolve the data inconsistencies.
(1) Demographic variables: age, sex, injured side
(2) Clinical data: pre-operative preparation time, comorbidity (none, one, two, and three or more), AO/OTA Fracture, and Dislocation Classification.
(3) Laboratory examination results: kalium (K), calcium (Ca), natrium (Na), balbumin (ALB), alkaline phosphatase (ALP), hemoglobin (HGB), total bilirubin (TBIL), creatinine (CREA), triglyceride (TG), high density lipoprotein cholesterol (HDLC), cystatin C (CYSC), white blood cell (WBC), platelet (PLT), and hypersensitive C-reactive protein (hsCRP). All results were obtained from the same laboratory of the Department of Laboratory Medicine of the Affiliated Hospital of Shandong University of Traditional Chinese Medicine. An identical test methodology was employed so as to achieve a consistent outcome.
We defined the waiting time for surgery of <48 h as early surgery and the waiting time for surgery of >48 h as delayed surgery (10).
Statistical analysisWe utilized R software (version 4.4.0, IBM Corporation, Armonk, New York, United States) and SPSS (version 26, R Foundation for Statistical Computing, Vienna, Austria) for data analysis and statistical processing. Patient data were randomly divided into training and validation sets using the “caret” package in R. Descriptive statistics were generated through SPSS. Variables with a p-value of less than 0.05 in univariate analysis were included in the multivariate logistic regression. In the multivariate logistic regression analysis variables with a p-value of less than 0.05 were identified as independent predictors. These independent risk factors were then used to develop the nomogram model.
Results Patient characteristicsA total of 1,116 patients with intertrochanteric fractures met the inclusion criteria to be included. The average age was 77.77 ± 11.19 years, with 762 (68%) being female and 354 (32%) male giving a male-to-female ratio of 1:2.15. Of the patients, 573 had left-sided fractures and 543 had right-sided fractures. The average waiting time for surgery was 5.46 ± 3.83 days. In the training set of 782 patients, 133 (17%) underwent early surgery, with 86 (65%) being female and 47 (35%) males. The remaining 649 patients (83%) underwent delayed surgery, comprising 458 (71%) females and 191 (29%) males. The validation set included 334 patients, of whom 56 (16%) received early surgery and 278 (84%) underwent delayed surgery. A summary of the characteristics of the variables in both the training and validation sets is provided in Table 1.
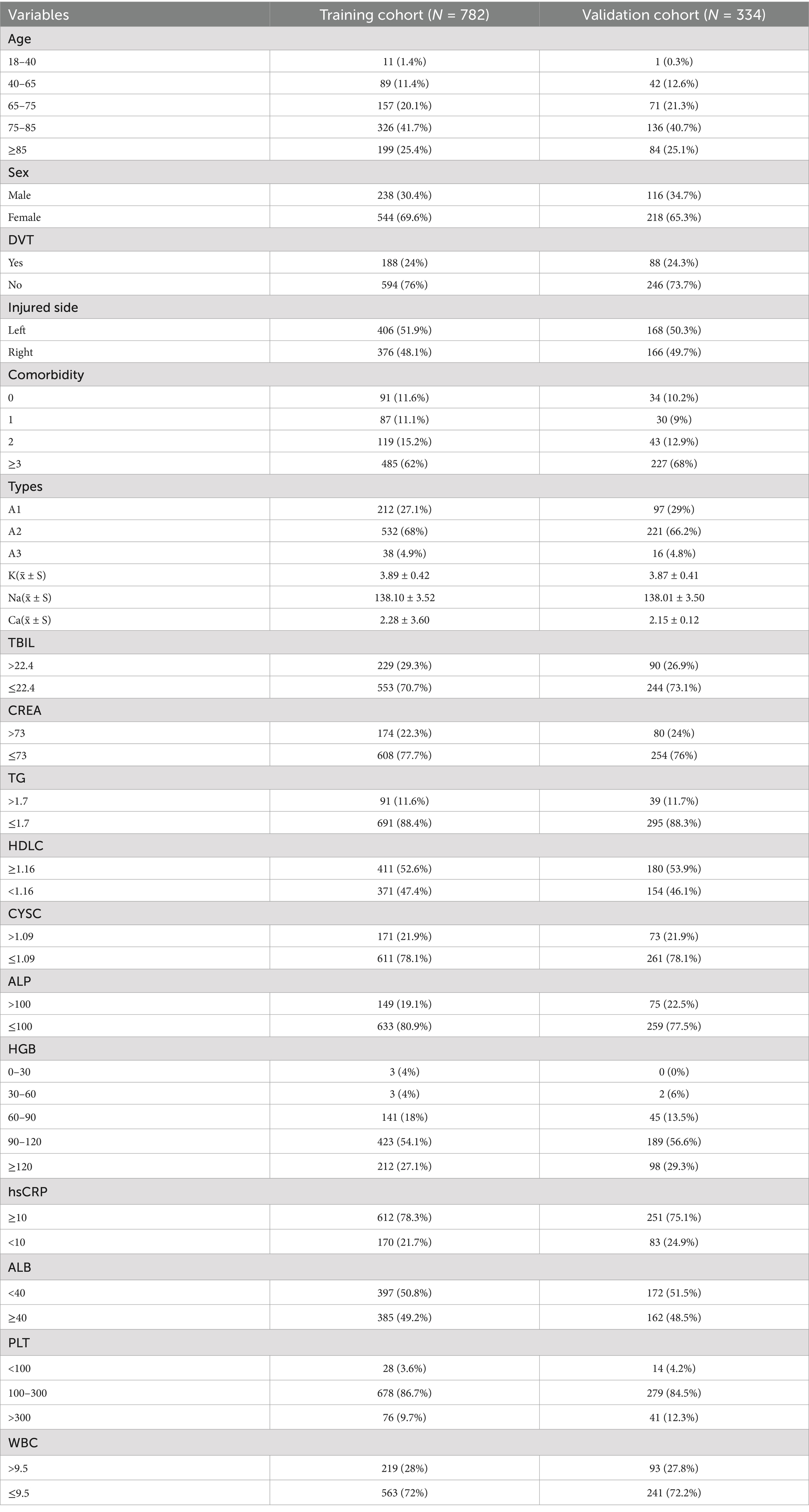
Table 1. Demographics of variables in the training and validation sets.
Screening of predictors and nomogram developmentWe identified 20 factors associated with prolonged preoperative waiting time in patients with intertrochanteric fractures undergoing surgery, based on previous studies conducted by our research group (9), along with relevant literature and guidelines. These 20 variables from the training set were included in a univariate logistic regression analysis. Seven variables with p-value of less than 0.05 in the univariate logistic regression analysis were included in the multivariate logistic regression analysis. Using the step wise backward validation of multifactorial logistic regression analysis, a total of 5 factors with p < 0.05 were identified as independent risk factors when the Akaike Information Criterion was at its minimum (Table 2). The five selected variables age, deep vein thrombosis (DVT), comorbidity, high-density lipoprotein cholesterol (HDLC), and high-sensitivity C-reactive protein (hsCRP) were used to construct the predictive model. The expected outcome of the model is a patient preoperative wait time greater than 48 h. The high risk is that patients delay undergoing surgery. The low risk is that patients timely undergoing surgery. The model was then visualized as a nomogram using the “rms” package in R software (Figure 1).
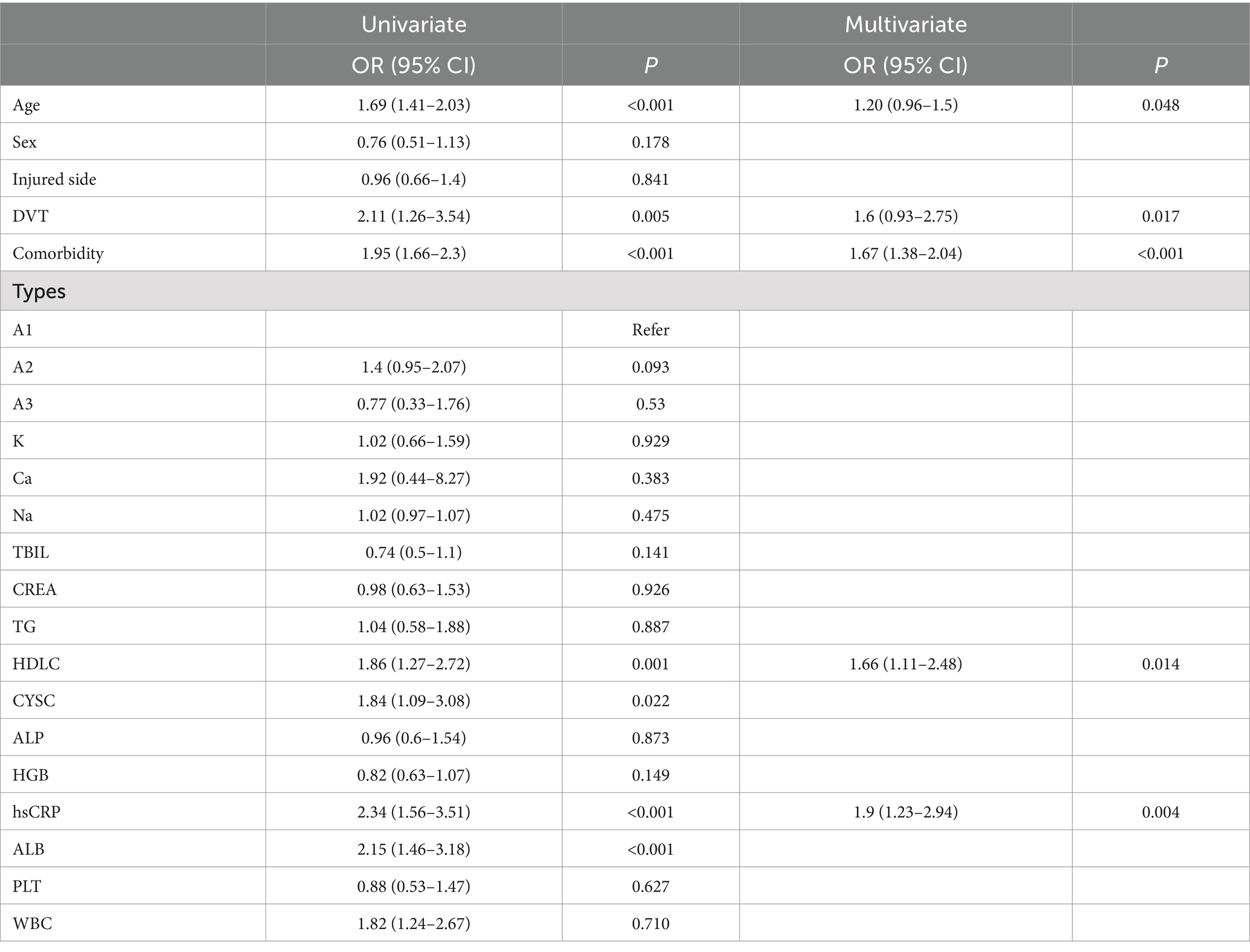
Table 2. Univariate and multivariate logistic regression analysis of risk factors for prolonged preoperative waiting time of intertrochanteric fracture patients undergoing operative treatment.
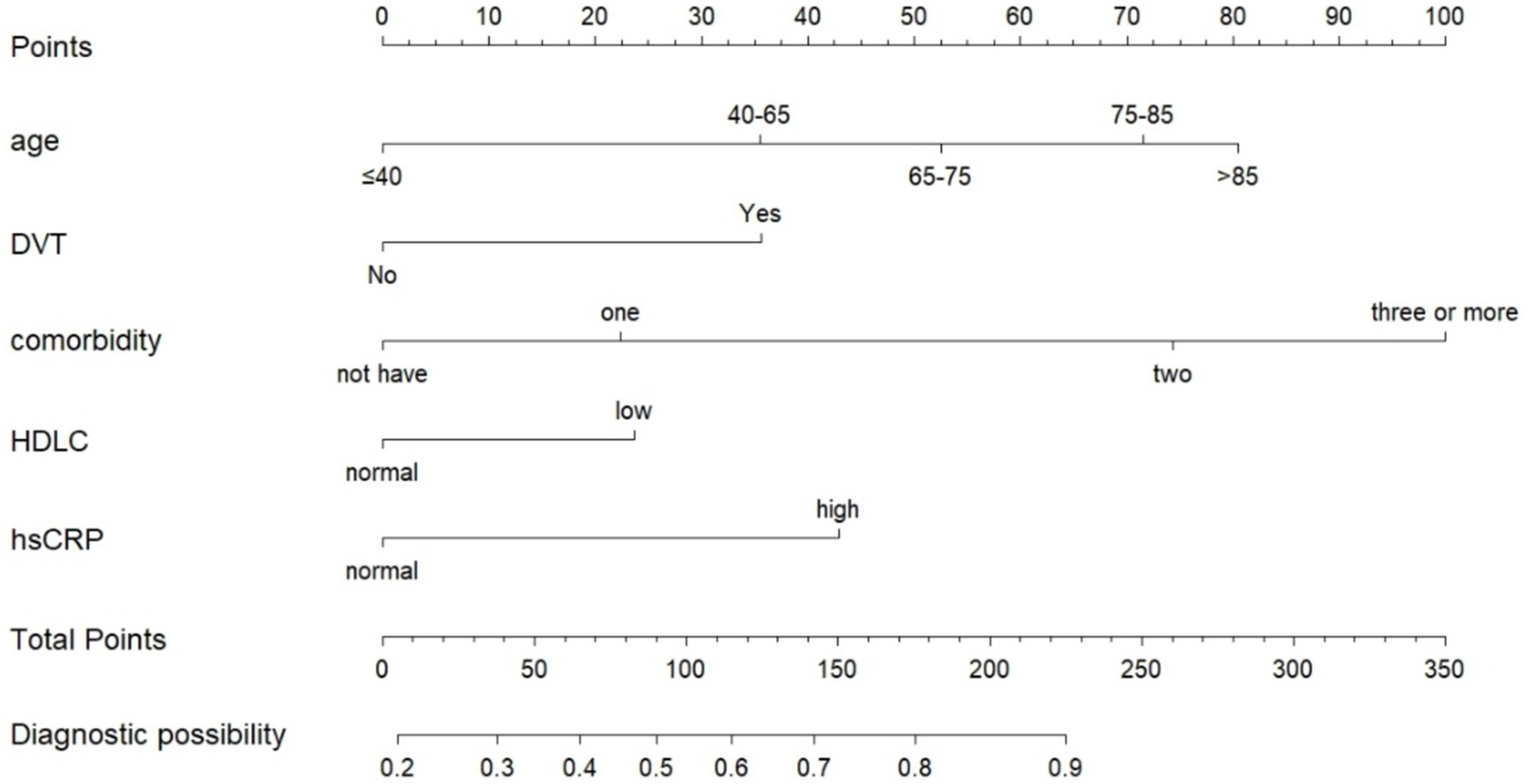
Figure 1. Nomogram for predicting prolonged preoperative waiting time of intertrochanteric fracture patients undergoing operative treatment.
Nomogram validation and clinical practiceReceiver operating characteristic curves, calibration curves, and decision curve analysis were generated for both the training and validation sets using the “pROC” and “rmda” packages, along with other methods in R software. After performing 500 bootstrap internal validations, the C-statistic for the training set was 0.799 and for the validation set, it was 0.727. The receiver operating characteristic curve is then plotted (Supplementary Figure S1). The receiver operating characteristic curves demonstrate that the model has excellent discriminatory ability (Figure 2). The calibration curves indicated strong agreement between the predicted and observed values for the preoperative waiting times in both the training and validation sets (Figure 3). The Hosmer–Lemeshow test yielded nonsignificant p-values of 0.729 and 0.211 for the two sets, respectively. The decision curve analysis curves revealed that the net benefit of using the nomogram to predict prolonged preoperative waiting times was maximized when threshold probabilities ranged from 0.02 to 0.60 for both sets. These results suggest that the model possesses strong clinical applicability and validity (Figure 4).
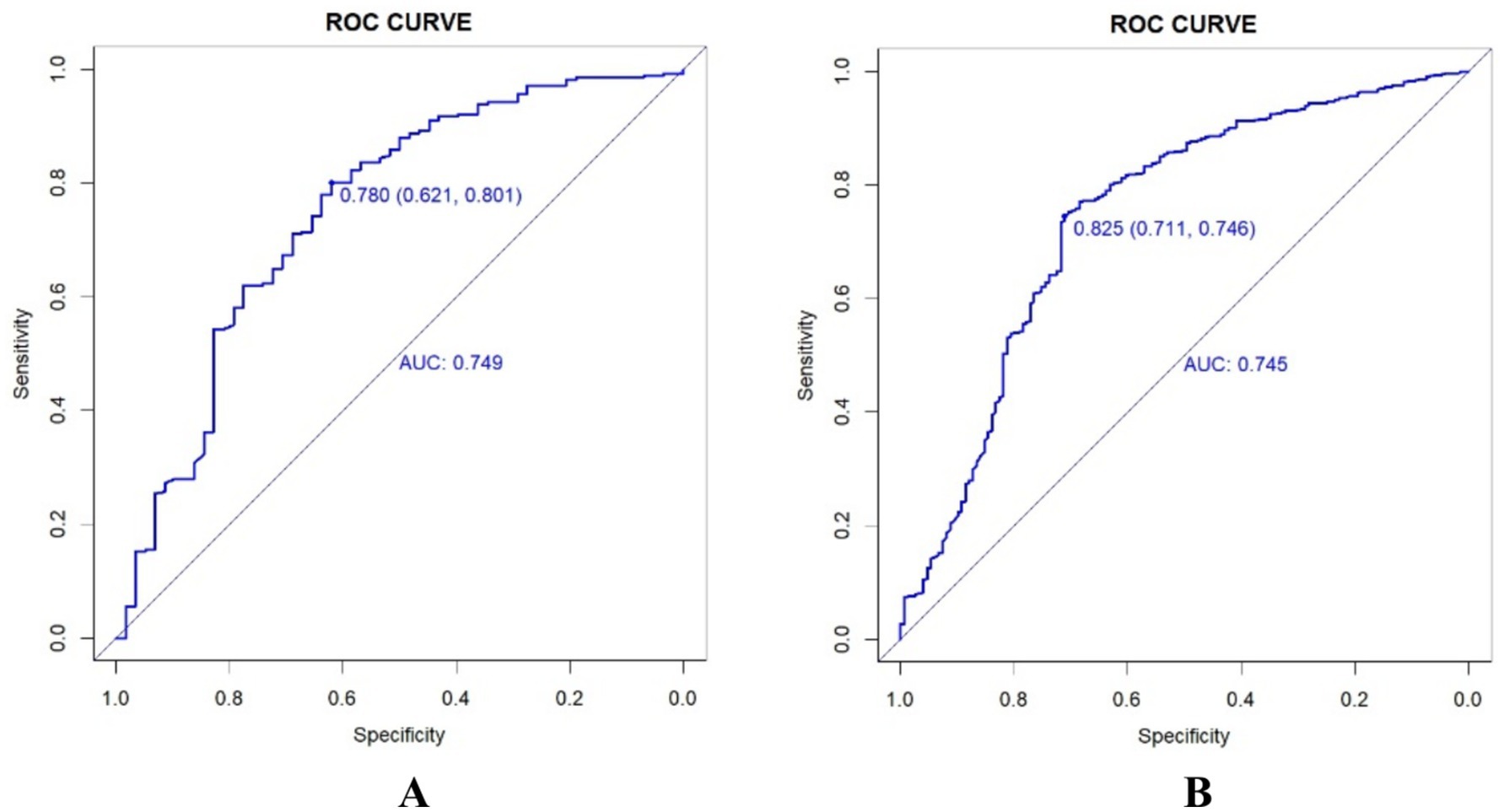
Figure 2. Receiver job characteristic curves for training sets (A) and validation sets (B).
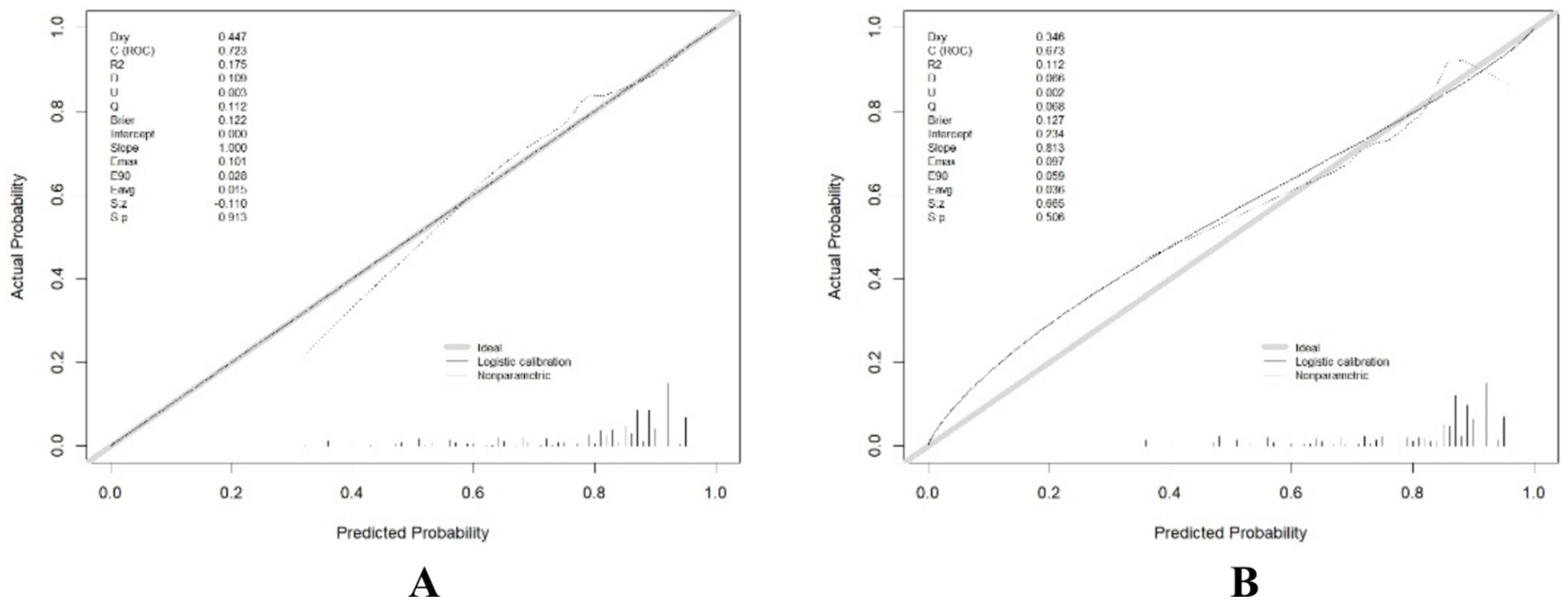
Figure 3. Comparison of calibration curves between the training set (A) and the testing set (B).
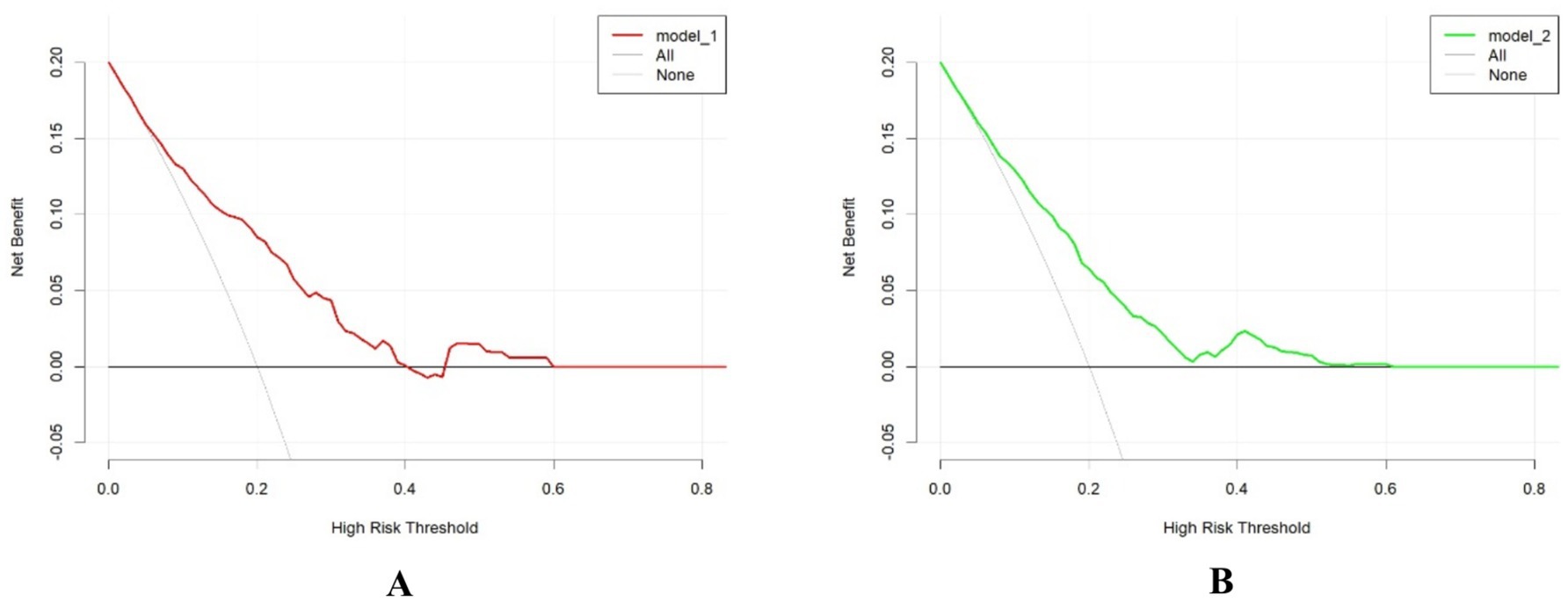
Figure 4. Comparison of decision curve analyses between the training set (A) and the testing set (B).
DiscussionOur study identified age, DVT, comorbidities, HDL-C, and hsCRP as independent risk factors for prolonged preoperative waiting time in patients with intertrochanteric femur fractures. There was a positive correlation between delayed cases and high-risk factors, with more high-risk factors being more likely to delay undergoing surgery. These fractures are increasingly common among older adults and are associated with high mortality rates which impose significant burdens on patients, their families, and society. The 1-year postoperative mortality rate fractures is 15.6–23% (11, 12). Therefore, reducing preoperative waiting times could be critical intervention to lower mortality rates. Accurate prediction of surgical delays at admission may enable physicians to make more informed decisions regarding patient management. In our cohort, 189 patients (16.9%) underwent surgery within 48 h of admission, with an average waiting time of 5.6 days. This finding is consistent with that of the previous study by Li et al. (13). The mean age of the patients in our study was 77.77 years, with 66.8% being over 65 years old, and 25.4% being over 85 years. This age, distribution reflects an increasing in older adults, which is in line with the findings of previous studies (14, 15). Older age often complicates surgical procedures and reduces the body’s ability likely to tolerate surgery without intervention. The study found that 68.3% of patients were female, a proportion higher than that of patients. However, sex did not appear to influence preoperative waiting times. The number of left-sided and right-sided fractures was approximately equal, and our analysis indicated that the side of the injury did not significantly affect surgical delays. Nevertheless, some studies suggest that left-sided intertrochanteric fractures are associated with a higher risk of nonunion and reoperation, possibly due to the biomechanics of locking screws (16, 17). Further investigation is needed to determine if the side of the injury affects surgical duration and length of stay.
Venous thromboembolism is a serious complication of intertrochanteric fractures and a leading cause of mortality. The condition is primarily driven by venous stasis resulting from the fracture, endothelial injury, and systemic hypercoagulability due to trauma collectively known as the Virchow Triad. These factors contribute significantly to the development of DV (18). In our study, a quarter of the patients developed DVT preoperatively, a finding consistent with that of Song et al. (19) DVT affects 28.7% of individuals over the age of 65. Previous research has also identified several risk factors for DVT, including age, high-energy trauma, female sex, diabetes mellitus, chronic obstructive pulmonary disease, A3 typing, hidden blood loss, and abnormalities in lactate dehydrogenase, blood sodium, and hematocrit levels (20–22). To address DVT, prophylactic anticoagulants and inferior vena cava filters are commonly used. Anticoagulants are routinely administered to patients with intertrochanteric fractures at our hospital, yet some still develop DVT. Inferior vena cava filters, while effective, are costly and not affordable for all patients. Additionally, the prolonged course of anticoagulant therapy may contribute to extended preoperative waiting times, making patients more susceptible to DVT.
Our analysis indicates that comorbidities are significant risk factors for prolonged preoperative waiting times. Of the patients with three or more comorbidities, only 71 (10%) underwent surgery within 48 h. This delay may be attributed to the prevalence of comorbidities among older adults, many of which are respiratory and circulatory conditions that contribute to surgical postponements. Our study found that hypokalemia and hyponatremia at admission did not significantly affect preoperative waiting times. This is likely because these electrolyte imbalances can often be corrected quickly with medication. Conversely, HDL-C plays a critical role in regulating atherosclerosis through cholesterol reverse transport mechanisms and by influencing vascular endothelial function, inflammation, and innate immunity. Low HDL-C levels are associated with an increased risk of atherosclerotic cardiovascular disease (23, 24). We identified 11 patients with low HDL cholesterol who were diagnosed with atherosclerotic cardiovascular disease after admission. Low HDL-C levels have also been linked to a higher risk of DVT (25).
While our study did not specifically examine the impact of high HDL-C levels on preoperative waiting times, research by Lee et al. (26) suggests that elevated HDL-C levels reduce the likelihood of hip fractures. Additionally, elevated preoperative C-reactive protein (CRP) levels (>10 mg/dL) are associated with both short-term and long-term postoperative mortality in older adults with hip fractures (27, 28). High CRP levels are linked to an increased incidence of postoperative complications and higher mortality rates, making elevated CRP a plausible factor in prolonged preoperative waiting times for femoral neck fractures (29). At our hospital, hsCRP is routinely tested upon admission and is similar to CRP. Elevated hsCRP levels are associated with an increased risk of postoperative incision infections (30). Despite prophylactic antibiotic administration preoperatively, many doctors choose to delay surgery until hsCRP levels normalize.
Our analysis identified high levels of cystatin C as statistically significant (p < 0.05) in univariate regression analysis. Elevated cystatin C levels are associated with an increased risk of intertrochanteric fractures (31) and have been linked to postoperative sarcopenia, which leads to more complications in patients with hip fractures (32). Furthermore, high cystatin C levels are thought to be associated with increased mortality in older adults with hip fractures (33). Cystatin C reflects weakness and decreased physical function, potentially resulting in reduced surgical tolerance. Its lack of significance in multivariate regression analysis may be due to multifactorial interference or insufficient statistical power, indicating the need for further analysis with larger sample sizes. Hypoproteinemia was found to be statistically significant in univariate logistic regression analysis. It is associated with malnutrition and an increased number of comorbidities (34) and can also contribute to the development of DVT (35).
The predictive model we developed can help assess whether patients with intertrochanteric fractures in the future can receive timely surgical treatment, especially during physical examinations at community hospitals for older adults. Recording and filing data are crucial for effective geriatric hip management and care (36). Ensuring prompt hospital admission, particularly in rural areas for transfer to central medical facilities in cities, is essential (37). The model can be used alongside relevant measures to minimize preoperative waiting times. For high-risk patients identified upon arrival, implementing a fast-track care approach for patients with hip fractures can help shorten admission and surgery times (38). Additionally, a rapid reimbursement system is crucial for financially disadvantaged, high-risk patients (39). Based on previous studies, there is no need to reduce the use of warfarin analogs for patients at high risk of prolonged preoperative waiting times (40, 41). However, opioid use should be minimized in older adults who are at a higher risk of extended waiting periods (42). Multidisciplinary management, including the establishment of specialized geriatric orthopedic wards, can improve care for high-risk older adults (43). Reducing unnecessary auxiliary examinations, creating green channels for expedited care, and optimizing empirical drug use can help minimize delays due to comorbidities and poor underlying conditions. These strategies contribute to more effective surgical outcomes, shorter hospital stays, improved patient prognosis, and reduced economic burden.
LimitationsThe present study was a single-center retrospective analysis. This study focused only on patients with intertrochanteric femoral fractures in China, so limitations due to selection bias cannot be excluded. In addition, there is ongoing debate in the literature about the relevance of nomograms to different patient populations based on race (44). Our data is derived from real-world situations and may have imbalances that affect the effectiveness of the model. Due to the limited clinical information available, we could not analyze the impact of sociological factors such as patients’ lifestyle habits, educational level, and family members’ status on surgical delays. Moreover, we could not analyze emergencies that occurred during the treatment. Because the families of most of the deceased patients refused to communicate with us, the loss of follow-up made it impossible to analyze the mortality rate of the patients and the risk factors for death.
ConclusionOur study identified age, DVT, comorbidities, HDL-C, and ultrasensitive CRP as significant risk factors for prolonged preoperative waiting times in patients with intertrochanteric femur fractures. By developing a risk prediction model for prolonged preoperative waiting times, we can more accurately identify high-risk patients who may experience delays in surgery. This model enables the formulation of more personalized, scientific, and optimized treatment plans for these patients, ultimately aiming to improve outcomes and reduce delays.
Data availability statementThe original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
Ethics statementThe studies involving humans were approved by Ethics Committee of the Affiliated Hospital of Shandong University of Traditional Chinese Medicine. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation was not required from the participants or the participants’ legal guardians/next of kin in accordance with the national legislation and institutional requirements.
Author contributionsRG: Data curation, Investigation, Methodology, Software, Validation, Visualization, Writing – original draft. X-mJ: Software, Writing – original draft. L-yX: Data curation, Writing – original draft. Z-mZ: Software, Writing – original draft. D-tY: Investigation, Writing – original draft. W-pX: Supervision, Writing – review & editing. Y-kZ: Writing – review & editing.
FundingThe author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interestThe authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statementThe authors declare that no Gen AI was used in the creation of this manuscript.
Publisher’s noteAll claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary materialThe Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fmed.2024.1503719/full#supplementary-material
References1. Jegathesan, T, and EBK, K. Are intertrochanteric fractures evolving? Trends in the elderly population over a 10-year period. Clin Orthop Surg. (2022) 14:13–20. doi: 10.4055/cios20204
Crossref Full Text | Google Scholar
2. Zhang, X, Yang, M, Zhang, J, Ye, P, Wong, RMY, Cheung, WH, et al. Establishing a Chinese older hip fracture registry for older patients: a Delphi study to define the focus and key variables for this registry. Osteoporos Int. (2023) 34:1763–70. doi: 10.1007/s00198-023-06832-5
Crossref Full Text | Google Scholar
4. Greve, K, Ek, S, Bartha, E, Modig, K, and Hedström, M. Waiting more than 24 hours for hip fracture surgery is associated with increased risk of adverse outcomes for sicker patients: a nationwide cohort study of 63,998 patients using the Swedish hip fracture register. Acta Orthop. (2023) 94:87–96. doi: 10.2340/17453674.2023.9595
Crossref Full Text | Google Scholar
5. Shen, L, He, X, Li, T, Xiang, Y, Luo, M, Zhang, Y, et al. A commentary on 'In-hospital waiting time to surgery and functional outcomes in geriatric hip fractures: a directed acyclic graph-based preplanned analysis from a prospective multicenter cohort study'. Int J Surg. (2024) 110:3107–8. doi: 10.1097/JS9.0000000000001180
Crossref Full Text | Google Scholar
6. Lei, H, Zhou, L, Huang, K, and Zhuang, W. Correlation between the waiting time and postoperative complications in elderly patients undergoing operation of hip fracture. Asian J Surg. (2024) 47:1798–9. doi: 10.1016/j.asjsur.2023.12.110
Crossref Full Text | Google Scholar
7. Qin, L, Yang, S, Zhao, C, Yang, J, Li, F, Xu, Z, et al. Prospects and challenges for the application of tissue engineering technologies in the treatment of bone infections. Bone Res. (2024) 12:28. doi: 10.1038/s41413-024-00332-w
Crossref Full Text | Google Scholar
8. Kjaervik, C, Gjertsen, JE, Engeseter, LB, Stensland, E, Dybvik, E, and Soereide, O. Waiting time for hip fracture surgery: hospital variation, causes, and effects on postoperative mortality: data on 37,708 operations reported to the Norwegian hip fracture register from 2014 to 2018. Bone Jt Open. (2021) 2:710–20. doi: 10.1302/2633-1462.29.BJO-2021-0079.R1
Crossref Full Text | Google Scholar
9. Liu, F, Chang, WJ, Wang, X, Gong, R, Yuan, DT, Zhang, YK, et al. Risk factors for prolonged preoperative waiting time of intertrochanteric fracture patients undergoing operative treatment. BMC Musculoskelet Disord. (2022) 23:912. doi: 10.1186/s12891-022-05865-x
Crossref Full Text | Google Scholar
10. Roberts, KC, Brox, WT, Jevsevar, DS, and Sevarino, K. Management of hip fractures in the elderly. J Am Acad Orthop Surg. (2015) 23:131–7. doi: 10.5435/JAAOS-D-14-00432
Crossref Full Text | Google Scholar
11. Babagoli, M, Ghaseminejad Raeini, A, Sheykhvatan, M, Baghdadi, S, and Shafiei, SH. Influencing factors on morbidity and mortality in intertrochanteric fractures. Sci Rep. (2023) 13:12090. doi: 10.1038/s41598-023-38667-9
Crossref Full Text | Google Scholar
12. Wang, PW, Yao, XD, Zhuang, HF, Li, YZ, Xu, H, Lin, JK, et al. Mortality and related risk factors of fragile hip fracture. Orthop Surg. (2022) 14:2462–9. doi: 10.1111/os.13417
Crossref Full Text | Google Scholar
13. Li, XP, Zhang, P, Zhu, SW, Yang, MH, Wu, XB, and Jiang, XY. All-cause mortality risk in aged femoral intertrochanteric fracture patients. J Orthop Surg Res. (2021) 16:727. doi: 10.1186/s13018-021-02874-9
Crossref Full Text | Google Scholar
14. Morikawa, M, Urabe, Y, Maeda, N, Suzuki, Y, Junpei, S, Kobayashi, T, et al. Association between falling direction and age in older patients with hip fractures. Z Gerontol Geriatr. (2021) 54:547–54. doi: 10.1007/s00391-020-01824-0
Crossref Full Text | Google Scholar
15. Feng, JN, Zhang, CG, Li, BH, Zhan, SY, Wang, SF, and Song, CL. Global burden of hip fracture: the global burden of disease study. Osteoporos Int. (2024) 35:41–52. doi: 10.1007/s00198-023-06907-3
Crossref Full Text | Google Scholar
16. Oosterhoff, JHF, Dijkstra, H, Karhade, AV, Poolman, RW, Schipper, IB, Nelissen, R, et al. Clockwise torque results in higher reoperation rates in left-sided femur fractures. Injury. (2023) 54:110757. doi: 10.1016/j.injury.2023.04.044
Crossref Full Text | Google Scholar
17. Gu, A, Doe, K, Bracey, L, Agarwal, A, Raffa, T, Farley, B, et al. Increased 1-year revision rates among left-sided intertrochanteric femur fractures. J Orthop Trauma. (2024) 38:431–4. doi: 10.1097/BOT.0000000000002829
Crossref Full Text | Google Scholar
18. Whiting, PS, and Jahangir, AA. Thromboembolic disease after orthopedic trauma. Orthop Clin North Am. (2016) 47:335–44. doi: 10.1016/j.ocl.2015.09.002
Crossref Full Text | Google Scholar
19. Song, K, Zhu, B, Yao, Y, Jiang, Q, Xiong, J, and Shi, H. Incidence and risk factors of preoperative deep vein thrombosis in patients with intertrochanteric fractures: a retrospective study. J Orthop Surg Res. (2022) 17:375. doi: 10.1186/s13018-022-03268-1
Crossref Full Text | Google Scholar
20. Ding, K, Wang, H, Jia, Y, Zhao, Y, Yang, W, Chen, W, et al. Incidence and risk factors associated with preoperative deep venous thrombosis in the young and middle-aged patients after hip fracture. J Orthop Surg Res. (2022) 17:15. doi: 10.1186/s13018-021-02902-8
Crossref Full Text | Google Scholar
21. Fan, J, Zhou, F, Xu, X, Zhang, Z, Tian, Y, Ji, H, et al. Clinical predictors for deep vein thrombosis on admission in patients with intertrochanteric fractures: a retrospective study. BMC Musculoskelet Disord. (2021) 22:328. doi: 10.1186/s12891-021-04196-7
Crossref Full Text | Google Scholar
22. Cong, Y, Wang, B, Fei, C, Zhang, H, Li, Z, Zhu, Y, et al. Dynamic observation and risk factors analysis of deep vein thrombosis after hip fracture. PLoS One. (2024) 19:e0304629. doi: 10.1371/journal.pone.0304629
Crossref Full Text | Google Scholar
23. Kirchgessner, TG, Sleph, P, Ostrowski, J, Lupisella, J, Ryan, CS, Liu, X, et al. Beneficial and adverse effects of an LXR agonist on human lipid and lipoprotein metabolism and circulating neutrophils. Cell Metab. (2016) 24:223–33. doi: 10.1016/j.cmet.2016.07.016
Crossref Full Text | Google Scholar
24. Catapano, AL, Pirillo, A, Bonacina, F, and Norata, GD. HDL in innate and adaptive immunity. Cardiovasc Res. (2014) 103:372–83. doi: 10.1093/cvr/cvu150
Crossref Full Text | Google Scholar
25. Li, W, Ling, H, Lu, R, Huang, Z, and Su, W. Nomogram based on high-density lipoprotein cholesterol for the occurrence of preoperative deep vein thrombosis in patients with intertrochanteric femur fracture: a retrospective study. J Orthop Surg Res. (2024) 19:22. doi: 10.1186/s13018-023-04497-8
Crossref Full Text | Google Scholar
26. Lee, JW, Kim, J, Kim, Y, Kim, YS, Kim, J, and Kang, HT. Higher high-density lipoprotein cholesterol levels increased vertebral osteoporotic fracture, but reduced hip fracture in men based on the National Health Insurance Service-National Health Screening Cohort. Spine J. (2024) 24:1929–38. doi: 10.1016/j.spinee.2024.05.003
Crossref Full Text | Google Scholar
27. Cacciola, G, Mancino, F, Holzer, LA, De Meo, F, De Martino, I, Bruschetta, A, et al. Predictive value of the C-reactive protein to albumin ratio in 30-day mortality after hip fracture in elderly population: a retrospective observational cohort study. J Clin Med. (2023) 12:4544. doi: 10.3390/jcm12134544
Crossref Full Text | Google Scholar
28. Long, A, Yang, D, Jin, L, Zhao, F, Wang, X, Zhang, Y, et al. Admission inflammation markers influence Long-term mortality in elderly patients undergoing hip fracture surgery: a retrospective cohort study. Orthop Surg. (2024) 16:38–46. doi: 10.1111/os.13932
Crossref Full Text | Google Scholar
29. Laggner, R, Taner, B, Straub, J, Tiefenböck, TM, Binder, H, Sator, T, et al. Do elevated serum C-reactive-protein levels excuse delayed surgery for femoral neck fractures? Antibiotics. (2023) 12:738. doi: 10.3390/antibiotics12040738
PubMed Abstract | Crossref Full Text | Google Scholar
30. Xie, L, Liu, G, Wang, X, Luo, Z, Li, Y, Wang, X, et al. Development of a nomogram to predict surgical site infection after open reduction and internal fixation for closed pilon fracture: a prospective single-center study. J Orthop Surg Res. (2023) 18:110. doi: 10.1186/s13018-023-03598-8
Crossref Full Text | Google Scholar
31. Fried, LF, Biggs, ML, Shlipak, MG, Seliger, S, Kestenbaum, B, Stehman-Breen, C, et al. Association of kidney function with incident hip fracture in older adults. J Am Soc Nephrol. (2007) 18:282–6. doi: 10.1681/ASN.2006050546
Crossref Full Text | Google Scholar
32. Chen, X, Shen, Y, Hou, L, Yang, B, Dong, B, and Hao, Q. Sarcopenia index based on serum creatinine and cystatin C predicts the risk of postoperative complications following hip fracture surgery in older adults. BMC Geriatr. (2021) 21:541. doi: 10.1186/s12877-021-02522-1
Crossref Full Text | Google Scholar
33. Zhang, BF, Liu, L, Xu, K, and Xu, P. Serum cystatin C as a biomarker to predict all-cause mortality in geriatrics hip fracture. Heliyon. (2024) 10:e24037. doi: 10.1016/j.heliyon.2024.e24037
Crossref Full Text | Google Scholar
34. Li, Y, Liu, F, Xie, H, and Zhu, Y. Investigation and analysis of frailty and nutrition status in older adult patients with hip fracture. Nutr Clin Pract. (2023) 38:1063–72. doi: 10.1002/ncp.10993
Crossref Full Text | Google Scholar
35. Zhu, Q, Xu, X, Chen, X, Yang, H, Yang, Y, and Chen, Y. Frequency and risk factors of deep venous thrombosis in aged patients with intertrochanteric fracture on admission. J Coll Physicians Surg Pak. (2024) 34:981–4. doi: 10.29271/jcpsp.2024.08.981
Crossref Full Text | Google Scholar
36. Xu, L, Yang, M, Zhang, X, Zhang, J, He, J, Wen, L, et al. The cost-effectiveness of a co-managed care model for elderly hip fracture patients in China: a modelling study. Lancet Reg Health West Pac. (2024) 49:101149. doi: 10.1016/j.lanwpc.2024.101149
Crossref Full Text | Google Scholar
37. Butler, SA, Salipas, A, and van der Rijt, A. Comparative study of outcomes for elderly hip fractures presenting directly to a referral hospital versus those transferred from peripheral centres. ANZ J Surg. (2019) 89:1314–8. doi: 10.1111/ans.15419
Crossref Full Text | Google Scholar
38. Pollmann, CT, Røtterud, JH, Gjertsen, JE, Dahl, FA, Lenvik, O, and Årøen, A. Fast track hip fracture care and mortality - an observational study of 2230 pa
留言 (0)