Attention-deficit/hyperactivity disorder (ADHD), as a neurodevelopmental disorders, is a group of syndromes characterized by obvious inattention, hyperactivity and impulsivity (1). The prevalence of ADHD was about 7% and more than 1 million children were affected worldwide (2). ADHD is often accompanied by cognitive impairment and learning difficulties, including executive dysfunction, bad school performance, poor family and peer relationships, and aggressive behavior. It was reported that the incidence of ADHD co-morbid sleep disorders was 25% to 55% in youth (3). The main manifestations are bedtime resistance, sleep difficulty, night awakenings, sleep apnea, and daytime sleepiness (4). Although ADHD symptoms usually appear in childhood, it may continue to adulthood (5, 6), which can seriously affect their quality of life, bringing a huge burden to patients, families and society.
ADHD has been attributed to genetic factors (7) and family factors (8). Notably, with the development of industrial lighting, some people are accustomed to sleeping with lamplight, whereas visible light could have adverse effects on sleep, retina function and psychiatric disorders (9, 10).
No published studies, however, have explored the association between lamplight exposure during sleep at night and ADHD. In addition, previous studies showed that short sleep duration increased the risk of ADHD (11, 12), but the association of long sleep duration with ADHD remains unclear (13–15). Thus, the aim of the present study was to examine the associations of lamplight exposure during sleep and different sleep durations with ADHD among preschool children in China.
Materials and methodsStudy participantsFrom October through December 2021, a cross-sectional survey was conducted in Chengdu, a provincial capital in Southwest China. It was mainly designed to assess the prevalence of and risk factors for psychobehavioral problems among preschool children. A total of 4360 preschool children from 30 kindergartens, were selected by cluster random sampling method. The study protocol was approved by the Ethics Committee of Soochow University (Approval NO. SUDA20210820H01). Written informed consent was obtained from each of the participants (guardians).
In the present study, we excluded 129 children aged less than 3 years and 34 children with missing information. Therefore, the final study population was 4197 children (2190 boys and 2007 girls, mean age 4.28 ± 0.93 years).
Assessment of lamplight exposure during sleep and sleep durationData were collected by a validated questionnaire administered by guardians via WJX (an online survey platform, www.wjx.cn). Information on two independent variables was obtained by the following questions: “How often did your child sleep with the lamplight on at night? (a) 0 night/week, (b) 1-2 nights/week, (c) ≥3 nights/week”, and “For how long did the child sleep daily including siesta? (a) <10 hours/day, (b) 10-12 hours/day, (c) >12 hours/day”. According to the National Sleep Foundation’s sleep duration recommendation (16), total sleep duration with <10 hours/day for preschool children was defined as insufficient sleep in our study.
Definition of ADHDADHD was screened using the Conners Parental Symptom Questionnaire (PSQ), which was compiled originally by the American scholar Conners and revised by Conners, Goyette, and Ulrich in 1978 (17). The PSQ has been widely applied to evaluate psychobehavioral problems of children and adolescents aged 3-17 years. It has been introduced or amended by many countries and shown high reliability and validity (18–20). Cronbach’s α value was 0.933 in our survey.
The 1978 version of PSQ was used in the present study, which included a total of 48 items and 6 measurement dimensions (i.e., conduct problems, learning problems, psychosomatic disorders, hyperactivity-impulsivity, anxiety, hyperactivity index). Hyperactivity index including 10 items was a special screening tool for ADHD. Participants were asked to rate their child’s behavior performance in the past six months. Each item was scored from 0 (not at all) to 3 (very often). ADHD was defined as having an average score of hyperactivity index of ≥1.5.
CovariatesThe children’s demographic characteristics including age (continuous), sex (male or female), lifestyle and family factors including snacks intake (0 days/week, 1-2 days/week, 3-4 days/week or ≥5 days/week), picky eating (yes or no), time of watching TV (0 hours/day, <1 hours/day, 1-2 hours/day or >2 hours/day), home lighting (dark, ordinary, or bright) were collected via the questionnaire. In addition, perinatal factors of the child’s mother including smoking or passive smoking during pregnancy (0 days/week, 1-2 days/week or ≥3 days/week), exercise during pregnancy (0 minutes/day, <20 minutes/day, 20-40 minutes/day, or >40 minutes/day), gestational hyperglycemia (yes or no), gestational hypertension (yes or no), gestational anemia (yes or no), and anxiety or depression during pregnancy (yes or no) were also collected.
Statistical analysesThe basic characteristics of the participants by ADHD status, lamplight exposure during sleep at night and different sleep durations are presented as numbers (percentages), and were compared using Chi-square test or Fisher’s exact test.
We used logistic regression to evaluate the associations of lamplight exposure during sleep at night and sleep duration with ADHD. Three multivariable models were constructed: model 1 was the basic model adjusted for age and sex; model 2 was adjusted as model 1 plus the child’s lifestyle and family factors; model 3 was adjusted as model 2 plus the perinatal factors of mothers. P-trend was calculated by modeling the independent variables as continuous ones in the regression models.
Effect modification of the association between lamplight exposure during sleep and ADHD by sex, picky eating, gestational hyperglycemia and gestational anemia was estimated in stratified analyses, and significance of interactions was evaluated on first-degree multiplicative models for each stratification variable separately.
The statistical analyses were performed using SPSS 26.0 statistical software (IBM Corp., USA). All tests were two-tailed, and a P value <0.05 was considered statistically significant.
ResultsOf the 4197 preschool children, 154 (3.7%) had ADHD. The percentage of the participants who slept with lamplight 0, 1-2, and ≥3 nights/week was 91.5%, 4.7%, and 3.8%, respectively. The proportion of the participants whose sleep duration of <10, 10-12, and >12 hours/day was 24.6%, 72.7%, and 2.7%, respectively.
Table 1 shows the characteristics of the participated children and their mothers by ADHD status. The boys were more likely to have ADHD than the girls. Those children dwelling in an environment without bright light, having frequent snacks intake, picky eating, and watching TV for a long time were more likely to have ADHD (all P< 0.001). Moreover, the prevalence of ADHD was higher in the children whose mother with smoking or passive smoking during pregnancy, less exercise during pregnancy, and gestational anemia (all P< 0.001).
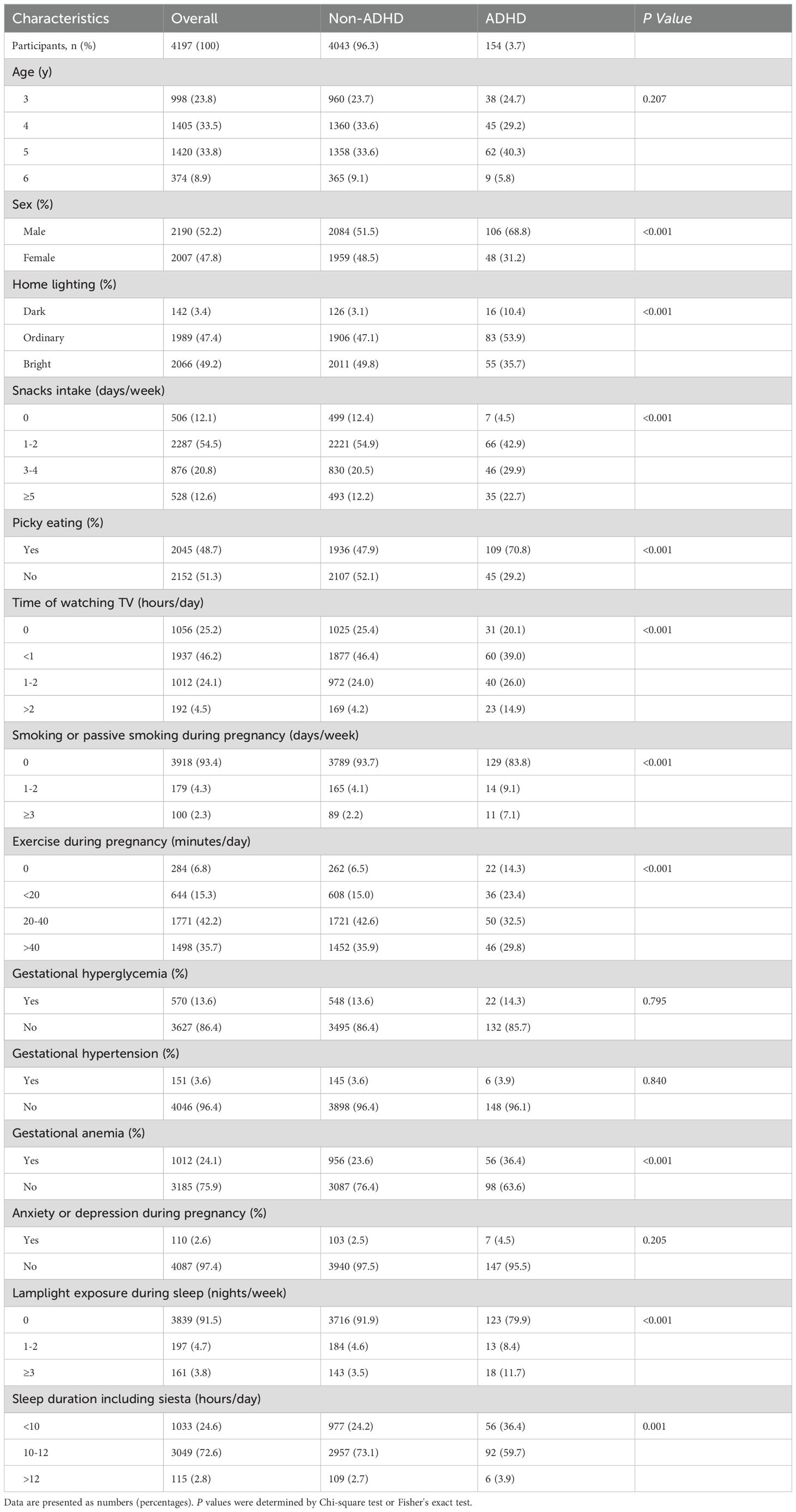
Table 1. Characteristics of the participants according to ADHD status.
The characteristics of the participants in term of lamplight exposure during sleep at night are presented in Table 2. Percentages of picky eating, time of watching TV and proportion of gestational anemia were different between the groups (P< 0.05). Moreover, age, home lighting, picky eating, time of watching TV, exercise during pregnancy, and anxiety or depression during pregnancy were also different with different sleep durations (P< 0.05) (Supplementary Table S1).
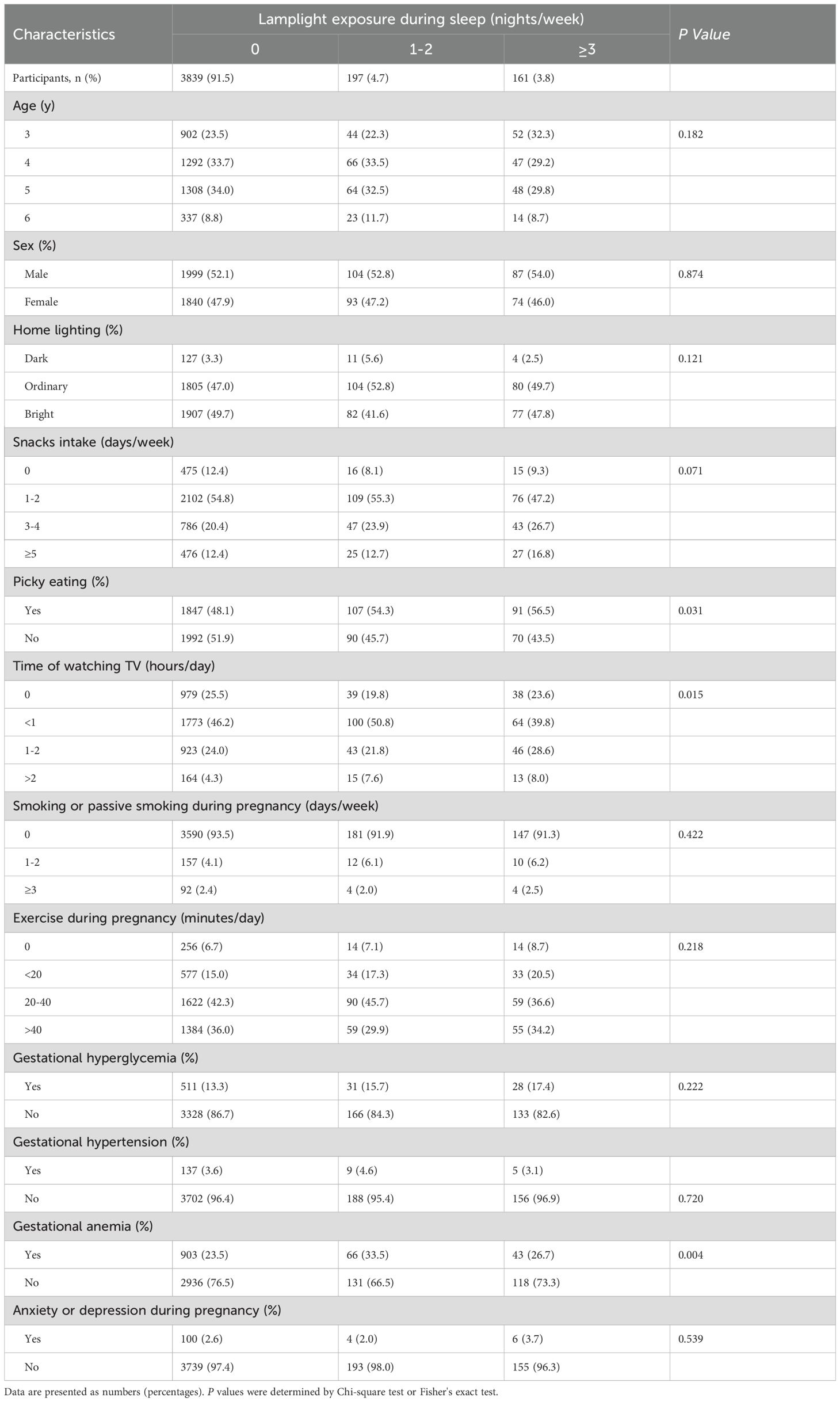
Table 2. Characteristics of the participants according to lamplight exposure during sleep.
As shown in Table 3, compared with the children who slept with the lamplight off, the multivariable adjusted OR was 1.71 (95% CI: 0.92, 3.21) and 3.37 (95% CI: 1.95, 5.82) for those who slept with the lamplight on 1-2 nights/week, and those who slept with the lamplight on ≥3 nights/week, respectively (P-trend <0.001).
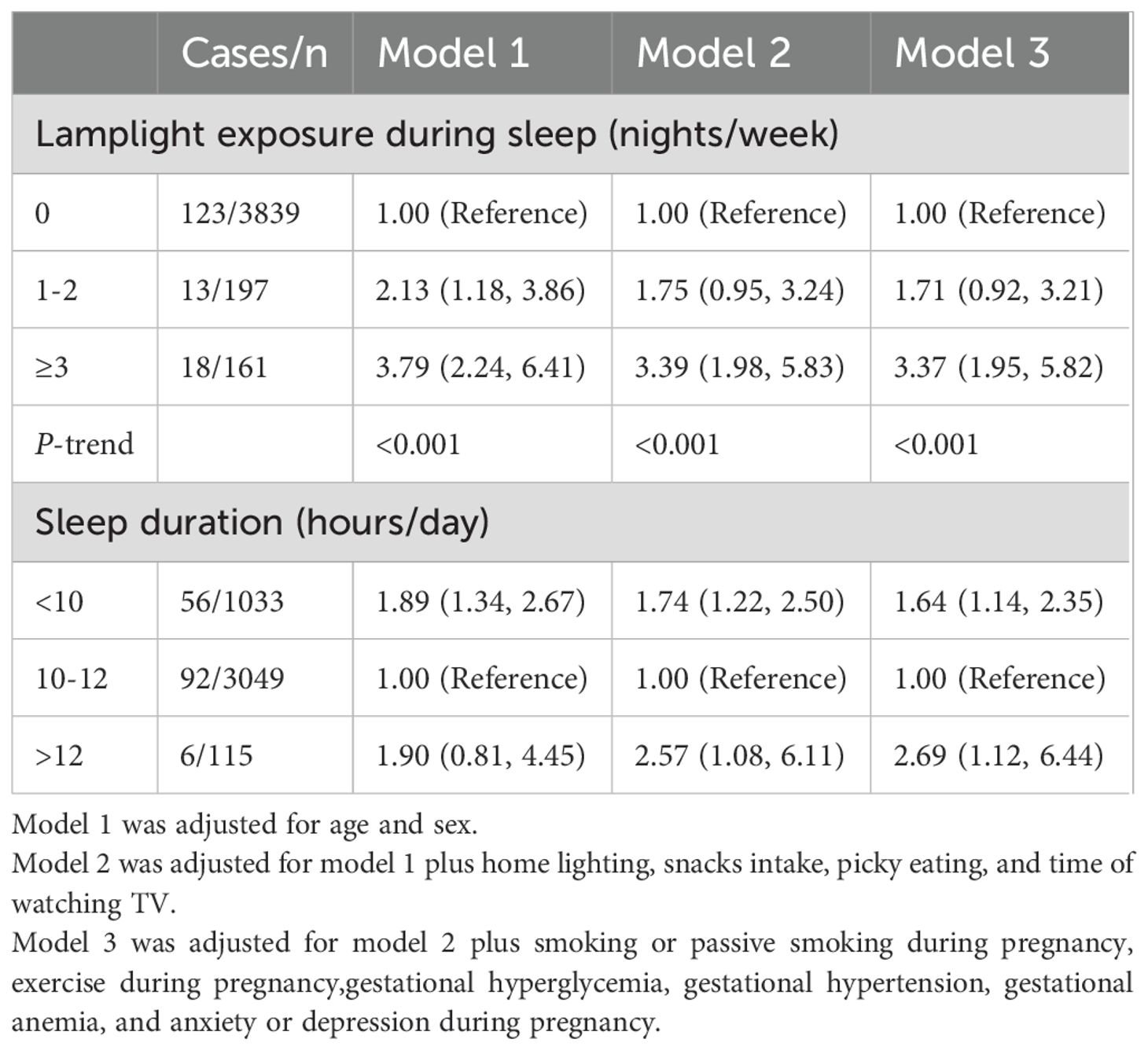
Table 3. ORs (95% CI) for lamplight exposure during sleep and sleep duration in association with ADHD among the preschool children.
Compared with those who slept for 10-12 hours/day, the children who slept less than 10 hours/day had higher odds of ADHD (multivariable-adjusted OR=1.64; 95% CI: 1.14, 2.35), similar with those with sleep duration >12 hours/day (multivariable-adjusted OR=2.69; 95% CI: 1.12, 6.44) (Table 3).
The associations between lamplight exposure during sleep and ADHD were similar in subgroups stratified by sex, picky eating, gestational hyperglycemia, and gestational anemia at baseline (all P-interaction > 0.05) (Figure 1).
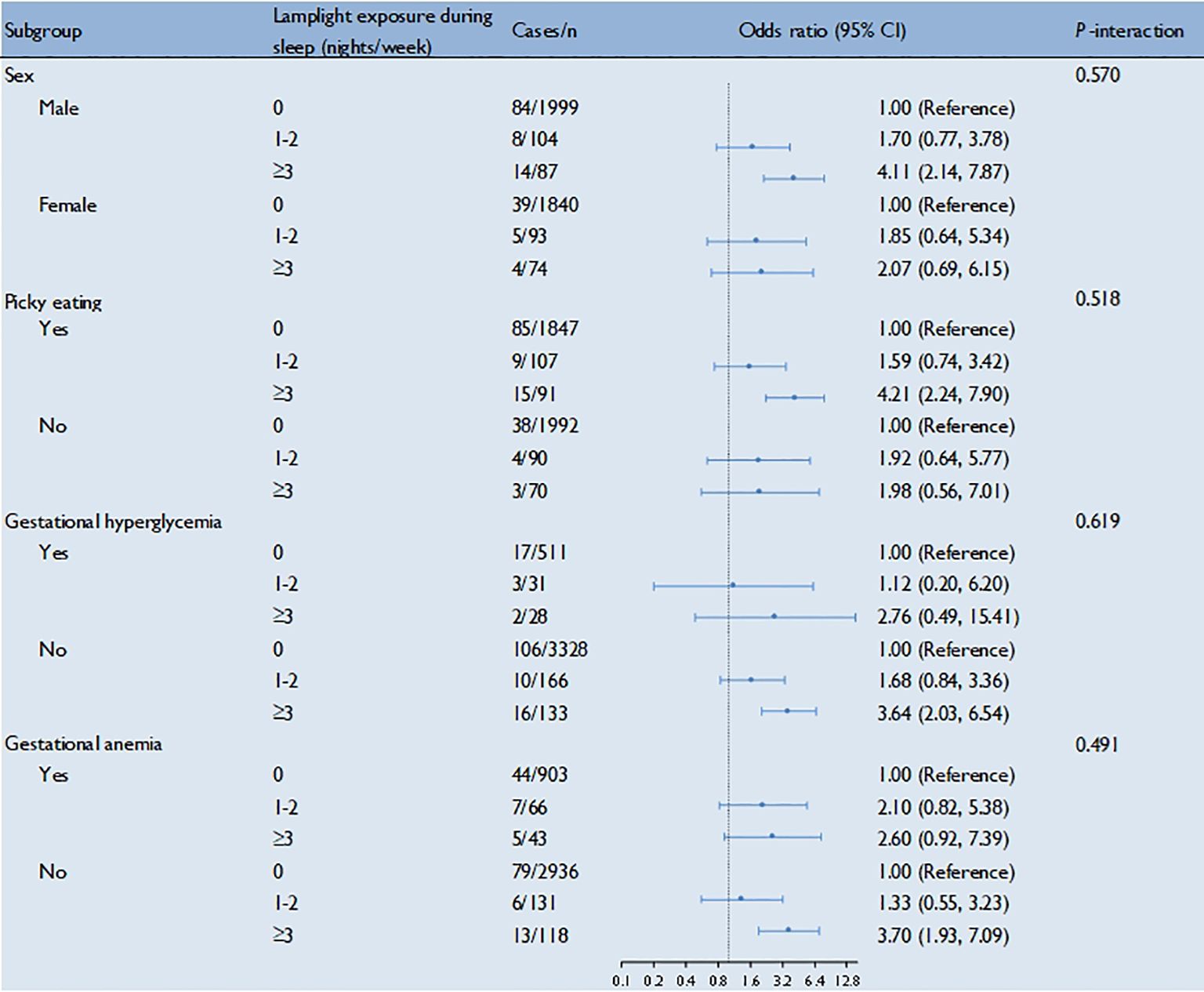
Figure 1. Lamplight exposure during sleep in association with ADHD among the preschool children by strata. Multivariable adjusted model: adjusted for age, sex, home lighting, snacks intake, picky eating, time of watching TV, smoking or passive smoking during pregnancy, exercise during pregnancy, gestational hyperglycemia, gestational hypertension, gestational anemia, and anxiety or depression during pregnancy.
DiscussionPrincipal findingsIn this cross-sectional study, we observed that lamplight exposure during sleep at night was associated with increased odds of ADHD among the preschool children. Moreover, both sleep duration of <10 hours/day and >12 hours/day increased the likelihood of ADHD as well.
Lamplight exposure during sleep at night, sleep duration and ADHDAccumulating evidence supports that exposure to lamplight (indoor and outdoor light) in the evening is related to various adverse health problems including psychobehavioral disorders (21–24). Outdoor light exposure at night was significantly associated with a higher risk of autism spectrum disorder (ASD, a neurodevelopmental disorder) in children (24); nighttime exposure to light could be able to induce neurological changes, mood disorders and depressive-like behaviors (21–24).
In our study, insufficient sleep duration increased odds of ADHD, which was consistent with previous studies (11, 12). Long sleep duration also increased the likelihood of ADHD, which was supported by Bogdan’s findings (13), but inconsistent with Lee’s (17). The inconsistency may come from different study design, screening tools for ADHD, classification of sleep duration, sample size and characteristics of the study populations.
Possible mechanismsThe underlying mechanisms for the association of lamplight exposure during sleep with ADHD remain unclear. However, we proposed several potential explanations.
First, nighttime light can directly affect cognition and mood through intrinsically photosensitive retinal ganglion cells (ipRGC) projections to brain regions involved in emotional regulation (25). Second, nighttime light can indirectly affect mood and behaviors by altering clock and inflammation genes expression, hormone secretion, neuroplasticity and neurotransmission (22). Third, nighttime lamplight is able to disturb the circadian rhythm, inhibit the secretion of melatonin, directly stimulate brain activity (26, 27), and consequently trigger sleep disorders, which have been associated with the risk of ADHD (28, 29). Additionally, studies have demonstrated that light exposure can alter gene expression linked to (neuro)development, including crf, crfbp, mr, and gr-alpha (30). Crf antagonists improved the ability to work memory, the same as all approved ADHD treatments (31). This suggests that nighttime lamplight exposure in preschool children might raise ADHD risk potentially via crf gene regulation.
In this study, we also observed positive associations of both short and long sleep duration with ADHD among the preschool children. Insufficient sleep could damage the prefrontal cortex of the brain and limit the link between the prefrontal cortex and the amygdala (32), thereby affecting cognition, emotion control and executive function (33), which may explain the neurobehavioral, neurocognitive, and functional manifestations of ADHD symptomatology (28). The underlying mechanisms for the association of excessive sleep with ADHD remain unclear, the following mechanism may be involved: excessive sleep may increase arterial stiffness (34), reduce blood flow, and thus adversely affect the nervous system of the children.
Strengths and limitationsTo the best of our knowledge, this is the first study to examine the association between lamplight exposure during sleep and ADHD. Other main strengths include a relatively large sample size and adjustment for a number of confounders in the regression models.
Nevertheless, the study has also several limitations. First, this study was based on a cross-sectional design, therefore causal and temporal relationships could not be inferred. Reverse causality (i.e. ADHD causes sleeping with the light on at night and changed sleeping duration) can not be precluded. Researchers should confirm causality through longitudinal study and experimental study in the future. Second, based on the PSQ scale, preschool children with a hyperactivity index greater than 1.5 were classified as ADHD in this study. This may have resulted in misclassification. To address this limitation, future studies should consider using clinically diagnosed ADHD cases to enhance accuracy. Third, reporting bias and recall bias might have occurred due to self-report by guardians of the children. Future studies should prefer using objective measures (e.g., actigraphy for sleep). Fourth, although we have adjusted for a number of confounders, residual confounding by unknown or unmeasured factors including other sleep disorders cannot be ruled out. For example, children with low socioeconomic status may have a greater likelihood of ADHD (35). A central disorder of hypersomnolence may cause prolonged nighttime sleepiness, and studies have shown that ADHD occurs with a high frequency in adults with this condition (36). Fifth, our study focused on preschool children in Chengdu city, which may have restricted generalizability of the results. Therefore, future studies from different geographic areas or age groups are warranted.
ConclusionsIn the present study, nighttime lamplight exposure was positively associated with ADHD among the preschool children in China. And also, both insufficient and long sleep duration were associated with increased odds of ADHD. Although longitudinal or intervention-based studies are needed, our findings underline the importance of keeping healthy sleep habits for ADHD prevention in children. Specifically, we proposes two recommendations to reduce the risk of ADHD in children. First, the sleep duration of preschool children should be within an appropriate range. Second, it is necessary to provide children a light-free sleep environment by turning off the light, drawing curtains, avoiding electronic screen before bed, and staying away from electronic products.
Data availability statementThe raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statementThe studies involving humans were approved by Ethics Committee of Soochow University (Approval NO. SUDA20210820H01). The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributionsHJ: Writing – original draft, Investigation, Project administration. YB: Data curation, Writing – original draft. YL: Formal analysis, Writing – original draft. HG: Investigation, Writing – original draft. RS: Investigation, Writing – review & editing. ST: Investigation, Writing – original draft. SH: Writing – review & editing. HZ: Conceptualization, Writing – review & editing.
FundingThe author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interestAuthors BY and YL were employed by company Sichuan Bingzhe Technology Co., Ltd.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s noteAll claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary materialThe Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2024.1489229/full#supplementary-material
Supplementary Table 1 | Characteristics of the participants according to different sleep durations.
References2. Thomas R, Sanders S, Doust J, Beller E, Glasziou P. Prevalence of attention-deficit/hyperactivity disorder: a systematic review and meta-analysis. Pediatrics. (2015) 135:e994–1001. doi: 10.1542/peds.2014-3482
PubMed Abstract | Crossref Full Text | Google Scholar
3. Stein MA, Zulauf-McCurdy C, DelRosso LM. Attention deficit hyperactivity disorder medications and sleep. Child Adolesc Psychiatr Clinics. (2022) 31:499–514. doi: 10.1016/j.chc.2022.03.006
PubMed Abstract | Crossref Full Text | Google Scholar
4. Sung V, Hiscock H, Sciberras E, Efron D. Sleep problems in children with attention-deficit/hyperactivity disorder: prevalence and the effect on the child and family. Arch Pediatr Adolesc Med. (2008) 162:336–42. doi: 10.1001/archpedi.162.4.336
PubMed Abstract | Crossref Full Text | Google Scholar
5. Robinson EV, Rogers R. Detection of feigned ADHD across two domains: the MMPI-2-RF and CAARS for faked symptoms and TOVA for simulated attention deficits. J Psychopathol Behav Assess. (2017) 40:376–85. doi: 10.1007/s10862-017-9640-8
Crossref Full Text | Google Scholar
7. Franke B, Faraone SV, Asherson P, Buitelaar J, Bau CH, Ramos-Quiroga JA, et al. The genetics of attention deficit/hyperactivity disorder in adults, a review. Mol Psychiatry. (2012) 17:960–87. doi: 10.1038/mp.2011.138
PubMed Abstract | Crossref Full Text | Google Scholar
8. Johnston C. Parent characteristics and parent-child interactions in families of nonproblem children and ADHD children with higher and lower levels of oppositional-defiant behavior. J Abnormal Child Psychol. (1996) 24:85–104. doi: 10.1007/BF01448375
PubMed Abstract | Crossref Full Text | Google Scholar
10. Touitou Y, Reinberg A, Touitou D. Association between light at night, melatonin secretion, sleep deprivation, and the internal clock: Health impacts and mechanisms of circadian disruption. Life Sci. (2017) 173:94–106. doi: 10.1016/j.lfs.2017.02.008
PubMed Abstract | Crossref Full Text | Google Scholar
11. Gruber R, Michaelsen S, Bergmame L, Frenette S, Bruni O, Fontil L, et al. Short sleep duration is associated with teacher-reported inattention and cognitive problems in healthy school-aged children. Nat Sci Sleep. (2012) 4:33–40. doi: 10.2147/NSS.S24607
PubMed Abstract | Crossref Full Text | Google Scholar
12. Scott N, Blair PS, Emond AM, Fleming PJ, Humphreys JS, Henderson J, et al. Sleep patterns in children with ADHD: a population-based cohort study from birth to 11 years. J Sleep Res. (2013) 22:121–8. doi: 10.1111/j.1365-2869.2012.01054.x
PubMed Abstract | Crossref Full Text | Google Scholar
13. Bogdan AR, Reeves KW. Sleep duration in relation to attention deficit hyperactivity disorder in american adults. Behav Sleep Med. (2018) 16:235–43. doi: 10.1080/15402002.2016.1188391
PubMed Abstract | Crossref Full Text | Google Scholar
14. Lee SH, Kim HB, Lee KW. Association between sleep duration and attention-deficit hyperactivity disorder: A systematic review and meta-analysis of observational studies. J Affect Disord. (2019) 256:62–9. doi: 10.1016/j.jad.2019.05.071
PubMed Abstract | Crossref Full Text | Google Scholar
15. Wynchank D, Ten Have M, Bijlenga D, Penninx BW, Beekman AT, Lamers F, et al. The association between insomnia and sleep duration in adults with attention-deficit hyperactivity disorder: results from a general population study. J Clin Sleep Med. (2018) 14:349–57. doi: 10.5664/jcsm.6976
PubMed Abstract | Crossref Full Text | Google Scholar
16. Hirshkowitz M, Whiton K, Albert SM, Alessi C, Bruni O, DonCarlos L, et al. National Sleep Foundation’s sleep time duration recommendations: methodology and results summary. Sleep Health. (2015) 1:40–3. doi: 10.1016/j.sleh.2014.12.010
PubMed Abstract | Crossref Full Text | Google Scholar
17. Al-Awad AME-H, Sonuga-Barke EJS. The application of the Conners’ Rating Scales to a Sudanese sample: An analysis of parents’ and teachers’ ratings of childhood behaviour problems. Br psychol Soc. (2002) 75:177–87.
PubMed Abstract | Google Scholar
18. Christiansen H, Hirsch O, Drechsler R, Wanderer S, Knospe EL, Günther T, et al. German validation of the conners 3® Rating scales for parents, teachers, and children. Zeitschrift für Kinder-und Jugendpsychiatrie und Psychotherapie. (2016) 44:139. doi: 10.1024/1422-4917/a000408
PubMed Abstract | Crossref Full Text | Google Scholar
19. Fumeaux P, Mercier C, Roche S, Iwaz J, Stéphan P, Revol O. Validation of the french version of conners’ Parent rating scale-revised, short form in ADHD-diagnosed children and comparison with control children. J Atten Disord. (2021) 25:124–33. doi: 10.1177/1087054718763908
PubMed Abstract | Crossref Full Text | Google Scholar
20. Izzo VA, Donati MA, Novello F, Maschietto D, Primi C. The Conners 3-short forms: Evaluating the adequacy of brief versions to assess ADHD symptoms and related problems. Clin Child Psychol Psychiatry. (2019) 24:791–808. doi: 10.1177/1359104519846602
PubMed Abstract | Crossref Full Text | Google Scholar
23. Walker WH 2nd, Borniger JC, Gaudier-Diaz MM, Hecmarie Melendez-Fernandez O, Pascoe JL, Courtney DeVries A, et al. Acute exposure to low-level light at night is sufficient to induce neurological changes and depressive-like behavior. Mol Psychiatry. (2020) 25:1080–93. doi: 10.1038/s41380-019-0430-4
PubMed Abstract | Crossref Full Text | Google Scholar
24. Xie Y, Jin Z, Huang H, Li S, Dong G, Liu Y, et al. Outdoor light at night and autism spectrum disorder in Shanghai, China: A matched case-control study. Sci Total Environ. (2022) 811:152340. doi: 10.1016/j.scitotenv.2021.152340
PubMed Abstract | Crossref Full Text | Google Scholar
25. LeGates TA, Altimus CM, Wang H, Lee HK, Yang S, Zhao H, et al. Aberrant light directly impairs mood and learning through melanopsin-expressing neurons. Nature. (2012) 491:594–8. doi: 10.1038/nature11673
PubMed Abstract | Crossref Full Text | Google Scholar
26. Cajochen C, Munch M, Kobialka S, Krauchi K, Steiner R, Oelhafen P, et al. High sensitivity of human melatonin, alertness, thermoregulation, and heart rate to short wavelength light. J Clin Endocrinol Metab. (2005) 90:1311–6. doi: 10.1210/jc.2004-0957
PubMed Abstract | Crossref Full Text | Google Scholar
27. Kim M, Subramanian M, Cho YH, Kim GH, Lee E, Park JJ. Short-term exposure to dim light at night disrupts rhythmic behaviors and causes neurodegeneration in fly models of tauopathy and Alzheimer’s disease. Biochem Biophys Res Commun. (2018) 495:1722–9. doi: 10.1016/j.bbrc.2017.12.021
PubMed Abstract | Crossref Full Text | Google Scholar
28. Carpena MX, Munhoz TN, Xavier MO, Rohde LA, Santos IS, Del-Ponte B, et al. The role of sleep duration and sleep problems during childhood in the development of ADHD in adolescence: findings from a population-based birth cohort. J Atten Disord. (2020) 24:590–600. doi: 10.1177/1087054719879500
PubMed Abstract | Crossref Full Text | Google Scholar
29. Gahan Fallone P, Christine Acebo P, Ronald Seifer P, Mary A. Carskadon P. Experimental restriction of sleep opportunity in children: effects on teacher ratings. Sleep. (2005) 28:1561–7. doi: 10.1093/sleep/28.12.1561
PubMed Abstract | Crossref Full Text | Google Scholar
30. van den Bos R, Zethof J, Flik G, Gorissen M. Light regimes differentially affect baseline transcript abundance of stress-axis and (neuro) development-related genes in zebrafish (Danio rerio, Hamilton 1822) AB and TL larvae. Biol Open. (2017) 6:1692–7. doi: 10.1242/bio.028969
PubMed Abstract | Crossref Full Text | Google Scholar
31. Hupalo S, Berridge CW. Working memory impairing actions of corticotropin-releasing factor (CRF) neurotransmission in the prefrontal cortex. Neuropsychopharmacology. (2016) 41:2733–40. doi: 10.1038/npp.2016.85
PubMed Abstract | Crossref Full Text | Google Scholar
32. Horne JA. Human sleep, sleep loss and behaviour. Implications for the prefrontal cortex and psychiatric disorder. Br J Psychiatry. (1993) 162:413–9. doi: 10.1192/bjp.162.3.413
PubMed Abstract | Crossref Full Text | Google Scholar
34. Yoshioka E, Saijo Y, Kita T, Okada E, Satoh H, Kawaharada M, et al. Relation between self-reported sleep duration and arterial stiffness: a cross-sectional study of middle-aged Japanese civil servants. Sleep. (2011) 34:1681–6. doi: 10.5665/sleep.1434
PubMed Abstract | Crossref Full Text | Google Scholar
35. Fan L, Qing W, Wang Y, Zhan M. Family socioeconomic status and attention deficit/hyperactivity disorder in preschool children: The mediating role of executive function. Int J Environ Res Public Health. (2022) 19:11608. doi: 10.3390/ijerph191811608
PubMed Abstract | Crossref Full Text | Google Scholar
36. Lopez R, Micoulaud-Franchi JA, Camodeca L, Gachet M, Jaussent I, Dauvilliers Y. Association of inattention, hyperactivity, and hypersomnolence in two clinic-based adult cohorts. J attention Disord. (2020) 24:555–64. doi: 10.1177/1087054718775826
留言 (0)