Over the last decade, competence-based medical education (CBME) has been advocated in medical teaching that accentuates medical knowledge, interpersonal and communication skills, and professional identity (1). Despite emphasis on ‘student-centered’ education, undergraduate medical students, unlike medical residents, often find themselves in passive, observational roles during clinical rotations. As a result, students have limited opportunities to reflect on their professional identity as future doctors and may later struggle to interact effectively with patients (2). This limited engagement can hinder the development of critical reflection, a cornerstone of effective medical practice. Critical reflection (3, 4) is a central tenet of good medical practice and should be cultivated early in medical students’ training for their careers. Most students report the desire to be supervised by their tutors during consultations or clinical examinations with autonomy and protection (5). To address this gap, there is a growing need for educational environments that provide students with active learning opportunities, allowing them to integrate theoretical knowledge with practical skills in a real-world context.
Teaching at the bedside or outpatient clinics is at the heart of medical education and provides essential clinical training (6). Compared to inpatient clinical work, outpatient clinical work is less time-consuming but provides different and unique opportunities to listen to and examine patients including their ideas, concerns and expectations. Thus, teaching in a clinic is an essential and irreplaceable part of education for medical students (7).
A supervised teaching clinic (STC) represents a strategic approach to fostering such a safe and supportive environment, particularly within the outpatient setting. Rather than the routine clinic shadowing, an STC is defined as a student-led consultation of real patients under the supervision of experienced tutors. This approach ensures that patients’ rights are always respected during teaching and learning activities.
This study evaluates the implementation of an STC within a gynecological clinic, focusing on its effectiveness in enhancing students’ clinical competencies and professional development. The analysis is framed around three key dimensions: goal direction, relationships, and supporting services, which are critical to creating a conducive learning environment.
2 Materials and methods 2.1 Routine gynecology clinic rotationThis study was carried out at Zhejiang University. Before participating in the STC, all students completed a clerkship involving theoretical courses including Internal Medicine, Surgery, Obstetrics and Gynecology, Paediatrics, and etc. As students had completed a gynecological inpatient rotation, they were familiar with the diagnosis and treatment of common gynecological conditions. They had also been trained to perform standard physical examinations. In routine gynecology clinic rotations, 5th year medical students spend a 5-day clerkship for an outpatient clinic shadowing, where they are supposed to observe their tutors’ consultations with various gynecologic patients. During this clinical shadowing, the primary focus is on the consultation between the attending physician and the patient, with the student primarily observing, as is typical in shadowing experiences. In some cases, they may be encouraged to perform simple procedures (Figure 1A). At the end of the gynecological rotation, students complete a consultation with a standardized patient (SP) and perform a physical examination of a model. Tutors would evaluate all the consultations using the Mini Clinical Exercise evaluation (mini-CEX) (8) with unbiased scores.
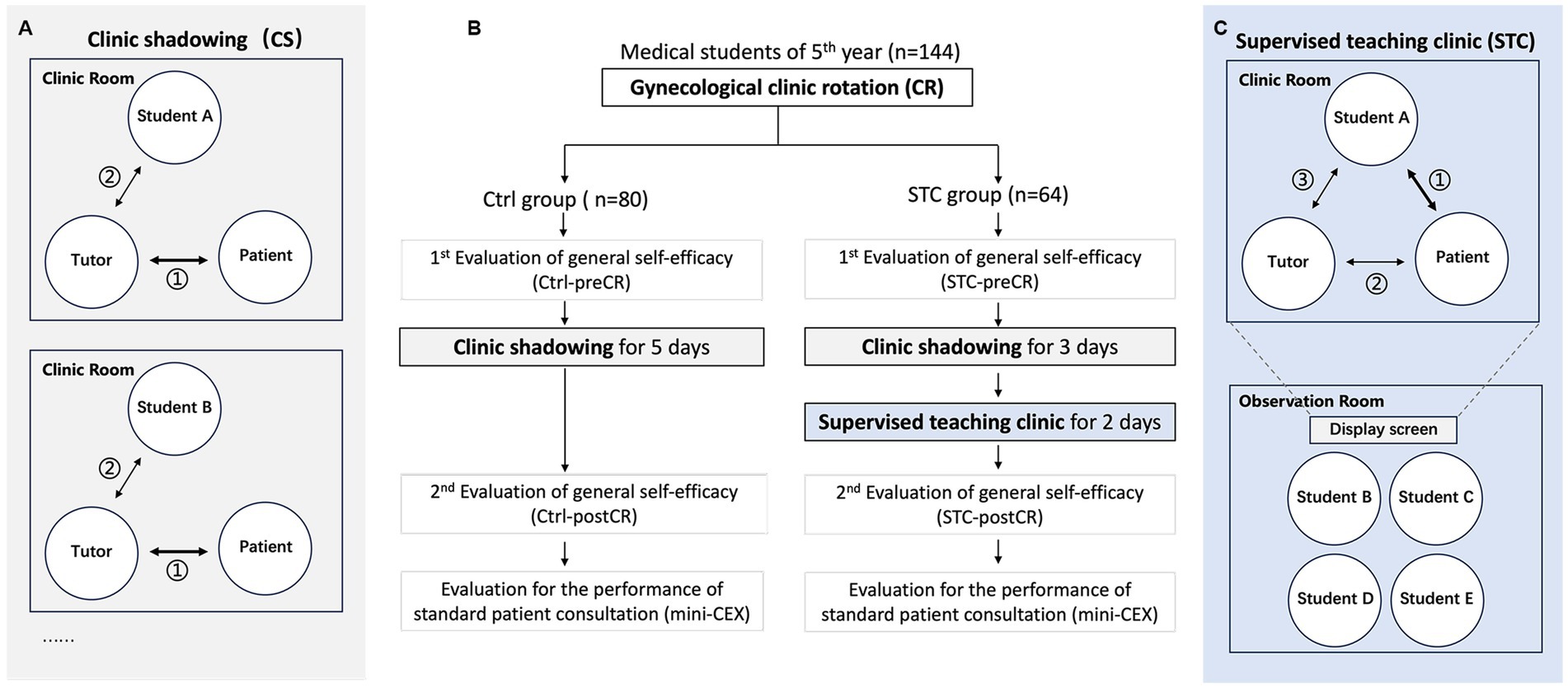
Figure 1. Overview and flow diagram of the study design. (A) The gray box on the left represents the traditional clinic rotation (clinic shadow), where the primary interaction occurs between the tutor and the patient. After the session, the tutor may briefly discuss the case with the student. (B) The diagram outlines the overall clinic rotation process. (C) The blue box on the right represents the supervised teaching clinic (STC), where the primary interaction occurs between the student and the patient. The tutor may interact with the patient afterward or as needed, followed by a feedback session between the tutor and the student.
2.2 ParticipantsA total of 144 rotation-batched medical students were divided by stratified random sampling (Supplementary Table S1) into (i) a control (Ctrl) group (n = 80; 35 males and 45 females) and (ii) a supervised teaching clinic (STC) group (n = 64; 30 males, 34 females) (Figure 1B). The STC group was further divided into subgroups containing 4 students each. The Ctrl group completed the 5 days’ clinic shadowing, while the STC group spent 3 days for clinic shadowing and 2 days for performing the STC during the rotation. Six gynecologic tutors (associate chief gynecologist or above) with at least 3 years of experience in clinical teaching oversaw the STC. We also recruited 97 gynecologic patients without emergent conditions or mental diseases in STC (Supplementary Table S2).
2.3 STC designDuring the STC, a student performed a consultation with a real patient under the supervision of the tutor. The STC involved three steps: First, a student independently interviewed a RP for consultation and performed a physical examination (including pelvic examination) if necessary. Second, the tutor made supplements or corrections (if necessary) to provide the patient with proper diagnosis and treatment. Third, after the patient left, the tutor commented on the student’s performance with proper feedback. During the STC, the consultation by the medical student is consider the most critical part, and the tutor tried not to interrupt the consultation and only provided minor suggestions if necessary. At the same time, students in the same subgroup sat in another room and observed the whole process (except the pelvic examination). Each student in the STC group participated in the consultation involving the real patients (Figure 1C). Written informed consent was obtained from each participant.
2.4 Outcome measuresStudents’ confidence and optimistic self-beliefs were evaluated using the Generalized Self-Efficacy Scale (GSES) (9). Students in both control group and STC group completed the GSES before and after the clinic rotation. All the students’ performance of consultations are evaluated by the Ctrl and STC groups independently completed the mini-CEX of consultation with an SP (Figure 1B). After participating in the STC, students completed an 8-item questionnaire to express their experiences and needs. The patients completed an 8-item questionnaire to report their perceptions of the consultation. Responses were measured by a 5-point Likert scale, from 1 indicating “strongly disagree” to 5 indicating “strongly agree.” Incomplete questionnaires (with no response to one or more of the eight questions) were not counted. Tutors were encouraged to write down their experiences and feelings during the STC. All data were collected and analyzed (see Figures 2, 3).
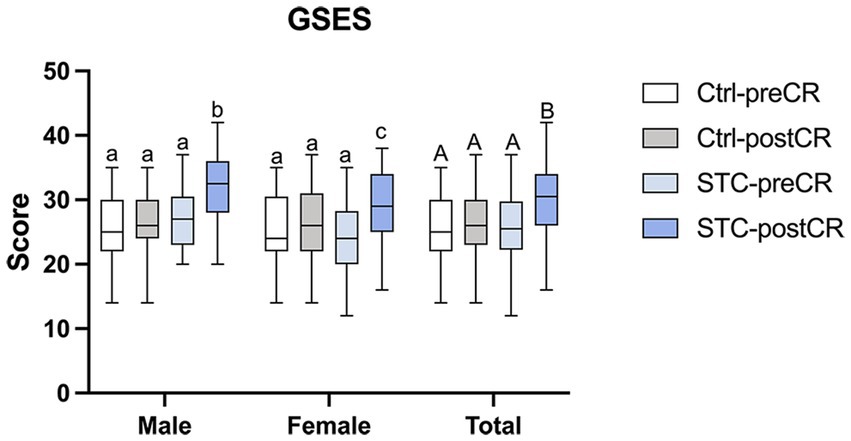
Figure 2. Students’ general self-efficacy before and after clinic rotation (CR). Results are expressed as the box plots. Lines represent min to max intervals. Higher numbers represent better scores. Values without a common letter are significantly different (p < 0.05). GSES = general self-efficacy scale; CR = clinic rotation; STC = supervised teaching clinic; Ctrl-preCR = students’ GSES in the control group before clinic rotation (white box); Ctrl-postCR = students’ GSES in the control group after clinic rotation (gray box); STC-preCR = students’ GSES in the STC group before clinic rotation (light blue box); STC-postCR = students’ GSES in the STC group after clinic rotation (blue box).
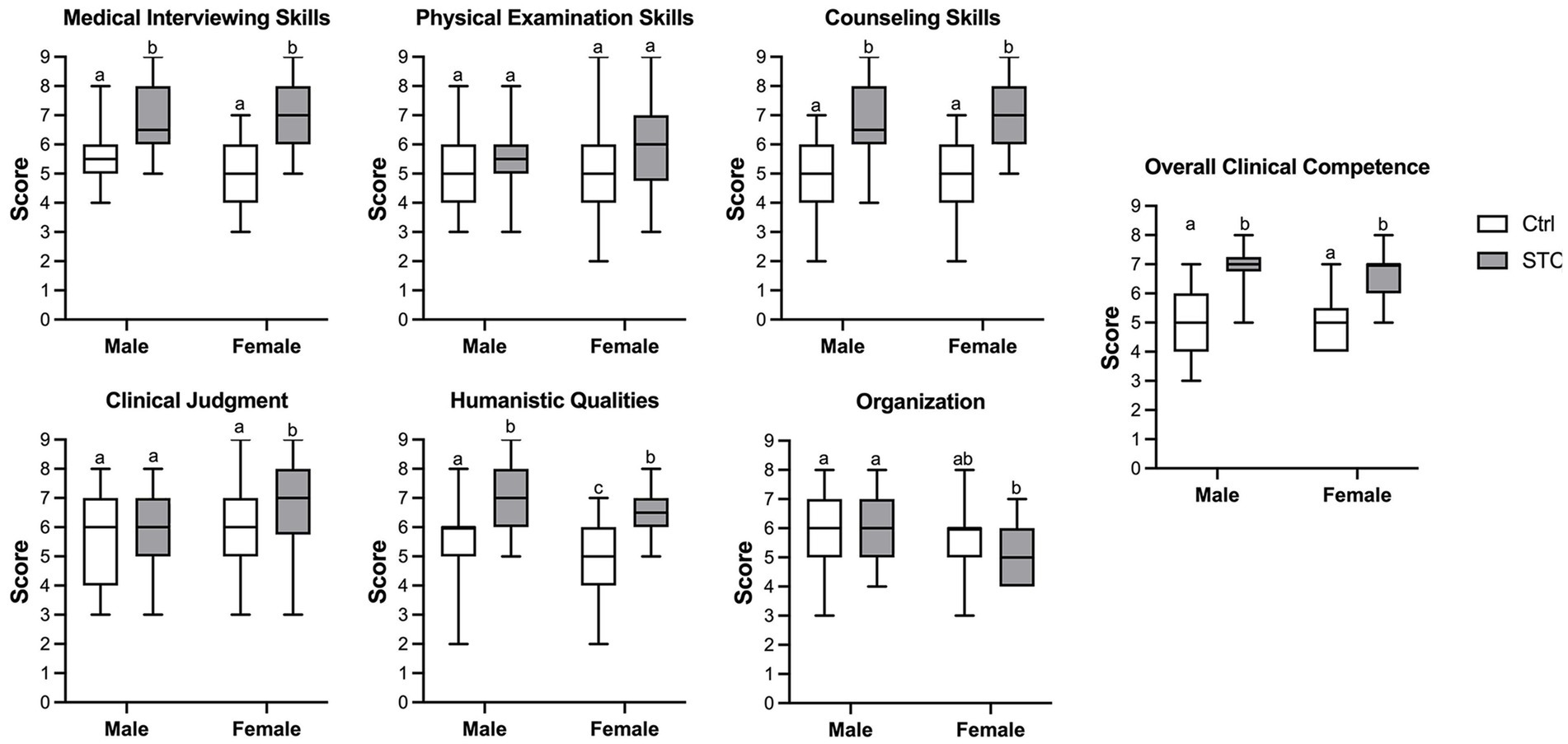
Figure 3. The performance of students’ consultation with standard patients. All the students’ performance of consultations with standard patients are evaluated independently completed the Mini Clinical Exercise evaluation (mini-CEX). Results are expressed as the box plots. Lines represent min to max intervals. Higher numbers represent better scores. Values without a common letter are significantly different (p < 0.05). Ctrl = control group; STC = the supervised teaching clinic group.
2.5 Statistical analysisContinuous variables are reported as the mean ± standard deviation. Data were analyzed by two-way analysis of variance (ANOVA) followed by Tukey’s post hoc tests. Comparisons between groups were made using the paired student’s t-test for continuous variables. Results with p < 0.05 were considered statistically significant. Statistical analysis was conducted using online GraphPad Software.
3 Results 3.1 Students’ GSES scoresAfter the STC training, students’ general self-efficacy improved. There was no significant difference between the Ctrl and STC groups before clinic rotation (Ctrl-preCR vs. STC-preCR), and no significant difference before and after the clinic rotation in Ctrl group (Ctrl-preCR vs. Ctrl-postCR). However, the GSES scores increased after the STC training (STC-preCR vs. STC-postCR). Interestingly, the increase in GSES scores was more pronounced among male medical students compared to female students in STC group (Figure 2).
3.2 Students’ performance of consultation after the gynecology clinic rotationThe performance of consultation with the SPs were compared between the Ctrl and STC groups at the end of the clinic rotation (Ctrl vs. STC). Both male and female students in the STC group scored higher on medical interviewing skills, counseling skills, humanistic qualities, and overall clinical competence. Furthermore, female students seem to get improvement in the clinical judgment, but not organization, rather than male students. There was no significant difference in physical examination skills, clinical judgment and organization scores between Ctrl and the STC group (Figure 3).
3.3 Feedback on the STCAll students in the STC group (n = 64) completed the questionnaire. The mean (SD) scores for the 8 items are as follows: “STC is necessary for clerkship” 4.92 (0.27); “STC meets the internship expectations” 4.84 (0.44); “STC is systematic and logical” 4.77 (0.52); “STC improves your clinical practice skills” 4.34 (0.94); “STC improves your clinical judgment” 4.64 (0.65); “STC improves your counseling skills” 4.86 (0.35); “You are satisfied with the overall experience” 4.80 (0.51); and “You expect more opportunities of STC” 4.81 (0.46) (Table 1).

Table 1. Feedback responses of STC from students.
Feedback on the STC was also collected from six tutors. They agreed with the items as follows: “Necessary for clerkship” (n = 5), “Helpful and meaningful for undergraduates” (n = 4), “A challenge for both students and tutors” (n = 3), “Mini-CEX is great to evaluate students’ performance” (n = 3), “Surprised by patients’ high satisfaction” (n = 2), and “The consultation is time consuming” (n = 2) (Table 2).
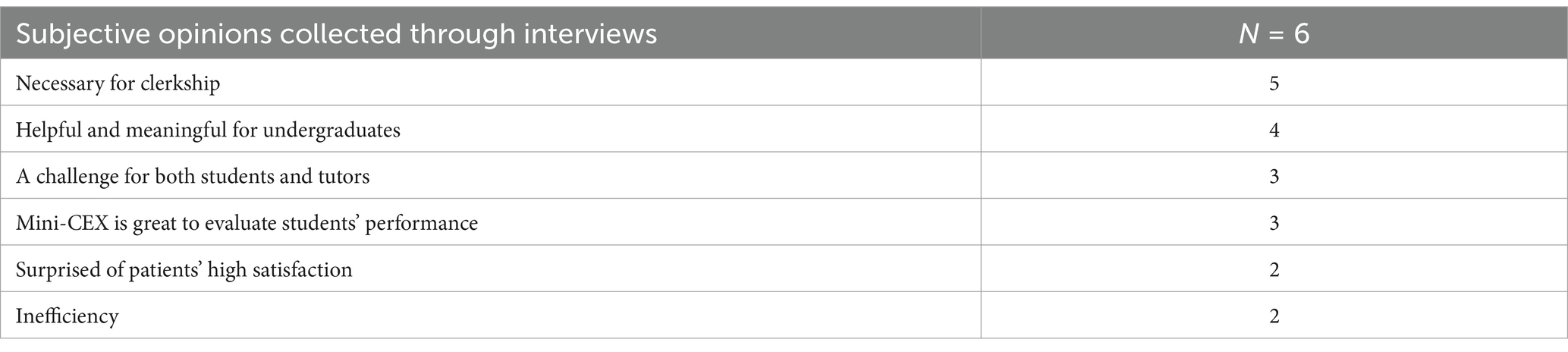
Table 2. Interview of tutors’ experiences of STC.
A total of 97 patient surveys were received and analyzed. All patients felt satisfied with the STC experience at different levels. The mean (SD) scores for the 8 questions were as follows: “Your doctor is qualified” 4.91 (0.29); “You received appropriate treatment” 4.88 (0.33); “It was effective counseling “4.96 (0.20); “Your doctor complied with rigorous medical ethics” 4.99 (0.10); “Your privacy was well-protected” 4.87 (0.34); “You were in a safe and comfort environment during the consultation” 4.94 (0.34); “You were satisfied with the overall experience” 4.94 (0.34); and “You would recommend STC to others” 4.87 (0.34) (Table 3).
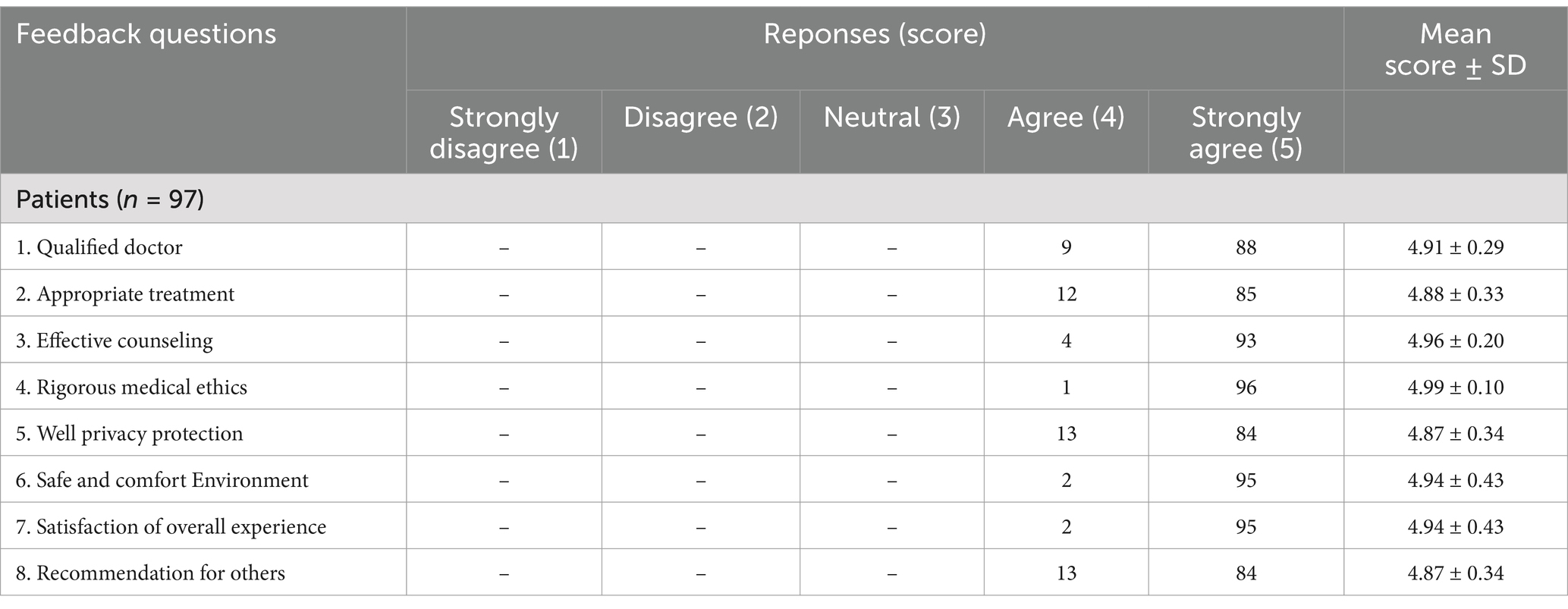
Table 3. Feedback responses of STC from patients.
4 DiscussionA well-established theoretical framework for describing educational environments puts forward three domains as critical to the quality of human environments: goal direction or content of education, relationships, and supporting services (10). It was also applicable to the educational context (11), serving as a framework to explore the needs, expectations and experiences of medical students regarding their learning during the STC. These findings suggest that the structured design of the STC model effectively balances student-centered education with patient-centered care (Figure 4).
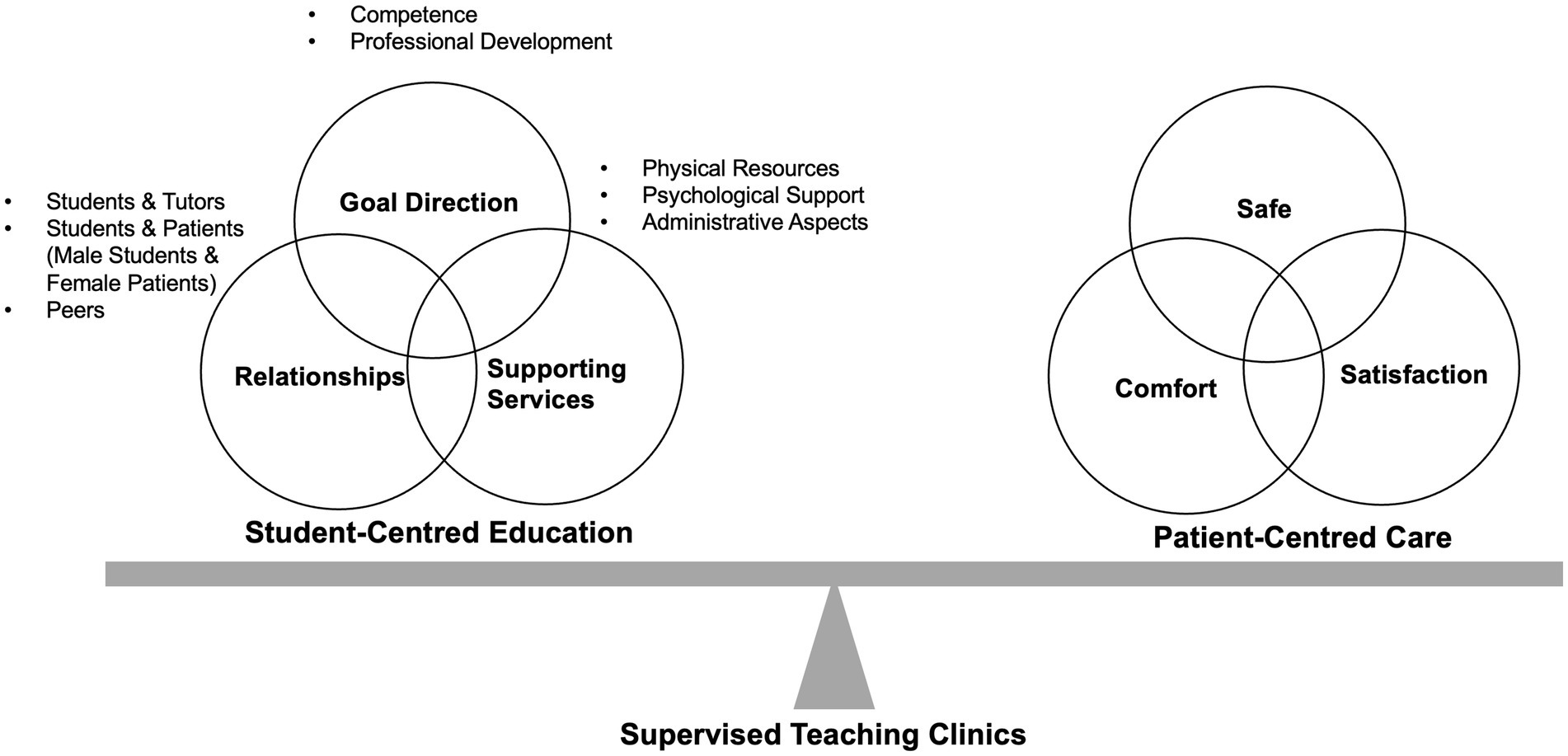
Figure 4. Balancing Student-Centered Education and Patient-Centered Care in the Supervised Teaching Clinic (STC) Model. The structured design of the supervised teaching clinic (STC) model effectively balances student-centered education with patient-centered care. The model is built upon three key pillars: goal direction, relationships, and supporting services.
4.1 Goal directionThe implementation of the STC in this study aligns strongly with the dimension of goal direction, a fundamental aspect of creating a conducive learning environment. In the context of medical education, goal direction refers to the clarity of educational objectives and the systematic approach toward achieving them (12). Within the STC, students were not merely passive observers but active participants in patient care, a shift that is essential for their professional development.
The STC provided a structured platform where students could set and pursue clear, tangible goals. This focus on goal-oriented tasks allowed students to progressively build their competencies in a controlled environment, with the opportunity to receive immediate feedback and make necessary adjustments. The observed improvement in students’ GSES after participating in the STC is a testament to the effectiveness of this approach. Self-efficacy, a crucial factor in professional development, is enhanced when learners can achieve small, incremental goals, leading to greater confidence and autonomy in their future practice (13).
The STC’s structure also prompted students to reflect on their professional identity. Allowing students to interview patients independently results in psychological insights and deeper learning reflections, emphasizing the concepts of communication, humanity, and empathy in the learning process that goes beyond medical theoretical knowledge and clinical skills exercises. Students reported that the STC was necessary for developing clinical judgment, practice skills, and counseling skills during their clerkship. By engaging in real patient interactions, students might be able to visualize their future roles as healthcare providers, a critical aspect of their professional identity formation. This aligns with the broader goals of CBME, where the emphasis is on not just acquiring knowledge, but also on developing the attitudes and behaviors necessary for professional practice. The ability to independently conduct patient interviews and physical exams, while under supervision, provided students with a unique opportunity to integrate their theoretical knowledge with practical skills, thereby solidifying their understanding of their professional responsibilities.
The goal direction within the STC was further reinforced by the use of structured evaluation tools like the mini-CEX. Mini-CEX is an appropriate tool for formative evaluation during clinical competence. Mini-CEX has been shown to enhance student-patient interactions, leading to improved care services, while also strengthening the interactions between students and evaluators during the assessment of clinical skills (8, 14). This tool provided a clear framework for tracking students’ progress and ensured feedback was focused and actionable. The systematic approach to evaluation helped students to identify areas for improvement and monitor their progress, contributing to a more effective learning experience.
4.2 Relationships and interpersonal skillsThe relational dimension of the STC cannot be overstated. Relationships, both between students and tutors, as well as between students and patients, play a pivotal role in the learning process. In traditional clinical settings, the hierarchical nature of the student-tutor relationship often limits the extent to which students can actively engage in patient care. However, the STC model employed in this study sought to redefine these relationships by fostering a more collaborative learning environment.
Achieving a balance between autonomy and supervision is often challenging, particularly in the context of medical education (15). Within the STC, the balance was characterized during the tutor-student relationship. Tutors provided guidance and support without overshadowing the students’ active participation in patient consultations. This balance is crucial in medical education, as it allows students to develop confidence in their clinical abilities while still benefiting from the expertise of their tutors. The presence of a supportive tutor during real patient interactions helped to alleviate the stress and anxiety that students often experience in clinical settings, particularly in sensitive fields like gynecology. This supportive relationship was further evidenced by the students’ high satisfaction ratings (Table 1), with many expressing a desire for more opportunities to participate in STCs.
Feedback is an essential component of effective teaching and learning (16–18). Literature suggested that learning is enhanced if feedback is specific (19), and a “move away from apprenticeship to experiential learning” has been advocated (20). STCs can serve this critical function if tutors are trained to give constructive feedback. According to the importance of constructive feedback, anticipatory thinking and ‘mental simulation’ can enhance learning (21). Repeated exposure to supervised patient clerking and examination by more widespread use of STCs would allow learners to develop their mastery, reinforcing Ericsson’s theory of deliberate practice (22) and Bloom’s theory of mastery (23). Such practice and refinement facilitate learning in a practical environment.
In addition to the tutor-student relationship, the STC also facilitated the development of strong student-patient relationships. Unlike simulated patient interactions, which can sometimes feel artificial, the use of real patients in the STC provided students with a more authentic clinical experience. This authenticity is critical for the development of interpersonal skills such as empathy, active listening, and effective communication (24). The positive feedback from patients, who reported high levels of satisfaction with their STC experience (Table 3), indicates that the students were able to establish meaningful connections with their patients. These relationships not only enhanced the students’ learning experience but also contributed to the overall quality of care provided during the consultations.
Male doctors may face some cultural or social barriers during gynecological clinical work, especially when they are still medical students (25). In our study, Improvement in general self-efficiency (Figure 2) and performance (Figure 3) during the consultation were observed in both male and female students.
Furthermore, the relational aspect of the STC extended to peer relationships within the student groups. The collaborative nature of the STC, where students observed and learned from each other’s consultations, fostered a sense of camaraderie and mutual support. This peer learning dynamic is particularly valuable in medical education, where the exchange of ideas and experiences among students can enhance understanding and retention of clinical knowledge (26). The opportunity to observe their peers in action also provided students with additional learning opportunities, as they could critically assess different approaches to patient care and incorporate best practices into their own consultations.
4.3 Supporting servicesThe third dimension, supporting services, is integral to the success of any educational program, particularly in a clinical setting. In the STC, the availability of robust support services ensured that students could focus on their learning without being hindered by logistical challenges. These services encompassed a range of resources, from the physical setup of the clinic to the psychological support provided to students.
The physical environment of the STC was carefully designed to mimic a real clinical setting, providing students with a realistic context in which to apply their skills. Teaching in the presence of real patients in a clinical setting is ideal for medical education (27). There is evidence that patient inclusion contributes to a positive medical learning environment (28). It provides a critical component for students to learn humanistic and professional behaviors (29), especially when doctors who are considered excellent tutors model positive patient care behaviors in clinical work. This environment also included the access to essential medical equipment, private consultation rooms, and comfortable spaces for students to discuss and reflect on their experiences. The importance of a well-equipped learning environment cannot be overstated, as it directly impacts the quality of the educational experience (30). To ensure the safety and comfort of all individuals, it is essential to view the environment of STC as a patient- centered clinic rather than an instructional setting.
In addition to the physical resources, the STC also provided significant psychological support to students. Medical education is inherently stressful, and the transition from theoretical learning to practical application can be daunting for many students (31). Qualified tutors should provide optimal patient care while ensuring a high quality of clinical teaching. Besides maximizing students’ opportunities to consult with real patients, they must maintain patients’ safety and privacy. To preserve the student-patient relationship and create a supportive environment for effective feedback, in-depth discussions about differential diagnosis or management should be conducted after the patients have departed (32). This psychological support was further reinforced by the structured nature of the STC, which included regular debriefing sessions where students could discuss their experiences and receive encouragement from their peers and tutors.
The supporting services also extended to the administrative aspects of the STC. The careful selection of patients, the scheduling of consultations, and the coordination of tutor involvement were all managed to ensure that the STC operated smoothly and efficiently. Real patient-based form of education introduces students to the supervised and structured clinical environment, providing opportunities to participate in medical interviews, humanistic qualities, history taking, physical examination, clinical reasoning, and organization (33). Emergent and vague cases are not appropriate for STCs. Common and frequently occurring gynecological diseases, such as endometriosis or leiomyoma, are ideal for STCs. Moreover, informed consent about recording the consultation process is needed.
4.4 Healthcare during the STCPatient involvement allows for greater patient inclusion in making decisions, encourages efficiency in history presentations and evaluations (34, 35). Previous reports show that patients also benefit from clinical teaching experiences with better understanding of their disease, more compassion and respect from the medical team, and increased inclusion during the medical care (36).
Patient satisfaction and consultation outcomes are always the most significant concerns during STCs. This study seeks to find the optimal balance between student-centered education and patient-centered care (Figure 4). Moreover, we found that patients received appropriate treatment and effective counseling during the STC and were satisfied with the overall experience. Patients have dual requirements for participating in the consultations: the need for reassurance of their medical conditions and hope to help students (37). All participating patients share the wish to help students learn, indicating a high potential for mutually beneficial student-patient relationships during STCs (38). Learning is founded on a reciprocal relationship between patients and students, leading to patients actively engaging in the learning process, which they perceive as a collaborative effort (39). Studies indicate that patients are generally satisfied with the care delivered by medical students and uphold a favorable perception of their interactions with these students (40, 41). The patient’s role includes a secondary benefit of student-led consultations: the sense of contributing to the education of future doctors (42). In the present study, patients involved in the STC reported high satisfaction (Table 3), maybe even higher than that in routine clinics. Since students always “asked more non-critical questions,” which made the patients feel taken more seriously. Patients were also pleased that two medical staff (including at least one certificated gynecologist) were dealing with their problems, making them feel safer and that the consultation was more effective.
4.5 Implications for practice and future researchThis study has important implications for clinical education. The STC model, with its emphasis on goal direction, relationships, and supporting services, serves as a guide for developing effective medical education. Integrating these three dimensions into the design and implementation of clinical teaching programs may maximize learning outcomes for medical students.
For practice, our findings suggest that medical schools should consider incorporating STCs into their curricula. This model, with its benefits such as improving clinical competency, enhancing interpersonal communication, and boosting student satisfaction, might be a valuable addition to traditional clinical training methods. However, the successful adoption of STCs requires significant investment in well-trained tutors, equipped clinical spaces, and robust administrative systems. For example, detailed and standardized mini-CEX scoring indicators based on teaching objectives should be set, which tutors can use in subsequent STC after training.
Future research should explore the long-term impacts of STCs on student outcomes. While this study demonstrated improvements in self-efficacy and clinical skills, further research is needed to determine if these gains translate into professional practice. Longitudinal studies that track students from their time in the STC through to their early years of practice would provide valuable insights into the effectiveness of this educational model. Additionally, research could explore the potential for adapting the STC model to other areas of medical education, such as surgical training or primary care, where the principles of goal direction, relationships, and supporting services are equally relevant.
4.6 LimitationsThe study’s observation period was short, focusing on the immediate effects of STC training. Long-term impacts on professional development and clinical skills acquisition may not be fully captured in this timeframe. Future research should consider longitudinal studies to evaluate the enduring effects of STC on students’ career trajectories and clinical competence. Additionally, although the mini-CEX was employed as an assessment methodology it is by nature subjective and based on tutor’s observations. Variability in grading standards among tutors may affect the consistency and reliability of the results.
5 ConclusionThis study has demonstrated the STC model at a tertiary teaching hospital., when designed with a focus on goal direction, relationships, and supporting services, provides a highly effective framework for medical education. The STC not only enhances students’ clinical competencies but also fosters the development of critical interpersonal skills and provides the necessary support for a positive learning experience. The findings of this study suggest that the STC model could be considered to further integrated into medical curricula, with continued research and investment to optimize its implementation. In the future of medical education, the STC offers a promising approach to preparing healthcare professionals for the challenges of clinical practice.
Data availability statementThe original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
Ethics statementThe studies involving humans were approved by Ethics Committec of Women’s Hospital, School of Medicine, Zhejiang University. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributionsSR: Conceptualization, Data curation, Formal analysis, Investigation, Writing – original draft, Writing – review & editing. HZ: Conceptualization, Data curation, Methodology, Writing – original draft, Writing – review & editing. AF: Conceptualization, Writing – review & editing. XX: Project administration, Writing – review & editing. WL: Conceptualization, Project administration, Resources, Writing – review & editing.
FundingThe author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
AcknowledgmentsWe would like to thank all the participants who participated in the study.
Conflict of interestThe authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s noteAll claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary materialThe Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fmed.2024.1498393/full#supplementary-material
References3. Lankshear, C, and Knobel, M. New literacies: Everyday practices and social learning. 3rd ed. Maidenhead, Berkshire, England: Open University Press, McGraw-Hill Education (2011).
4. Schaepkens, SPC, Veen, M, and de la Croix, A. Is reflection like soap? A critical narrative umbrella review of approaches to reflection in medical education research. Adv Health Sci Educ Theory Pract. (2022) 27:537–51. doi: 10.1007/s10459-021-10082-7
PubMed Abstract | Crossref Full Text | Google Scholar
6. Schimbeno, V, Bosle, C, Stegmeier-Petroianu, A, Etminan, N, and Hoffmann, K. Competence-based teaching and learning in the outpatient clinic: development of a clinical elective in ambulatory medicine. GMS J Med Educ. (2019) 36:Doc36. doi: 10.3205/zma001244
Crossref Full Text | Google Scholar
8. Weller, JM, Castanelli, DJ, Chen, Y, and Jolly, B. Making robust assessments of specialist trainees' workplace performance. Br J Anaesth. (2017) 118:207–14. doi: 10.1093/bja/aew412
PubMed Abstract | Crossref Full Text | Google Scholar
9. Cheung, SK, and Sun, SY. Assessment of optimistic self-beliefs: further validation of the Chinese version of the general self-efficacy scale. Psychol Rep. (1999) 85:1221–4. doi: 10.2466/pr0.1999.85.3f.1221
PubMed Abstract | Crossref Full Text | Google Scholar
10. Schönrock-Adema, J, Bouwkamp-Timmer, T, van Hell, EA, and Cohen-Schotanus, J. Key elements in assessing the educational environment: where is the theory? Adv Health Sci Educ Theory Pract. (2012) 17:727–42. doi: 10.1007/s10459-011-9346-8
PubMed Abstract | Crossref Full Text | Google Scholar
11. Xu, X, Schönrock-Adema, J, Jaarsma, ADC, Duvivier, RJ, and Bos, NA. A conducive learning environment in international higher education: a systematic review of research on students’ perspectives. Educ Res Rev. (2022) 37:100474. doi: 10.1016/j.edurev.2022.100474
Crossref Full Text | Google Scholar
12. Manzone, J, Regehr, G, Garbedian, S, and Brydges, R. Assigning medical students learning goals: do they do it, and what happens when they Don't? Teach Learn Med. (2019) 31:528–35. doi: 10.1080/10401334.2019.1600520
PubMed Abstract | Crossref Full Text | Google Scholar
14. Sharma, R, Gupta, T, Haidery, TH, Sinha, S, and Kumar, A. Current trends in Mini-clinical evaluation exercise in medical education: a bibliometric analysis. Cureus. (2022) 14:e33121. doi: 10.7759/cureus.33121
PubMed Abstract | Crossref Full Text | Google Scholar
15. Singman, EL, Boland, MV, Tian, J, Green, LK, and Srikumaran, D. Writing Committee of the Ophthalmology Program Directors' study G. Supervision and autonomy of ophthalmology residents in the outpatient clinic in the United States II: a survey of senior residents. BMC Med Educ. (2019) 19:105. doi: 10.1186/s12909-019-1620-0
PubMed Abstract | Crossref Full Text | Google Scholar
16. Rolfe, IE, and Sanson-Fisher, RW. Translating learning principles into practice: a new strategy for learning clinical skills. Med Educ. (2002) 36:345–52. doi: 10.1046/j.1365-2923.2002.01170.x
PubMed Abstract | Crossref Full Text | Google Scholar
18. Gagne, RM, Wager, WW, Golas, KC, Keller, JM, and Russell, JD. Principles of instructional design, 5th edition. Perform Improv. (2005) 44:44–6. doi: 10.1002/pfi.4140440211
Crossref Full Text | Google Scholar
20. Hesketh, E, Bagnall, G, Buckley, EG, Friedman, MG, Goodall, E, Harden, RM, et al. A framework for developing excellence as a clinical educator. Med Educ. (2001) 35:555–64. doi: 10.1046/j.1365-2923.2001.00920.x
PubMed Abstract | Crossref Full Text | Google Scholar
22. Ericsson, KA, Krampe, RT, Tesch-Romer, C, Ashworth, C, Carey, G, Crutcher, RJ, et al. The role of deliberate practice in the acquisition of expert performance. Psychol Rev. (1993) 100:363–406. doi: 10.1037/0033-295X.100.3.363
Crossref Full Text | Google Scholar
23. Bloom, BS. Learning for mastery. Instruction and curriculum In: Regional education Laboratory for the Carolinas and Virginia, topical papers and reprints, number 11968 (1968).
24. Gilligan, C, Powell, M, Lynagh, MC, Ward, BM, Lonsdale, C, Harvey, P, et al. Interventions for improving medical students' interpersonal communication in medical consultations. Cochrane Database Syst Rev. (2021) 2:CD012418. doi: 10.1002/14651858.CD012418.pub2
PubMed Abstract | Crossref Full Text | Google Scholar
25. Craig, LB, Buery-Joyner, SD, Bliss, S, Everett, EN, Forstein, DA, Graziano, SC, et al. To the point: gender differences in the obstetrics and gynecology clerkship. Am J Obstet Gynecol. (2018) 219:430–5. doi: 10.1016/j.ajog.2018.05.020
PubMed Abstract | Crossref Full Text | Google Scholar
26. Jawhari, AA, Safhi, MA, Magadmi, MM, Alobaidi, RH, Alghamdi, KM, Basyouni, RN, et al. Effect of peer-assisted learning on enhancing clinical research skills among medical students: Students' and Tutors' perceptions. Adv Med Educ Pract. (2021) 12:685–96. doi: 10.2147/AMEP.S315041
PubMed Abstract | Crossref Full Text | Google Scholar
27. Herrera-Aliaga, E, and Estrada, LD. Trends and innovations of simulation for twenty first century medical education. Front Public Health. (2022) 10:619769. doi: 10.3389/fpubh.2022.619769
PubMed Abstract | Crossref Full Text | Google Scholar
28. Gruppen, L, Irby, DM, Durning, SJ, and Maggio, LA. Interventions designed to improve the learning environment in the health professions: a scoping review. MedEdPublish. (2018) 7:7. doi: 10.15694/mep.2018.0000211.1
PubMed Abstract | Crossref Full Text | Google Scholar
29. Weissmann, PF, Branch, WT, Gracey, CF, Haidet, P, and Frankel, RM. Role modeling humanistic behavior: learning bedside manner from the experts. Acad Med. (2006) 81:661–7. doi: 10.1097/01.ACM.0000232423.81299.fe
PubMed Abstract | Crossref Full Text | Google Scholar
30. Closs, L, Mahat, M, and Imms, W. Learning environments' influence on students' learning experience in an Australian Faculty of Business and Economics. Learn Environ Res. (2022) 25:271–85. doi: 10.1007/s10984-021-09361-2
PubMed Abstract | Crossref Full Text | Google Scholar
31. Opoku, EN, Khuabi, LJ, and Van Niekerk, L. Exploring the factors that affect the transition from student to health professional: an integrative review. BMC Med Educ. (2021) 21:558. doi: 10.1186/s12909-021-02978-0
PubMed Abstract | Crossref Full Text | Google Scholar
32. Cheema, B, Li, M, Ho, D, Amari, E, Buckley, H, Canfield, C, et al. Patient-present teaching in the clinic: effect on agency and professional behaviour. Med Educ. (2022) 56:270–9. doi: 10.1111/medu.14623
留言 (0)