This work may not be copied, distributed, displayed, published, reproduced, transmitted, modified, posted, sold, licensed, or used for commercial purposes. By downloading this file, you are agreeing to the publisher’s Terms & Conditions.
AbstractObjective: To evaluate a novel curriculum aimed to increase nonpsychiatry providers’ confidence in treating mental health conditions.
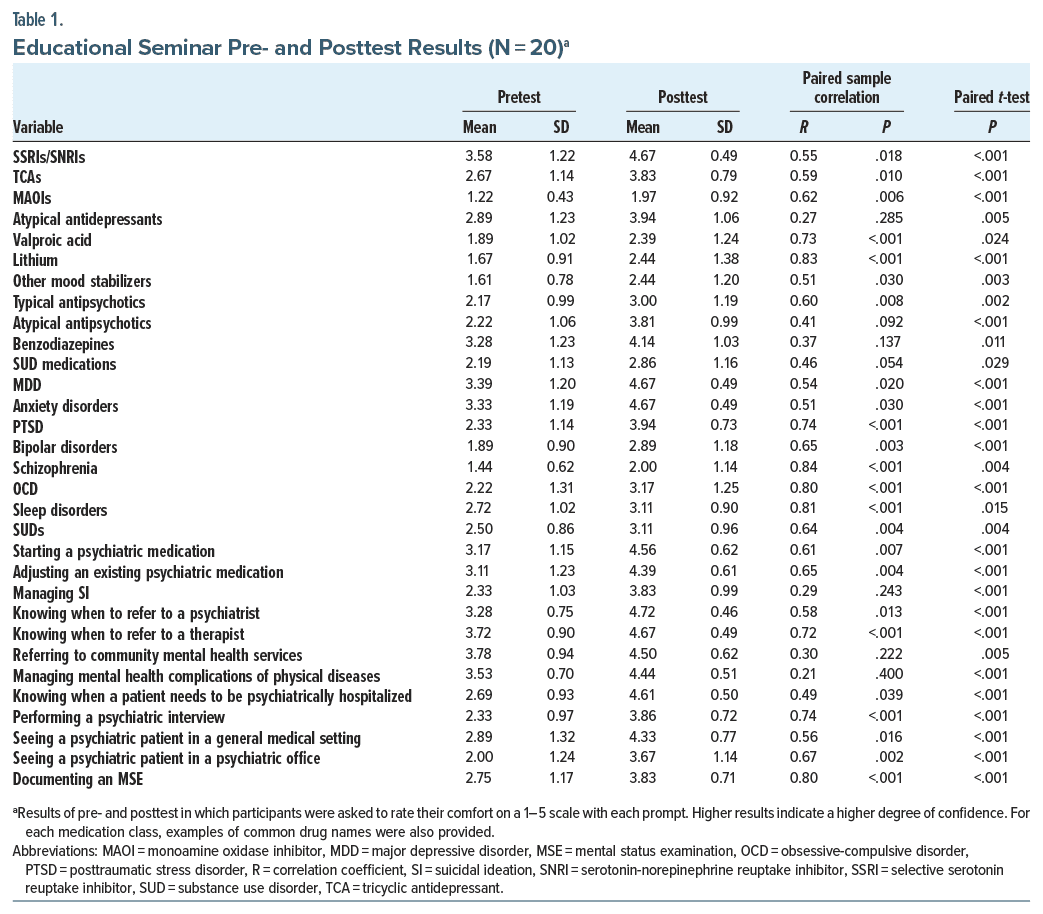
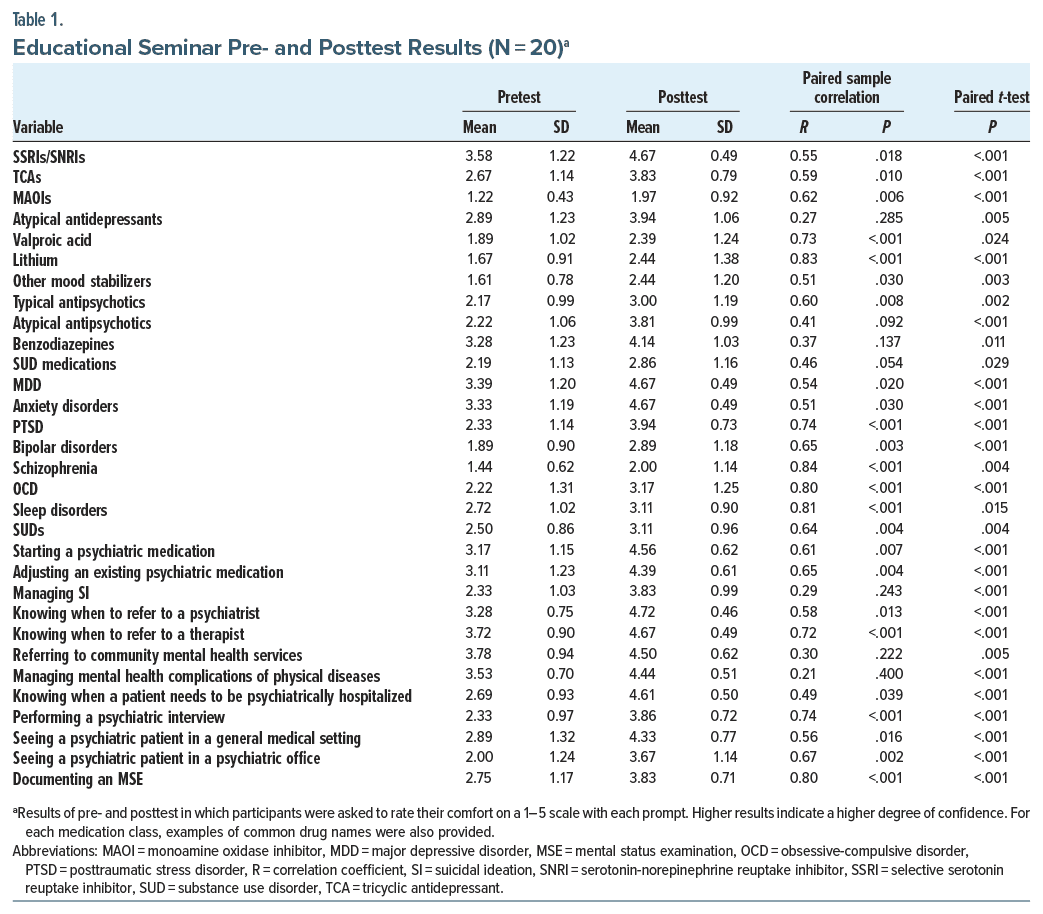
Methods: The study sample consisted of a cohort of convenience of nonbehavioral health physicians and advanced practice providers. The authors administered pre and posttests to measure provider confidence in treating specific mental health diagnoses, utilizing specific classes of psychotropic medications, and managing specific clinical scenarios. Questions were ranked using a Likert scale from 1 (least comfortable) to 5 (very comfortable). Paired sample t-tests were utilized to compare the pre- and posttest survey results. A follow-up survey was administered 1 month following the completion of the seminar, and the results were analyzed qualitatively.
Results: Twenty nonbehavioral health care providers attended an educational 2-day seminar on August 3–4, 2023. There were statistically significant improvements between the pre- and posttest measures of confidence in all 31 items measured. At 1-month follow-up, 87.5% (N = 14) rated their overall impression of the seminar as “excellent” and 12.5% (N = 2) rated their impression as “very good.” At the 1- month follow-up, 15 participants reported treating patients for depression and anxiety, compared to 13 who had done so prior to the seminar.
Conclusions: An educational seminar hosted by psychiatrists is an effective intervention for increasing provider confidence in treating mental health conditions and could serve as a valuable method for expanding the mental health workforce.
Prim Care Companion CNS Disord2024;26(6):24m03777
Author affiliations are listed at the end of this article.
The prevalence of mental disorders in the general population is a significant public health concern, with a lifetime prevalence of 46.4%.1 The COVID 19 pandemic has exacerbated mental health challenges, leading to a surge in rates of mental illness globally.2 Access to mental health providers is limited, and this problem has been exacerbated by the pandemic.3 Workforce shortages exist across mental health professions and have worsened in all areas,4 and currently, 51.8% of patients who do receive mental health care do so in a primary care setting rather than from a psychiatrist.5 Despite this demand, nonpsychiatric providers feel inadequately trained in psychiatry to address the burgeoning mental health needs of their patient population.6
Recognizing the imperative to bridge this training gap, several models have been explored to integrate psychiatric expertise into primary care settings, the most widely studied of which is the collaborative care model.7 While these models demonstrate effectiveness, they are often hindered by logistical challenges and limited by clinical, organizational, and financial barriers.8 Educational initiatives to increase the capability of clinicians already responding to the mental health needs of the community could serve to bridge these gaps.9 While primary care is a natural ally in this aim, specialty physicians may be an untapped resource. In response to these limitations, our proposed curriculum aims to enhance the competency of nonpsychiatry clinicians in managing mental health conditions within the primary care setting. Crucially, the curriculum emphasizes the importance of discerning when to refer patients to a psychiatrist for specialized care, ensuring a collaborative and comprehensive approach to mental health management.
The concept of provider “comfort” with mental health topics was previously explored by Stilwell et al.6 They found that midwestern primary care providers expressed a limited degree of comfort in managing mental health diagnoses and using psychotropic medications. They also found that adding the hypothetical option of having either a therapist or psychiatrist, respectively, as “backup” increased these providers’ reported confidence. We hypothesized that by utilizing a modified version of the survey conducted by Stilwell et al,6 we could determine whether we might see an improvement in provider confidence on this measure by conducting a relatively brief educational intervention.
METHODSThis study consisted of a 31-item survey adapted from a previously utilized assessment developed by Stilwell et al,6 which measured provider confidence before and after an educational intervention as well as a follow-up qualitative survey. The study sample consisted of a cohort of convenience of primary care and specialty providers who attended the educational seminar hosted at Clarkson College in Omaha, Nebraska, August 3–4, 2023. There were no exclusion criteria, and all attendees were eligible to participate. The Nebraska Methodist Hospital Institutional Review Board reviewed and approved the study. Each participant signed a consent form that outlined interventions to maintain confidentiality and was offered a maximum of $250 upon completion of the final survey. The provision of this sum was deemed sufficient to partially compensate for missed clinical time that resulted from participation in this seminar. The study population was generated from physicians and advanced practice providers who responded to an advertisement posted in organization wide emails and spread via word of mouth.
The study intervention involved a 2-day seminar, totaling approximately 13 hours of instruction. The itinerary for the 2 days of instruction can be found in Figure 1. The seminar was developed specifically for this project and taught by 2 of the authors (D.H.R. and R.R.A.) based on their experience in education and consultation and focused on managing common presentations of major mental health conditions that might be encountered in outpatient clinics. Topics of instruction were the basics of psychiatric assessment including the mental status examination, pathophysiology, practical psychopharmacology, basics of psychotherapy, models of psychiatric care (including collaborative care, integrated behavioral health, and consultation), and special topics. The seminar also emphasized a model of risk stratification by teaching participants to screen and triage patients who could be safely managed by nonpsychiatrists versus those who should be promptly referred to psychiatry or an emergency department. For example, the module on depression focused on screening for bipolar disorder and psychosis and recommended referral to a psychiatrist for management rather than discussing treatment during the seminar. Following completion of the seminar, participants were eligible to participate in a bimonthly case consultation with one of the authors (D.H.R.) that lasted 1 hour each and took the form of virtual office hours to discuss patients and continued for 6 months following the completion of the seminar. Additionally, participants were provided access to archived lectures on psychopharmacology from the 2022 Annual Psychopharmacology Conference presented by the Massachusetts General Hospital Psychiatry Academy.
The primary outcome measure of the study was change in provider comfort level as measured on a survey adapted with permission from Stilwell et al.6 The originally published survey was utilized to measure provider confidence in a sample of Midwest primary care providers without an associated intervention, and in the present study, this measure was adapted by adding additional questions and utilizing it as a longitudinal assessment. This survey was administered immediately prior to and immediately following completion of the seminar, and anonymity was ensured by generating a unique identification code for each respondent. The 31- item survey asked respondents to rate their comfort level on a 5-point Likert scale (1 = least comfortable and 5 = most comfortable) regarding managing specific diagnoses (eg, unipolar depression, anxiety disorders, and posttraumatic stress disorder), utilizing specific medication classes (eg, selective serotonin reuptake inhibitors, tricyclic antidepressants, mood stabilizers, and atypical antipsychotics), and managing specific clinical scenarios (eg, “knowing when to refer to a psychiatrist” and “knowing when a patient needs to be psychiatrically hospitalized”).
Data analyses were conducted in SPSS. Descriptive statistics and paired sample correlations were computed for each pre- and posttest outcome pair. Paired sample t-tests were used to compare the pre- and posttest survey results.
One month following the completion of the seminar, an additional follow-up survey was sent to evaluate the quality of the seminar and the changes in clinical practice that resulted from the seminar. The survey included a mix of Likert scale and short answer questions, which were analyzed qualitatively by grouping responses that were reported by more than one participant and reviewing for recurring themes.
RESULTSThe study population consisted of a cohort of 20 nonpsychiatrist clinicians that ranged in career phase from recent graduates to recently retired. The participants constituted a diverse training background (11 MD, 6 advanced practice registered nurses, 2 physician assistants, and 1 provisionally licensed mental health practitioner) and type of specialization (5 family medicine, 1 gastroenterology, 1 internal medicine, 1 nephrology, 2 obstetrics/ gynecology, 2 palliative care, and 8 surgical oncology).
All 20 participants completed both the pre- and posttests. A paired sample t-test was performed to evaluate whether there was a significant difference between the pre- and posttest confidence ratings for each item. Overall, there was a statistically significant improvement in comfort between pre- and posttest for all items assessed. These results are displayed in Table 1. Of the seminar participants, 80% (N=16) completed the follow-up survey, and the results are displayed in Table 2. Of the respondents, 87.5% (N=14) rated their overall impression of the seminar as “excellent,” and 12.5% (N=2) rated their impression as “very good.” Regarding depression, 56.25% of respondents reported that their confidence in managing depression changed “very much” after attending the seminar, and the remaining 43.75% reported that it changed “somewhat.” Regarding anxiety, 43.75% of respondents reported that their confidence in managing anxiety improved “very much” after attending the seminar, and the remaining 56.25% reported that it changed “somewhat.” At the 1-month follow-up, 15 participants reported treating patients for depression and anxiety compared to 13 who had done so before.
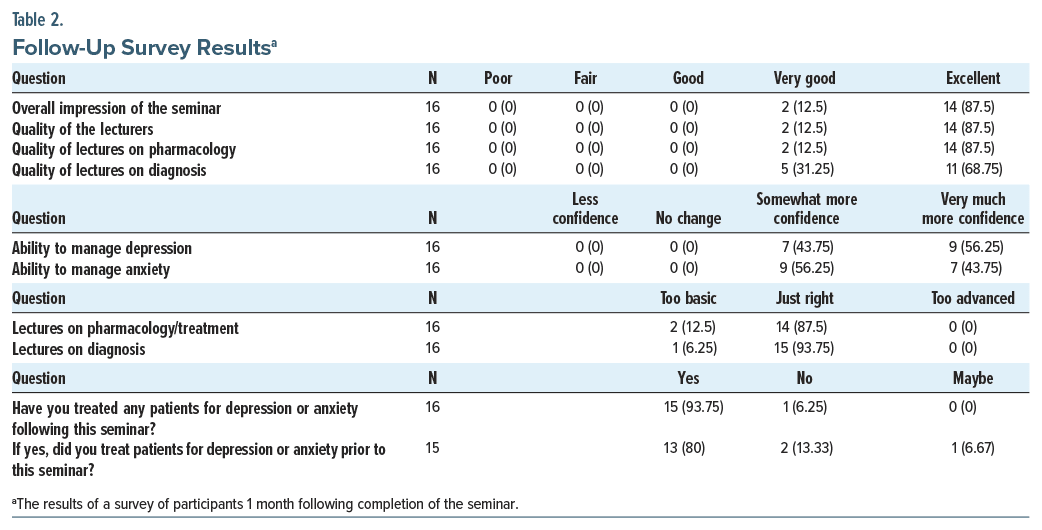
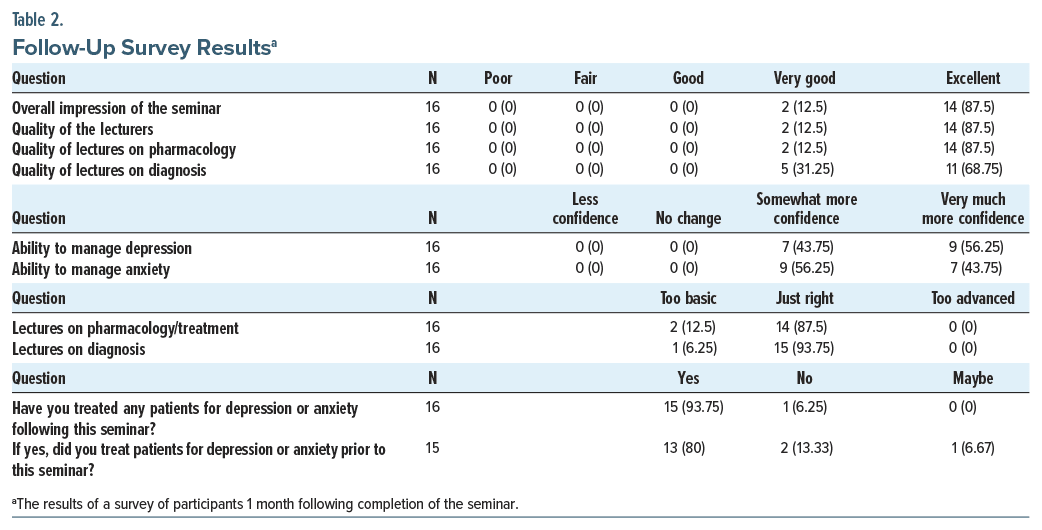 Themes that emerged from a qualitative review of survey comments also revealed that, following completion of the seminar, participants (1) felt more confident in diagnosing and managing mental health conditions, (2) were more likely to titrate medications more quickly, (3) were more likely to escalate to higher doses of medications, (4) expressed more confidence in switching medications when necessary, and (5) felt that the project was worth repeating for more clinicians.
Themes that emerged from a qualitative review of survey comments also revealed that, following completion of the seminar, participants (1) felt more confident in diagnosing and managing mental health conditions, (2) were more likely to titrate medications more quickly, (3) were more likely to escalate to higher doses of medications, (4) expressed more confidence in switching medications when necessary, and (5) felt that the project was worth repeating for more clinicians.
The present study demonstrated that a 2-day educational seminar significantly increased provider confidence across all domains studied. Follow-up survey results indicated that 87.5% rated the seminar as “excellent,” and 56.25% reported that their confidence in managing depression increased “very much,” with similar results of 43.75% for anxiety. Qualitative feedback highlighted increased confidence in diagnosing and managing mental health conditions, quicker medication titration, and a willingness to repeat the project for more clinicians.
On comparable items, the results of our pretest survey were strikingly similar to those previously reported by Stilwell et al.6 The results of their survey are reported without raw averages on a bar graph, so the degree of similarity is not directly calculable, but visually, the comfort level for each diagnosis and medication class was within 1 standard deviation of our results. The Stilwell et al6 study had a larger study population (N = 54) and was limited exclusively to providers in primary care. Our study further expands this population but also, uniquely, involves multiple subspecialty clinicians to further generalize these results. Due to the consistency of these findings, this further supports the conception of provider “comfort” in managing mental health as a valid instrument of measurement. Stilwell et al6 found that the idea of having either a therapist or psychiatrist as backup significantly increased provider confidence. Our design allowed for follow-up meetings to discuss patient issues or general concerns but did not allow for access to a psychiatrist at the point of care. Even without this safety net, this study adds to this literature by demonstrating that a relatively brief, scalable educational intervention can significantly increase provider confidence.
This is the first study, to our knowledge, that demonstrated the efficacy of an educational intervention for both primary and specialty care providers. This is an important finding because mental illness and mental health treatment cannot be neatly siloed into either primary care or psychiatry. After all, mental health affects and is affected by many other medical illnesses. Specialists see many patients that have psychiatric comorbidity, and many patients see them more than their primary care providers. Additionally, many of the concerns that patients seek specialty care for, such as globus phenomenon, chest pain, constipation, and abdominal pain, have roots in or are exacerbated by psychological distress in many cases. Having more facility with diagnosing and even engaging in the conversation of mental health concerns may be of substantial value for the providers, their patients, and society. Our intervention was well received by all participants, and while each attendee brought varying levels of experience to the seminar, a significant majority of them felt that the level of content was appropriate to their level of expertise. A replication of this study is currently underway as of the time of this writing. Participants were offered compensation for their participation in this study, but the authors feel that this was unlikely to have influenced the study results as the compensation was nominal compared to the cost of lost productivity, and most participants chose to donate their compensation back to the study organization to facilitate future seminars.
One limitation of this study is the potential effect of increased provider confidence generalized to all items, not just the ones that were specifically addressed during this seminar (eg, schizophrenia). This halo effect may suggest a heightened familiarity with approaching patients with mental health issues and being able to recognize when to refer. Conversely, this may be a weakness of the depth of participant concentration during the survey completion. Additionally, several items that were not significantly addressed in this seminar had nonsignificant correlations (eg, managing suicidal ideation), indicating that there was a nonlinear distribution of scores, and while these were significant, it is possible that with a larger sample size, this effect may have disappeared. Follow-up times for this study were short, and it is possible that with time, these effects may have disappeared. Finally, as this was a pilot study, the sample size was low, and information about practice patterns before and after the seminar was limited. These limitations will be addressed with subsequent studies.
CONCLUSIONThis study demonstrates that an educational intervention delivered in the form of a 2-day seminar is an effective intervention for increasing provider confidence in managing mental health conditions. This study was novel in that it provided additional validation of the survey instrument and involved specialists as well as primary care providers. The study results support the idea that educational interventions can be a valuable tool in addressing the training gap among nonpsychiatric providers. The researchers plan to replicate the study to further validate the findings and explore longer-term impacts on clinical practice.
Article InformationPublished Online: December 3, 2024. https://doi.org/10.4088/PCC.24m03777
© 2024 Physicians Postgraduate Press, Inc.
Submitted: May 24, 2024; accepted August 22, 2024.
To Cite: Lydiatt MF, Lydiatt WM, Mitchell JC, et al. Bridging the gap: an educational intervention to enhance mental health competency among primary and specialty care providers. Prim Care Companion CNS Disord. 2024;26(6):24m03777.
Author Affiliations: University of Nebraska Medical Center, Omaha, Nebraska (MF Lydiatt); Nebraska Methodist Hospital, Omaha, Nebraska (WM Lydiatt); Midwest Gastrointestinal Associates, Omaha, Nebraska (Mitchell); Munroe Meyer Institute, Omaha, Nebraska (HV Lydiatt); University of Vermont, Burlington, Vermont (Althoff); and Massachusetts General Hospital, Boston, Massachusetts (Rubin).
Corresponding Author: Maxwell F. Lydiatt, MD, Department of Psychiatry, University of Nebraska Medical Center, 510 S 42nd St, Omaha, NE 68131 ([email protected]).
Relevant Financial Relationships: None.
Funding/Support: Supported by Rhonda and Howard Hawks Foundation and Clarkson College.
Role of the Sponsor: The sponsors of this study, the Rhonda and Howard Hawks Foundation and Clarkson College, had no role in the conduct of the study; the collection or analysis of data; or the preparation of the manuscript.
Acknowledgments: The authors would like to express their gratitude to the Rhonda and Howard Hawks Foundation for generously funding this study, as well as Clarkson College President Andreia Nebel, EdD, PT, DPT, FNAP, and Jade Liles, BS, for hosting the seminar and Clarkson Institute for partial funding and logistical support. Dr Nebel and Ms Liles report no conflicts of interest related to the subject of this article.
留言 (0)