Water is essential for human life, and the global demand for freshwater has surged six-fold over the past century, increasing by about 1% annually since the 1980s (du Plessis, 2023). This demand strains water quality. In addition, approximately 1.6 billion people are facing economic water scarcity, and two-thirds of the world’s population are experiencing water shortages for at least 1 month annually. Industrialization, agriculture, and urbanization have polluted vital water bodies, harming health and hindering sustainable development (Ondrasek, 2013). Worldwide, it is estimated that 80% of industrial and municipal wastewater is discharged untreated into the environment, posing serious risks to both human health and ecosystems. Water-related diseases such as cholera, typhoid, polio, ascariasis, cryptosporidiosis, and various diarrheal illnesses claim the lives of approximately 3.4 million people annually in developing countries (Osiemo et al., 2019). Bangladesh is a stark example, where inadequate sanitation and insufficient wastewater treatment intensify the dual crises of water pollution and scarcity. The country, home to an intricate network of over 230 rivers, faces escalating threats from pollution driven by human activities related to water, sanitation, and hygiene. These challenges are dire, with water pollution alone contributing to 8.5% of all deaths in Bangladesh (Islam et al., 2021). Addressing these issues requires urgent, coordinated efforts to improve water management and sanitation infrastructure, not only in Bangladesh but across regions facing similar vulnerabilities. Globally, cholera remains a major health threat in over 47 countries; there are approximately 2.9 million cases of cholera and 95,000 deaths due to cholera annually (Bilal et al., 2023). In Bangladesh, cholera affects around 100,000 people and causes nearly 4,500 deaths annually. Outbreaks of the disease spike biannually, during spring and the post-monsoon season (Almagro-Moreno et al., 2015), due to seasonal factors, such as flooding, drought, and the water temperature (Ivers, 2018).
Cholera is a disease caused by the bacterium Vibrio cholerae. The bacterium secretes cholera toxin (CT), which causes severe watery diarrhea (Monir et al., 2022). V. cholerae thrives in stagnant or contaminated water, and remains highly infectious for up to 24 h after excretion. It survives the longest at water temperatures of around 30°C with 15% salinity and a pH of 8.5. The primary route of transmission is the consumption of contaminated water or food. The infectious dose of Vibrio cholerae ranges from 1,000 to 100 million colony-forming units, with an incubation period varying from 12 h to 5 days (Sigman and Luchette, 2012). Among the over 200 known serogroups of V. cholerae, the O1 and O139 serogroups have been responsible for the most recent and widespread epidemics. The O1 serogroup is further classified into the classical, El Tor, and altered El Tor biotypes (Azman et al., 2013). Cholera toxin (CT), a heat-sensitive exotoxin produced by V. cholerae, binds to the mucosal lining of the small intestine. This interaction disrupts cellular processes by elevating cyclic adenosine monophosphate (cAMP) levels, resulting in severe fluid and electrolyte loss (Alam et al., 2012). Additionally, V. cholerae employs the toxin-coregulated pilus (TcpA) as a receptor for the cholera toxin phage (CTXφ), which facilitates colonization and further exacerbates the disease (De Haan and Hirst, 2004; Boyd and Waldor, 2002). Efforts to control cholera have centered on improving water, sanitation, and hygiene (WaSH), deploying antibiotics, and expanding access to oral cholera vaccines (OCVs) (Holmgren, 2021b). However, the persistent recurrence of outbreaks in Bangladesh underscores the limitations of these measures and the urgent need for complementary strategies. Promising avenues include exploring the use of probiotics as a novel intervention to disrupt V. cholerae colonization and toxin production (Davies et al., 2017).
Probiotics are live microorganisms that provide health benefits when administered in adequate amounts. They have been gaining much attention for their potential to combat infectious diseases, such as cholera (Hsueh and Waters, 2019). While traditional treatments, such as antibiotics and oral rehydration therapy (ORT), remain crucial, they face limitations, including increasing antibiotic resistance (Chowdhury et al., 2022; Nalin, 2021). Thus, probiotics have been considered as a supplementary or alternative approach due to their ability to improve gut health, inhibit pathogen growth, and modulate the immune system. Strains like Lactobacillus and Bifidobacterium have shown promise in inhibiting V. cholerae growth and biofilm formation, which are key factors for the persistence of the pathogen (Plaza-Diaz et al., 2019). These probiotics produce acidic byproducts that lower the pH level, creating a hostile environment for V. cholerae (Alamdary and Bakhshi, 2020). They also boost host immune responses by enhancing immunoglobulin A (IgA) production, which strengthens the mucosal barrier against CT (Gou et al., 2022). Moreover, probiotics, such as Lactobacillus rhamnosus GG, have been shown to reduce the levels of proinflammatory cytokines, such as interleukin-8 (IL-8), helping to maintain intestinal integrity and prevent severe inflammation during V. cholerae infection (Nandakumar et al., 2009). Engineered probiotics, such as Lactococcus lactis, have been designed to detect and disrupt V. cholerae quorum sensing, and thereby reduce its virulence (Mao et al., 2018). In addition, recombinant Escherichia coli strains expressing GM1 ganglioside mimics have been shown to neutralize CT (Yu et al., 2016). Additionally, probiotics can enhance the effectiveness of OCVs by promoting a favorable gut environment (Amdekar et al., 2010). Commensal bacteria like Ruminococcus obeum can interfere with V. cholerae quorum sensing and further shows the potential of using probiotics to modulate the gut microbiome in favor of the host and against the pathogen (Jimenez and Sperandio, 2019). These multi-faceted benefits—from antimicrobial action to immune support—highlight the potential of probiotics in cholera management, particularly in regions where conventional methods are limited. This review examines the water pollution situation in Bangladesh, its link to cholera outbreaks, and the role of probiotics in mitigating the impact of the disease.
2 Water pollution in BangladeshBangladesh is a nation with a vast river system and a dense population, and water contamination is a major environmental and public health issue in the country (Figure 1). The country’s water resources, including over 230 rivers, are under significant threat due to both natural and human activities. Severe contamination is observed in both surface and groundwater sources, posing serious risks to public health, the environment, and the economy (Uddin and Jeong, 2021). There are significant regional variations in water quality in Bangladesh. In this section, data on the water pollution in key regions of Bangladesh are summarized with a focus on the dissolved oxygen (DO), biochemical oxygen demand (BOD), chemical oxygen demand (COD), and heavy metal levels.

Figure 1. Pathways of water pollution leading to health impacts in Bangladesh. The pollutants enter water bodies, leading to contaminated rivers, human exposure, and adverse health effects.
Rivers near Dhaka city, including the Buriganga, Turag, and Shitalakshya rivers, are severely polluted due to industrial activities and urban runoff. The Buriganga river has critically low DO levels (0.9–2.8 mg/L) and high COD levels (140–800 mg/L) due to untreated effluents (Sarkar et al., 2019). Similarly, the Turag river has near-zero DO levels, COD levels of 102–475 mg/L, and high BOD levels (Ahmed et al., 2016). The Shitalakshya river shows near-zero DO levels, and elevated BOD and COD levels, especially during the dry season, due to industrial effluents (Mourshed et al., 2017). In northern Bangladesh, rivers, such as the Teesta, Korotoa, and Atrai rivers, are impacted by agricultural runoff and urban wastes. The Teesta river has high levels of heavy metals, such as cadmium, iron, and manganese, exceeding the standards of the World Health Organization and the Food and Agriculture Organization of the United Nations (Chettri and Joshi, 2022). The Korotoa river has high concentrations of chromium and cadmium, and DO levels below 4 mg/L (Hassan et al., 2024). The Atrai river has moderate-to-high pollution levels due to seasonal agricultural and urban waste discharge (Anik et al., 2022). Rivers in the southern coastal regions, including the Karnaphuli and Meghna rivers, are polluted from industrial discharges and agricultural runoff (Gani et al., 2023). The Karnaphuli river is polluted from shipbreaking yards and industries, and has high levels of heavy metals, such as lead, cadmium, and mercury (Chowdhury et al., 2024). The Meghna river is contaminated by upstream pollution sources; it has COD levels of 20.84–114.6 mg/L, and high levels of heavy metals, such as iron and chromium, that exceed the safe limits (Flura et al., 2016). The Ganges and Padma rivers in western Bangladesh are important as sources of water for drinking and for agriculture, but they are becoming increasingly polluted. The Ganges river has moderate DO levels and elevated BOD levels as well as high concentrations of arsenic and lead (Mukherjee et al., 1993). The Padma river shows fluctuating water quality, with occasionally high coliform levels and suboptimal DO, BOD, and COD levels that reflect agricultural runoff and industrial discharges (Flura et al., 2016). The groundwater in rural Bangladesh is heavily contaminated with arsenic; the concentration often exceeds 10 μg/L, and reaches up to 500 μg/L in some areas. This contamination affects millions of people who rely on tube wells for drinking water, and leads to widespread health issues, such as arsenicosis and cancer (Chakraborti et al., 2010). Overview of key water quality parameters in the table below showed the actual water quality in Bangladesh (Table 1).
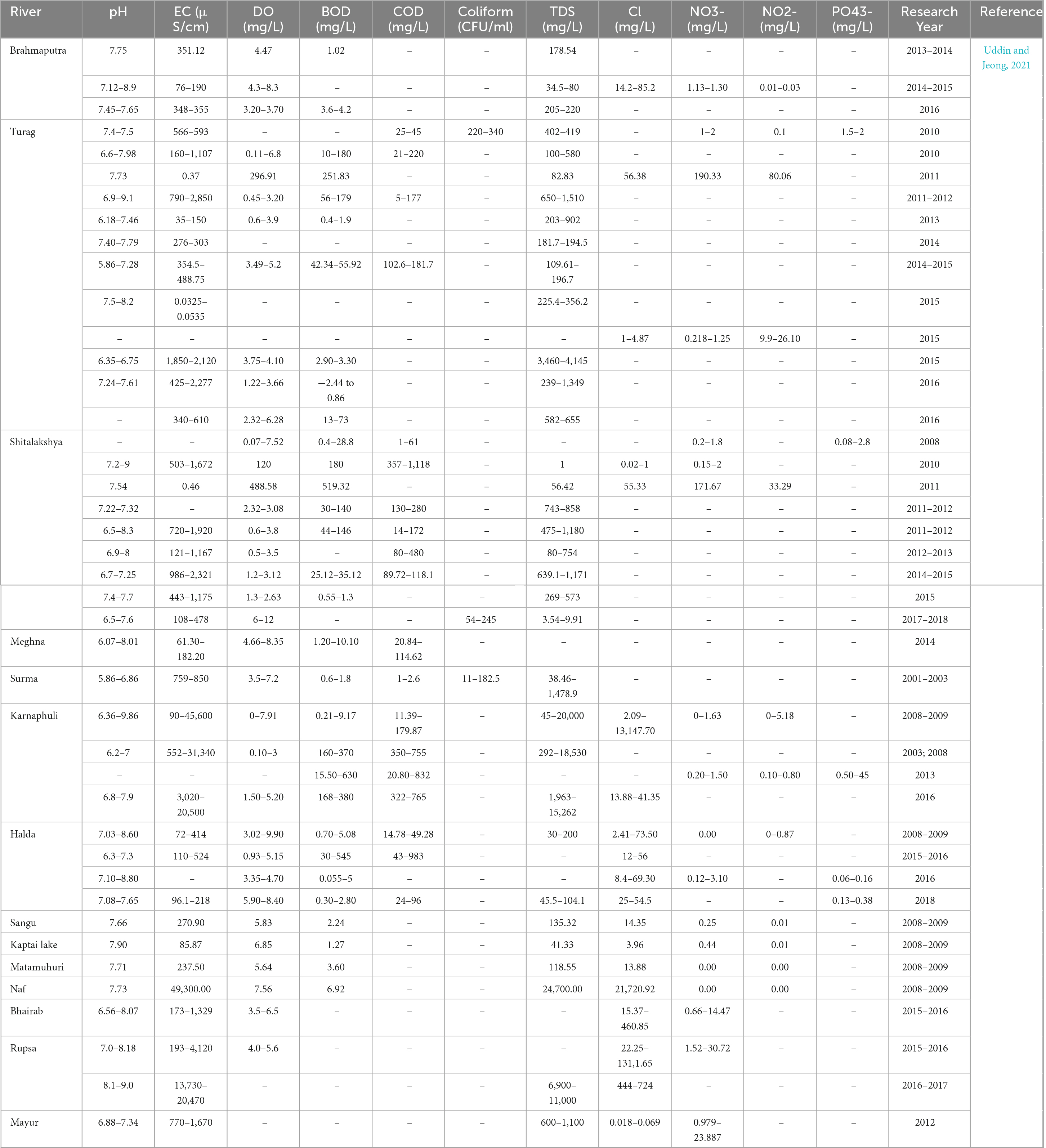
Table 1. Overview of key water quality parameters for major rivers in Bangladesh.
2.1 Types of water pollution in BangladeshWater pollution is the contamination of water bodies—rivers, lakes, seas, and groundwater—primarily caused by human activities. It occurs when harmful substances, such as chemicals, wastes, and pathogens, are introduced into the water, rendering it unsafe for consumption, disrupting ecosystems, and degrading the environment (Chakraborti et al., 2010). In Bangladesh, the water pollution can be categorized into different types, organic, inorganic, chemical, and pathogenic.
Organic pollution is mainly caused by untreated domestic sewage and industrial effluents that are high in biodegradable matter. As the biodegradable matter decomposes, the DO level decreases, which is harmful to aquatic life. Indicators like the COD and BOD are used to measure this type of pollution. Rivers like the Buriganga, Turag, and Shitalakshya rivers have critically low DO levels, indicating severe organic contamination (Islam and Azam, 2015). Inorganic pollutants, such as salts and metals, persist in the environment and cannot be biodegraded. In Bangladesh, industrial discharges, agricultural runoff, and natural leaching are the primary sources of inorganic pollutants. Key contaminants, such as arsenic and iron, are found in groundwater, and arsenic poses a significant public health risk (Rahman et al., 2021). Chemical pollution primarily arises from industrial processes, particularly in the textile, dyeing, and leather industries. Untreated chemicals, including dyes, acids, and heavy metals, are released into rivers, causing severe water degradation. The Karnaphuli river near Chittagong is notably affected by these pollutants (Islam et al., 2017). Pathogenic pollution occurs when harmful microorganisms, such as bacteria, viruses, and protozoa, contaminate water. Improper sewage disposal, human wastes, and inadequate sanitation contribute to this problem. Waterborne diseases, such as cholera, diarrhea, and dysentery, are prevalent in Bangladesh, particularly in rural areas with limited access to clean water (Table 2; Knappett et al., 2011). Agriculture, while vital to Bangladesh, contributes significantly to water pollution. Fertilizers and pesticides, such as carbamates and organophosphates, wash into water bodies, contaminating surface water and groundwater. This runoff bioaccumulates in the food chain, posing risks to ecosystems and human health (Chopra et al., 2011). Thermal pollution occurs when industries discharge heated water into natural water bodies, raising the water temperature and disrupting ecosystems; this is particularly harmful to temperature-sensitive species. In Bangladesh, this issue is seen in regions where industrial plants discharge heated cooling water (Kibria and Yousuf Haroon, 2017). Improper disposal of plastic and solid wastes also contributes heavily to water pollution. Rivers and canals in urban areas like Dhaka are clogged with non-biodegradable wastes, worsening floods during monsoons and harming aquatic life. Plastic accumulation also creates breeding grounds for disease vectors (Mourshed et al., 2017).
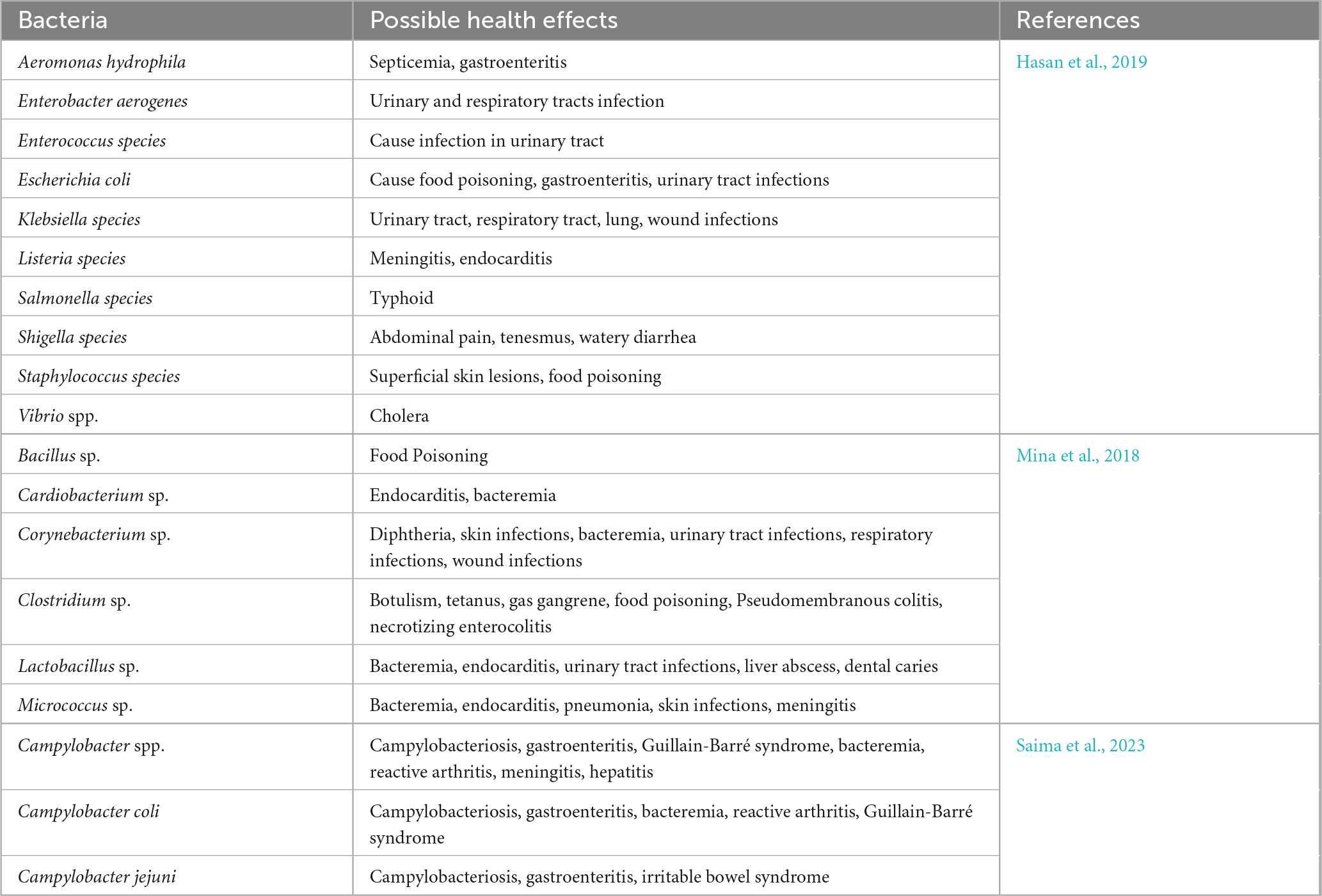
Table 2. Bacteria in Bangladesh water and their health hazards.
2.2 Major sources of water pollution in BangladeshWater pollution is a major environmental challenge in Bangladesh that threatens public health, aquatic ecosystems, and environmental sustainability. The primary sources of the pollution are diverse, and are driven by rapid industrialization, urbanization, and agricultural practices (Singh et al., 2004). The key sources of water pollution in Bangladesh are discussed below with examples from various studies and reports.
Rapid industrialization, especially in textiles, dyeing, leather, and pharmaceuticals, has led to large volumes of untreated wastewater being discharged into water bodies. The textile sector alone produced around 217 million cubic meters of wastewater in 2016, and the figure was projected to rise to around 349 million cubic meters by 2021 (Hossain et al., 2018). Such wastewater containing dyes, chemicals, and/or heavy metals, such as chromium, cadmium, and lead, severely contaminates water sources around Dhaka and Chittagong (Mina et al., 2018). The tannery sector in Hazaribagh also contributes to water pollution by releasing hazardous chemicals, such as sulfides and acids (Anawar et al., 2000). Pharmaceutical and chemical industries further pollute aquatic ecosystems, as seen in the heavily impacted Karnaphuli river (Chowdhury et al., 2024).
Urbanization and population growth have led to increases in household and municipal wastes, much of which ends up in water bodies due to poor waste management. Inadequate sewage treatment, such as at the Pagla Sewage Treatment Plant, results in raw sewage being discharged into rivers like the Buriganga and Shitalakshya rivers. Raw sewage contains organic matter and pathogens that lead to the spread of waterborne diseases, such as cholera (Majed and Islam, 2022). Urban solid wastes, including plastics, are frequently dumped into water bodies, causing blockages and pollution. The Buriganga river is biologically inactive in some sections due to severe solid waste pollution (Reza and Yousuf, 2016; Karn and Harada, 2001).
Agricultural runoff from excessive fertilizer and pesticide use is a major source of non-point source water pollution. Fertilizers, pesticides like DDT and carbofuran, and contaminants in irrigation water lead to bioaccumulation in water bodies, which poses risks to aquatic life and human health (Chhabra, 2021). The healthcare sector also contributes to water pollution by disposing of pharmaceuticals, disinfectants, and biological wastes. Many of Bangladesh’s 600 hospitals lack proper waste disposal systems, and as a result, toxic substances enter water bodies and pose health risks (Hassan et al., 2008).
The shipbreaking industry in coastal Chittagong is another significant source of pollution; it releases heavy metals, asbestos, and oil residues into the sea, contaminating the Karnaphuli river and nearby waters. Ships also discharge bilge water containing hazardous substances, which further degrade the water quality and marine ecosystems (Islam et al., 2013). Natural sources, such as arsenic and iron, also contribute to water pollution. The groundwater in Bangladesh contains high levels of arsenic, affecting millions of people who rely on tube wells for drinking water. Long-term exposure to arsenic can lead to severe health issues, including skin lesions and cancers (Huq et al., 2020).
3 Linking water pollution to cholera outbreaksWater pollution and cholera are closely linked, particularly in developing countries like Bangladesh, where access to clean water is limited. Frequent flooding and widespread contamination of water bodies by V. cholerae, the bacterium responsible for cholera, contribute significantly to the transmission of the disease (Pandey et al., 2014). This section explores how water pollution contributes to cholera outbreaks, with examples from recent studies.
Cholera is primarily transmitted through the ingestion of water contaminated with V. cholerae. The bacteria is naturally present in freshwater and brackish water, and it often attaches to plankton, particularly zooplankton like copepods, which act as reservoirs (Lutz et al., 2013). The zooplankton play a crucial role in facilitating the survival of the bacteria between epidemics, especially during periods of high plankton density following phytoplankton blooms (de Magny et al., 2011). Cholera spread is a complex interplay of human activity, travel, and hydroclimatic processes, affecting the distribution, growth, and incidence of V. cholerae in aquatic ecosystems, and can be improved through epidemiological research and environmental predictive modeling (Usmani et al., 2021). Studies have also shown that the survival of V. cholerae in environmental reservoirs is influenced by the water temperature and salinity, and the presence of organic wastes (Huq et al., 1984; McCarthy, 1996). In Bangladesh, a strong correlation between environmental conditions and cholera outbreaks has been documented, especially during the monsoon season when increased rainfall leads to sewage mixing with drinking water, which increases the risk of cholera (Akanda et al., 2013). Conversely, during the dry season, increased salinity also creates favorable conditions for V. cholerae proliferation (Jutla et al., 2013). Studies have further demonstrated a link between water pollution and the incidence of cholera, and both natural and human-induced changes in water quality in Bangladesh have been linked to the persistence of V. cholerae in polluted and stagnant waters. Water of poor quality, characterized by high pollution levels, low oxygen levels, and pH imbalances, provides ideal conditions for V. cholerae survival (Nguyen et al., 2023). For instance, in Bakerganj, Bangladesh, a study found a strong association between water pollution parameters (such as water temperature, salinity, and conductivity) and the incidence of cholera. A six-week lag was observed between peaks in water temperature and cholera cases, highlighting the role of environmental factors in cholera transmission (Huq et al., 2005). In addition, moderate salinity was found to support bacterial growth, especially in coastal areas during the dry season (Grant et al., 2015). Data from the Matlab Demographic Surveillance Site have also highlighted the role of environmental factors, such as elevated water temperatures and salinity, in promoting V. cholerae growth and cholera outbreaks.
4 Current management strategies for cholera in BangladeshIn Bangladesh, cholera remains a significant public health issue that is driven by environmental factors, the population density, and the limited access to clean water and sanitation. Effective management strategies are crucial for controlling outbreaks. Bangladesh has developed a robust surveillance system, including hospital and community monitoring, particularly during the peak seasons (Hegde et al., 2021). Environmental testing helps predict outbreaks, and both passive and active surveillance enable early interventions (Azman et al., 2015). Once an outbreak is detected, rapid response teams provide medical care, distribute oral rehydration solutions (ORS), and educate communities on prevention measures (Zohura et al., 2022). ORS are highly effective for mild dehydration, while intravenous fluids, such as Dhaka solution, are used for severe cases, reducing the fatality rates (Davies et al., 2017). Antibiotics are prescribed for severe cases, but due to concerns of antimicrobial resistance, they need to be used prudently and require careful monitoring (Leibovici-Weissman et al., 2014). In addition, community engagement is important and can be promoted through public health campaigns focusing on hygiene practices, safe water use, and ORS preparation, particularly in high-risk areas (Khan et al., 2019). Bangladesh’s vaccination strategy combines reactive and preventive approaches to control cholera. Reactive vaccinations contain disease outbreaks, while preventive vaccinations target high-risk populations before outbreaks. This dual approach ensures effective use of vaccines mediated successfully by WaSH (Ronsmans et al., 1988; Chowdhury et al., 2023). Bangladesh employs both reactive and preventive vaccination strategies; however, logistical challenges, such as maintaining the cold chain for vaccine storage, remain (Dimitrov et al., 2014; Uddin et al., 2014). WaSH interventions, including clean water provision, latrine construction, and hygiene education, are essential for cholera prevention, and they have been supported by local governments and non-governmental organizations (Lantagne and Yates, 2018). Bangladesh is also a hub for cholera research, with the icddr,b, an international health research organization located in Dhaka, providing valuable insights into vaccine efficacy, rehydration solutions, and the role of micronutrients, such as zinc (Holmgren, 2021a). Technological innovations, such as the mHealth Diarrhea Management (mHDM) platform, help guide healthcare providers with evidence-based treatments, enabling better antimicrobial stewardship (Chowdhury et al., 2022). Prophylactic measures, including OCVs and selective chemoprophylaxis, are used to prevent the spread of cholera, especially among the close contacts of confirmed cases (Weil et al., 2014). Zinc and vitamin A supplementation are recommended for children under five years old to manage cholera, reduce diarrhea severity, enhance immune response, and promote intestinal lining recovery, as part of standard pediatric cholera management in Bangladesh (Albert et al., 2003; Liberato et al., 2015). New therapies, such as probiotics and phage therapy, are being explored as adjunct treatments, and they appear promising as solutions for dealing with antibiotic-resistant cholera strains and reducing the bacterial load in patients (Hsueh and Waters, 2019; Bhandare et al., 2019).
The evaluation of these strategies underscores a prioritized approach to cholera management, tailored to the severity of cases and the specific implementation context. Oral rehydration salts (ORS) and intravenous fluids remain the cornerstone of cholera treatment, particularly in acute cases, due to their immediate life-saving potential. In parallel, vaccination campaigns and WaSH interventions are indispensable for long-term prevention. However, these measures face persistent logistical challenges, including maintaining vaccine cold chains and ensuring the development of adequate sanitation infrastructure. Probiotics are emerging as a promising adjunctive therapy, offering significant potential in addressing antibiotic-resistant Vibrio cholerae strains. Incorporating probiotics into existing management frameworks could fill critical gaps in treating resistant cases, thereby bolstering Bangladesh’s public health resilience. To fully harness this potential, further research is needed to evaluate the integration of probiotics with established therapies. Such efforts could pave the way for sustainable and effective alternatives to conventional antibiotics, strengthening both immediate treatment outcomes and long-term disease control.
5 Probiotics: an overviewProbiotics, derived from the Greek words “pro” (for) and “bios” (life), refer to live microorganisms that provide health benefits when consumed in sufficient amounts. Unlike antibiotics, which aim to kill harmful bacteria, probiotics work to enhance or restore the microbial balance in the host (Gou et al., 2022). The most widely accepted definition of probiotics comes from the Food and Agriculture Organization and the World Health Organization of the United Nations, who described them as “live microorganisms which, when administered in adequate amounts, confer a health benefit on the host” (Reid et al., 2005). According to this definition, probiotics need to be alive, administered in proper doses, and scientifically proven to offer health advantages. Similarly, the following criteria have been proposed for microorganisms to be classified as probiotics: they must be alive when administered, present in sufficient quantities, have demonstrated health benefits, and be safe for consumption (Kaur et al., 2021).
The concept of probiotics dates back to the early 20th century, when Nobel laureate Élie Metchnikoff suggested that the consumption of fermented milk could promote longevity by improving gut health due to the presence of beneficial bacteria in the milk. His work laid the foundation for modern probiotic research. Probiotics have since been shown to positively affect digestive health, boost immune function, and influence mental health via the gut-brain axis (Tong et al., 2020).
Probiotics predominantly consist of bacteria that are commonly of the genera Lactobacillus, Bifidobacterium, Streptococcus, and Bacillus, although some yeast strains, such as Saccharomyces boulardii, also exhibit probiotic properties (Gupta and Garg, 2009). Lactobacillus species are known to improve gut health, enhance lactose digestion, prevent diarrhea, and support respiratory health (Reid, 1999). Bifidobacterium species are known to play a crucial role in maintaining a healthy gut environment, preventing infections, and supporting immune functions (Turroni et al., 2022). These bacteria promote gut health by producing short-chain fatty acids that help maintain the integrity of the intestinal lining. Yeast probiotics, particularly S. boulardii, have gained attention for their effectiveness in treating gastrointestinal disorders, such as antibiotic-associated diarrhea and infections caused by Clostridium difficile. S. boulardii can withstand the acidic conditions of the stomach, temporarily colonize the gut, and enhance immunity and the gut barrier (Czerucka et al., 2007).
Beyond gut health, probiotics have been linked to mental health benefits through the gut-brain axis (Lenoir-Wijnkoop et al., 2007). Strains of Lactobacillus and Bifidobacterium have been shown to produce neurotransmitters, such as gamma-aminobutyric acid and serotonin, which regulate mood. The results of clinical studies suggest that probiotics can help alleviate symptoms of anxiety, depression, and stress, and may therefore provide a potential therapeutic approach for mental health (Bermúdez-Humarán et al., 2019).
Probiotics also contribute to metabolic health by addressing imbalances in the gut microbiota that are linked to obesity and type 2 diabetes. They help improve insulin sensitivity, reduce inflammation, and promote weight management. For instance, Bifidobacterium lactis has been shown to reduce body fat and improve glucose tolerance in animal models, indicating its potential for managing metabolic disorders (Nagpal et al., 2016).
Moreover, probiotics play an essential role in immune health. They enhance immune responses by increasing the IgA levels, boosting natural killer cell activity, and improving macrophage functions, which can help protect against infections, and possibly even against cancer. Certain strains, such as Lactobacillus casei, have demonstrated the ability to enhance immune responses to respiratory infections (Śliżewska et al., 2020). These findings highlight the broad potential applications of probiotics for promoting health.
5.1 Mechanism of action of probioticsProbiotics exert beneficial effects through several mechanisms, including the modulation of immune responses, enhancement of gut barrier function, competitive exclusion of pathogens, production of antimicrobials, modulation of the gut microbiota composition, interaction with the gut-brain axis, and effects on metabolic health. They modulate immune responses by balancing pro- and anti-inflammatory cytokines, enhancing IL-10 production, and reducing the levels of tumor necrosis factor-α and IL-6, which drive conditions like inflammatory bowel disease (Cristofori et al., 2021). Probiotics also strengthen the intestinal barrier by promoting the production of proteins like occludin and claudin, which prevent pathogen translocation (Castro-Herrera et al., 2020). Through competitive exclusion, probiotics compete with pathogens for adhesion sites, and they also produce antimicrobial substances, including bacteriocins and organic acids, which inhibit pathogen growth (Tejero-Sariñena et al., 2012; Chen et al., 2018). Furthermore, probiotics influence the composition of the gut microbiota and support gut health by promoting the growth of beneficial bacteria and suppressing the growth of harmful species, such as Clostridium species (Wieërs et al., 2019). Additionally, they interact with the gut-brain axis to induce the production of neurotransmitters like gamma-aminobutyric acid, which can modulate brain function, offering potential therapeutic benefits for mental health conditions (Tette et al., 2022). In terms of metabolic health, probiotics help regulate energy metabolism, improve glucose tolerance, and enhance insulin sensitivity, primarily through the production of short-chain fatty acids (Everard and Cani, 2014). Moreover, probiotics interact with the enteric nervous system to influence gut motility and secretion, which is beneficial for conditions like irritable bowel syndrome (Kunze et al., 2009). They also enhance mucosal immunity by increasing the production of secretory IgA, which strengthens the host defense against pathogens (Azad et al., 2018). Probiotics can regulate inflammatory pathways, including the nuclear factor kappa B signaling pathway, and thereby reduce inflammation in conditions like inflammatory bowel disease (Versalovic et al., 2008). Probiotics can also protect against enteric infections by preventing pathogen adhesion and enhancing immune responses (Resta-Lenert and Barrett, 2003), which further highlights the therapeutic potential of probiotics.
5.2 Current research on probiotics in cholera controlIn addition to the traditional cholera control measures, probiotics have emerged as a promising adjunctive treatment. Probiotics can inhibit V. cholerae colonization and neutralize toxins through competitive exclusion, the production of antimicrobial compounds, enhancement of intestinal barrier function, and modulation of the host immune response, and thereby prevent the spread of the disease (Hsueh and Waters, 2019; Chowdhury et al., 2022). This section reviews evidence from various studies that highlight the efficacy of probiotics for preventing and managing cholera infections.
Maintaining a balanced gut microbiota is crucial for limiting the colonization and virulence of V. cholerae. Research has demonstrated that the gut microbiota can affect V. cholerae by modulating chemical signaling pathways, such as those involved in quorum sensing and bile acid metabolism. By influencing these pathways, the commensal bacteria can alter the ability of V. cholerae to express virulence factors and establish an infection. The gut microbiota also competes with V. cholerae for nutrients, which can limit the pathogen’s growth. The interactions between V. cholerae and the gut microbiota are complex and involve various microbial and host factors. Probiotics can modulate the gut microbiota to enhance host resistance against V. cholerae colonization. For example, R. obeum has been identified as a key bacterium that increases in abundance during recovery from cholera; it was found to restrict V. cholerae colonization by producing autoinducer-2, which interferes with the pathogen’s quorum-sensing pathways and downregulates the expression of virulence genes. This natural antimicrobial effect suggests that promoting the growth of such beneficial bacteria through probiotic supplementation could serve as a strategy for preventing and/or mitigating V. cholerae infections (Hsiao et al., 2014).
The ability of V. cholerae to form biofilms is a critical factor for its survival and persistence, both in aquatic environments and the human gut. Probiotics have been shown to have significant potential in disrupting V. cholerae biofilms. For instance, lactobacilli isolated from fecal samples have been shown to inhibit biofilm formation and to disperse formed biofilms by more than 90%. This effect is partly due to the production of acidic byproducts by the lactobacilli; the acidic byproducts alter the pH and disrupt biofilm matrices. Mao et al. (2018) demonstrated that the oral administration of Lactococcus lactis, a widely used fermentative bacterium, significantly reduced the intestinal burden of Vibrio cholerae in infected newborn mice. By producing lactic acid, L. lactis enhanced colonization resistance and improved survival rates. Furthermore, an engineered strain of L. lactis was developed to detect quorum-sensing signals from V. cholerae and produce an enzyme reporter for stool-based diagnostics, opening new avenues for innovative surveillance and intervention strategies (Mao et al., 2018). In addition to L. lactis, Saccharomyces boulardii, a probiotic yeast, has shown potential in binding and neutralizing cholera toxin in vitro. Similarly, Lactobacillus rhamnosus GG and Bifidobacterium longum demonstrated significant toxin removal capabilities, neutralizing 68 and 59% of cholera toxin, respectively, under laboratory conditions. These findings highlight the importance of live probiotic cultures in cholera management, as these effects were both concentration-dependent and absent in non-viable cells or their supernatants. Probiotic activity extends beyond toxin neutralization. Certain Lactobacillus strains have shown remarkable ability to inhibit biofilm formation by V. cholerae and disperse preformed biofilms, achieving inhibition rates exceeding 90% in some cases. These effects were strain-specific and pH-dependent, with biofilm dispersal activity diminishing under neutralized pH conditions. Given that the physiological pH of intestinal biofilms is slightly acidic, strains exhibiting dispersive activity under such conditions are particularly promising for therapeutic applications (Kaur et al., 2018). These findings underscore the multifaceted potential of probiotics in cholera management, ranging from toxin neutralization and biofilm disruption to diagnostic innovation. Future research should prioritize the identification of robust, pH-tolerant strains with clinically significant activity, paving the way for integrative approaches in combating this persistent global health challenge.
L. lactis expressing V. cholerae antigens can stimulate both systemic and mucosal immune responses, providing enhanced protection against cholera (Lei et al., 2011). This dual role of probiotics in competing directly with pathogens and in priming the immune system makes them valuable tools for both prevention and treatment. Engineered probiotics also hold promise as diagnostic tools. For example, L. lactis was engineered to detect quorum-sensing signals from V. cholerae and to express a reporter enzyme that can be detected in fecal samples (Amrofell et al., 2020). This ability to detect and respond to specific pathogenic signals may enable a targeted approach for controlling V. cholerae infections in real time. Another promising approach involves engineering probiotics to neutralize CT directly. In one study, recombinant E. coli strains that express GM1 ganglioside mimics on their surfaces were developed; these mimics could bind to CT and neutralize its harmful effects (Yu et al., 2016). The GM1-expressing E. coli conferred significant protection against fatal V. cholerae infections in infant mice, even when they were administered post-infection. The high affinity of these recombinant probiotics for CT highlights their potential usefulness as therapeutic agents in both the prevention and treatment of cholera, offering an alternative to traditional antibiotic therapies (Focareta et al., 2006). In another similar study, probiotics engineered to detect and respond to V. cholerae as an innovative therapeutic strategy were shown to produce antimicrobial compounds that inhibit V. cholerae and disrupt its quorum-sensing mechanisms, which are essential for its virulence and for biofilm formation (Cruz et al., 2022).
Probiotics can influence V. cholerae through metabolic interactions within the gut environment. Studies using zebrafish models have shown that E. coli strains capable of metabolizing glucose into acidic byproducts significantly reduce V. cholerae colonization. The resulting acidic environment inhibits V. cholerae growth, and is a mechanism by which the metabolic byproducts of commensal or probiotic bacteria can create unfavorable conditions for the pathogen (Nag et al., 2018). The use of multiple probiotic strains together can result in enhanced antimicrobial effects against V. cholerae. For example, a combination of Leuconostoc mesenteroides and Bacillus subtilis in a malted ragi food product was found to significantly inhibit V. cholerae growth, biofilm formation, and adhesion to extracellular matrices. The synergistic action of these probiotics not only enhanced their antimicrobial activity, but also increased the nutritional value of the food, suggesting that functional foods incorporating probiotics could serve dual roles in nutrition and disease prevention (VidyaLaxme et al., 2014). Combining probiotics with conventional cholera treatments, such as ORT and vaccines, could also enhance the overall treatment efficacy. For instance, studies have shown that probiotics capable of acidifying the gut environment can work synergistically with glucose-based ORT to inhibit V. cholerae growth (Basumatary et al., 2021).
Additionally, probiotics have been observed to modulate gut microbial communities in ways that may support the efficacy of OCVs. By promoting a healthier gut microbiota, probiotics can enhance the host immune response to vaccination, and also potentially enhance host defenses against cholera infection (Sit et al., 2019). For example, Bifidobacterium breve BBG-01 was studied for its potential to boost the immunogenicity of an inactivated cholera vaccine. Although the enhancement of vaccine-induced immune responses was not significant, the probiotic did modify the gut microbiota by increasing the Bifidobacterium and reducing the Enterobacteriaceae counts. This shift toward a healthier gut microbiota may promote the overall effectiveness of vaccination by creating a less favorable environment for V. cholerae colonization and enhancing the baseline immunity of the host (Matsuda et al., 2011). Some other studies have explored using probiotics as a vaccine delivery system. For example, L. lactis expressing V. cholerae antigens was found to induce strong mucosal and systemic immunity, and may represent a novel approach to vaccination. The dual role of probiotics as both a vaccine adjuvant and a protective agent against cholera highlights their usefulness and versatility in cholera control strategies (Zamri et al., 2012).
Probiotics can also modulate the host inflammatory response to V. cholerae infection to provide a protective effect. For instance, L. rhamnosus GG has been shown to reduce the expression of IL-8 and other chemokines in human intestinal epithelial cells exposed to V. cholerae. By attenuating the inflammatory response, such probiotics can help maintain the gut integrity and reduce the damage caused by excessive inflammation, which is often a hallmark of severe cholera. This anti-inflammatory effect is yet another layer of protection conferred by probiotics during cholera infection (Nandakumar et al., 2009). Additionally, studies have shown that the ingestion of yogurt containing Lactobacillus acidophilus and Bifidobacterium enhances IgA responses to CT in mice. IgA plays a key role in neutralizing toxins and preventing them from adhering to and penetrating the intestinal epithelium, thereby enhancing mucosal immunity. The use of dietary probiotics to enhance mucosal immunity could therefore be an effective strategy for bolstering the body’s natural defenses against cholera (Tejada-Simon et al., 1999).
The potential for probiotics to provide long-term protection against cholera has also been demonstrated. For example, Bacillus velezensis used in aquaculture showed not only antimicrobial activity against V. cholerae, but also enhancement of host immune response. This dual role in enhancing the frontline antimicrobial defense and boosting long-term immunity suggests that probiotics may useful in broader cholera control programs, particularly in regions where cholera is endemic and where maintaining long-term immunity is crucial (Zhu et al., 2021). Despite these promising findings, translating laboratory and animal model successes to human clinical trials has been inconsistent. Probiotic strains derived from healthy children showed inhibitory effects on Vibrio biofilm formation and adhesion, yet the antibacterial activity against V. parahaemolyticus biofilms was limited. These observations highlight the need for further research to identify robust, strain-specific probiotics for cholera prevention and treatment (Kaur et al., 2018). Probiotics can also play a role in environmental management for preventing cholera outbreaks. Certain probiotics can disrupt V. cholerae biofilms in natural water bodies, and thereby reduce the environmental reservoirs of the pathogen (Kaur et al., 2018). By targeting V. cholerae in its natural habitats, probiotics can help limit the spread of V. cholerae from environmental sources, and thus provide an additional layer of protection in communities where waterborne transmission is a major concern. After studying several articles, we developed a concept that can create a solution to decrease cholera infection in those countries under cholera infection and probiotics should be a solution to decrease this infection (Figure 2).
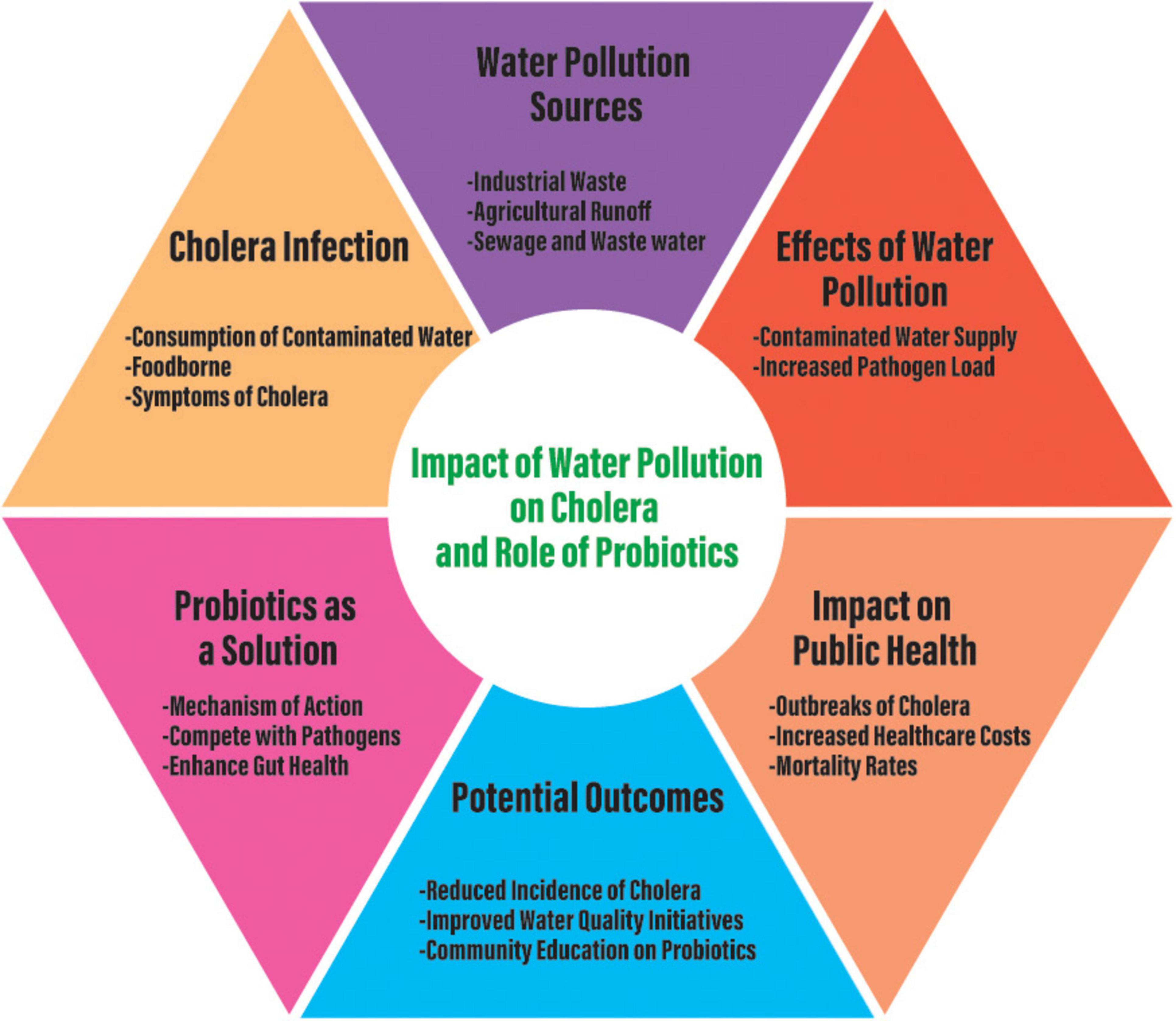
Figure 2. Conceptual diagram regarding cholera infection due to water pollution and the role of probiotics to solve cholera infection to save human life.
6 ConclusionDriven largely by water pollution and conditions of inadequate sanitation, cholera continues to be a significant public health challenge in Bangladesh. The intricate link between environmental factors, such as water pollution, and cholera outbreaks underscores the need for comprehensive strategies to manage and prevent the disease. The traditional methods of managing cholera, including ORT, antibiotics, and vaccination programs, have proven effective, but they are not without limitations. The emergence of antibiotic resistance, logistical challenges in vaccine distribution, and the recurring nature of outbreaks highlight the need for novel and complementary approaches. Probiotics offer a promising avenue for cholera prevention and management. They provide beneficial effects against cholera through various mechanisms, such as the competitive exclusion of the pathogen, enhancement of the gut barrier function, modulation of immune responses, and disruption of pathogen signaling. The development of engineered probiotics may further expand their usefulness, and provide innovative solutions that may enable us to detect and respond to specific pathogenic signals in real time. Additionally, the integration of probiotics with existing interventions, such as vaccines and ORS, can enhance the overall efficacy of cholera control measures. In addressing the cholera epidemic, it is crucial to consider the population groups most affected by this disease. Vulnerable groups, particularly young children and elderly individuals, are often at higher risk due to their weaker immune systems. Additionally, occupations that involve exposure to contaminated water sources, such as fishermen and agricultural workers, should be prioritized in public health interventions. A better understanding of these demographics can guide targeted strategies for prevention and management. Recent studies emphasize the potential of specific probiotic strains, such as Lactobacillus rhamnosus GG and Saccharomyces boulardii, in combating diarrheal diseases, including cholera. Combining probiotics with established interventions like ORS and vaccines could enhance their efficacy by improving gut health and boosting immune responses. Additionally, research on mechanisms like quorum sensing disruption and biofilm inhibition can drive the development of engineered probiotics with targeted action against V. cholerae. Long-term clinical trials and innovative strategies, such as using probiotics to neutralize contaminated water sources, are essential to validate their application in endemic regions like Bangladesh. To ensure practical application, it is essential to propose targeted policy recommendations tailored to the specific conditions of Bangladesh.
Cholera can be managed through immediate measures like emergency response centers, safe water supply, hygiene promotion, vaccination, isolation, and long-term strategies. Long-term measures include improving sanitation, investing in modern water treatment plants, promoting community-led sanitation, and enhancing water quality. Communicating cholera effectively requires a coordinated approach integrating immediate containment with long-term preventive measures. Research should focus on identifying gaps in sanitation and water quality management while fostering innovative solutions tailored to the needs of vulnerable populations. Collaboration among governments, NGOs, and local communities is crucial for sustainable health outcomes. Policies should focus on improving access to clean water and sanitation facilities, increasing awareness of probiotics’ role in public health, and encouraging partnerships between researchers, policymakers, and community stakeholders. Furthermore, investment in infrastructure for the production and distribution of probiotics could facilitate their accessibility and affordability. By harnessing the natural protective effects of probiotics and integrating them into broader cholera control strategies, more sustainable and effective measures can be established. These measures would not only reduce the disease burden but also contribute to improving overall public health outcomes in vulnerable populations. The ongoing exploration of probiotics as a complementary tool in cholera prevention holds immense potential for addressing this persistent public health challenge in Bangladesh.
Author contributionsMRC: Writing – original draft, Writing – review & editing, Investigation. AI: Writing – original draft, Writing – review & editing, Data curation, Formal analysis, Investigation. VY: Writing – original draft, Writing – review & editing, Data curation, Supervision. TS: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing.
FundingThe authors declare that financial support was received for the research, authorship, and/or publication of this article. This work was supported by the Education and Research Support Fund from Shinshu University (2024) to TS.
AcknowledgmentsWe would like to express our sincere gratitude to Ms. Ikeda Hotaru for her invaluable assistance in creating the illustrations for this review.
Conflict of interestThe authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statementThe authors declare that no Generative AI was used in the creation of this manuscript.
Publisher’s noteAll claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
ReferencesAhmed, K., Rahman, A., Sarkar, M., Islam, J., Jahan, I., Moniruzzaman, M., et al. (2016). Assessment on the level of contamination of Turag river at Tongi area in Dhaka, Bangladesh. J. Sci. Ind. Res. 51, 193–202. doi: 10.3329/bjsir.v51i3.29431
Crossref Full Text | Google Scholar
Akanda, A. S., Jutla, A. S., Gute, D. M., Sack, R. B., Alam, M., Huq, A., et al. (2013). Population vulnerability to biannual cholera outbreaks and associated macro-scale drivers in the Bengal Delta. Am. J. Trop. Med. Hyg. 89, 950–959. doi: 10.4269/ajtmh.12-0492
PubMed Abstract | Crossref Full Text | Google Scholar
Alam, M., Islam, M. T., Rashed, S. M., Johura, F. T., Bhuiyan, N. A., Delgado, G., et al. (2012). Vibrio cholerae classical biotype strains reveal distinct signatures in Mexico. J. Clin. Microbiol. 50, 2212–2216. doi: 10.1128/jcm.00189-12
PubMed Abstract | Crossref Full Text | Google Scholar
Alamdary, S. Z., and Bakhshi, B. (2020). Lactobacillus acidophilus attenuates toxin production by Vibrio cholerae and shigella dysenteriae following intestinal epithelial cells infection. Microb. Pathog. 149:104543. doi: 10.1016/j.micpath.2020.104543
PubMed Abstract | Crossref Full Text | Google Scholar
Albert, M. J., Qadri, F., Wahed, M. A., Ahmed, T., Rahman, A. S., Ahmed, F., et al. (2003). Supplementation with zinc, but not vitamin A, improves seroconversion to vibriocidal antibody in children given an oral cholera vaccine. J. Infect. Dis. 187, 909–913. doi: 10.1086/368132
PubMed Abstract | Crossref Full Text | Google Scholar
Amdekar, S., Dwivedi, D., Roy, P., Kushwah, S., and Singh, V. (2010). Probiotics: multifarious oral vaccine against infectious traumas. FEMS Immunol. Med. Microbiol.
留言 (0)