Sensorineural hearing loss (SNHL) is one of the most common types of hearing loss (HL), which affects social interactions and increases the likelihood of developing dementia and depression (Li et al., 2014; Mener et al., 2013; Livingston et al., 2020). SNHL is mainly caused by the impairment of non-renewable hair cells (HCs) and spiral ganglion neurons (SGNs) in the inner ear. Congenital gene mutations (Lv et al., 2021), prolonged noise exposure (Guo et al., 2021; Liberman, 2017), utilization of ototoxic medications (He et al., 2017; Lang et al., 2005; Liu et al., 2019), and aging (Bao and Ohlemiller, 2010; He et al., 2021; Kujawa and Liberman, 2015) are the major risk factors for SNHL. Hitherto, the specific pathophysiologic mechanisms of SNHL remain unclear. Since there is currently no effective treatment for almost all SNHL, patients can usually only rectify their hearing impairment through hearing aids and cochlear implants, but the patient experience is not ideal (Giraudet et al., 2018; Petit et al., 2023; Ferguson et al., 2017). Although different species of SNHL have distinct pathophysiologic mechanisms, their potential mechanisms often involve inner ear gene mutations, oxidative stress, apoptosis, inappropriate inflammation, and autophagy (Wong and Ryan, 2015). Accumulated data indicate that endoplasmic reticulum stress (ERS) plays a role in the above cellular processes and is involved in a variety of disease processes (Zhang et al., 2024). Recently, more and more studies have been conducted on the role of ERS in various types of SNHL, indicating that ERS plays a role in SNHL, which has potential therapeutic benefits for predicting pharmacological manipulations targeting ERS (Wu J. et al., 2020).
The endoplasmic reticulum (ER) in eukaryotes is an organelle comprising a continuous membrane; it is responsible for the processing, folding, and transportation of secreted and membrane-bound proteins, as well as the regulation of intracellular Ca2+ concentrations and formation of cell membrane lipids (Schwarz and Blower, 2016). It is believed that glucose deficiency, abnormal calcium regulation, hyperglycemia, hyperlipidemia, viral infections, and hypoxia contribute to the production and accumulation of unfolded/misfolded proteins (UFP/MFP), which leads to ERS (Fedoroff, 2006; Feldman et al., 2005; Fonseca et al., 2011; Görlach et al., 2006; Iurlaro and Muñoz-Pinedo, 2016; Kaufman et al., 2002; Sawada et al., 2008; Zhang and Wang, 2012). To restore ER homeostasis, the adaptive unfolded protein response (UPR) is activated (Hetz et al., 2020). However, when ERS is severe, oxidative stress, apoptosis, inflammation, and autophagy downstream of maladaptive UPR are activated and amplified, leading to cell damage or death (Iurlaro and Muñoz-Pinedo, 2016). It has been identified that ERS-induced cell death was involved in a variety of diseases, including neurodegenerative disorders (Duran-Aniotz et al., 2017; Valdés et al., 2014), cardiovascular ailments (Ren et al., 2021), and liver damage disorders (Zhang et al., 2022). In addition to the previously mentioned areas, research has highlighted the critical role of ERS in various forms of SNHL, including genetic, drug-induced, age-related, and noise-induced SNHL (Jia et al., 2018; Wen et al., 2021; Lee et al., 2021). The involvement of ERS across these diverse types of SNHL suggests its widespread and significant influence in this domain, although comprehensive reviews detailing the entire underlying mechanism remain lacking. Therefore, this review aims to elucidate the mechanisms and identify potential novel therapeutic targets of ERS in inner ear cells, hereby enhancing our understanding the role of ERS in SNHL and offering new perspectives for the treatment.
2 Molecular mechanisms underlying ERSThe key process of ERS is the UPR, which is mediated mainly by three transmembrane protein receptors located on the ER: pancreatic endoplasmic reticulum kinase (PERK), inositol-requiring enzyme 1α (IRE1α), and activating transcription factor 6 (ATF6). Typically, these three proteins combine with the heat shock protein 70 family member BiP (also referred to as GRP78) to maintain ER homeostasis. When ER homeostasis is disrupted, leading to ERS, BiP dissociates from its receptor proteins and binds to UFP/MFP, triggering oligomerization and phosphorylation of the three UPR receptor proteins (Ron and Walter, 2007). Cumulative UFP/MFP is degraded by ubiquitination via the endoplasmic reticulum-associated degradation (ERAD; Hetz et al., 2015). However, the adaptive capacity of the UPR is finite. When ERS is hard to mitigate within the cell, the pro-cell death responses downstream of the maladaptive UPR are activated and amplified, leading to tissue and organ damage (Figure 1; Hetz et al., 2020).
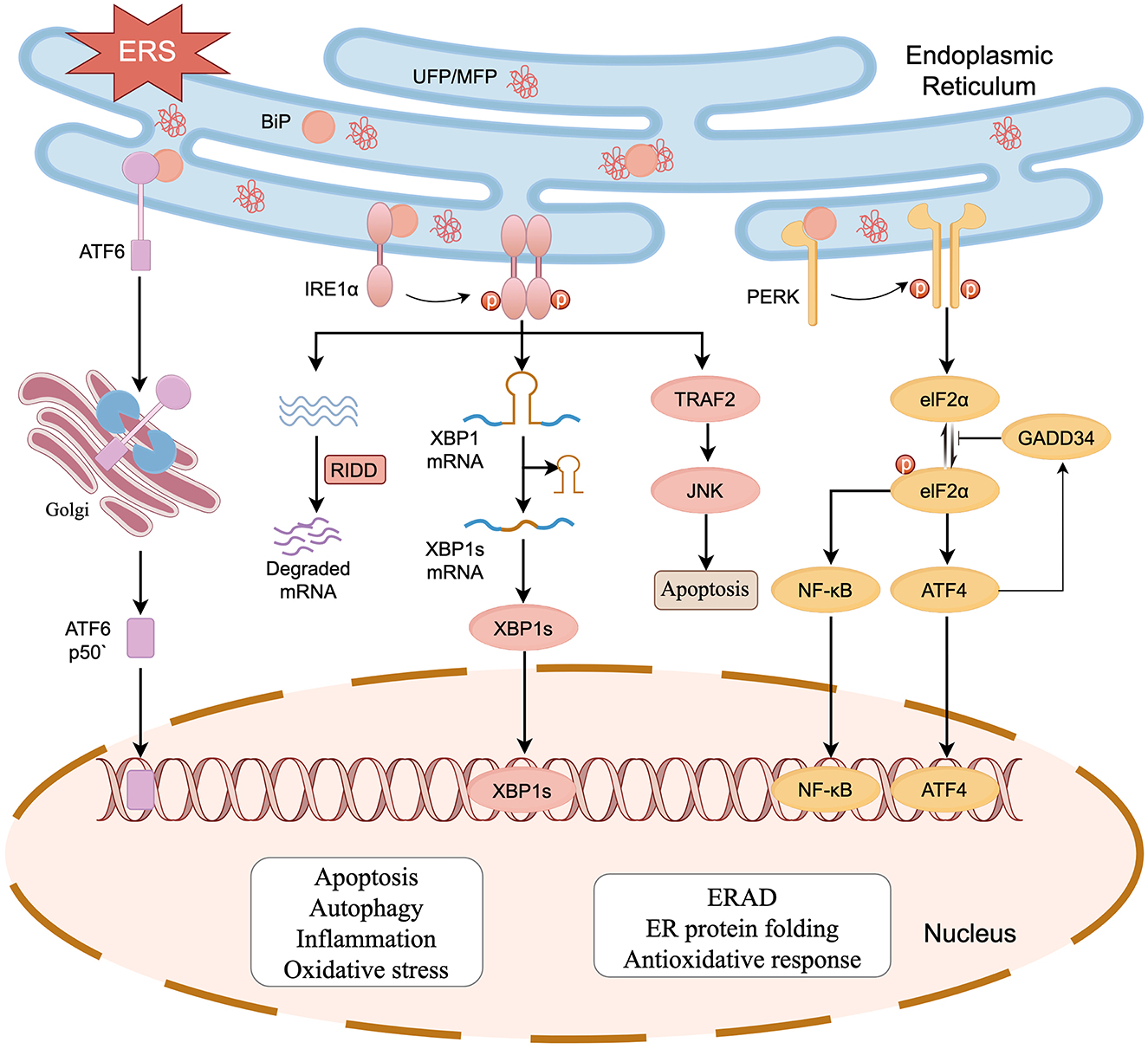
Figure 1. The UPR initiated by ERS in SNHL. Activation of the UPR is regulated by three transmembrane protein receptors: PERK, IRE1α, and ATF6. When UFP/MFP accumulates in the ER, BiP dissociates from PERK, IRE1α, and ATF6, after which it participates in the processing of UFP/MFP. PERK and IRE1α are activated by dimerization and phosphorylation. PERK phosphorylates eIF2α reducing protein translation. IRE1α exerts nucleic acid endonuclease activity and splices XBP1 mRNA. Meanwhile, IRE1α also breaks down a segment of mRNA via a biological mechanism known as regulated IRE1-dependent decay (RIDD), reducing the protein burden in the ER. ATF6 is spliced into ATF6P50 by the Golgi apparatus to exert its biological activity. The three activated receptor proteins also start the transcription of UPR in the nucleus. The cell damage and death responses downstream of UPR (e.g., oxidative stress, apoptosis, inflammation, and autophagy) can act on HCs, SGNs, and stria vascularis, which in turn leads to SNHL (figure drawn by Figdraw).
2.1 The IRE1α, PERK, and ATF6 signaling pathwaysIRE1α, a conserved ERS receptor expressed extensively in the ER membrane, comprises an N-terminal ER lumenal structural domain, a transmembrane region, and a C-terminal cytoplasmic region. The cytoplasmic region contains a site-specific nucleic acid endonuclease structural domain and a serine/threonine-protein kinase structural domain. During ERS, IRE1α detects UFP/MFP via its N-terminal luminal structural domain, separates from BiP and undergoes dimerization and phosphorylation, which activates the RNase structural domain. The activated IRE1α specifically recognizes and cleaves mRNA encoding X box binding protein 1 (XBP1), thereby initiating splicing of XBP1 mRNA to generate an XBP1 protein with transcription factor activity (Calfon et al., 2002; Shen et al., 2001; Yoshida et al., 2001). XBP1 upregulates the expression of genes related to protein transport, folding, secretion, and degradation (e.g., ERAD) in response to ERS and promotes adaptive cell survival (Kaufman, 2002; Yücel et al., 2019). IRE1α also breaks down a segment of mRNA via regulated IRE1-dependent decay (RIDD), thereby reducing the protein burden in the ER (Chen and Brandizzi, 2013). PERK is an ER transmembrane protein belonging to the serine/threonine kinase family and activated by its phosphorylation and dimerization, which in turn leads to phosphorylation of eukaryotic translation initiation factor 2 subunit-α (eIF2α), thereby reducing translation of most proteins and lowering the ER load (Ron and Walter, 2007; Kaufman, 2002). Phosphorylated elF2α promotes the expression of activating transcription factor 4 (ATF4; Blais et al., 2004; Harding et al., 1999). At the early stage of UPR, ATF4 upregulates the transcriptional expression of ER chaperone proteins to restore ER homeostasis. In the prolonged UPR state, ATF4 binds to UPR components and promotes the expression of C/EBP homologous protein (CHOP) to induce ATP depletion, oxidative stress, and apoptosis (Prasad and Greber, 2021). ATF4 also upregulates the expression of growth arrest and DNA damageinducible 34 (GADD34), which inhibits phosphorylation of eIF2α via negative feedback (Hetz et al., 2020). ATF6 is a type II transmembrane protein in the ER. In the case of ER homeostasis imbalance, ATF6 separates from BiP and enters the Golgi via vesicle transport, liberating a 50 kDa basic leucine zipper fragment known as “ATF6p50,” a process facilitated by site-1 protease (S1P) and site-2 protease (S2P). ATF6p50 is transported to the nucleus, resulting in the upregulation of UPR-associated proteins such as XBP1, CHOP, and ERAD components, thereby regulating protein homeostasis in cytoplasm (Haze et al., 1999; Ye et al., 2000; Jin et al., 2017).
2.2 ERS and oxidative stress, apoptosis, inflammation, and autophagyAn imbalance in redox homeostasis is one of the characteristics of ERS (Ron and Walter, 2007). CHOP can increase the expression of target genes such as ER oxidoreductase 1α (ERO1α) and GADD34, leading to the generation of oxidative stress. GADD34 induces the generation of reactive oxygen species (ROS) by upregulating synthesis of protein (Han et al., 2013; Marciniak et al., 2004). ERO1α is essential for the formation of disulfide bonds, which contribute to protein folding and transfer of electrons to molecular oxygen, thereby promoting the oxidation of ER proteins (Chen et al., 2015; Ramming et al., 2015). In addition, the UPR plays a role in PERK-mediated activation of nuclear factor erythroid 2-related factor (NRF2), which helps maintain glutathione levels, buffering the accumulation of ROS (Cullinan and Diehl, 2004; Cullinan et al., 2003; Figure 2A).
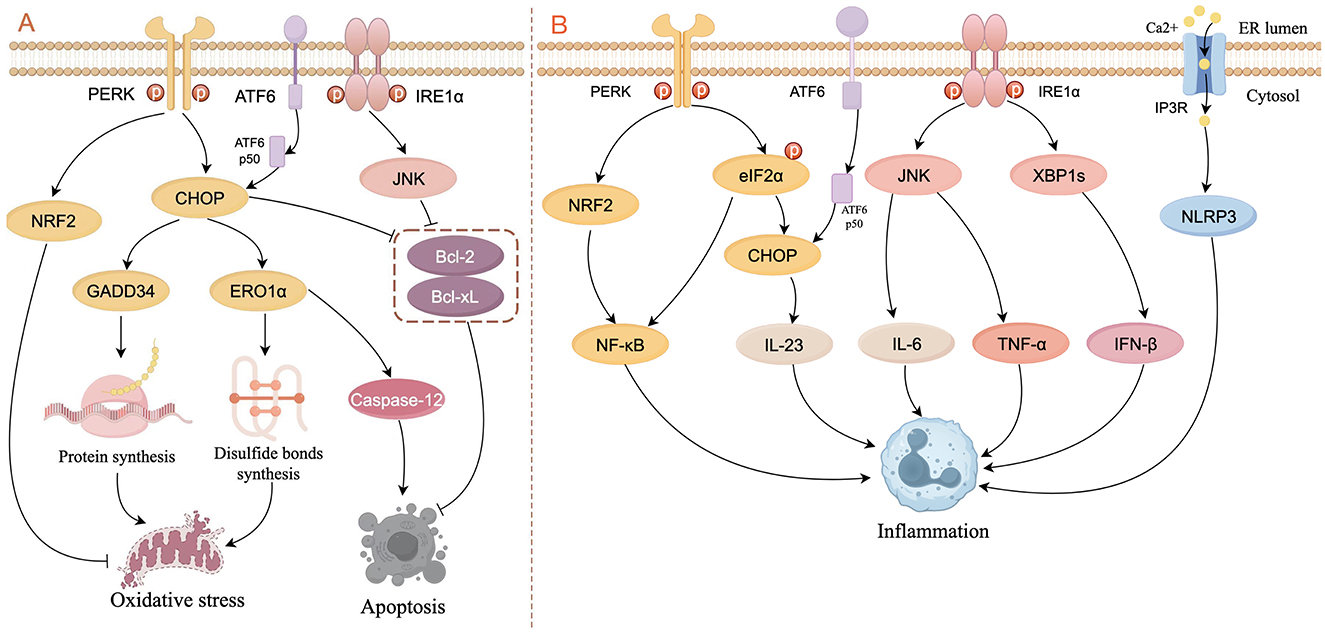
Figure 2. Schematic diagram of ERS signaling in the control of oxidative stress, apoptosis (A), and inflammation (B). (A) In the PERK pathway, CHOP activates GADD34 and ERO1α to respectively increase the formation of proteins and disulfide bonds, thereby leading to oxidative stress. CHOP also induces apoptosis by activating caspase-12 or inhibiting the activity of Bcl-2 and Bcl-xL. NRF2 is activated by PERK to inhibit oxidative stress. ATF6p50 increases apoptosis by up-regulating the expression of XBP1 and CHOP through the PERK pathway. The IRE1α/JNK pathway inhibits apoptosis by suppressing the activity of Bcl-2 and Bcl-xL. (B) In the PERK pathway, NRF2 and phosphorylated elF2α activate NF-κB to induce inflammation, and CHOP increases the expression of IL-23. In the IRE1α pathway, JNK increases the expression of IL-6 and TNF-α, and XBP1s increase the expression of IFN-β. ERS can result in the opening of the IP3R channel, thereby activating the NLRP3 inflammasome (figure drawn by Figdraw).
It is widely recognized that ERS-induced apoptotic signaling is mediated mainly by IRE1, PERK, and ATF6, which regulate B-cell lymphoma 2 (Bcl-2) family proteins directly or indirectly to activate intrinsic and caspase-induced apoptotic pathways. CHOP is considered to be an important factor in inducing apoptosis: not only does CHOP inhibit the expression of anti-apoptotic genes such as Bcl-2 (Tabas and Ron, 2011), but also activates the apoptosis-specific molecule caspase-12 in the ER by activating ERO1α, thereby initiating apoptosis activated by other caspase proteins (Gu et al., 2016; Wu H. et al., 2020; Nakagawa et al., 2000). Activated IRE1α recruits and activates the adapter molecule (i.e., TRAF2) of apoptosis signal-regulating kinase 1 (ASK1) and upregulates phosphorylation of c-Jun N-terminal kinase (JNK), which inhibits the expression of Bcl-2 and B-cell lymphoma-extra large (Bcl-xL), thereby promoting apoptosis (Urano et al., 2000; Saveljeva et al., 2015). ATF6p50 increases apoptosis by up-regulating the expression of XBP1 and CHOP through the PERK pathway (Yoshida et al., 2000). Studies have shown that apoptosis caused by overexpression of CHOP and GRP78, as well as activation of caspase-12, is associated with kidney injury (Gao et al., 2014; Kong et al., 2013). In another study in auditory cells, researchers demonstrate that ERS not only activates the apoptotic pathway mediated by caspase-3/caspase-9 but also induces receptor-interacting serine/threonine-protein kinase 1 (RIPK1)-mediated necroptosis (Saveljeva et al., 2015; Kishino et al., 2019; Figure 2A).
ERS and the UPR are involved extensively in inflammatory signaling. PERK activates NRF2 and phosphorylates eIF2α to upregulate the expression of nuclear factor kappa B (NF-κB), thereby inducing inflammation (Deng et al., 2004; Ma et al., 2024). IRE1 binds to the TRAF2-JNK pathway to induce pro-inflammatory cytokine expression (e.g., IL-6 and TNF-a; Kawasaki et al., 2012). Under conditions of ERS, the opening of the Ca2+ channel inositol 1,4,5-triphosphate receptor type 3 (IP3R) leads to active transport of Ca2+ between the ER and mitochondria, thereby activating the NLRP3 inflammasome (Li et al., 2020). In addition, XBP1 and CHOP stimulate inflammatory cytokine production directly by binding to cytokine promoter and enhancer elements (Goodall et al., 2010; Smith et al., 2008; Figure 2B).
Autophagy maintains cellular homeostasis in eukaryotes through the degradation and recycling of intracellular biomolecules and damaged organelles (Yang et al., 2016). Autophagy is linked to ERS and regulated by the UPR. Under hypoxia-induced ERS, ATF4, and CHOP increased the expression of microtubule-associated protein 1 light chain 3β (MAP1LC3B) and autophagy-regulated gene 5 (ATG5), thereby promoting autophagy (Rouschop et al., 2010). The PERK pathway induces autophagy by inhibiting the activity of mammalian target of rapamycin complex 1 (mTORC1), a core factor that inhibits autophagy, through the ATF4-mediated expression of Sestrin2 and DDIT4 genes (Brüning et al., 2013; Jin et al., 2009). In addition, PERK can also inhibit AKT1 or activate AMPK through CHOP, thereby inhibiting mTORC1 activity and promoting autophagy (Cybulsky, 2017; Ohoka et al., 2005; Rashid et al., 2015). Meanwhile, eIF2α-ATF4 promotes autophagy by binding to the amino acid response element (AARE) sequence of the p62 promoter (B'chir et al., 2013). In endothelial cells, autophagy is promoted by increasing the conversion of LC3I to LC3II via the IRE1α-XBP1 pathway (Margariti et al., 2013). The IRE1α-JNK pathway phosphorylates Bcl-2, which activates the Beclin1-PI3K complex to enhance autophagic responses (Heath-Engel et al., 2008; Wei et al., 2008). Tunicamycin (an ERS activator) causes splicing of XBP1 mRNA and triggers autophagy, which was confirmed by reports that knockdown of IRE1α, XBP1, and Forkhead box O1 (FoxO1) inhibited the increased expression of LC3-II; additionally the interaction between XBP1 and FoxO1 was confirmed to regulate ERS-induced autophagy in HEI-OC1 auditory cells (Kishino et al., 2017; Figure 3).
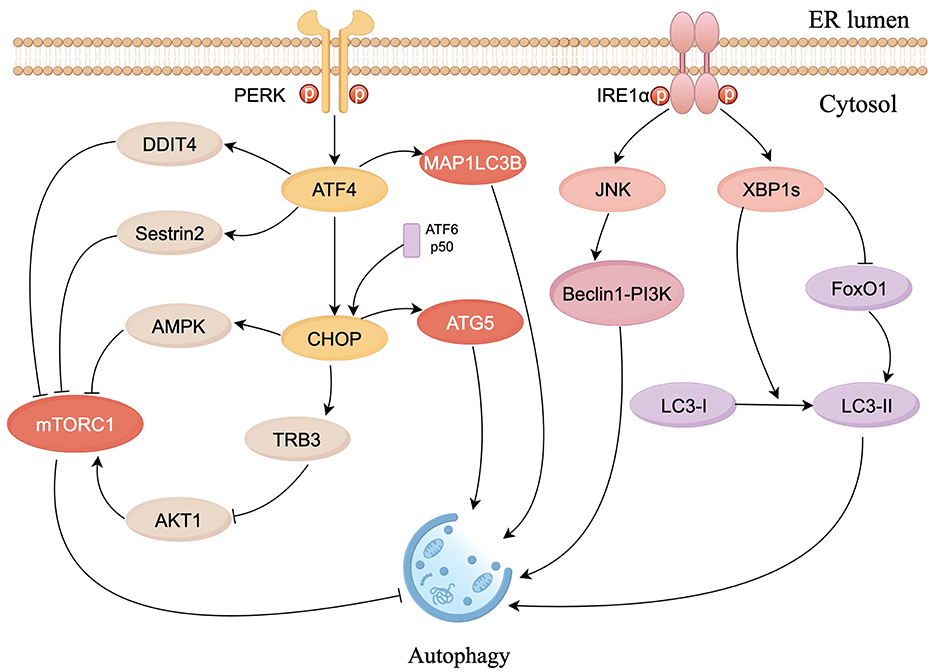
Figure 3. Schematic diagram of ERS signaling in the control of autophagy. The PERK pathway inhibits mTORC1 activity via ATF4 and CHOP to promote autophagy. CHOP constrains the phosphorylation of AKT1 by upregulating tribbles homolog 3 (TRB3) to inhibit mTORC1. ATF4 and CHOP also respectively activate MAP1LC3B and ATG5, to directly induce autophagy. IRE1α/JNK pathway activates Beclin1-PI3K complex to enhance autophagic responses. XBP1s can induce autophagy by facilitating LC3I to LC3II conversion and suppress autophagy by inhibiting FoxO1 (figure drawn by Figdraw).
Taken together, ERS is widely involved in multiple gene expressions, oxidative stress, apoptosis, inflammation and autophagy processes. Since the specific pathological mechanism of SNHL is still unclear, this suggests that ERS may participate in the occurrence and development of SNHL by communicating with the above biological processes.
3 ERS and SNHL 3.1 ERS in genetic SNHLApproximately 1 in 500 newborns are estimated to have congenital hearing loss, and more than half of such cases are attributable to genetic factors (Omichi et al., 2019). However, treatments to reverse or prevent genetic SNHL remain limited. Currently, there are over 250 genes linked to both syndromic and non-syndromic deafness (Carpena and Lee, 2018), and some of these genes and their protein products are tightly associated with ERS.
Usher syndrome (USH) is a condition in which patients with USH experience reduced hearing and congenital SNHL. USH is associated with three USH proteins: Cdh23, scaffold, and Myo7a. The absence of any one of these proteins contributes to the development of severe USH (Blanco-Sánchez et al., 2014; Bonnet and El-Amraoui, 2012). Studies conducted in zebrafish inner ear hair cells (HCs) demonstrate that the three USH proteins form a complex that regulates ER vesicular transportation in the HCs; inhibiting the synthesis of this complex leads to ERS and promotes apoptosis of HCs through the Cdk5- Mekk1-JNK pathway (Blanco-Sánchez et al., 2014; Kang et al., 2012). In addition, the mutation of Cdh23 gene induces apoptosis in HCs and is thought to be a pathological cause in patients with non-syndromic autosomal recessive deafness (DFNB12) and USH type 1D (USH1D; Bolz et al., 2001; Bork et al., 2001; Miyagawa et al., 2012; Han et al., 2012). Studies of a DFNB12 mouse model (erl mouse) in which deafness is caused by a Cdh23 point mutation revealed that expression of BiP and CHOP in outer hair cells (OHCs), SGNs, and stria vascularis increased significantly, and confirmed that apoptosis was inhibited significantly after CHOP knockout (Hu et al., 2016). P4-ATPase is a phospholipid flippase that selectively transports phospholipids from the ectoplasm to the cytoplasmic leaflet to maintain lipid membrane asymmetry (Coleman et al., 2009; Tang et al., 1996; Zhou and Graham, 2009). Deletion of proteins belonging to the P4-ATPase superfamily can lead to hearing disorders (Chepurwar et al., 2023; Coleman et al., 2014; Pater et al., 2022; Stapelbroek et al., 2009). Transmembrane protein 30A (TMEM30A) is one of the most common forms of P4-ATPase. Lack of TMEM30A disrupts HC planar polarity in the cochlea of mice, a process accompanied by an increase in ERS, as detected by increased expression of CHOP and BiP (Tone et al., 2020; Xing et al., 2023). Mesencephalic astrocyte-derived neurotrophic factor (MANF), located in the ER, mainly interacts with BiP to maintain protein folding homeostasis (Glembotski et al., 2012; Mizobuchi et al., 2007; Yan et al., 2019). Research shows that MANF is expressed in HCs and neurons, as well as in some non-sensory cells in the cochlea (Herranen et al., 2020). Meanwhile, in manf knockout mice, the OHCs gradually die soon after hearing formation, and expression of CHOP increases, indicating that MANF plays an important role in maintaining hearing by opposing ERS (Herranen et al., 2020). TMCC2 is an ER-resident transmembrane protein and is widely expressed in HCs of the mouse inner ear (Wisesa et al., 2019; Hoyer et al., 2018; Sohn et al., 2016; Zhang et al., 2014; Hopkins et al., 2011; Ren et al., 2023). Researchers performed auditory brainstem response (ABR) measurements on Tmcc2 knockout mice and showed that TMCC2 deletion leads to congenital HL. Further research has shown that the cause of HL is associated with a progressive loss of HCs. Meanwhile, an increase in ERS was observed in Tmcc2 knockout HCs, although the general morphology and functions of ER were not affected. This suggests that deletion of TMCC2 would likely lead to auditory HC death through increased ERS (Ren et al., 2023). Gap junctions facilitate intercellular communication and play an important role in maintaining cellular homeostasis (Cohen-Salmon et al., 2002; Simon and Goodenough, 1998). CX31, a significant component of gap junctions, is highly expressed in the inner ear HCs and SGNs of mice. Deficiency or malfunction of CX31 causes SNHL associated with upregulation of the chaperone protein BiP in the UPR pathway in HCs and SGNs (Xia et al., 2010; López-Bigas et al., 2001). This points to a potential connection between hearing impairment resulting from CX31 deficiency and ERS-induced death in the cochleae.
3.2 Drug-induced SNHL 3.2.1 Cisplatin-induced SNHLCisplatin is a common chemotherapeutic agent used to treat various types of cancer. The introduction of cisplatin into the inner ear triggers a cascade of events, including inflammation, oxidative stress, and DNA damage, leading ultimately to the death of HCs and subsequent SNHL (Qu et al., 2023). Cisplatin-induced apoptosis-associated activation of caspase-3 in the cytoplasm requires calcium, as well as activity of the calcium-dependent protease calpain, which is associated with ERS suggesting that the ER is a potential target for cisplatin (Mandic et al., 2003). Mandic et al. found that cisplatin induces calmodulin-dependent activation of the ER-specific caspase-12 in the cytoplasm, and increases expression of BiP (Mandic et al., 2003). Studies in cultured murine cochlear explants showed that cisplatin increases expression of BiP, CHOP, and caspase-3/9/12 in the inner ear, suggesting that cisplatin-induced apoptosis is associated with activation of the caspase-12 apoptotic pathway downstream of the UPR (Xiao et al., 2016). The expression of ATF4 and CHOP increases progressively in cisplatin-treated hair cell-like OC1 cells, and cisplatin toxicity is reduced significantly in chop-knockout cells indicating that the PERK/ATF4/CHOP pathway is involved in cisplatin-mediated ototoxicity (Qu et al., 2023). The protein arginine methyltransferase 3 (PRMT3) and cannabinoid systems are involved in cisplatin-induced ototoxicity associated with ERS, and apoptotic signaling (including caspase-3, caspase-9, poly-adenosine diphosphate-ribose polymerase, and phospho-p53) is enhanced, in HEI-OC1 cells (Lim et al., 2019). Overexpression of PRMT3 or FAAH1 increased apoptosis and ERS signaling, whereas knockdown of PRMT3 or the activation of cannabinoid 1 receptor (CB1R) and inhibition of FAAH1 mitigated cisplatin ototoxicity (Lim et al., 2019). ERS is involved in cisplatin-induced ototoxicity through activation of ER autophagy proteins (Gentilin et al., 2019); indeed, the ER autophagy receptor FAM134B has been shown to promote ER autophagy during ERS (Mo et al., 2020). Increased expression of LC3B in cisplatin-treated HEI-OC1 cells correlates with time-dependent expression of ER autophagy receptor FAM134B (Yang et al., 2023). Knockdown of FAM134B decreases cisplatin-induced autophagy, and attenuates ERS as well as expression of apoptotic factors, suggesting that FAM134B-induced autophagy in the ER is an important pathway in cisplatin-mediated ototoxicity (Yang et al., 2023).
3.2.2 Aminoglycoside antibiotic-induced SNHLAn overdose of Aminoglycoside antibiotic (AmAn) causes significant ototoxicity by inhibiting protein synthesis and inducing ROS in host cells, leading to apoptosis of HCs (Francis et al., 2013; Shulman et al., 2014; Xie et al., 2011). Oishi et al. conducted genome-wide transcriptomic and proteomic analyses and reported a substantial increase in the expression of BiP, GRP94, ATF4, and calreticulin in the gentamicin-treated group (Oishi et al., 2015). Furthermore, gentamicin significantly reduces the number of SGNs in XBP1 haploid mice (Oishi et al., 2015). Tu et al. discovered that chronic kanamycin induces extensive apoptosis in SGNs, which correlates positively with the expression level of caspase-12 (Tu et al., 2019). These studies indicate that SGNs are an important target for AmAn drugs, resulting in ototoxicity via ERS. In addition, Wu et al., found that neomycin induced significant apoptosis in HEI-OC1 cells through the PERK/eIF2α/ATF4 pathway (Wu et al., 2022). Thus, AmAn causes damage to inner ear HCs and SGNs by promoting the ERS pathway, leading to ototoxicity.
3.2.3 Other types of drug-related SNHLAcetaminophen (APAP) is a non-steroidal anti-inflammatory drug and has ototoxic side effects (Blakley and Schilling, 2008; Curhan et al., 2010, 2012). A metabolite of APAP, N-acetyl-P-benzoquinone imine (NAPQI), causes damage to the ER and triggers ERS (Ramachandran and Jaeschke, 2018; Xiaomeng et al., 2020). Kalinec et al. demonstrated that APAP and NAPQI trigger ERS and ototoxicity in HEI-OC1 cells via the PERK/eIF2α/CHOP pathway, and found that the PERK pathway-mediated cell death pathway was independent of ATF4 (Kalinec et al., 2014). This implies that ototoxicity induced by APAP is a result of ERS-induced death signaling via a different pathway (Kalinec et al., 2014). Pyridoxine, also known as vitamin B6, can cause peripheral neuropathy (Schaumburg et al., 1983). In 2019, Park et al. discovered that treatment of an auditory neuroblastoma cell line with a surplus of pyridoxine resulted in elevated ROS levels, mitochondrial dysfunction, and upregulation of UPR (including p-PERK, GRP78, CHOP, and caspase-12; Park et al., 2019). This indicates that the administration of excess pyridoxine may contribute to the impairment of auditory nerve cells through the ERS-induced apoptotic pathway, potentially leading to SNHL. However, whether apoptosis is directly mediated by ERS still needs to be further verified.
3.3 Age-related hearing lossAge-related hearing loss (ARHL) arises in conjunction with the natural progression of aging, resulting in significant morbidity (Eggermont et al., 2017). Chronic ERS is part of the aging process. Wang et al. found that accumulation of ubiquitinated proteins, as well as reduced expression of BiP and high expression of CHOP and caspase3/9, occurs in the cochlea of mice aged 12–14 months (Wang et al., 2015). Lee et al. conducted in vitro and in vivo experiments, which revealed that in the cochlea aging causes a substantial reduction in the expression of heat shock proteins, including HSF1, HSP70, and HSP40, all of which are essential for preserving ER balance; in addition, expression of p-eIF2α and CHOP increases as that of HSF1 falls (Lee et al., 2021). These studies suggest that ERS is involved in the progression of cochlear senescence and that strategies aimed at reducing ERS-dependent apoptosis in the aging cochlea could play a role in preventing ARHL.
3.4 Noise-induced hearing lossNoise-induced hearing loss (NIHL) is the most common occupational disease in many Asian countries (Fuente and Hickson, 2011). Previous studies have confirmed that cochlear cells undergo apoptosis and necrosis during the pathogenesis of NIHL, although the exact process is unclear. One study in guinea pigs explored the role of ERS in cochlear damage induced by exposure to intense noise. Both ER-related BiP and CHOP levels in the cochlea were elevated significantly after exposure to noise, accompanied by marked apoptosis, necrosis, and degeneration of OHCs (Xue et al., 2016). Researchers speculated that the ERS response was activated by inducing BiP to mitigate noise-induced damage to cochlear cells and that the CHOP pathway was activated to eliminate the most severely injured cells (Xue et al., 2016). TMTC4 is expressed extensively in the ER and plays a role in regulating Ca2+ dynamics and the UPR (Li et al., 2018). Inactivation of the gene tmtc4 led to the development of NIHL in mice; however, concomitant knockdown of chop attenuates HL (Li et al., 2018). These studies demonstrate the direct link between NIHL and ERS, but the role of ERS in NIHL still requires further research for clarification.
To sum up the above, hearing loss caused by genetics, drugs, noise and aging is related to ER homeostasis in inner ear cells, and furthermore, most studies have shown that SNHL is positively correlated with ERS. It is important to note that studies still lack evidence of a direct causal relationship between SNHL and ERS. Although the specific mechanism remains uncertain, ERS shows a strong correlation with SNHL. Thus, it appears that ERS has considerable potentiality for the study of mechanisms underlying SNHL and provides new potential targets for the treatment.
4 Potential targets and strategies against ERS for SNHLIn recent years, scientists and clinicians have conducted numerous studies on ERS-mediated mechanisms of SNHL to identify therapeutic measures that target the mechanism underlying activation of the ERS response (Figure 4). The UPR is an important pathway in ERS-induced SNHL, in which the PERK/eIF2α/ATF4 pathway plays a central role. Several novel treatment strategies for SNHL have been proposed (Table 1). Salubrinal (Sal), a selective protein phosphatase I complex inhibitor, reduces HCs apoptosis in erl mice by inhibiting expression of BiP, CHOP, and caspase-3 in OHCs, SGNs, and stria vascularis (Hu et al., 2016). Thus, Sal is a promising option for patients with early DFNB12 and USH. Sal also inhibits cisplatin-induced cochlear cell apoptosis by dephosphorylating eIF2α, and by decreasing BiP and CHOP expression (Lu et al., 2022). Pitavastatin (PTV), a new-generation lipophilic statin, attenuates neomycin-induced ototoxicity by reducing the phosphorylation of PERK and eIF2α (Wu et al., 2022). Meanwhile, in vivo and in vitro experiments show that PTV reduces the expression of GRP78 and CHOP to suppress neomycin-induced ERS (Wu et al., 2022). Taurine ursodeoxycholic acid (TUDCA) is a co-cholestatic acid. Researchers found that the addition of TUDCA to gentamicin-induced cochlear explants alleviates ERS by inhibiting overexpression of BiP, CHOP, and caspase 3 (Jia et al., 2018). Studies also show that TUDCA reduces cisplatin-induced SNHL by increasing the efficacy of UFP/MFP processing in the ER (Wen et al., 2021). In 2023, Sun et al. conducted single-cell transcription experiments on cells from the cochlea and found that: (1) loss of protein homeostasis and apoptosis are the hallmark of ARHL; and (2) upregulation of the ER chaperone protein, HSP90AA1, alleviates damage to the cochlea caused by aging (Sun et al., 2023). Interestingly, it is the UPR that connects the loss of protein homeostasis with apoptosis. This suggests that ERS-induced apoptosis via UPR has enormous research potential in the context of ARHL. Inhibiting the apoptosis mediated by maladaptive UPR could be a novel treatment option for ARHL.
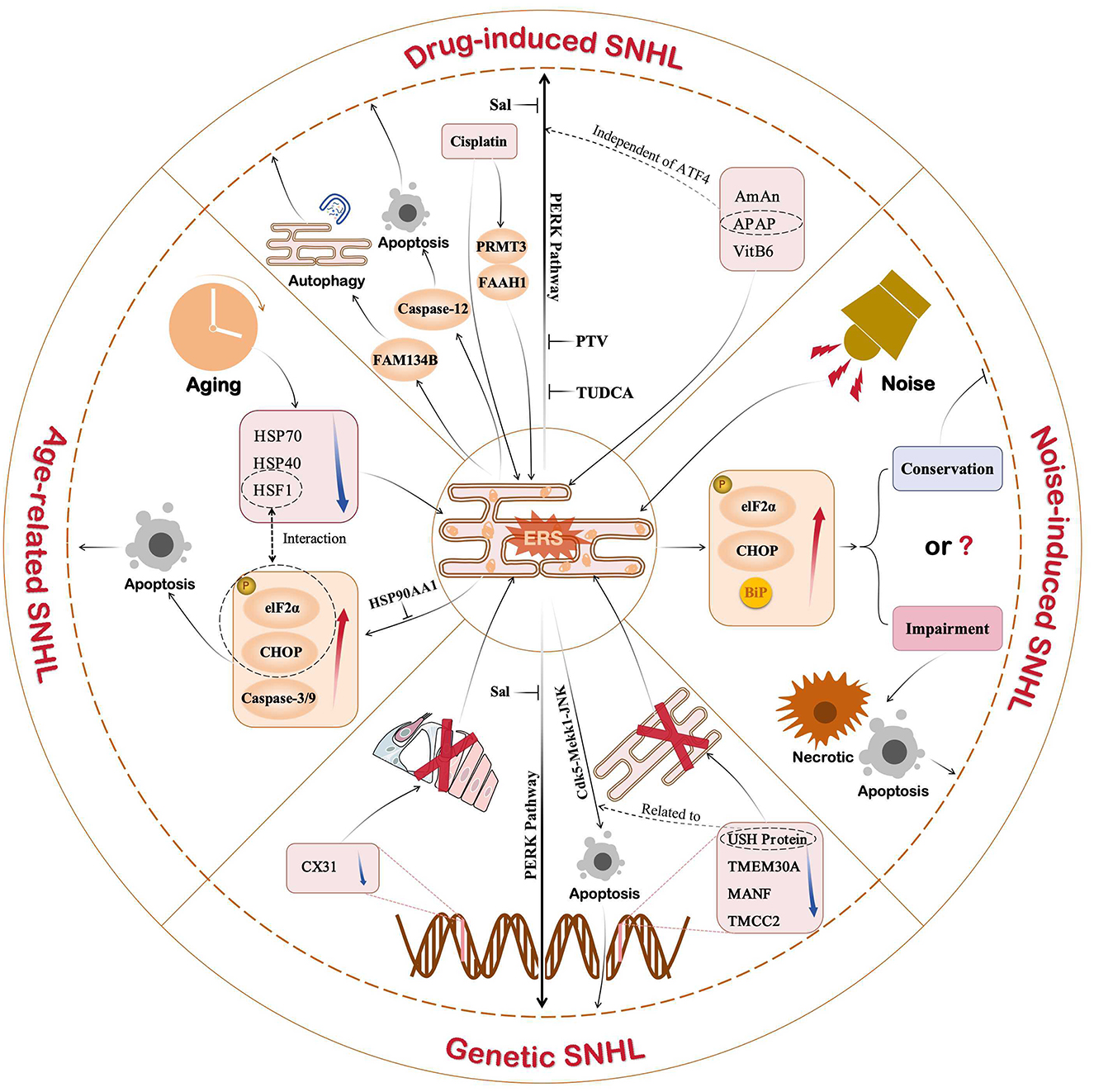
Figure 4. Role of ERS in different types of SNHL. Current studies show that ERS is associated with drug-induced, noise-induced, age-induced, or genetic SNHL. In addition to noise-induced SNHL, ERS shows a strong correlation with SNHL. Of the three UPR pathways, the PERK pathway plays an important role in SNHL. Therefore, drugs targeting the PERK pathway, such as Sal, PTV, and TUDCA, are promising new ideas for SNHL.
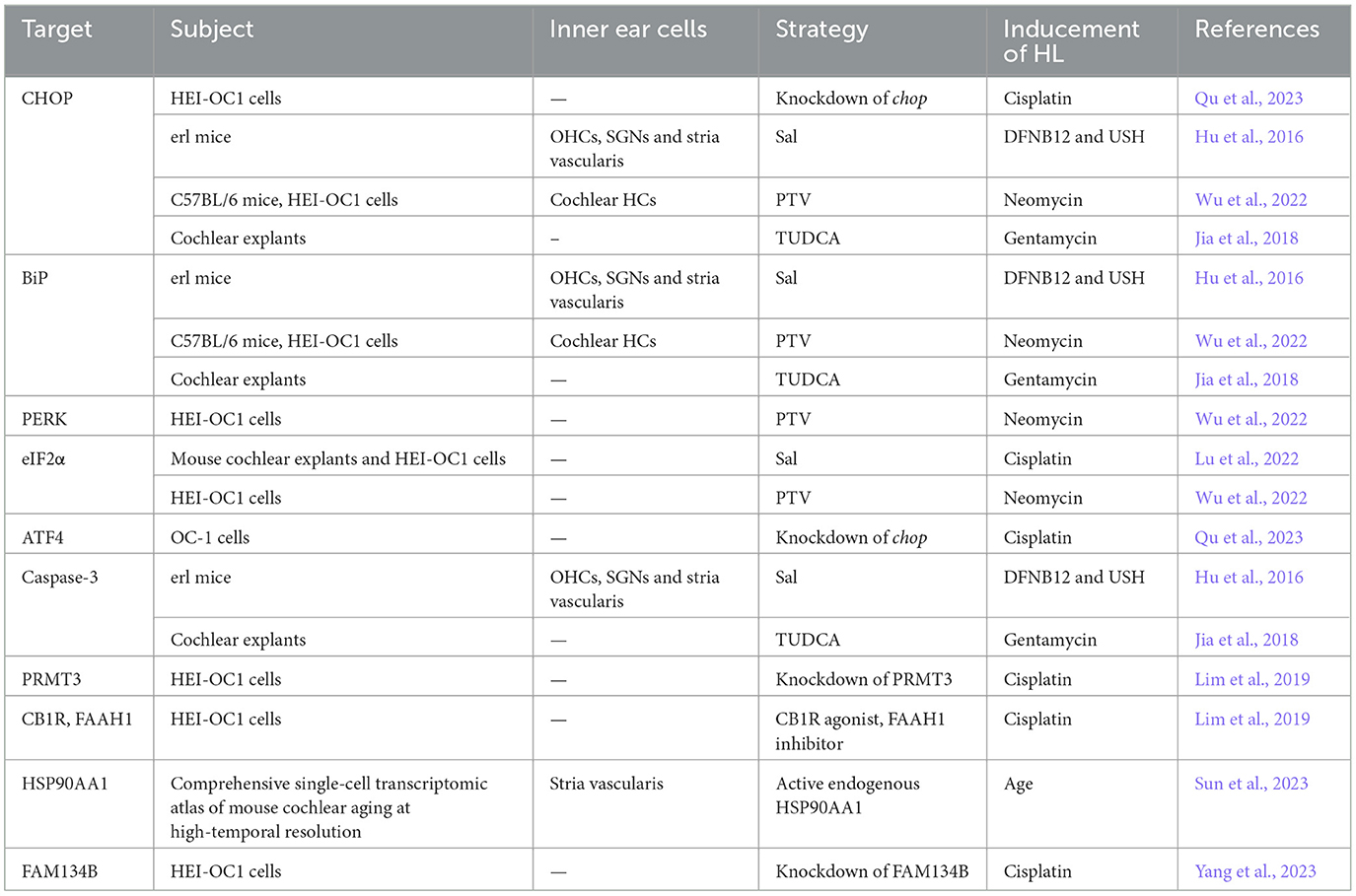
Table 1. Potential targets and treatment strategies for ERS-mediated SNHL.
5 Conclusions and future prospectsER stress is a ubiquitous etiological mechanism involved in a variety of disease processes. Under the influence of genetic and environmental factors, ERS participates in the pathogenesis of SNHL by regulating cell function and fate through extensive communication with the biological processes behind gene expression, oxidative stress, apoptosis, inflammation and autophagy. An increasing amount of research has elucidated that ERS-induced cell death in the inner ear is essential in SNHL, suggesting a positive correlation between ERS and SNHL; however, the specific causal relationship between the two has yet to be clarified. There still remain several unclear questions, such as which cells in the inner ear are mainly affected by ERS and through which specific pathway does the UPR cause damage to the inner ear? Even though numerous medications appear to reduce ERS, they have only been tested in animals and cells, and there remains a notable lack of clinical trials. To sum up, ERS is a novel therapeutic focus in the context of SNHL and has tremendous research potential. The question of how to balance the protective and disease-causing arms of the UPR needs to be considered when identifying/designing new drugs for SNHL treatment. All abbreviations of specialized terminology included in this article are summarized in a table (Table 2).
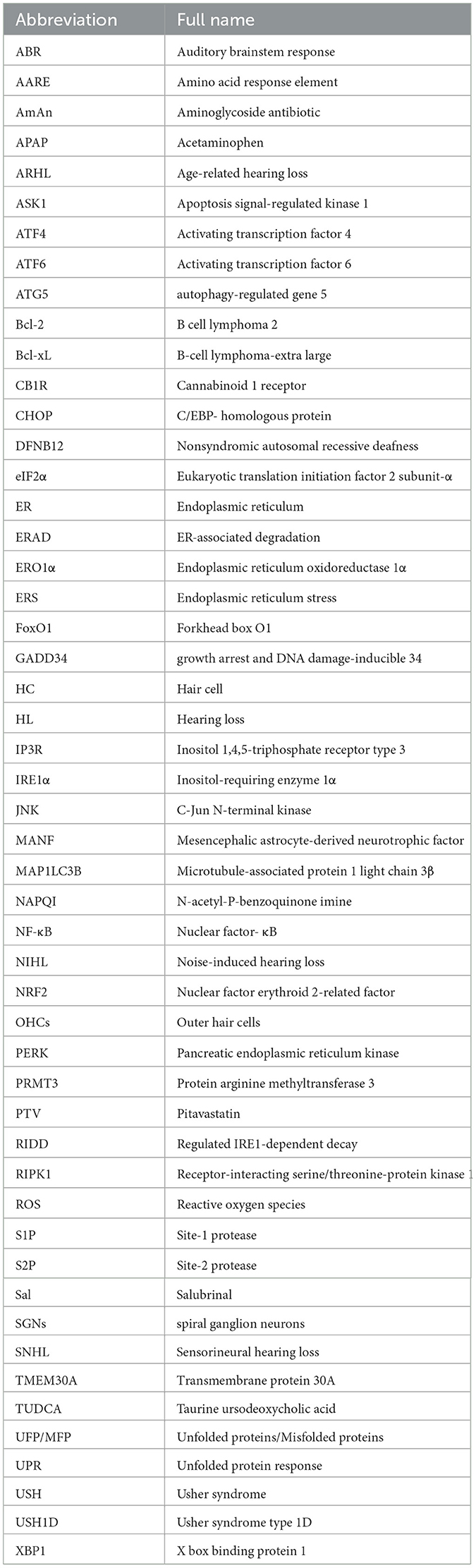
Table 2. List of abbreviations.
Author contributionsGL: Conceptualization, Visualization, Writing – original draft, Writing – review & editing. HY: Visualization, Writing – review & editing. PZ: Data curation, Writing – review & editing, Visualization. YG: Writing – review & editing. LY: Writing – review & editing. SX: Writing – review & editing. YY: Writing – review & editing. HX: Funding acquisition, Writing – review & editing. HY: Funding acquisition, Methodology, Supervision, Writing – review & editing.
FundingThe author(s) declare financial support was received for the research, authorship, and/or publication of this article. This work was supported by the National Natural Science Foundation of China, granted by Nos. 82000979 and 82201293, the Fund of Lin He Academician Workstation of Jining Medical University granted by No. JYHL2019MS13, and the National College Students Innovation and Entrepreneurship Training Program granted by No. S202410443014.
AcknowledgmentsWe would like to thank Melissa Chaehyun Lee of Stanford University for improving some grammatical expressions and correcting spelling errors during the revision process.
Conflict of interestThe authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's noteAll claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
ReferencesB'chir, W., Maurin, A.-C., Carraro, V., Averous, J., Jousse, C., Muranishi, Y., et al. (2013). The eIF2alpha/ATF4 pathway is essential for stress-induced autophagy gene expression. Nucleic Acids Res. 41, 7683–7699. doi: 10.1093/nar/gkt563
PubMed Abstract | Crossref Full Text | Google Scholar
Blais, J. D., Filipenko, V., Bi, M., Harding, H. P., Ron, D., Koumenis, C., et al. (2004). Activating transcription factor 4 is translationally regulated by hypoxic stress. Mol. Cell Biol. 24, 7469–7482. doi: 10.1128/MCB.24.17.7469-7482.2004
PubMed Abstract | Crossref Full Text | Google Scholar
Blakley, B. W., and Schilling, H. (2008). Deafness associated with acetaminophen and codeine abuse. J. Otolaryngol. Head Neck Surg. 37, 507–509. doi: 10.2310/7070.2008.0096
Crossref Full Text | Google Scholar
Blanco-Sánchez, B., Clément, A. Jr. J. F., Washbourne, P., and Westerfield, M. (2014). Complexes of Usher proteins preassemble at the endoplasmic reticulum and are required for trafficking and ER homeostasis. Dis. Model Mech. 7, 547–559. doi: 10.1242/dmm.014068
PubMed Abstract | Crossref Full Text | Google Scholar
Bolz, H., von Brederlow, B., Ramírez, A., Bryda, E. C., Kutsche, K., Nothwang, H. G., et al. (2001). Mutation of CDH23, encoding a new member of the cadherin gene family, causes Usher syndrome type 1D. Nat. Genet. 27, 108–112. doi: 10.1038/83667
PubMed Abstract | Crossref Full Text | Google Scholar
Bonnet, C., and El-Amraoui, A. (2012). Usher syndrome (sensorineural deafness and retinitis pigmentosa): pathogenesis, molecular diagnosis and therapeutic approaches. Curr. Opin. Neurol. 25, 42–49. doi: 10.1097/WCO.0b013e32834ef8b2
PubMed Abstract | Crossref Full Text | Google Scholar
Bork, J. M., Peters, L. M., Riazuddin, S., Bernstein, S. L., Ahmed, Z. M., Ness, S. L., et al. (2001). Usher syndrome 1D and nonsyndromic autosomal recessive deafness DFNB12 are caused by allelic mutations of the novel cadherin-like gene CDH23. Am. J. Hum. Genet. 68, 26–37. doi: 10.1086/316954
PubMed Abstract | Crossref Full Text | Google Scholar
Brüning, A., Rahmeh, M., and Friese, K. (2013). Nelfinavir and bortezomib inhibit mTOR activity via ATF4-mediated sestrin-2 regulation. Mol. Oncol. 7, 1012–1018. doi: 10.1016/j.molonc.2013.07.010
PubMed Abstract | Crossref Full Text | Google Scholar
Calfon, M., Zeng, H., Urano, F., Till, J. H., Hubbard, S. R., Harding, H. P., et al. (2002). IRE1 couples endoplasmic reticulum load to secretory capacity by processing the XBP-1 mRNA. Nature 415, 92–96. doi: 10.1038/415092a
PubMed Abstract | Crossref Full Text | Google Scholar
Chen, B. L. (2015). CCAAT-enhancer-binding protein homologous protein deficiency attenuates oxidative stress and renal ischemia-reperfusion injury. Antioxid Redox Signal 23, 1233–1245. doi: 10.1089/ars.2013.5768
PubMed Abstract | Crossref Full Text | Google Scholar
Chepurwar, S., von Loh, S. M., Wigger, D. C., Neef, J., Frommolt, P., Beutner, D., et al. (2023). A mutation in ATP11A causes autosomal-dominant auditory neuropathy type 2. Hum. Mol. Genet. 32, 1083–1089. doi: 10.1093/hmg/ddac267
PubMed Abstract | Crossref Full Text | Google Scholar
Cohen-Salmon, M., Ott, T., Michel, V., Hardelin, J. P., Perfettini, I., Eybalin, M., et al. (2002). Targeted ablation of connexin26 in the inner ear epithelial gap junction network causes hearing impairment and cell death. Curr. Biol. 12, 1106–1111. doi: 10.1016/S0960-9822(02)00904-1
PubMed Abstract | Crossref Full Text | Google Scholar
Coleman, J. A., Kwok, M. C., and Molday, R. S. (2009). Localization, purification, and functional reconstitution of the P4-ATPase Atp8a2, a phosphatidylserine flippase in photoreceptor disc membranes. J. Biol. Chem. 284, 32670–32679. doi: 10.1074/jbc.M109.047415
PubMed Abstract | Crossref Full Text | Google Scholar
Coleman, J. A., Zhu, X., Djajadi, H. R., Molday, L. L., Smith, R. S., Libby, R. T., et al. (2014). A phospholipid flippase ATP8A2 is required for normal visual and auditory function and photoreceptor and spiral ganglion cell survival. J. Cell Sci. 127, 1138–1149. doi: 10.1242/jcs.145052
PubMed Abstract | Crossref Full Text | Google Scholar
Cullinan, S. B., and Diehl, J. A. (2004). PERK-dependent activation of Nrf2 contributes to redox homeostasis and cell survival following endoplasmic reticulum stress. J. Biol. Chem. 279, 20108–20117. doi: 10.1074/jbc.M314219200
PubMed Abstract | Crossref Full Text | Google Scholar
Cullinan, S. B., Zhang, D., Hannink, M., Arvisais, E., Kaufman, R. J., and Diehl, J. A. (2003). Nrf2 is a direct PERK substrate and effector of PERK-dependent cell survival. Mol. Cell Biol. 23, 7198–7209. doi: 10.1128/MCB.23.20.7198-7209.2003
PubMed Abstract | Crossref Full Text | Google Scholar
Curhan, S. G., Eavey, R., Shargorodsky, J., and Curhan, G. C. (2010). Analgesic use and the risk of hearing loss in men. Am. J. Med. 123, 231–237. doi: 10.1016/j.amjmed.2009.08.006
PubMed Abstract | Crossref Full Text | Google Scholar
Deng, J., Lu, P. D., Zhang, Y., Scheuner, D., Kaufman, R. J., Sonenberg, N., et al. (2004). Translational repression mediates activation of nuclear factor kappa B by phosphorylated translation initiation factor 2. Mol. Cell Biol. 24, 10161–10168. doi: 10.1128/MCB.24.23.10161-10168.2004
PubMed Abstract | Crossref Full Text | Google Scholar
Duran-Aniotz, C., Cornejo, V. H., Espinoza, S., Ardiles, Á. O., Medinas, D. B., Salazar, C., et al. (2017). IRE1 signaling exacerbates Alzheimer's disease pathogenesis. Acta Neuropathol. 134, 489–506. doi: 10.1007/s00401-017-1694-x
留言 (0)