Intertrochanteric Fracture (ITF) commonly occurs in elderly patients, with a high incidence rate of approximately 3.4% (1). In elderly patients, these fractures are often comminuted and unstable, and are frequently accompanied by osteoporosis, hypertension, diabetes, and cardiovascular diseases, resulting in poor physical function. With the aging global population, the incidence of unstable intertrochanteric fractures is expected to increase annually (2). The goal of surgical treatment for elderly patients with intertrochanteric fractures is to restore the hip structure, stabilize the fracture, and allow early mobilization, thereby preventing complications such as bedsores, infections, and deep vein thrombosis of the lower limbs caused by prolonged bed rest, as well as preventing the exacerbation of underlying diseases and reducing mortality (3).
Regarding the treatment of Type IV ITF, some scholars advocate the use of Proximal Femoral Nail Antirotation (PFNA) (4, 5). However, in elderly patients, PFNA is associated with a high incidence of complications such as fracture displacement, femoral neck screw cut-out, and hip varus deformity postoperatively (6, 7). Consequently, some scholars propose total hip arthroplasty (THA) as an alternative, as it can reconstruct the hip structure and allow for early mobilization, avoiding complications associated with PFNA. Currently, there is still controversy regarding the optimal surgical approach for patients over 65 years old with Evans-Jensen Type IV intertrochanteric fractures (8).
Through a literature review, we found that there is no specific study focusing on the best surgical method for this particular patient group. This study aims to retrospectively compare the differences between the two surgical approaches in terms of perioperative outcomes, hip function, quality of life, and postoperative complications in patients over 65 with Evans-Jensen Type IV ITF, providing a reference for the selection of surgical methods in clinical practice for elderly patients with Evans-Jensen Type IV ITF.
MethodsA retrospective analysis was conducted on 40 patients aged 65 and older with intertrochanteric fractures (ITF) admitted to the Affiliated Central Hospital of Shenyang Medical College between 2020 and 2023. A total of 20 patients who underwent hip replacement surgery were included in the THA group. Another 20 patients with the same fracture type who were treated with PFNA served as the control group, defined as the PFNA group. All patients were informed of the differences between PFNA and THA treatment options and chose the surgical method based on their personal preferences.
Inclusion criteriaPatients over 65 years old with newly diagnosed closed fractures, Evans-Jensen Type IV fractures, and who met the surgical indications for PFNA or THA.
Exclusion criteriaPatients with pathological fractures, those unable to undergo surgery due to severe medical conditions, patients who were lost to follow-up, and patients whose postoperative limb function assessment was affected by other diseases.
Ethical approvalThis study was approved by the Medical Ethics Committee of the Affiliated Central Hospital of Shenyang Medical College, and informed consent was obtained from all patients and their families.
Preoperative patient preparation and managementAfter admission, patients received skin traction on the affected limb, swelling reduction, pain relief, and treatment to prevent deep vein thrombosis of the lower limbs. Preoperative examinations were completed. All patients underwent preoperative hip x-rays (Philips Digital Radiography System, Netherlands) and CT scans of the affected hip with three-dimensional reconstruction (Philips 256-slice spiral CT scanner, Netherlands, with a slice thickness of 0.6 mm).
Surgical methods and brief procedure AnesthesiaThe anesthesia method used was either spinal anesthesia or general anesthesia.
PFNA groupThe patient was placed in a supine position, with the affected limb fixed on the traction table. Under fluoroscopy, a closed reduction of the fracture ends was performed. A longitudinal incision was made approximately 3 cm above the greater trochanter, followed by layer-by-layer dissection to expose the greater trochanter. The main femoral nail, femoral neck helical screws, and distal locking screws were inserted under fluoroscopy, paying attention to the anteversion angle and tip distance. Finally, the proximal intramedullary nail cap was screwed in. Muscle contraction exercises began the day after surgery, and monthly follow-up hip x-rays were performed to determine the time for mobilization and weight-bearing based on fracture healing.
THA groupThe patient was positioned on the side of the unaffected limb, and a lateral approach to the hip joint was used. Part of the external rotator muscle group was cut at the insertion point of the greater trochanter, while preserving the piriformis muscle and as much of the medial femoral distance as possible. A suitably sized acetabular cup and liner were installed, taking care to ensure proper abduction and anteversion angles. The lesser trochanter fracture was reduced and fixed, and a titanium cable was used to bundle the proximal femur to prevent fracture during the insertion of the femoral prosthesis. A properly sized Wagner femoral stem was implanted, ensuring the anteversion angle was correct and that both lower limbs were of equal length. The greater trochanter fracture fragments were reduced and fixed with a tension band. Postoperatively, functional exercises were initiated based on the patient's condition, with the gradual introduction of weight-bearing practice using assistive devices as needed (Figure 1).
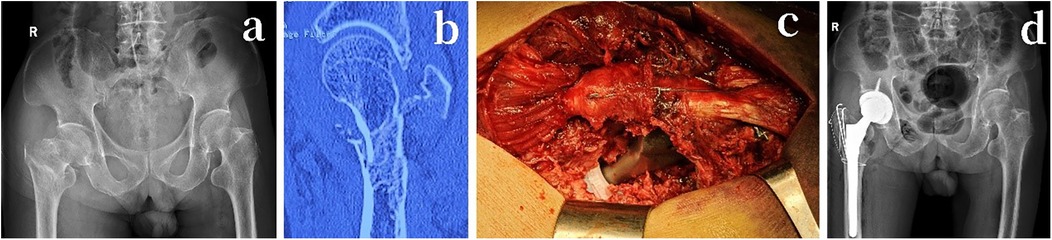
Figure 1. An 78-year-old male patient with a right-sided Evans-Jensen type IV intertrochanteric femur fracture due to a fall. (a) Preoperative anteroposterior x-ray of both hip joints. (b) Preoperative coronal CT scan. (c) Intraoperative total hip arthroplasty, with the use of Kirschner wires for tension band fixation of the greater trochanter and titanium cables for securing the proximal femur. (d) Postoperative anteroposterior x-ray of both hip joints on the first day after surgery.
Postoperative managementPostoperatively, active treatment of underlying diseases continued, along with infection prevention and prevention of deep vein thrombosis in the lower limbs. Preoperative x-rays (Figure 1a), preoperative CT scans (Figure 1b), and postoperative x-rays taken on the first day (Figure 1d) were retained to compare and evaluate the surgical outcomes.
After the patient recovered from anesthesia, they were guided to perform ankle pump exercises, along with contraction and relaxation exercises for the knee and hip muscles. Patients in the hip replacement group were instructed to begin walking exercises with the assistance of a walker as early as possible. In the PFNA group, patients were advised to perform appropriate ankle pump and muscle contraction exercises while in bed. Follow-up x-rays of both hips were performed at 1, 2, and 3 months to assess hip recovery and fracture healing, and to guide patients on postoperative rehabilitation exercises and full weight-bearing activities. x-rays of both hips may be reviewed at 6 and 12 months postoperatively as needed to evaluate the recovery status of the fracture.
Clinical efficacy evaluation indicatorsFollow-up was conducted primarily through telephone and outpatient visits at 1 month, 3 months, and 6 months postoperatively. During the follow-up, patient scoring surveys were conducted, imaging examinations were completed, and relevant data were collected.
1. Recording surgical and rehabilitation data:
Surgical duration: Time from skin incision to skin closure;
Intraoperative blood loss: Volume of blood collected in the suction device and gauze;
Time to first postoperative ambulation (T1) and time to full weight-bearing on the affected limb (T2).
2. Functional assessment:
Postoperative Harris hip scores and excellent rates for the affected hip were evaluated at 1 month, 3 months, and 6 months for both groups;
Excellent: 90–100 points, Good: 80–89 points, Fair: 70–79 points, Poor: below 70 points (9).
3. SF-36 Quality of Life Questionnaire (10):
The SF-36 consists of 36 items and is a brief survey designed to assess health and functional status across various age groups, different diseases, and control populations.
It includes 8 dimensions: physical functioning, role physical, bodily pain, general health, social functioning, role emotional, and mental health. The total score across these dimensions represents the overall score of the questionnaire.
4. Postoperative complications:
Includes infections, internal fixation failure, hip dislocation, etc.
Statistical analysisAll analyses were conducted using SPSS 26.0 software (IBM, Armonk, NY, USA). Categorical variables were presented as numbers or percentages. Continuous variables were expressed as means ± standard deviation. Categorical variables were evaluated using Fisher's exact test. The Shapiro-Wilk test was used to determine whether continuous variables followed a normal distribution; continuous variables that were normally distributed were analyzed using independent samples t-tests. The significance level for all statistical tests was set at p < 0.05.
Results Baseline and surgical data, including age, sex, surgical time, and intraoperative blood loss, were collectedA total of 40 patients with Type IV ITF were included, with 20 patients in the PFNA group (4 males, 16 females) and an average age of 72.8 ± 5.2 years. The THA group also had 20 patients (6 males, 14 females) with an average age of 73.7 ± 5.5 years. There were no statistically significant differences in age or sex between the two groups (p > 0.05) (Table 1).
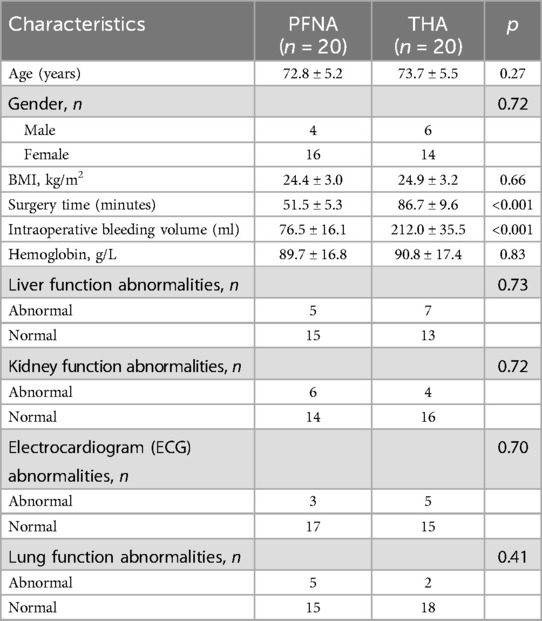
Table 1. Baseline and surgical data.
The PFNA group had a shorter surgical time (51.5 ± 5.3 vs. 86.7 ± 9.6 min, p < 0.001), and the intraoperative blood loss was less in the PFNA group (76.5 ± 16.1 vs. 212.0 ± 35.5 ml, p < 0.001). The differences were statistically significant (Table 1).
Functional scores and prognosis assessmentThe THA group demonstrated an earlier time to first mobilization (3.1 ± 1.4 vs. 43.3 ± 13.09 days, p < 0.001) and an earlier time to full weight-bearing on the affected limb (33.5 ± 3.1 vs. 77.9 ± 12.0 days, p < 0.001). These differences were statistically significant.
In follow-up evaluations at 1, 3, and 6 months postoperatively, the Harris scores showed that the excellent/good rate in the PFNA group was 10%, 55%, and 55%, respectively, while the THA group had rates of 70%, 85%, and 90%. The hip function scores in the THA group were significantly higher than those in the PFNA group (1st month p < 0.001, 3rd month p = 0.04, 6th month p = 0.02).
For the SF-36 scale, the THA group scored higher than the PFNA group at all time points: 1 month (75.1 ± 4.0 vs. 66.1 ± 8.0, p < 0.001), 3 months (82.3 ± 3.7 vs. 79.4 ± 4.8, p = 0.04), and 6 months (88.7 ± 2.8 vs. 85.5 ± 2.6, p = 0.001). All differences were statistically significant (Table 2).
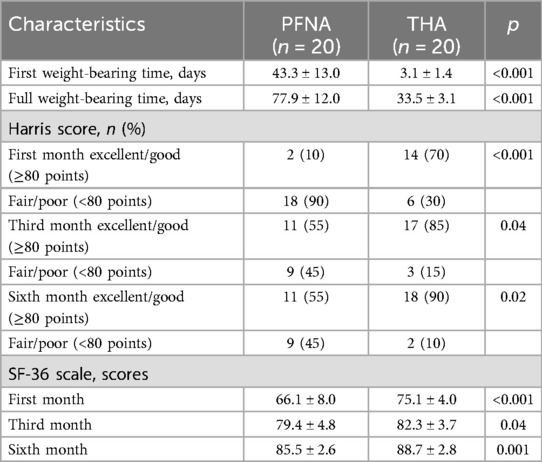
Table 2. Functional scores and prognostic indicators.

Table 3. Postoperative complications statistics for two groups of patients (n = 20).
Postoperative complicationsThe PFNA group had more postoperative complications, with a total of 5 cases, including: 2 cases of pulmonary infection, both cured after anti-infective treatment in the respiratory department. 2 cases of screw cut-out at the femoral head, both of which required a second-stage total hip replacement (Figure 2). 1 case of screw cut-out at the femoral neck, considered to be due to improper screw placement, which was treated with revision surgery and repositioning of the screw.
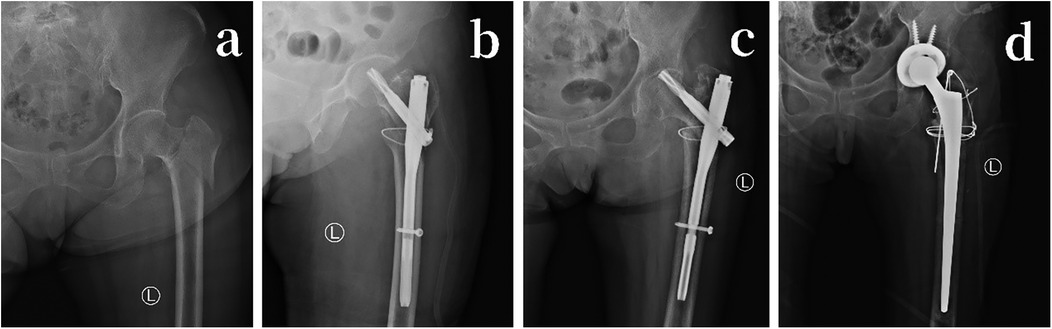
Figure 2. (a) 73-year-old female with a fall-induced intertrochanteric fracture of the left femur. (a) Preoperative anteroposterior x-ray of the left hip joint. (b) Postoperative first-day anteroposterior x-ray of the left hip joint, using PFNA internal fixation with external lateral wall bundling with titanium cables. (c) Postoperative 5-month anteroposterior x-ray of the left hip joint, showing proximal screw cutting of PFNA. (d) Removal of PFNA internal fixation, followed by total hip joint replacement surgery; postoperative first-day anteroposterior x-ray of the left hip joint.
In the THA group, there were 2 postoperative complications: 1 case of hip dislocation, which occurred in a patient with cerebral atrophy due to excessive hip flexion postoperatively. This was treated with closed reduction.1 case of limb length discrepancy, where the affected limb was 1.6 cm longer than the healthy side. Since there was no significant limping, no further intervention was required (Table 3).
DiscussionElderly patients with intertrochanteric fractures (ITF) who have uncontrolled underlying medical conditions generally have poor overall health, making them unable to tolerate anesthesia and surgery, thus necessitating conservative treatment. However, the mortality rate for conservative treatment within one year can be as high as 84.4% (11). With advancements in medical technology and the introduction and application of Enhanced Recovery After Surgery (ERAS) principles (12), surgical treatment opportunities for elderly ITF patients have significantly increased, and surgery has become the primary treatment method for this injury (13).
Intramedullary fixation and total hip arthroplasty (THA) are currently the mainstream surgical methods for treating type IV ITF. However, there are several contentious points (14–17): Performing PFNA on unstable fractures can present challenges with preoperative reduction, and it is often difficult to effectively stabilize fragmented bone during surgery. This results in a high incidence of postoperative internal fixation failure (18, 19), which adversely affects fracture healing, and revision surgeries can cause additional trauma (20). Patients with associated lateral wall deficiencies often require additional internal fixation treatments, such as greater trochanteric plating. THA carries the risk of intraoperative vascular and sciatic nerve injuries, significant blood loss, and severe damage to the surrounding structures of the hip. There is also a risk of femoral fracture during the procedure, and if bone cement is used during surgery, there is a possibility of cement-related complications (21). Furthermore, there is ongoing debate regarding the choice of prosthesis type during the surgery.
In this study, the SF-36 scores, Harris scores, and excellent rates at each follow-up stage for the THA group were all higher than those for the PFNA group. Possible reasons for this include: THA can prevent discomfort caused by the wear of the metal femoral head against the bony structure of the acetabulum; the surgery preserves the piriformis and part of the external rotator muscles, which is crucial as patients often present with greater trochanter fractures and displacements, thus increasing the likelihood of successfully retaining these external rotator muscles; intraoperatively suturing and repairing torn or incised joint capsules effectively reduces trauma, restores hip structure, and lowers the risk of postoperative hip dislocation (22). Additionally, using titanium cables to bundle the proximal femur before inserting the femoral prosthesis can prevent femoral fracture; employing titanium cables to stabilize the lesser trochanter fracture and using K-wires and steel wires in a tension band configuration to stabilize the greater trochanter fracture effectively restores and stabilizes the fractures, restoring the hip musculature and bony structure.
The use of the Wagner SL biological femoral stem in this study offers several advantages (23): the stability of the SL stem relies on the mid- to distal femur, providing a stable biomechanical structure for the hip postoperatively; the anteversion angle can be freely adjusted during the procedure to prevent postoperative hip dislocation; and the femoral side is shaped by drilling into the medullary cavity, which avoids stress concentration and reduces the risk of femoral fracture. In the PFNA group, the internal fixation method only involved three screws of varying lengths, while the proximal structure in IV-type ITF is compromised, leading to instability in the fixation of both the greater and lesser trochanters. During postoperative activities, the iliopsoas and gluteal muscles can exert strong traction on the fractured fragments, resulting in significant pain; early weight-bearing can also increase the risk of internal fixation failure and the occurrence of hip internal rotation (especially in type IV fractures). Therefore, clinicians often determine the timing for full weight-bearing based on the healing progress of the fracture in PFNA patients. Consequently, the THA group achieved early rehabilitation and weight-bearing, which is beneficial for the recovery of cardiopulmonary function and the function of the affected hip joint.
Our research team believes that for patients over 65 years old with multiple underlying diseases and severe osteoporosis suffering from Evans-Jensen type IV intertrochanteric fractures, Wagner SL biological stem total hip arthroplasty (THA) is the recommended first-choice treatment. Intraoperative injection of a “cocktail mix of analgesics” significantly reduces early postoperative pain (24). Additionally, the preoperative and intraoperative use of tranexamic acid (25) effectively reduces intraoperative blood loss, avoiding the need for blood transfusion.
Although total hip arthroplasty involves significant surgical trauma, may lead to postoperative limb length discrepancies, and has limitations regarding the lifespan of the prosthesis, considering the patients' age and health status, THA remains the superior choice. For patients with Evans-Jensen type IV intertrochanteric fractures, while proximal femoral nail anti-rotation (PFNA) treatment aligns with modern minimally invasive surgical principles, it carries a high risk of screw cut-out (incidence rate of 15%, i.e., 3 out of 20 cases), which may necessitate secondary surgery. Moreover, due to the requirement for postoperative bed rest, factors such as pain and infection increase the likelihood of cardiopulmonary function deterioration. For elderly patients, these issues can further impact survival rates. Therefore, we recommend prioritizing total hip arthroplasty (THA) for this specific patient population to reduce the incidence of secondary surgeries, lower the risk of postoperative complications, promote early rehabilitation and recovery, improve patients' quality of life, and ultimately enhance survival rates. Although extramedullary fixation and conservative treatment are alternative options, we do not recommend them as first-line treatments for elderly patients with intertrochanteric fractures.
This study has certain limitations. Firstly, it is a retrospective and non-randomized study. Secondly, all surgeries were performed by the same research team, and the clinical outcomes may vary due to differences in the surgeons' individual experience. Future studies could consider incorporating computer-assisted robotic surgery to address this limitation. Lastly, this research represents an initial study, and the relatively small sample size may affect the accuracy of the experimental results. Further multi-center, large-sample, and long-term follow-up studies are needed to validate our conclusions.
ConclusionFor patients aged 65 and older with Evans-Jensen IV-type intertrochanteric fractures, especially those with comorbidities who cannot tolerate prolonged bed rest, hip arthroplasty should be considered as a treatment option. This approach allows patients to engage in rehabilitation exercises earlier after surgery, prevents the exacerbation of underlying medical conditions, and facilitates faster recovery of hip function on the affected side, leading to improved quality of life for the patients.
Data availability statementThe original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Ethics statementThe studies involving humans were approved by Ethics Committee of the Central Hospital Affiliated to Shenyang Medical College. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributionsZ-CC: Data curation, Funding acquisition, Project administration, Supervision, Writing – review & editing. MS: Data curation, Investigation, Project administration, Writing – original draft. H-RL: Investigation, Methodology, Software, Validation, Writing – original draft. HZ: Data curation, Investigation, Validation, Writing – original draft. TB: Data curation, Investigation, Writing – original draft. R-DX: Data curation, Investigation, Writing – original draft. S-YD: Data curation, Investigation, Writing – original draft.
FundingThe author(s) declare financial support was received for the research, authorship, and/or publication of this article. This study was supported by Natural Science Foundation of Liaoning Province (Grant no. 2024-MS-222), Liaoning Provincial Department of Education Fund Project (JYTMS20231396) and the Science and Technology Plan Project of Shenyang City (Grant no. 22-321-32-13).
AcknowledgmentsWe thank the patient for the participation and cooperation. This study obtained ethical approval from the Ethics Committee of Shenyang Medical College Affiliated Central Hospital.
Conflict of interestThe authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statementThe author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher's noteAll claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References1. Liu P, Jin D, Zhang C, Gao Y. Revision surgery due to failed internal fixation of intertrochanteric femoral fracture: current state-of-the-art. BMC Musculoskelet Disord. (2020) 21(1):573. doi: 10.1186/s12891-020-03593-8
PubMed Abstract | Crossref Full Text | Google Scholar
2. Soylemez MS, Uygur E, Poyanli O. Effectiveness of distally slotted proximal femoral nails on prevention of femur fractures during and after intertrochanteric femur fracture surgery. Injury. (2019) 50(11):2022–9. doi: 10.1016/j.injury.2019.07.022
PubMed Abstract | Crossref Full Text | Google Scholar
3. Kim H, Won D, Chang JE, Lee JM, Ryu JH, Min SW, et al. Ultrasound assessment of the anatomic landmarks for spinal anesthesia in elderly patients with hip fracture: a prospective observational study. Medicine (Baltimore). (2019) 98(27):e16388. doi: 10.1097/MD.0000000000016388
PubMed Abstract | Crossref Full Text | Google Scholar
4. Söylemez MS, Fidan F, Polat A, Kazdal C, Kurtan A. Proximal femoral lateral locking plate versus short cephalomedullary nails for treating AO/OTA 31 A3 intertrochanteric femoral fractures: a retrospective clinical study. Acta Chir Orthop Traumatol Cech. (2021) 88(3):196–203. doi: 10.55095/achot2021/031
Crossref Full Text | Google Scholar
5. Wang R, Zhang H, Wei Q, Ding C, Cao L, Yi M, et al. Intramedullary nails in combination with reconstruction plate in the treatment of unstable intertrochanteric femoral fractures with lateral wall damage. Int Orthop. (2021) 45(11):2955–62. doi: 10.1007/s00264-021-05004-6
PubMed Abstract | Crossref Full Text | Google Scholar
6. Nie B, Wu D, Yang Z, Liu Q. Comparison of intramedullary fixation and arthroplasty for the treatment of intertrochanteric hip fractures in the elderly: a meta-analysis. Medicine (Baltimore). (2017) 96(27):e7446. doi: 10.1097/MD.0000000000007446
PubMed Abstract | Crossref Full Text | Google Scholar
7. Ren H, Ao R, Wu L, Jian Z, Jiang X, Yu B. Effect of lesser tro-chanter posteromedial wall defect on the stability of femo-ralintertrochateric fracture using 3D simulation. J Orthop Surg Res. (2020) 15(1):242. doi: 10.1186/s13018-020-01763-x
PubMed Abstract | Crossref Full Text | Google Scholar
8. Jianfeng Q, Dazhi W, Xin M, Chen J. Therapeutic effect of artificial femoral head replacement and proximal femoral nail antirotation on elderly unstable intertrochanteric fractures. Int J Clin Med. (2020) 11(04):135–43. doi: 10.4236/ijcm.2020.114014
Crossref Full Text | Google Scholar
9. Yapici F, Ucpunar H, Camurcu Y, Emirhan N, Tanoglu O, Tardus I. Clinical and radiological outcomes of patients treated with the talon distal fixproximal femoral nail for intertrochanteric femur fractures. Injury. (2020) 51(4):1045–50. doi: 10.1016/j.injury.2020.03.006
PubMed Abstract | Crossref Full Text | Google Scholar
10. McHorney CA, Ware JE Jr, Raczek AE. The MOS36-item short-form health survey (SF-36): II. Psychometric and clinical tests of validity in measuring physical and mental health constructs. Med Care. (1993) 31(3):247–63. doi: 10.1097/00005650-199303000-00006
PubMed Abstract | Crossref Full Text | Google Scholar
11. Chlebeck JD, Birch CE, Blankstein M, Kristiansen T, Bartlett CS, Schottel PC. Nonoperative geriatric hip fracture treatment associated with increased mortality: a matched cohort study. J Orthop Trauma. (2019) 33(7):346–50. doi: 10.1097/BOT.0000000000001460
PubMed Abstract | Crossref Full Text | Google Scholar
12. Auyong DB, Allen CJ, Pahang JA, Clabeaux JJ, MacDonald KM, Hanson NA. Reduced length of hospitalization in primary total knee arthroplasty patients using an update enhanced recovery after orthopedic surgery (ERAS)pathway. J Arthroplasty. (2015) 30(10):1705–9. doi: 10.1016/j.arth.2015.05.007
PubMed Abstract | Crossref Full Text | Google Scholar
13. Oc Y, Varol A, Yazar EA, Ak S, Akpolat AO, Kilinc BE. Treatment strategy for elderly patients with the isolated greater trochanteric fracture. SAGE Open Med. (2020) 8:2050312120964138. doi: 10.1177/2050312120964138
PubMed Abstract | Crossref Full Text | Google Scholar
14. Iwata H, Takada N, Kuroyanagi G, Ikuta K, Usami T, Sekiya I, et al. Effect of hydroxyapatite tubes on the lag screw intraoperative insertion torque for the treatment of intertrochanteric femoral fractures. Injury. (2021) 52(11):3377–81. doi: 10.1016/j.injury.2021.07.032
PubMed Abstract | Crossref Full Text | Google Scholar
15. Moon NH, Shin WC, Kim JS, Woo SH, Son SM, Suh KT. Cementless total hip arthroplasty following failed internal fixation for femoral neck and intertrochanteric fractures: a comparative study with 3–13 years’ follow–up of 96 consecutive patients. Injury. (2019) 50(3):713–9. doi: 10.1016/j.injury.2019.01.018
PubMed Abstract | Crossref Full Text | Google Scholar
16. Imerci A, Aydogan NH, Tosun K. The effect on outcomes of the application if circumferential cerclage cable following in treamedullary nailing in reverse intertrochanteric femoral fractures. Eur J Orthop Surg Traumatol. (2019) 29(4):835–42. doi: 10.1007/s00590-018-2356-y
PubMed Abstract | Crossref Full Text | Google Scholar
17. Polat G, Akgül T, Ekinci M, Bayram S. A biomechanical comparison of three fixation techniques in osteoporotic reverse oblique intertrochanteric femur fracture with fragmented lateral cortex. Eur J Trauma Emerg Surg. (2019) 45(3):499–505. doi: 10.1007/s00068-018-1061-1
PubMed Abstract | Crossref Full Text | Google Scholar
18. Hao Y, Zhang Z, Zhou F, Ji H, Tian Y, Guo Y, et al. Risk factors for implant failure in reverse oblique and transverse intertrochanteric fractures treated with proximal femoral nail antirotation (PFNA). J Orthop Surg Res. (2019) 14(1):350. doi: 10.1186/s13018-019-1414-4
PubMed Abstract | Crossref Full Text | Google Scholar
19. Ling L, Qu Z, Zhou K. Effect of fracture reduction with different medial cortical support on stability after cephalomedullary nail fixation of unstable pertrochanteric fractures: a biomechanical analysis. Indian J Orthop. (2021) 56(1):34–40. doi: 10.1007/s43465-021-00443-0
PubMed Abstract | Crossref Full Text | Google Scholar
20. Zheng L, Wong DW, Chen X, Chen Y, Li P. Risk of proximal femoral nail antirotation (PFNA) implant failure upon different lateral femoral wall thickness in intertrochanteric fracture: a finite element analysis. Comput Methods Biomech Biomed Engin. (2022) 25(5):512–20. doi: 10.1080/10255842.2021.1964488
PubMed Abstract | Crossref Full Text | Google Scholar
21. Nakada TA, Oda S, Matsuda K, Sadahiro T, Nakamura M, Abe R, et al. Continuous hemodiafiltration with PMMA hemofilter in the treatment of patients with septic shock. Mol Med. (2008) 14(5–6):257–63. doi: 10.2119/2007-00108.Nakada
PubMed Abstract | Crossref Full Text | Google Scholar
22. Kanda A, Kaneko K, Obayashi O, Mogami A, Morohashi I. Preservation of the articular capsule and short lateral rotator in direct anterior approach to total hip arthroplasty. Eur J Orthop Surg Traumatol. (2018) 28(6):1111–6. doi: 10.1007/s00590-018-2166-2
PubMed Abstract | Crossref Full Text | Google Scholar
23. Böhm P, Bischel O. The use of tapered stems for femoral revision surgery. Clin Orthop Relat Res. (2004) 420:148–59. doi: 10.1097/00003086-200403000-00021
Crossref Full Text | Google Scholar
24. Lunn TH, Husted H, Solgaard S, Kristensen BB, Otte KS, Kjersgaard AG, et al. Intraoperative local infiltration analgesia for early analgesia after total hip arthroplasty: a randomized, double-blind, placebo-controlled trial. Reg Anesth Pain Med. (2011) 36(5):424–9. doi: 10.1097/AAP.0b013e3182186866
PubMed Abstract | Crossref Full Text | Google Scholar
25. Colomina MJ, Contreras L, Guilabert P, Koo M, M Ndez E, Sabate A. Clinical use of tranexamic acid: evidences and controversies. Braz J Anesthesiol. (2022) 72(6):795–812. doi: 10.1016/j.bjane.2021.08.022
留言 (0)