• One in five Medicaid beneficiaries had mental and physical comorbidities (complex needs).
• Increased socioeconomic deprivation score is associated with increased complex needs.
• There is spatial autocorrelation of the prevalence of complex needs.
• Areas with greater deprivation need more integrated mental and physical health services.
IntroductionBeginning in late 2015, Utah Medicaid identified a limited proportion of substantial need and substantial healthcare use patients who accounted for a disproportionate expenditure of Medicaid costs. Some beneficiaries in the top percentile of healthcare costs have frequent contact with high-cost healthcare services that may not be fully addressing their complex needs, particularly those needs related to comorbid physical and mental health conditions (1). Typically, persons with physical and mental health comorbidities have poorer health outcomes and higher healthcare costs (2). Medicaid beneficiaries with physical and mental health comorbidities cost up to 75% more than those without mental health comorbidities (3).
The high proportion of mental health conditions among Medicaid beneficiaries with physical health conditions nationally has been documented (2). Despite the presence of high levels of physical and mental health comorbidities among beneficiaries, Medicaid-covered mental health services have historically been segregated from physical health services (4). This fragmentation of the healthcare system makes both mental health and physical health services more difficult to access, resulting in unmet patient needs and increased healthcare costs (5).
Physical and mental health comorbidities are exacerbated by socioeconomic deprivation (6, 7). A better understanding of the healthcare needs of these patients and the socioeconomic factors that affect healthcare use can help achieve healthcare cost containment and improve population health outcomes (8).
Limited information is available regarding the association between comorbid physical and mental health conditions and geographical socioeconomic disparities among Utah Medicaid beneficiaries. To fill this knowledge gap, we sought to characterize the complex needs of Utah Medicaid beneficiaries and examine how complex needs are associated with socioeconomic deprivation as measured by the Singh area deprivation index (ADI) (9). We hypothesized that socioeconomic deprivation was associated with an increased prevalence of comorbidities.
Methods Study design and eligibility criteriaWe conducted a cross-sectional retrospective cohort analysis of Utah Medicaid claims data from the Division of Medicaid and Health Financing at the Utah Department of Health (UDOH). Medicaid claims data are the medical bills submitted to Utah Medicaid for the services provided to Medicaid beneficiaries by care providers; each claim is associated with a date of service. To capture the entire population of Medicaid beneficiaries in a 12-month period, we reviewed claims data for all Medicaid beneficiaries eligible for at least 1 month in Utah during Fiscal Year 2017 (from 1 July 2016 to 30 June 2017). We extracted Utah Medicaid claims costs using Structured Query Language from the Medicaid centralized data warehouse, which contains patient-managed care, fee for service, and pharmacy claims. Claims costs during the 12 months before a beneficiary’s most recent claim based on the date of service in the study period were used. This design was selected in order to simulate rolling patient identification, which is more representative of data that would be used operationally to identify high utilizers and less likely to be biased by an arbitrary time cut point that might not capture changes in care-seeking behavior (10). Persons eligible for at least 1 month during the 12 months without any medical claims were assigned a cost of $0. Data were collected at the individual patient level and included the patient’s unique identifier, date of birth, number of months they were eligible for Medicaid, diagnosis codes, address, demographic information, and medical costs.
The sampling population included beneficiaries enrolled in managed care or fee-for-service. Refugees and custody medical patients were excluded. We limited the analysis to adults aged ≥18 years. The Institutional Review Boards at the Utah Department of Health (Approval #533) and the Centers for Disease Control and Prevention (HSR #2018-00189) determined that this study did not constitute human subjects’ research.
Data analysisThe International Classification of Diseases, Tenth Revision and the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-10-CM and ICD-9-CM) codes from claims data were used to define the main outcome of interest: beneficiaries with chronic physical and mental health conditions (11, 12). Chronic disease algorithms from the Centers for Medicare & Medicaid Services Chronic Conditions Data Warehouse (CCW) were used to classify chronic disease combinations (13). Based on previous published analysis conducted on the data, which identified that those with complex physical and mental health conditions were clustered (14), we defined complex needs of Medicaid beneficiaries as a chronic physical condition plus a mental health condition from the CCW Chronic Conditions categories (CCW-CC), or at least two physical conditions and any mental health condition from the CCW Other Chronic, Mental Health, or Potentially Disabling Conditions categories (CCW-OC) (Supplementary Figure 1).
Beneficiary addresses were geocoded using ArcGIS 10.5 (Environmental Systems Research Institute, Redlands, CA, USA). Software matching option parameters were set to 70% for spelling sensitivity, 70% minimum candidate score, and 70% minimum score match. A comparison of matched to unmatched addresses revealed that more addresses in urban areas vs. those in rural areas were geocoded. Because of this, we assigned a population-adjusted centroid value to any address having a zip code comprising a single census block group (all rural areas in Utah) with >50% unmatched addresses. Persons with missing addresses and those whose address was listed as homeless were excluded from the geocoding process. All geocoded addresses were assigned to their census block groups.
Because Utah’s Medicaid data lack information on key socioeconomic characteristics of beneficiaries, we used the 2015 Singh area deprivation index (ADI) to look for area-level effects of socioeconomic position. The ADI calculates a score by census block group using 17 U.S Census Bureau measures that characterize the level of socioeconomic need in a neighborhood (9). Higher index values represent higher levels of deprivation. We applied Utah-specific ADI quintiles adapted from Knighton et al. (15) from the original Singh method. Knighton et al. quintiles are the rounded census block group area deprivation scores binned into five approximately equal size groups, from lowest score (least deprivation) to highest score (highest deprivation). We calculated the proportion of beneficiaries with complex needs and ADI quintiles at the census block group level. We calculated Spearman’s rank correlation to measure the association between these two variables.
We measured healthcare utilization by the number of emergency department visits, number of hospital inpatient visits, and dollar amount in claims, including for managed care patients, during the study period. We used the X2 test to assess trends in the proportion of beneficiaries with complex needs by utilization. We used mixed-effects multivariable logistic regression (glmr in the lme4 package in R v3.5.3 [R Foundation for Statistical Computing, Vienna, Austria]) including census block group as a random effect to measure the association of complex needs with area deprivation index quintile and healthcare utilization while adjusting for sex, age groups (categorized as 18–40, 41–65, and > 65), ethnicity, and number of months (categorized as 1–3, 4–6, 7–9, and > 9) on Medicaid. We tested for multicollinearity using the variance inflation factor. We conducted an analysis of variance to compare full and reduced models. We conducted a sensitivity analysis excluding beneficiaries with no claims and those with <12 months of continued eligibility for Medicaid. We present odds ratios and 95% confidence intervals for the full model, which demonstrated the best fit.
We used GeoDa (16) and QGIS (17) software for spatial mapping of counts and proportions of complex needs. The census block group-level map was overlaid with Medicaid-covered mental health facility locations to find the census blocks with the highest counts and proportions of beneficiaries with complex needs. We also identified the census block groups with the highest counts and limited or no access to mental health facilities. Local Empirical Bayesian Moran’s I statistic (16) measured the presence of spatial dependence of the proportions of complex needs at the census block level in Utah.
Results Descriptive statisticsAmong adult beneficiaries, 157,739 (93.9%) beneficiary addresses were geocoded. The proportions with complex needs were similar between Medicaid beneficiaries whose addresses had been geocoded and those whose addresses had not (18.9% geocoded vs. 18.1% non-geocoded, p = 0.07, Supplementary Table 1). Only beneficiaries with geocoded addresses were included in the analysis. Among these, 60.9% were aged 18–40 years, 65.5% were women, and 12.6% were Hispanic. Additionally, 75.5% were enrolled in Medicaid for more than 9 months, 4.3% had visited the emergency room more than three times, and 2.2% had greater than two hospital admissions in 12 months.
Among beneficiaries with complex needs (n = 29,742), the most common chronic physical conditions included hypertension (56.0%), rheumatoid arthritis or osteoarthritis (35.5%), hyperlipidemia (33.7%), and diabetes (30.7%). The most common mental health conditions were depression (68.8%), anxiety disorders (56.2%), and traumatic brain injury and non-psychotic mental disorders attributed to brain damage (24.8%) (Table 1). Among beneficiaries with complex needs, the prevalence of drug use disorders and alcohol use disorders was 16.0 and 15.2%, respectively. The most common comorbidities were hypertension and depression (35.8%), hypertension and anxiety disorders (30.5%), and rheumatoid arthritis or osteoarthritis and depression (24.5%).
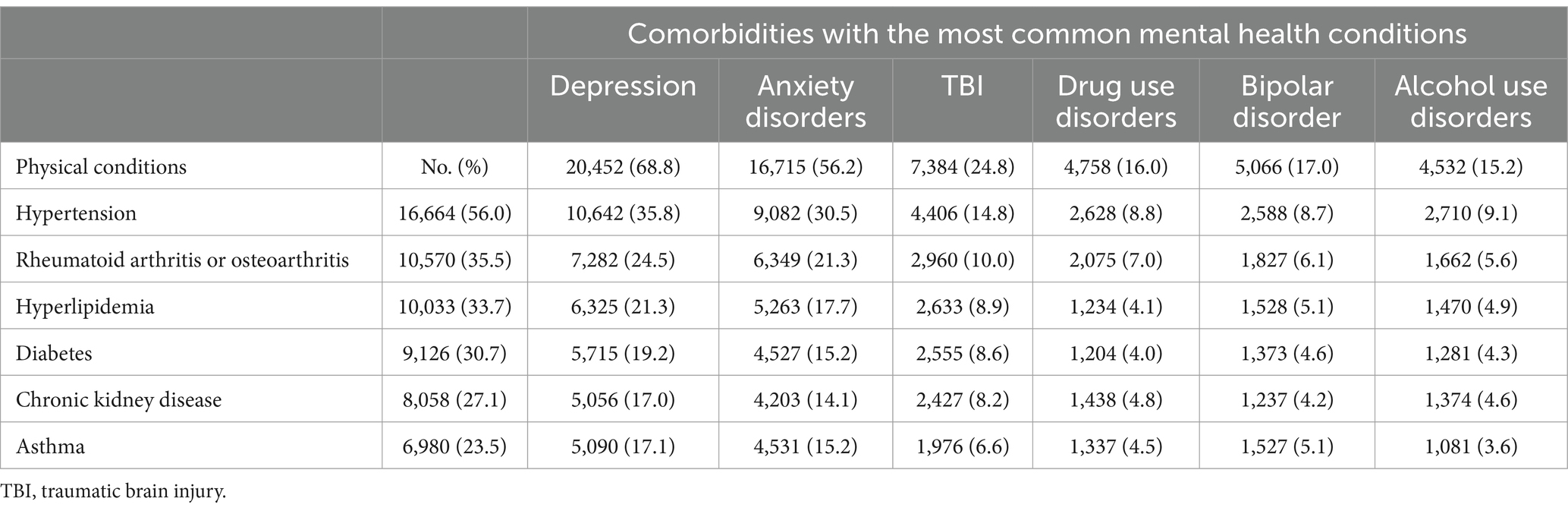
Table 1. Common comorbidities among Medicaid adult beneficiaries with complex needs (physical and mental health comorbidities) (n = 29,742), Utah – 2017.
Bivariable and multivariable analysesBeneficiaries with complex needs differed from those without complex needs in their ADI quintile, number of emergency department visits, number of hospital inpatient visits, and dollar amount paid in claims (Table 2). In our multivariable mixed-effects logistic regression that controlled for sex, age, ethnicity, and number of months on Medicaid, the proportion of beneficiaries with physical and mental health comorbidity increased significantly (p < 0.001) with deprivation quintile, reaching 20.4% among beneficiaries in the most deprived quintile compared to 15.2% among beneficiaries in the least deprived quintile. The odds of having complex needs among beneficiaries with ≥3 emergency department visits were greater than for beneficiaries with no visits (12.80, 95% confidence interval [CI] 12.07, 13.56). Similarly, the odds of having complex needs increased with increasing in-patient hospitalizations. The median amount paid in claims for beneficiaries with complex needs was $4,218 while for those without complex needs, it was $1,127. Beneficiaries with >$5,000 in paid claims had 6.26 (95% CI 5.98, 6.55) greater odds of having complex needs compared to patients with $1–$500 in paid claims.
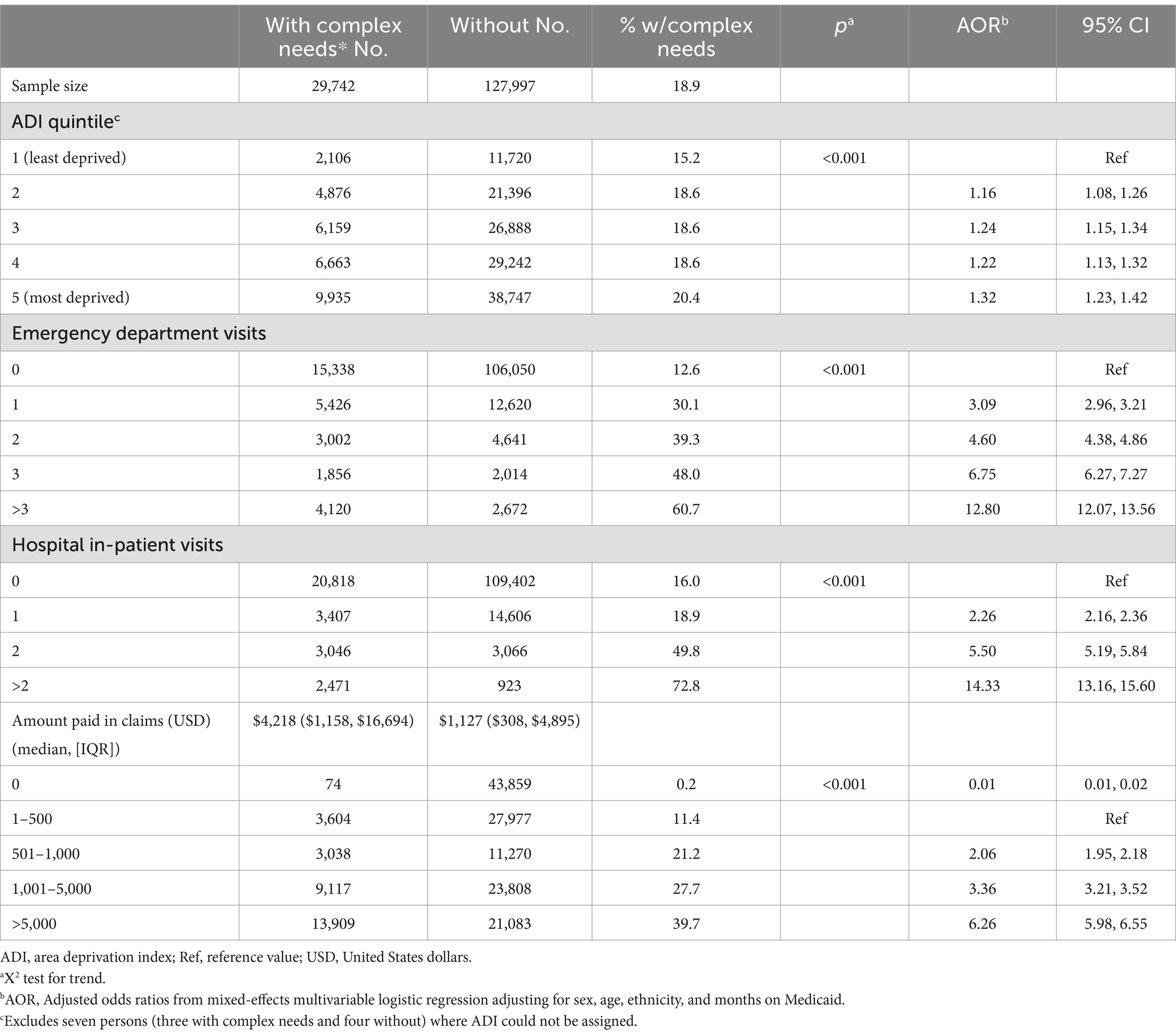
Table 2. Medicaid adult beneficiaries (N = 157,739) with and without complex needs (physical and mental health comorbidities) by the area deprivation index and healthcare utilization, Utah – 2017.
Geocoded adults were assigned to 1,680 census block groups, which were then grouped by their respective ADI quintile. The ADI divides census blocks into five approximately equally-sized groups based on their rounded ADI score, ranging from high to low. Blocks with equal scores were grouped, and each quintile contained from 292 to 377 census block groups. There was a significant positive association between the ADI and the prevalence of complex needs (ρ = 0.21, p < 0.001) (Figure 1). The median prevalence of complex needs for the lowest ADI quintile was 14.0 and 19.3% for the highest quintile.
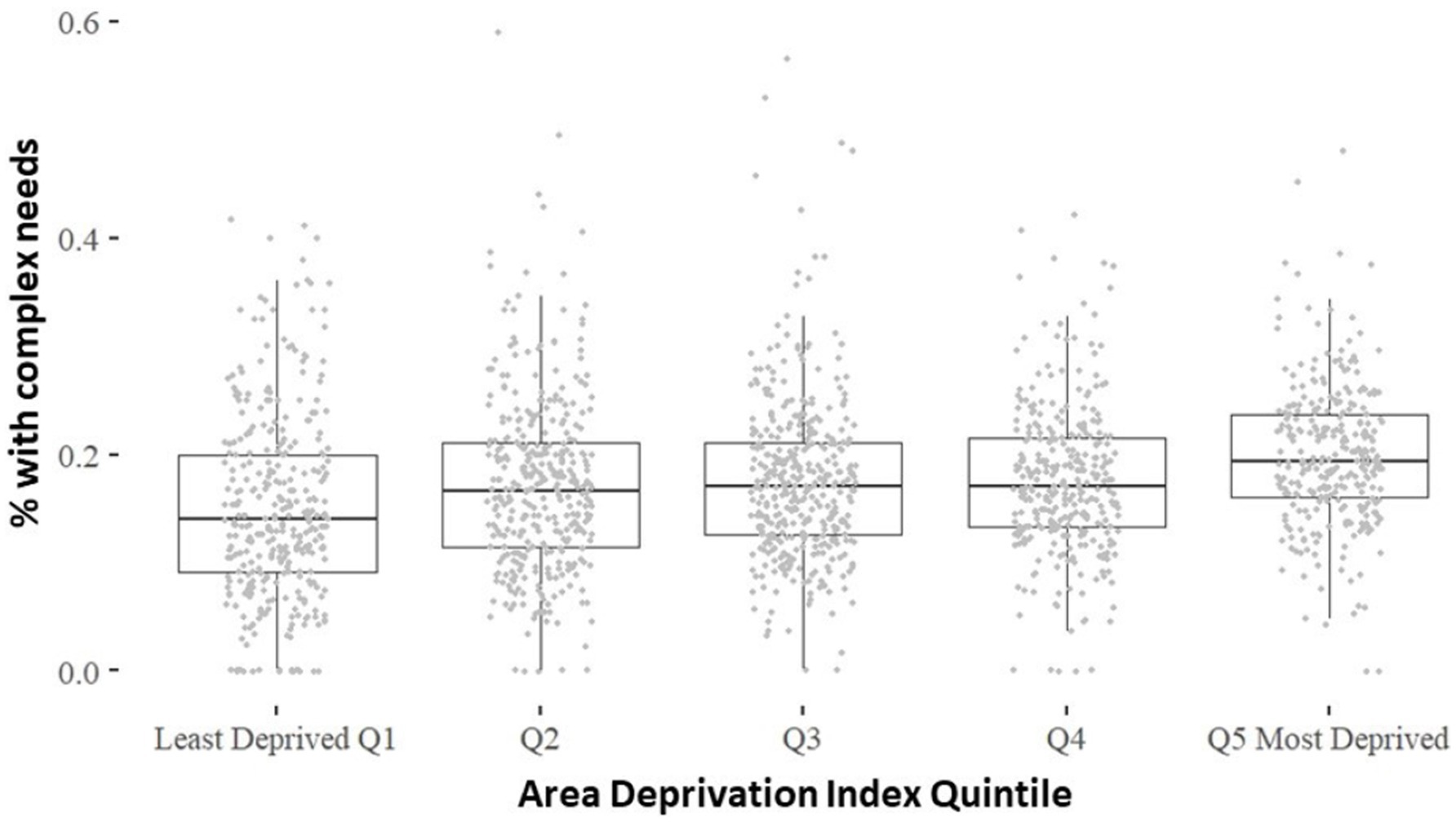
Figure 1. (p = 0.21, p < 0.001). * 1 physical condition with depression or 22 physical conditions with 21 mental health conditions.
Geospatial analysisThe bivariate spatial mapping of the prevalence of complex needs with the location of Medicaid-covered mental health facilities is presented in Figure 2. There was a statistically significant spatial autocorrelation of the prevalence of complex needs (Moran’s I index: 0.65; p < 0.001). This indicates that the high prevalence of beneficiaries with complex needs and the low prevalence of beneficiaries with complex needs are strongly consistent with clustering at the census block level. Among all census block groups, the median number of beneficiaries with complex needs was 12, and the median prevalence was 17%. The highest prevalence quantile (21.8–63.0%) contained 13,304 beneficiaries with complex needs. Within this group, 97 census blocks had the highest counts of beneficiaries with complex needs, totaling 7,250 beneficiaries. The median census block group prevalence of physical and mental health comorbidities in these blocks was 26%. The six census blocks with the highest counts of complex needs had no Medicaid-covered mental health facilities.
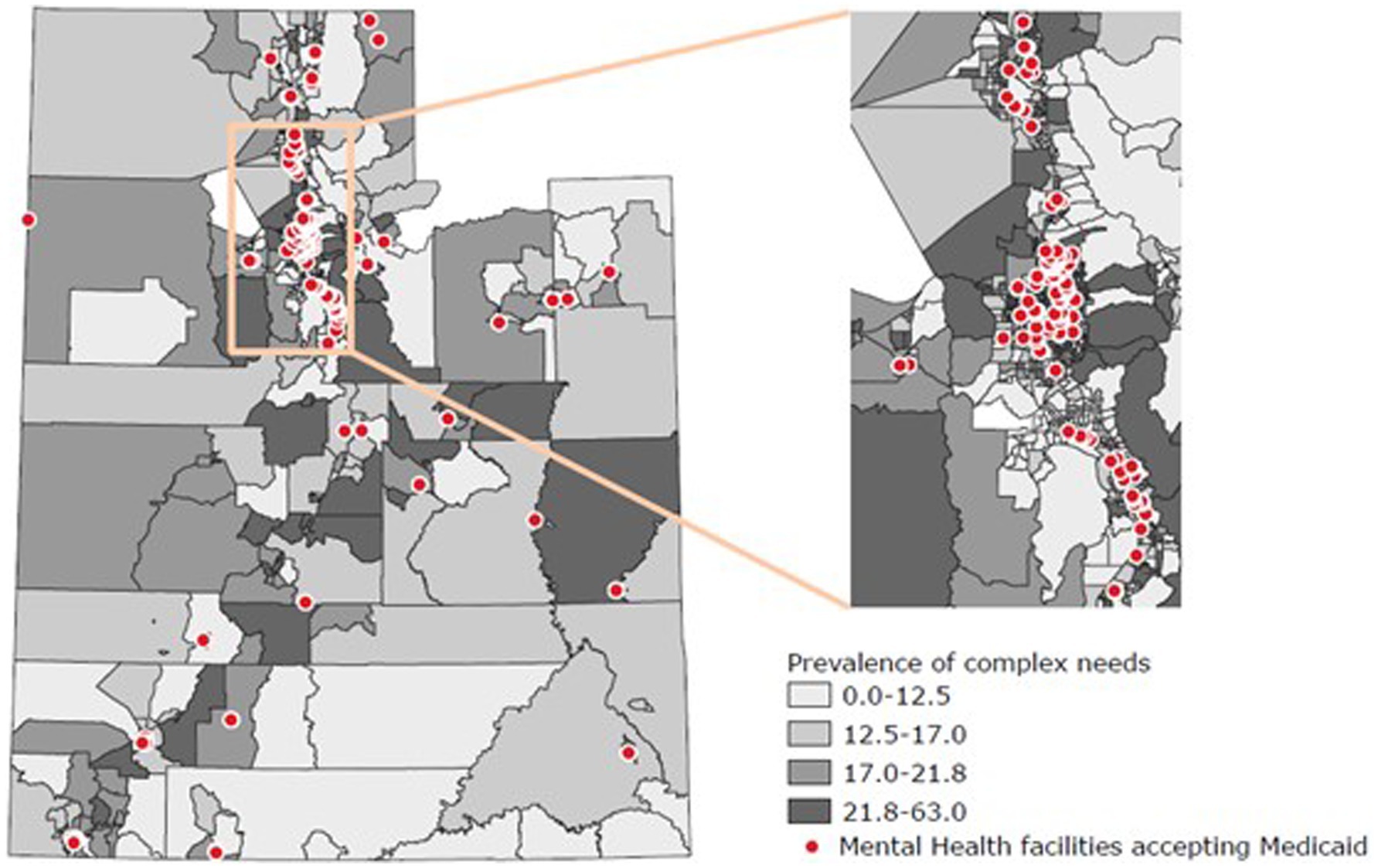
Figure 2. Spatial mapping of proportion of Medicaid adult beneficiaries with complex needs (physical and mental health comorbidities) by census block group and locations of mental health facilities accepting Medicaid — Utah, 2017.
DiscussionIn this study, we report that approximately one in five Medicaid adult beneficiaries in Utah had complex needs. This group of beneficiaries contributed disproportionately to the expenditure of resources as measured by the number of emergency department visits, the number of inpatient hospitalizations, and claims costs over the study period. Persons with >3 emergency department visits had approximately 13 times the odds of having complex needs than those with no visits, and persons with >$5,000 paid claims during this 12-month period had six times the odds of having complex needs than those with $1–$500 in paid claims.
Our analysis also demonstrated that at an ecological level, socioeconomic disparities were related to the prevalence of complex needs, with the proportion of beneficiaries with complex needs increasing with increasing socioeconomic deprivation at the census block group level. Our findings are consistent with the literature, which reports that people of low socioeconomic positions and communities with higher deprivation are more likely to be depressed and are more likely to have higher rates of obesity, diabetes, and chronic medical conditions (18). This is likely because beneficiaries living in higher deprivation communities often have greater exposure to stressors that negatively impact health, such as higher rates of pollution, crime, and unemployment, and lower access to services that can improve quality of life, such as safe housing, green spaces, and healthy food options. A United States-wide study of geospatial hotspots found that the highest-ranking census tracts in the nation exhibited poorer mental and physical health. Utah performed better than many other states, with fewer hotspots than neighboring states such as Nevada, New Mexico, and Arizona (19). Geographic conditions associated with disparity have a profound impact on psychological and behavioral factors that influence both physical and mental health (20).
The findings concerning the lack of mental health facilities in locations with high ADI were surprising. Other national-level studies have reported conversely that low-income areas have a higher proportion of outpatient mental health facilities (21). Nevertheless, studies that have reported on mental health providers (instead of facilities) have concluded that similar to our study, communities with higher deprivation have a shortage of mental health providers (22). Expansion of preventive and routine mental health services in underserved areas can result in substantial improvements to mental health and reductions in the use of emergency services and hospitalizations. Additional studies might contribute to an improved understanding of how the availability of mental health facilities in socially deprived regions influences mental and physical health outcomes in Utah.
LimitationsOur results cannot be generalized beyond the Utah Medicaid population; however, they do provide insight into the association between patients with complex medical needs and the ADI. Inherent bias exists in the use of aggregate characteristics as a proxy for individual deprivation (15). Furthermore, bias is introduced by reliance on healthcare services claims data. Beneficiaries with complex needs who did not have any medical claims in the defined period would have been undercounted, and it is not possible from the data to estimate the extent of this bias. A separate sensitivity analysis was conducted to exclude beneficiaries with no claims or those with <12 months of Medicaid eligibility, revealing no difference in conclusions. We identify the standard limitations of the modifiable area unit problem and the ecological fallacy of the spatial autocorrelation analysis. We also recognize that our analysis was limited to conditions listed in the Medicaid CCW, which is not an exhaustive list of possible chronic physical and mental health conditions. Because address geocoding was not possible for approximately 6.1% of beneficiaries, there might be an underrepresentation of high-deprivation socioeconomic groups that lack a permanent address. However, the prevalence of complex medical needs patients did not differ between beneficiaries with geocoded addresses and those without.
ConclusionThis study reports on 8% of adults residing in Utah (Utah adult population estimated to be 2,176,739 in 2017) (23). It describes a population that relies on state resources for healthcare needs. Our analysis reveals that areas with greater socioeconomic deprivation have greater comorbid physical and mental health needs and lower access to mental health facilities. In Utah, funding for public mental health services is decentralized, with regions or counties having autonomous local mental health authorities. Literature reveals that decentralization contributes to a lack of integration of physical and mental health services (24). For complex needs patients with mental and chronic physical health comorbidities, integrated healthcare systems might improve health outcomes and reduce use and costs (25). The development of integrated programs addressing both physical and mental health with a focus on socioeconomically deprived areas might benefit Medicaid recipients in populations such as those in Utah. The provision of integrated preventive and clinical care for beneficiaries with physical and mental health conditions might result in reduced high-cost services, such as unnecessary emergent care and inpatient hospitalizations.
Data availability statementThe data analyzed in this study is subject to the following licenses/restrictions: our study used restricted data from Medicaid Utah. Requests to access these datasets should be directed to Utah Department of Health and Human Services, TWVkaWNhaWRPcHNAdXRhaC5nb3Y=.
Ethics statementThe studies involving humans were approved by the Institutional Review Boards at the Utah Department of Health (Approval #533) and the Centers for Disease Control and Prevention (HSR #2018-00189) determined that this study did not constitute human subjects’ research. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation was not required from the participants or the participants’ legal guardians/next of kin in accordance with the national legislation and institutional requirements.
Author contributionsRH: Conceptualization, Formal analysis, Methodology, Validation, Visualization, Writing – original draft, Writing – review & editing. SB: Conceptualization, Formal analysis, Investigation, Methodology, Validation, Visualization, Writing – original draft, Writing – review & editing. CG: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Validation, Visualization, Writing – original draft, Writing – review & editing. NF: Supervision, Writing – original draft, Writing – review & editing. AD: Supervision, Writing – original draft, Writing – review & editing.
FundingThe author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interestThe authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s noteAll claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary materialThe Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2024.1454783/full#supplementary-material
References1. Blumenthal, D, Chernof, B, Fulmer, T, Lumpkin, J, and Selberg, J. Caring for high-need, high-cost patients—an urgent priority. N Engl J Med. (2016) 375:909–11. doi: 10.1056/NEJMp1608511
PubMed Abstract | Crossref Full Text | Google Scholar
2. Trivedi, RB, Post, EP, Sun, H, Pomerantz, A, Saxon, AJ, Piette, JD, et al. Prevalence, comorbidity, and prognosis of mental health among US veterans. Am J Public Health. (2015) 105:2564–9. doi: 10.2105/AJPH.2015.302836
PubMed Abstract | Crossref Full Text | Google Scholar
3. Boyd, C, Leff, B, Weiss, C, Wolff, J, Hamblin, A, and Martin, L. Full report: clarifying multimorbidity patterns to improve targeting and delivery of clinical services for medicaid populations. Hamilton, NJ: Center for Health Care Strategies, Inc (2010). 14 p.
5. Clarke, JL, Bourn, S, Skoufalos, A, Beck, EH, and Castillo, DJ. An innovative approach to health care delivery for patients with chronic conditions. Popul Health Manag. (2017) 20:23–30. doi: 10.1089/pop.2016.0076
PubMed Abstract | Crossref Full Text | Google Scholar
6. Katikireddi, SV, Skivington, K, Leyland, AH, Hunt, K, and Mercer, SW. The contribution of risk factors to socioeconomic inequalities in multimorbidity across the lifecourse: a longitudinal analysis of the Twenty-07 cohort. BMC Med. (2017) 15:152. doi: 10.1186/s12916-017-0913-6
PubMed Abstract | Crossref Full Text | Google Scholar
7. Pathirana, TI, and Jackson, CA. Socioeconomic status and multimorbidity: a systematic review and meta-analysis. Aust N Z J Public Health. (2018) 42:186–94. doi: 10.1111/1753-6405.12762
PubMed Abstract | Crossref Full Text | Google Scholar
8. Wilkness, S, Pandit, S, Arabo, F, Malone, S, and Tewarson, H. Building complex care programs: a road map for states. National Governors Association Center for Best Practices. (2017). Available at: https://classic.nga.org/files/live/sites/NGA/files/pdf/2017/ComplexCare_RoadMap_12.17_Health.pdf (Accessed December 6, 2018).
10. Johnson, TL, Rinehart, DJ, Durfee, J, Brewer, D, Batal, H, Blum, J, et al. For many patients who use large amounts of health care services, the need is intense yet temporary. Health Aff. (2015) 34:1312–9. doi: 10.1377/hlthaff.2014.1186
PubMed Abstract | Crossref Full Text | Google Scholar
11. Centers for Disease Control and Prevention, National Center for Health Statistics. ICD-9-CM – international classification of diseases, ninth revision, clinical modification. (2011). Available at: https://www.cdc.gov/nchs/icd/icd9cm.htm (Accessed January 10, 2019).
12. Centers for Disease Control and Prevention, National Center for Health Statistics. ICD-10-CM – international classification of diseases, tenth revision, clinical modification. (2017). Available at: https://www.cdc.gov/nchs/icd/icd10cm.htm (Accessed January 9, 2019).
14. Grafe, CJ, Horth, RZ, Clayton, N, Dunn, A, and Forsythe, N. How to classify super-utilizers: a methodological review of super-utilizer criteria applied to the Utah Medicaid population, 2016-2017. Popul Health Manag. (2020) 23:165–73. doi: 10.1089/pop.2019.0076
PubMed Abstract | Crossref Full Text | Google Scholar
15. Knighton, AJ, Savitz, L, Belnap, T, Stephenson, B, and VanDerslice, J. Introduction of an area deprivation index measuring patient socioeconomic status in an integrated health system: implications for population health. EGEMS. (2016) 4. doi: 10.13063/2327-9214.1238
Crossref Full Text | Google Scholar
16. Anselin, L. An introduction to spatial autocorrelation analysis with GeoDa. Illinois: Spatial Analysis Laboratory, University of Illinois, Champagne-Urbana, Illinois (2003).
19. Beauchamp, AM, Shen, GC, Hussain, SH, Adam, A, Highfield, L, and Zhang, K. Cultural context index: a geospatial measure of social determinants of health in the United States. SSM Popul Health. (2024) 25:101591. doi: 10.1016/j.ssmph.2023.101591
PubMed Abstract | Crossref Full Text | Google Scholar
20. Meyer, OL, Castro-Schilo, L, and Aguilar-Gaxiola, S. Determinants of mental health and self-rated health: a model of socioeconomic status, neighborhood safety, and physical activity. Am J Public Health. (2014) 104:1734–41. doi: 10.2105/AJPH.2014.302003
PubMed Abstract | Crossref Full Text | Google Scholar
21. Cummings, JR, Allen, L, Clennon, J, Ji, X, and Druss, BG. Geographic access to specialty mental health care across high-and low-income US communities. JAMA Psychiatry. (2017) 74:476–84. doi: 10.1001/jamapsychiatry.2017.0303
PubMed Abstract | Crossref Full Text | Google Scholar
22. Thomas, KC, Ellis, AR, Konrad, TR, Holzer, CE, and Morrissey, JP. County-level estimates of mental health professional shortage in the United States. Psychiatr Serv. (2009) 60:1323–8. doi: 10.1176/ps.2009.60.10.1323
PubMed Abstract | Crossref Full Text | Google Scholar
24. Hogan, MF. Perspective: public-sector mental health care: new challenges: decentralization and greater complexity may be barriers to improving quality in today’s public mental health systems. Health Aff. (1999) 18:106–11. doi: 10.1377/hlthaff.18.5.106
Crossref Full Text | Google Scholar
25. Reiss-Brennan, B, Brunisholz, KD, Dredge, C, Briot, P, Grazier, K, Wilcox, A, et al. Association of integrated team-based care with health care quality, utilization, and cost. JAMA. (2016) 316:826–34. doi: 10.1001/jama.2016.11232
留言 (0)