Dextrocardia is a congenital malposition of the heart that occurs in approximately 1 in 10,000–12,000 individuals (1). Radiofrequency ablation (RFA) has recently become widely used to treat atrial fibrillation (AF). Additionally, left atrial appendage occlusion (LAAO) is increasingly accepted to prevent cerebral infarction and bleeding complications associated with oral anticoagulant therapy (2). While there have been reports of RFA and LAAO procedures performed in patients with dextrocardia (3–5), there have been no reports of the simultaneous “one-stop” surgery (combined RFA and LAAO) in this patient population.
Case descriptionAn 85-year-old male patient with dextrocardia (Figure 1) was hospitalized 4 years ago due to cerebral infarction, during which an electrocardiogram revealed AF. He was later referred to our hospital after recurrent cerebral infarctions despite regular oral anticoagulant therapy (rivaroxaban 15 mg/day). A 24 hour Holter electrocardiogram confirmed persistent AF (Figure 2). The patient's CHA2DS2-VASc score was 5, and his HAS-BLED score was 3, both indicating the need for “one-stop” surgery (6, 7). After explaining the risks and benefits of the procedure, the patient agreed to proceed with treatment after signing the informed consent form.
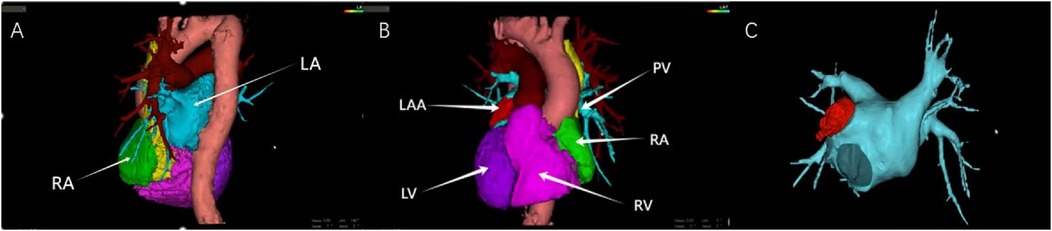
Figure 1. (A) Computed tomography (CT) three-dimensional (3D) reconstruction of the heart (RA, right atrium; LA, left atrium); (B) CT 3D reconstruction of the heart (LAA, left atrial appendage, LV, left ventricle, PV, pulmonary vein, RA, right atrium, and RV, right ventricle); (C) CT 3D reconstruction of the left atrium.

Figure 2. Electrocardiogram of a patient with atrial fibrillation.
Given the patient's advanced age and dextrocardia, the heart structure was relatively complex. To ensure a safe “one-stop” procedure, we used ICE to exclude LAA thrombus, assist with puncture guidance, and monitor the pericardium. The ventricular electrode was advanced under fluoroscopy in an anteroposterior view, while the coronary sinus electrode was introduced under fluoroscopic guidance at a 45° right anterior oblique view. Despite thorough preparation, transseptal (TS) puncture was a challenging task. Fortunately, we completed it under ICE and x-ray guidance, with fluoroscopic angles opposite those typically used in standard TS punctures. The needle tip was directed toward the patient's leg at 10–11 o'clock, contrary to the usual 4–5 o'clock direction, with the puncture site confirmed under a 45° left anterior oblique view and ICE (Figure 3). A long guide wire was inserted in the right anterior oblique position to confirm entry into the left atrium (LA). Heparin (6,000 IU) was administered based on the patient's body weight, and the activated coagulation time was maintained at 250–300 s. A Pentaray electrode was used to construct the electroanatomical voltage mapping of the LA and pulmonary veins (Figure 4A). Bilateral pulmonary vein isolation was performed during AF (Figure 4B), and no pulmonary vein potentials were detected after a 30 min observation period.
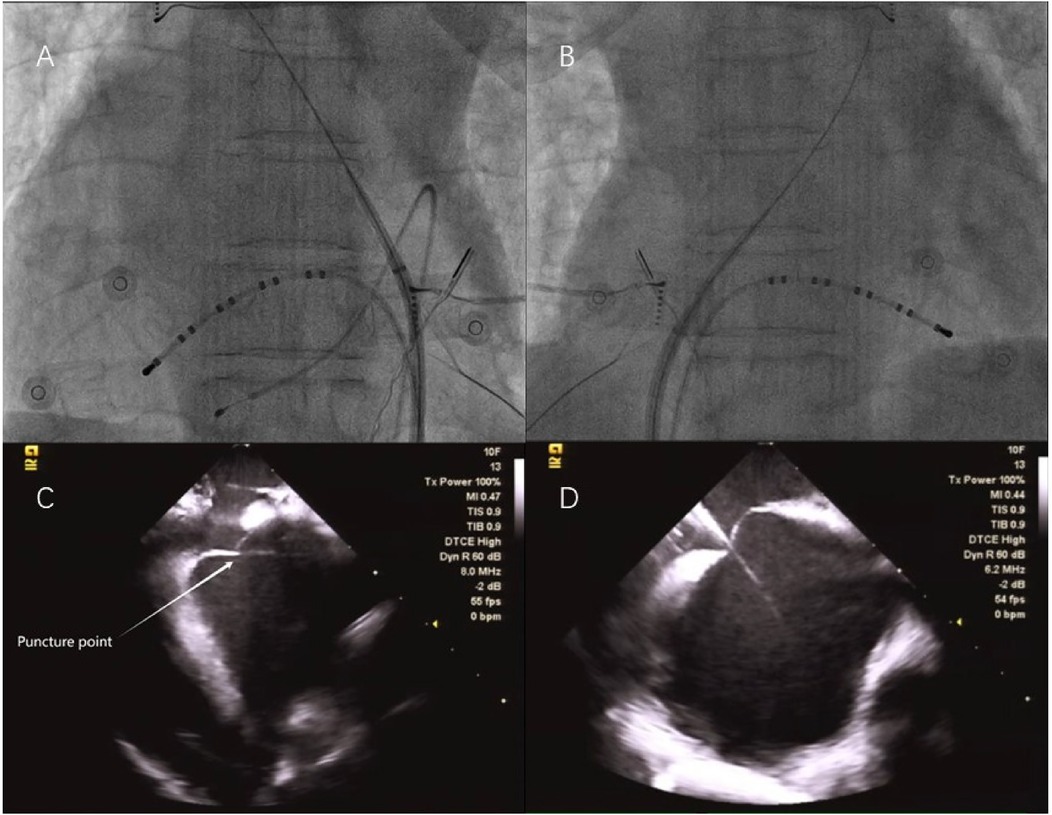
Figure 3. (A) X-ray image of the first transseptal (TS) puncture at position A–P; (B) X-ray image of the second TS puncture, taken at a 180° mirror image; (C) Intracardiac echocardiography (ICE) image of the first TS puncture; and (D) ICE image of the second TS puncture.
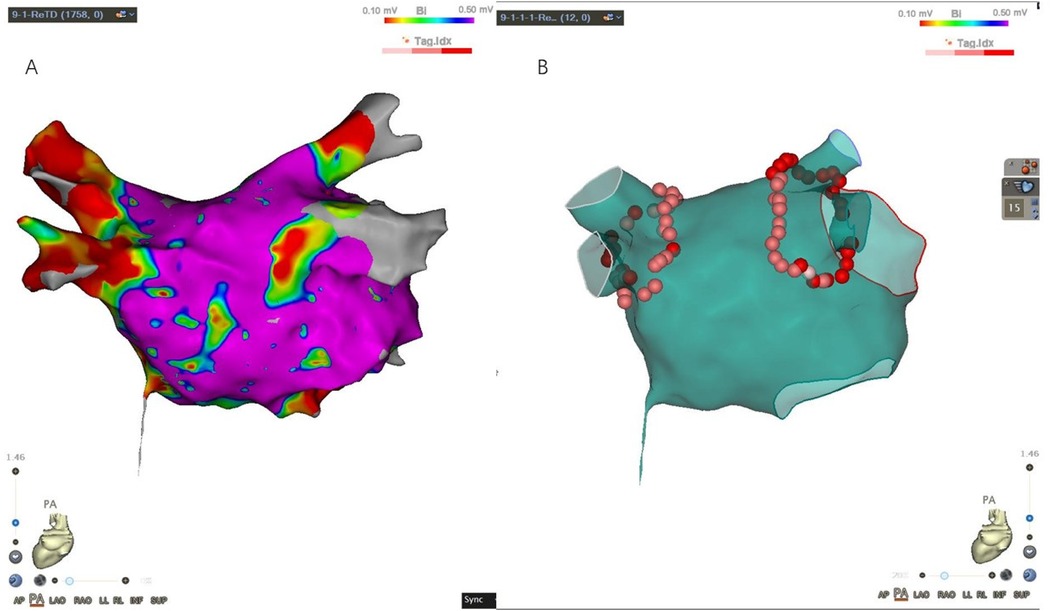
Figure 4. (A) Left atrial electroanatomical map during atrial fibrillation; (B) ablation map.
After withdrawing the ablation catheter, we attempted to place the pig-tail catheter into the LAA along the TS sheath. However, due to the initial puncture site being backward and upward, we performed a second TS puncture. This second puncture differed in two key aspects: (1) the patient had an atrial septal aneurysm (ASA), which made it difficult to direct the Swartz sheath to the proper puncture site. Therefore, we used the VIZIGO bidirectional adjustable bent sheath; and (2) we adjusted the angiographic system settings to achieve a 180° mirror image (Figure 3). Though the process was challenging, the second puncture site was lower, facilitating subsequent LAAO. The LAA was angiographically evaluated, and its size was measured. A LAAO-I 28 device was selected and deployed under x-ray guidance. Both final angiographic and ICE results were excellent, with no peridevice leaks detected after the procedure (Figure 5). The patient continued to receive rivaroxaban (15 mg/day) and amiodarone (200 mg/day) after surgery. At the 3-month follow-up, the patient remained in sinus rhythm (Figure 6) with no postoperative complications. The oral anticoagulant therapy was discontinued, and the patient was switched to aspirin (100 mg/day) and clopidogrel (75 mg/day) for antiplatelet therapy (Table 1).
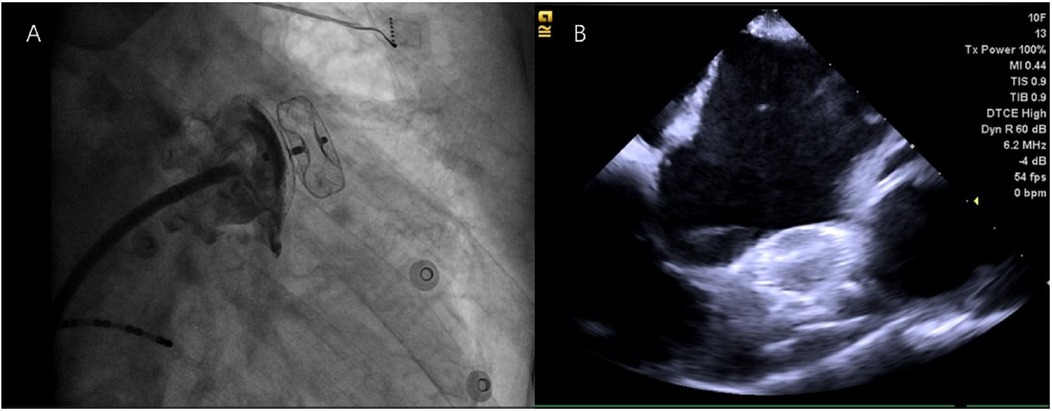
Figure 5. No peridevice leaks were detected after the procedure, as shown in x-ray (A) and intracardiac echocardiography (B).
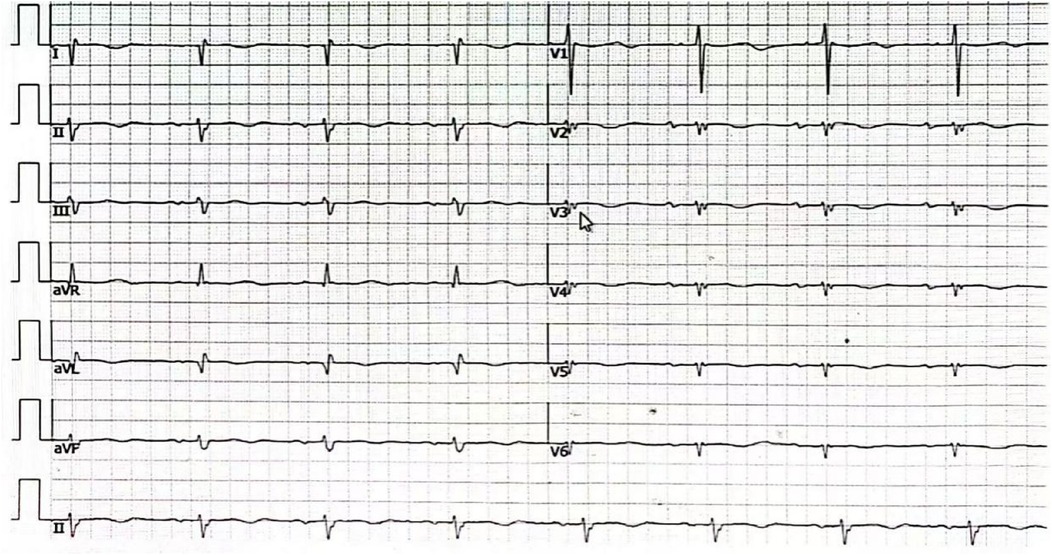
Figure 6. The electrocardiogram of the patient remained in sinus rhythm 3 months after the procedure.
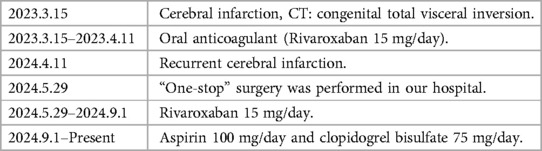
Table 1. A table displaying the timeline with relevant data from the episode of care.
DiscussionAs far as we know, this is the first reported case of successful “one-stop” surgery in a patient with dextrocardia. Despite encountering some unexpected challenges, the procedure proceeded smoothly and safely, ultimately delivering significant benefits to the patient.
The cardiac anatomy of patients with dextrocardia differs from that of individuals with normal heart positioning, which undoubtedly increases the difficulty of the surgery. According to previous literature (3–5), adjusting the settings of the angiographic system to achieve a 180° mirror image may be highly beneficial to the success of the operation.
ICE plays two key roles during the procedure: (1) detecting the pericardium by advancing the ICE catheter through the femoral vein into the middle of the right atrium to establish the “Home View”, then withdrawing it to the “Euclistosis ridge” view of the lower right atrium. The catheter is then bent forward across the tricuspid valve into the right ventricle and rotated counterclockwise after slightly easing the bend, and (2) assisting with TS puncture by slightly advancing the ICE catheter from the “Home View” and rotating it counterclockwise by approximately 90° to visualize the fossa ovalis.
Accurate localization of the TS puncture site is crucial for performing “one-stop” surgery in patients with dextrocardia and AF. Given the challenges associated with TS puncture in these cases, intraoperative ultrasound imaging is essential, particularly when dealing with complex atrial septal anatomies (e.g., thickened interatrial septum and ASA). The VIZIGO bidirectional adjustable bent sheath can assist in the puncture. Moreover, a lower TS puncture site is critical for patients with dextrocardia to complete LAAO successfully.
This case, however, has certain limitations and deficiencies. For example, (1) the postoperative follow-up period is relatively short, and (2) this is a single case, which makes it difficult to generalize the findings to a broader population.
Data availability statementThe original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding authors.
Ethics statementWritten informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributionsZZ: Conceptualization, Investigation, Writing – original draft, Writing – review & editing. XF: Writing – original draft, Writing – review & editing. MG: Writing – original draft, Writing – review & editing. JG: Supervision, Writing – original draft, Writing – review & editing. RW: Resources, Writing – original draft, Writing – review & editing.
FundingThe author(s) declare financial support was received for the research, authorship, and/or publication of this article. This study was supported by the supporting funds for the “Introduction of Talents” doctoral program in the First Hospital of Shanxi Medical University from 2020 to 2021 (Grant No. 09686#); Basic Research Program of Shanxi Province (Grant No. 202203021222378); Project funded by China Postdoctoral Science Foundation (Grant No. 2023M732152).
Conflict of interestThe authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statementThe author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher's noteAll claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References1. Bohun CM, Potts JE, Casey BM, Sandor GG. A population-based study of cardiac malformations and outcomes associated with dextrocardia. Am J Cardiol. (2007) 100:305–9. doi: 10.1016/j.amjcard.2007.02.095
PubMed Abstract | Crossref Full Text | Google Scholar
2. Lakkireddy DR, Wilber DJ, Mittal S, Tschopp D, Ellis CR, Rasekh A, et al. Pulmonary vein isolation with or without left atrial appendage ligation in atrial fibrillation: the aMAZE randomized clinical trial. JAMA. (2024) 331:1099–108. doi: 10.1001/jama.2024.3026
PubMed Abstract | Crossref Full Text | Google Scholar
3. Yamada T, McElderry HT, Doppalapudi H, Platonov M, Epstein AE, Plumb VJ, et al. Successful catheter ablation of atrial fibrillation in a patient with dextrocardia. Europace. (2008) 10:1120–2. doi: 10.1093/europace/eun165
PubMed Abstract | Crossref Full Text | Google Scholar
5. Castriota F, Nerla R, Squeri A, Micari A, Del Giglio M, Cremonesi A. Working in the mirror: left atrial appendage closure in a patient with dextrocardia. JACC Cardiovasc Interv. (2016) 9:e117–20. doi: 10.1016/j.jcin.2016.03.032
PubMed Abstract | Crossref Full Text | Google Scholar
6. Potpara T, Grygier M, Häusler KG, Nielsen-Kudsk JE, Berti S, Genovesi S, et al. Practical guide on left atrial appendage closure for the non-implanting physician: an international consensus paper. Europace. (2024) 26(4):euae035. doi: 10.1093/europace/euae035
PubMed Abstract | Crossref Full Text | Google Scholar
7. Tzeis S, Gerstenfeld EP, Kalman J, Saad EB, Sepehri Shamloo A, Andrade JG, et al. 2024 European heart rhythm association/heart rhythm society/Asia pacific heart rhythm society/Latin American heart rhythm society expert consensus statement on catheter and surgical ablation of atrial fibrillation. Europace. (2024) 26(4):euae043. doi: 10.1093/europace/euae043
留言 (0)