Lumbar disk herniation (LDH) is a common clinical spinal disorder in which the fibrous annulus of the lumbar disk partially or completely ruptures due to various causes. This rupture causes the nucleus pulposus tissue to protrude backward, irritating or compressing the nerve roots and cauda equina (1). Low back pain and neurological dysfunction are the main clinical manifestations (2). In recent years, the incidence of LDH has been increasing annually and shows a trend toward younger age groups (3). It is estimated that approximately 2–3% of the world’s population experiences LDH (4), which mainly affects adults between the ages of 20 and 50 years (3). Intensive work, long hours, sedentary behavior, and prolonged standing are considered the main causes of LDH. Difficulties in standing, walking, and performing simple tasks in patients with LDH have significantly impacted global productivity, public health, and the quality of life for those affected (5, 6). The United States spent up to $4 billion on treating LDH through medication and surgery in 2015 alone (7).
The treatment of LDH can be broadly categorized into surgical and non-surgical approaches. Although surgical treatments can provide rapid pain relief, they are associated with significant drawbacks, such as postoperative complications, technical challenges, a high risk of reoperation, and substantial costs (8–10). Consequently, 80–85% of patients opt for non-surgical treatments (11).
Non-surgical treatment options for LDH include a variety of therapeutic approaches aimed at alleviating symptoms and improving function without the need for invasive procedures. These options include physical therapy, pharmacological treatments, chiropractic care, and acupuncture (12–14). Suspension exercise training (SET) is emerging as a promising non-invasive therapy for treating skeletal and muscular disorders, including LDH. SET is simple, easy to perform, painless, relatively inexpensive, and effective (10). Despite its potential benefits, there has been no comprehensive systematic review or meta-analysis specifically evaluating the efficacy of SET for treating LDH. Our study aimed to provide a new option for the treatment of LDH.
2 MethodsThis study was registered in PROSPERO (CRD42024554074) and strictly adhered to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement (15).
2.1 Literature search and selectionWe searched the CNKI, Chinese Wanfang, PubMed, Cochrane, Web of Science, and Embase databases for Chinese and English literature up to June 2024. The search terms included “sling exercise, ““suspension exercise,” and “LDH.” The inclusion criteria were as follows: (1) treatment involving suspension exercise; (2) patients diagnosed with LDH; (3) study design as a randomized controlled trial or a clinical trial; and (4) the visual analog scale (VAS) score, Japanese Orthopedic Association (JOA) score, and Oswestry Disability Index (ODI) score of suspension exercise for LDH. The exclusion criteria were as follows: (1) no control group in the trial; (2) no data on baseline or endpoint outcomes; (3) patients with psychiatric disorders; and (4) reviews, dissertations, or conference papers.
Duplicates were removed using EndNote X9 software. Two authors (SL and XX) independently read the titles and abstracts of the literature to determine whether the inclusion criteria were met. The studies that initially met the inclusion criteria were read in full to determine final inclusion. For disagreements regarding the studies, a third author (HY) was involved to help determine inclusion through discussion.
2.2 Data extraction and quality assessmentData extraction from the final included studies was performed independently by two authors (SL and HY), and the extracted information included the first author, year of publication, basic information about the participants, types of interventions, intervention duration, outcome indicators, and follow-up time.
The Cochrane Collaboration’s risk-of-bias guidelines (16) were used to evaluate the quality of the included studies. The guidelines included the following: (1) random sequence generation, (2) allocation concealment, (3) blinding of participants and personnel, (4) blinding of outcome assessments, (5) incomplete outcome data, (6) selective reporting, and (7) other bias. The quality of the studies was evaluated independently by two authors. In case of a disagreement, a third author was involved in discussions until an agreement was reached.
2.3 Types of outcome indicatorsThe primary outcome indicators included the visual analog scale (VAS) (17), and the secondary outcome indicators included the Japanese Orthopedic Association (JOA) (18) and Oswestry Disability Index (ODI) (19).
2.4 Data synthesis and statistical analysisAll outcome indicators in this study were continuous variables measured on the same rating scale and were analyzed using mean difference (MD) and a 95% confidence interval (CI) as effect sizes. The effect size resulting from the meta-analysis provided a statistically standardized representation of the quantitative results of each study. It was calculated based on the mean pre-post change in the experimental group minus the mean pre-post change in the comparison group and then divided by the pooled pretest standard deviation. The meta-analysis was performed using RevMan 5.4 and Stata 17.0. Heterogeneity was quantified using the I2 statistic, and a fixed effects model was employed if the difference in the heterogeneity test was not statistically significant (I2 < 50%; p > 0.05). Otherwise, a random effects model was applied. Subgroup and sensitivity analyses were performed to explore the sources of heterogeneity for the outcome indicators. The subgroup analyses were performed according to the type of interventions, while the sensitivity analyses were performed by removing each study item to assess the reliability and consistency of the results. Publication bias was assessed using funnel plots and Egger’s asymmetry test for outcome measures with more than 10 included studies. All statistical significance levels were set at α = 0.05.
3 Results 3.1 Search resultsA total of 287 studies were identified through database searches, and 208 studies remained after removing duplicates using EndNote X9. Two authors reviewed the titles and abstracts of the studies according to the inclusion and exclusion criteria for preliminary screening. In case of a disagreement between the two authors, a third author was involved in the discussion and decided whether to include a study. A total of 189 irrelevant studies were excluded, leaving 19 articles that were read in full. An additional eight articles that did not meet the inclusion criteria were excluded, resulting in a final total of 11 articles that were included in the meta-analysis. The literature screening process is shown in Figure 1.
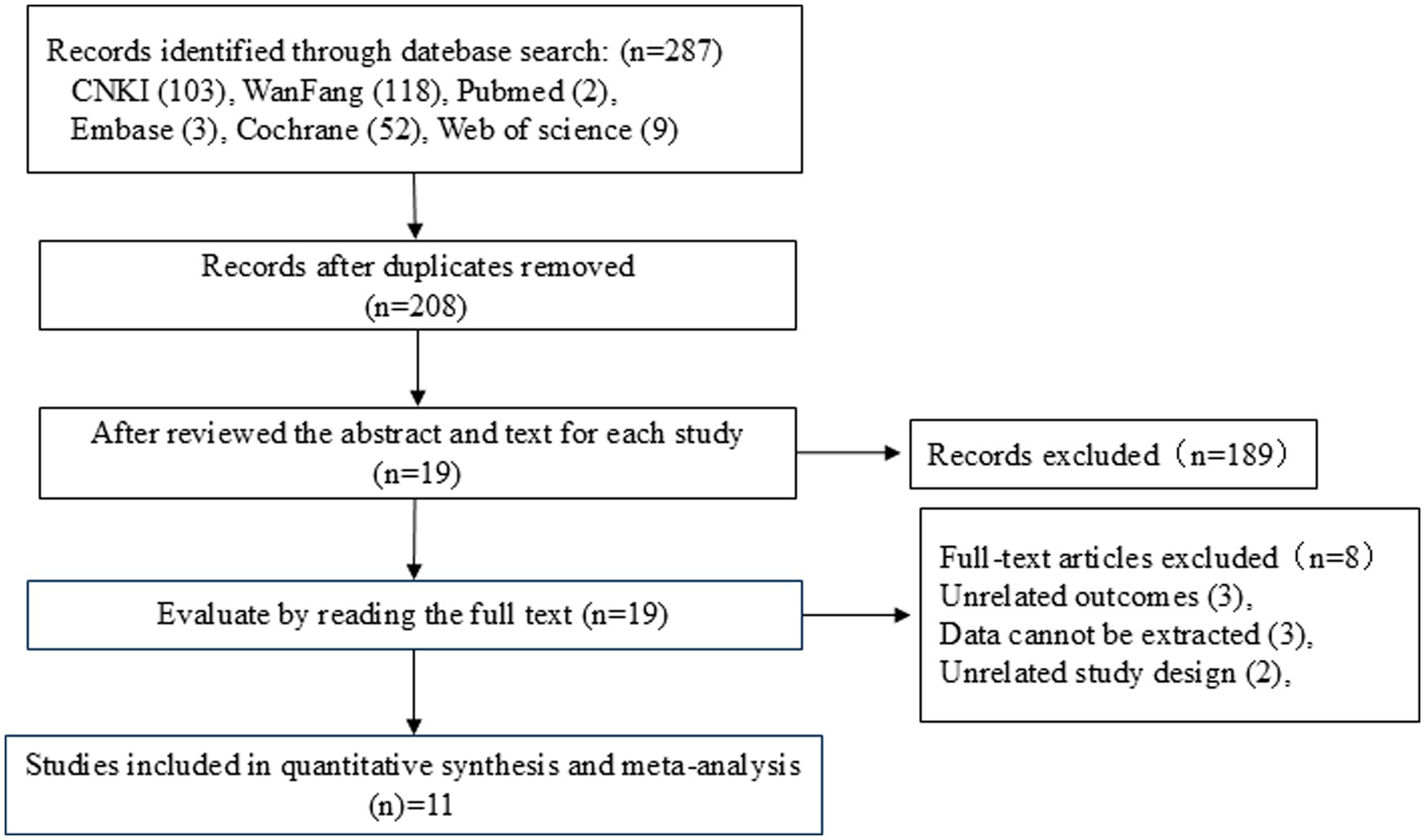
Figure 1. Literature screening flowchart.
3.2 Basic characteristics of the included studiesThis meta-analysis included 11 studies (20–30), involving 943 patients—472 in the test group and 471 in the control group. There were 463 male participants and 397 female participants, with two studies not reporting the sex of the participants. The mean age of the patients ranged from 37.2 to 58.6 years, with one study not reporting the mean age. The intervention period ranged from 2 to 8 weeks. The outcome indicators included the VAS, JOA, and ODI scores. Six studies reported follow-up, while five did not (see Table 1).
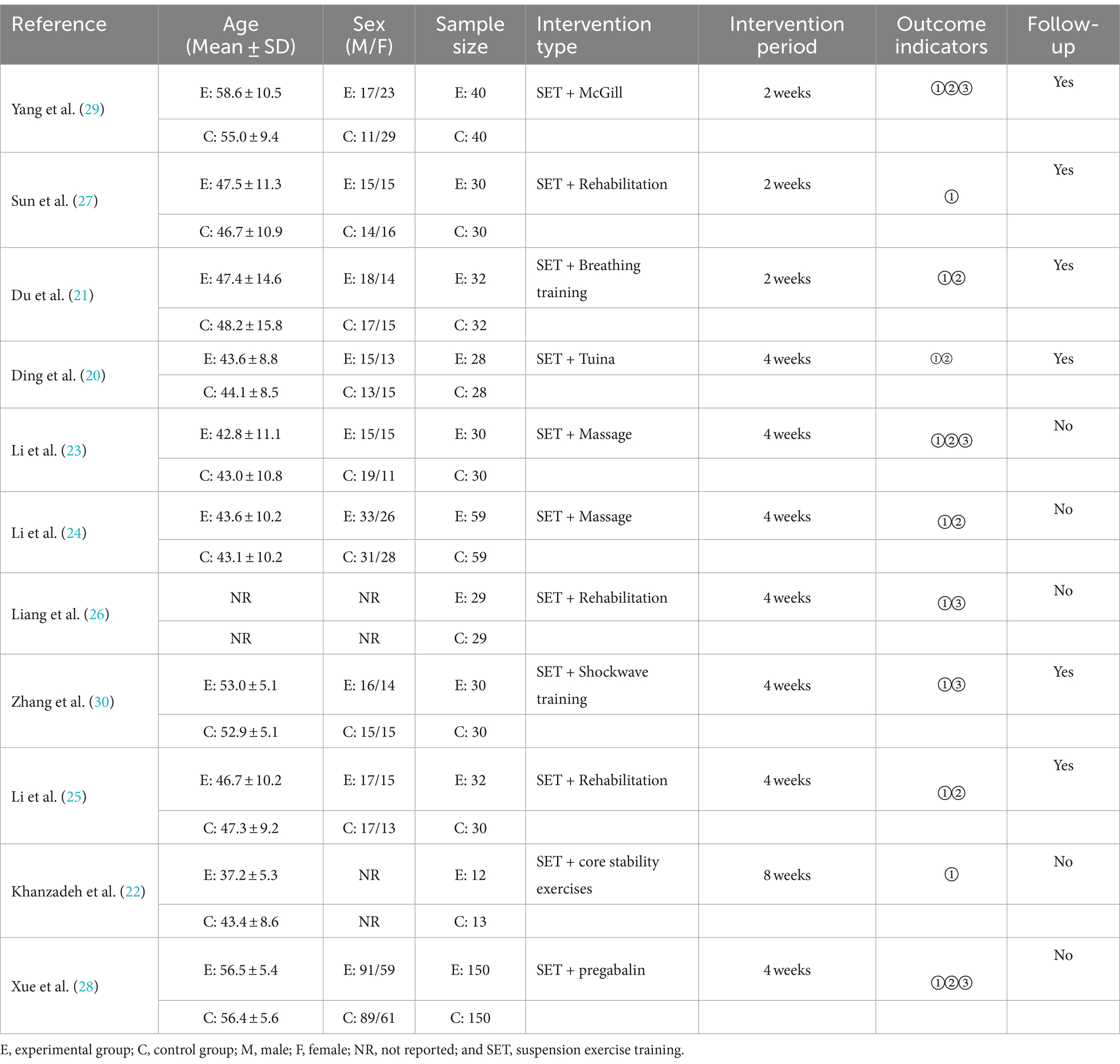
Table 1. Basic characteristics of the included studies.
3.3 Quality evaluation resultsThis meta-analysis used the Cochrane Collaboration’s risk-of-bias guidelines to assess the quality of the included studies. Regarding random sequence generation, 11 studies were assessed as low risk because they all reported random allocation using the random number expression method. Regarding allocation concealment, 11 studies reported that the method used for allocation concealment was not clearly stated, and thus they were assessed as uncertain risk. In terms of blinding of participants and personnel, one study that indicated that the intervention was conducted uniformly was assessed as uncertain risk, while 10 studies that did not report implementation blinding were assessed as high risk. Regarding blinding of outcome assessments, two studies that reported that the blinding of outcome assessments was performed by uniform professionals were assessed as uncertain risk, while nine studies that did not report on the blinding of outcome assessment were assessed as high risk. In terms of incomplete outcome data, six studies with complete outcome data were assessed as low risk, while five studies were assessed as uncertain risk for not reporting follow-up. In terms of selective reporting, all 11 studies that reported findings were assessed as low risk. In terms of other biases, all 11 studies were assessed as low risk, with no additional biases identified. The results of the quality assessment are shown in Figure 2.
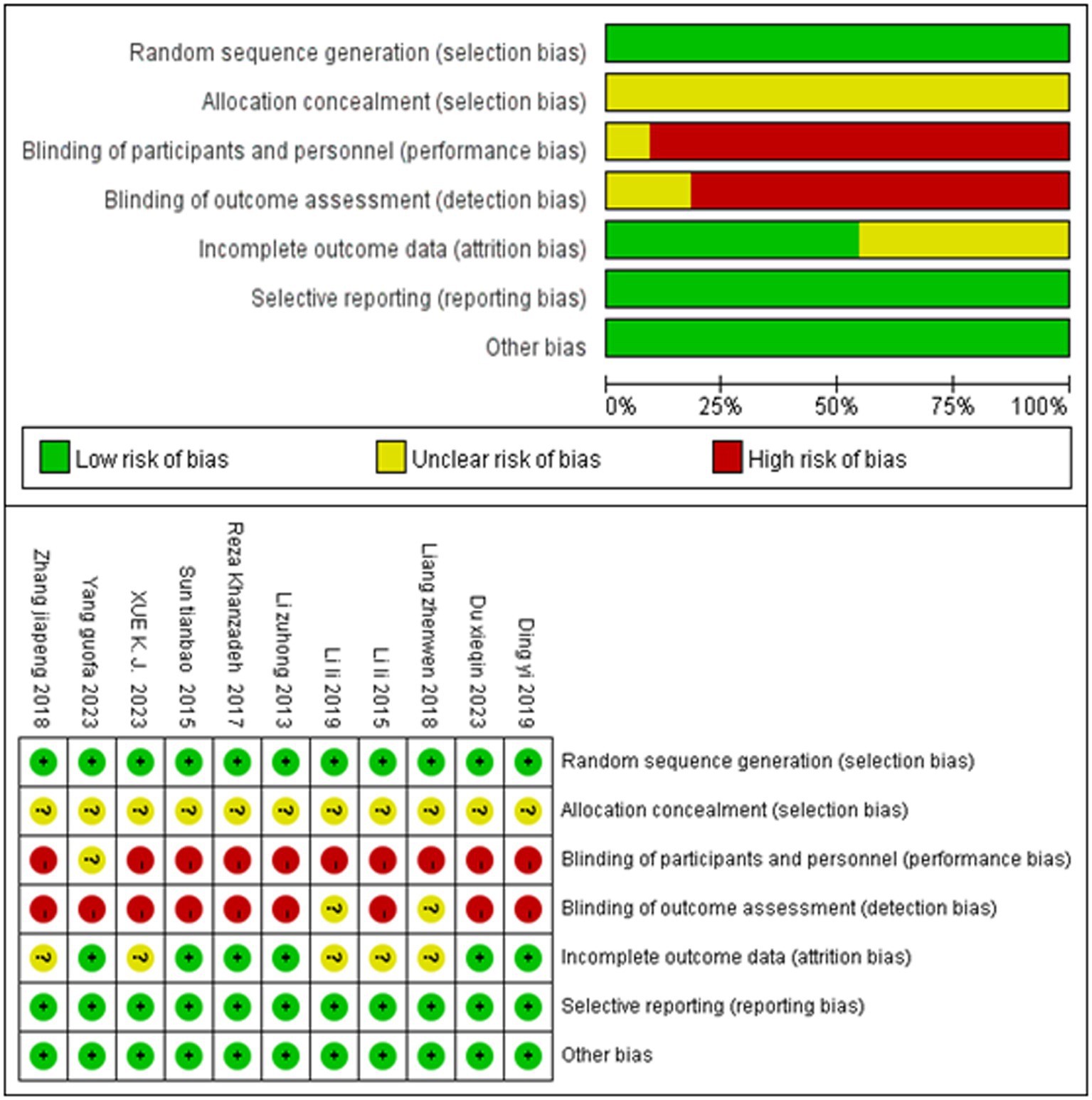
Figure 2. Quality evaluation results.
3.4 Meta-analysis results 3.4.1 Meta-analysis of SET on the VAS scoresTwo studies assessed the VAS scores at different time points; therefore, a total of 13 VAS score comparisons were reported across 11 studies. A fixed effects model was used to integrate the results. SET significantly reduced the VAS score among the patients with LDH compared to the controls (MD = −0.96, 95% CI, −1.10 to −0.82; p < 0.00001, I2 = 23%) (Figure 3).
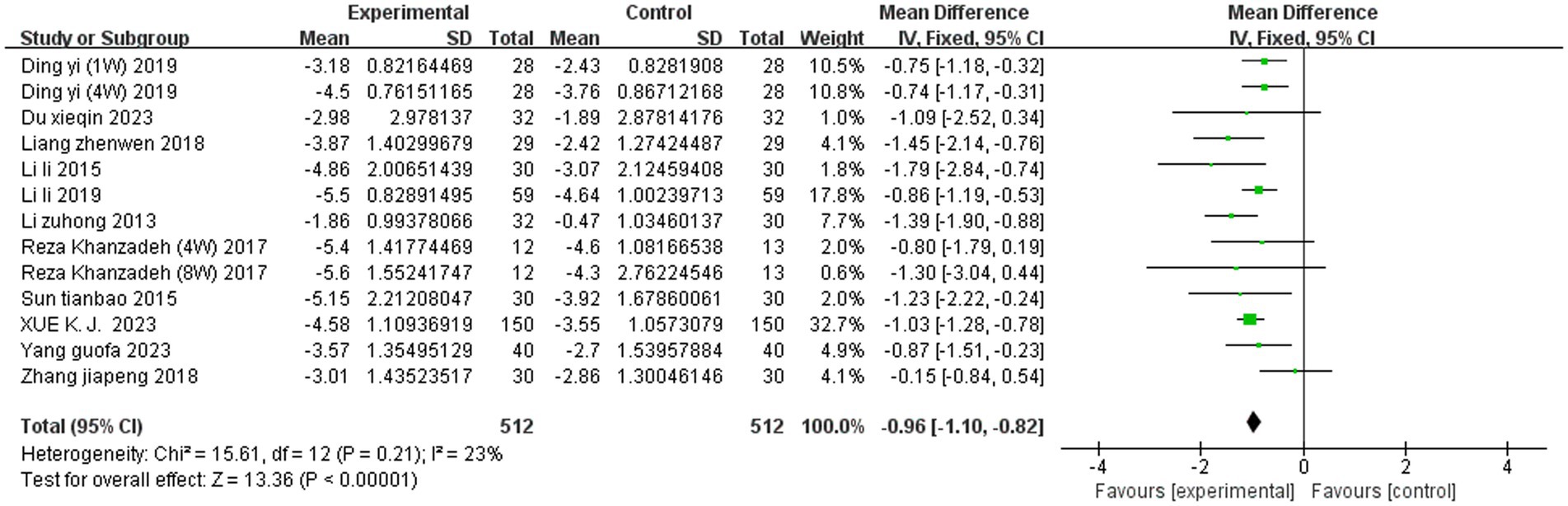
Figure 3. Meta-analysis of SET on the VAS score.
3.4.2 Meta-analysis of SET on the JOA scoresSeven studies reported the JOA scores. A random effects model was used to integrate the results. SET significantly improved the JOA score among the patients with LDH compared to the controls (MD = 3.29, 95% CI, 1.67 to 4.90; p < 0.0001, I2 = 92%). Subgroup analyses of the JOA score based on intervention modality revealed that SET combined with traditional Chinese medicine (TCM) (MD = 4.29, 95% CI, 2.73 to 5.86; p < 0.00001, I2 = 80%)had better efficacy compared to SET combined with non-TCM (MD = 0.96, 95% CI, 0.49 to 1.43; p < 0.0001, I2 = 0%) and that intervention modality was the main source of heterogeneity in the JOA score among the patients with LDH (Figures 4, 5).
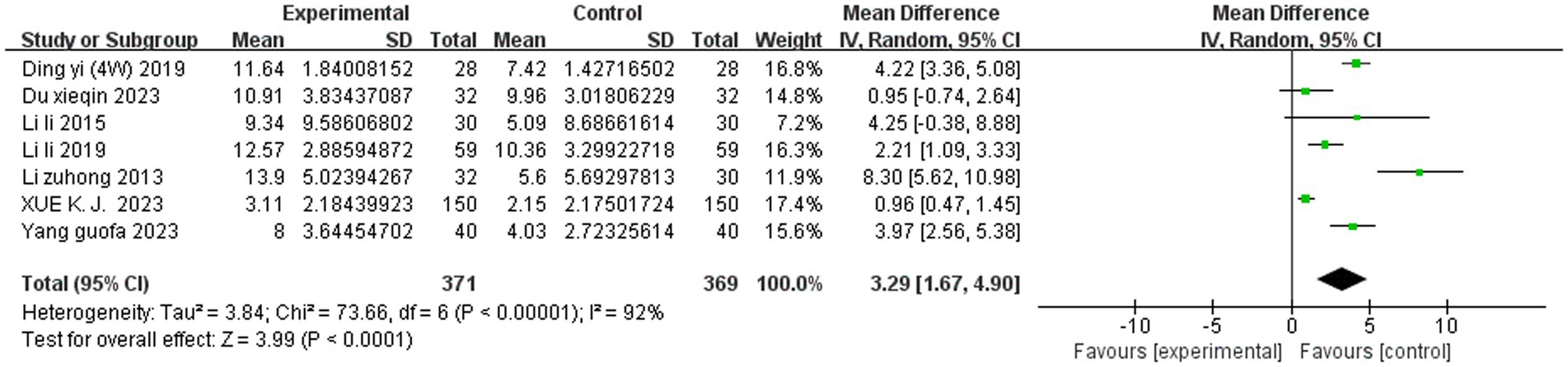
Figure 4. Meta-analysis of SET on the JOA score.
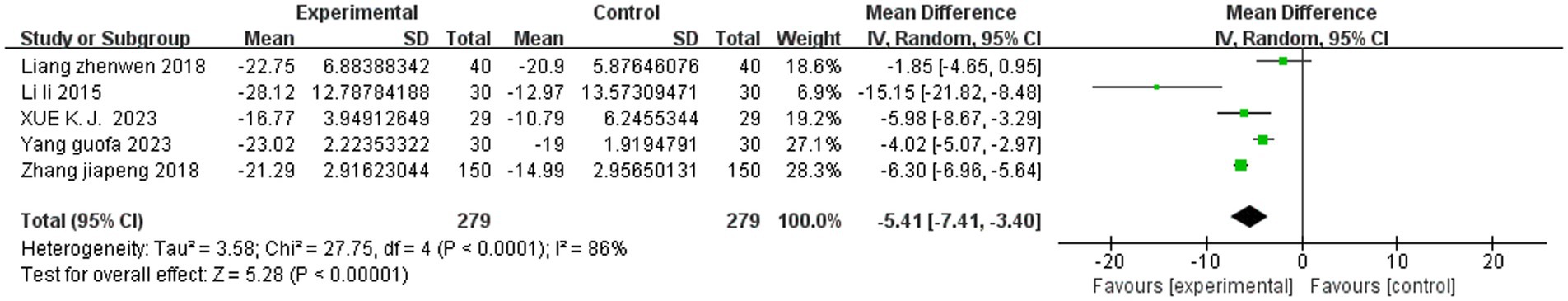
Figure 5. Subgroup analysis of SET on the JOA score.
3.4.3 Meta-analysis of SET on the ODI scoresFive studies reported the ODI scores. A random effects model was used to integrate the results. SET significantly improved the ODI score among the patients with LDH compared to the controls (MD = −5.41, 95% CI, −7.41 to −3.40, p < 0.00001, I2 = 86%). Subgroup analyses based on the intervention period and intervention type did not reveal any sources of heterogeneity (Figure 6).
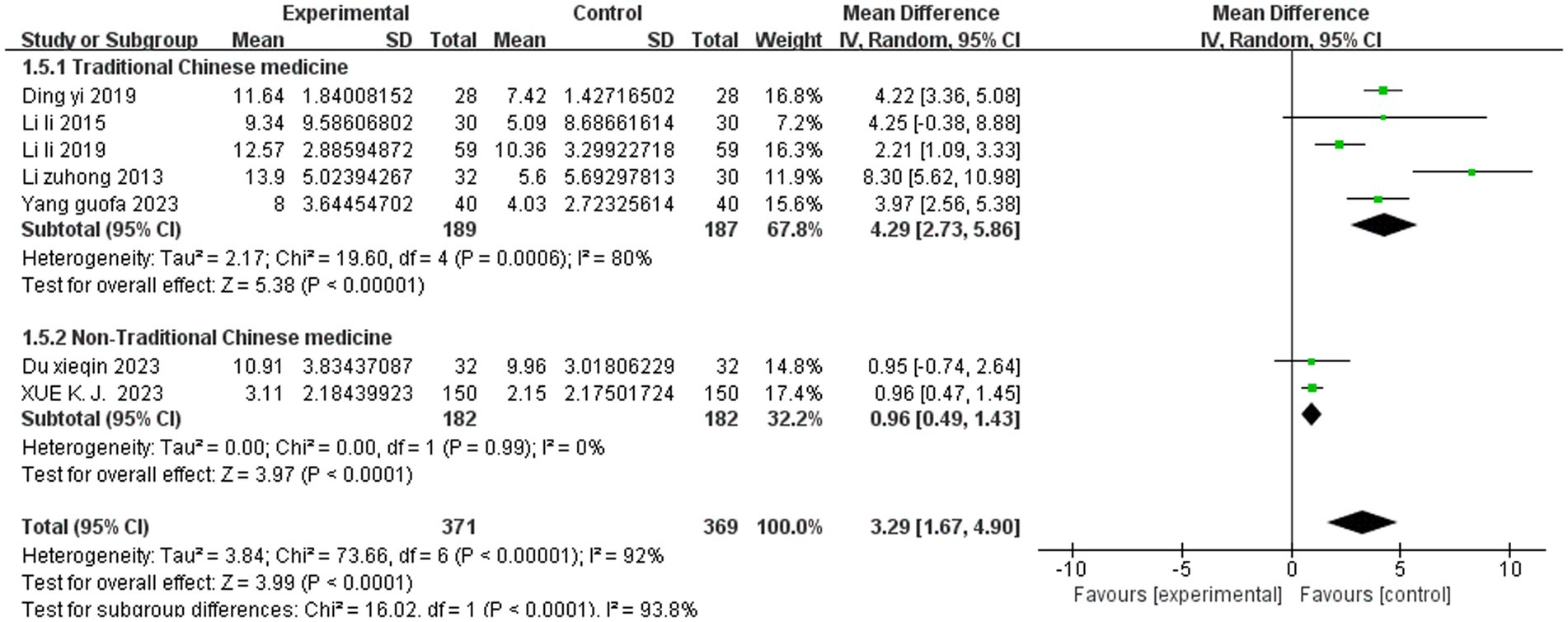
Figure 6. Meta-analysis of SET on the ODI score.
3.5 Sensitivity analysisHeterogeneity for the two outcome indicators, the JOA score and ODI score, was high in this study. By removing one JOA score and one ODI score (whose treatments in this study were different from those in the other studies) through sensitivity analysis, the remaining combined results showed a significant decrease in heterogeneity (I2 = 83% and I2 = 80%). However, there was still no statistically significant difference in the total combined results for the JOA scores (MD = 3.73, 95% CI, 2.17 to 5.19, p < 0.00001) and ODI scores (MD = −5.37, 95% CI, −8.33 to −2.42, p < 0.0004), indicating that the findings of this study are relatively reliable. The detailed sensitivity analyses for the VAS score, JOA score, and ODI score are presented in Supplementary Tables S2–S4 of the attachment, respectively.
3.6 Publication bias analysisFunnel plots and Egger’s asymmetry test were conducted for the VAS scores of the outcome indicators that included more than 10 studies. The results showed that the left and right sides were largely symmetrical, with the majority of the studies positioned in the upper middle. However, one study (30) fell outside the 95% confidence interval (dashed angled lines) (see Figure 7). The Egger’s test indicated no publication bias (p = 0.888) (see Figure 8).
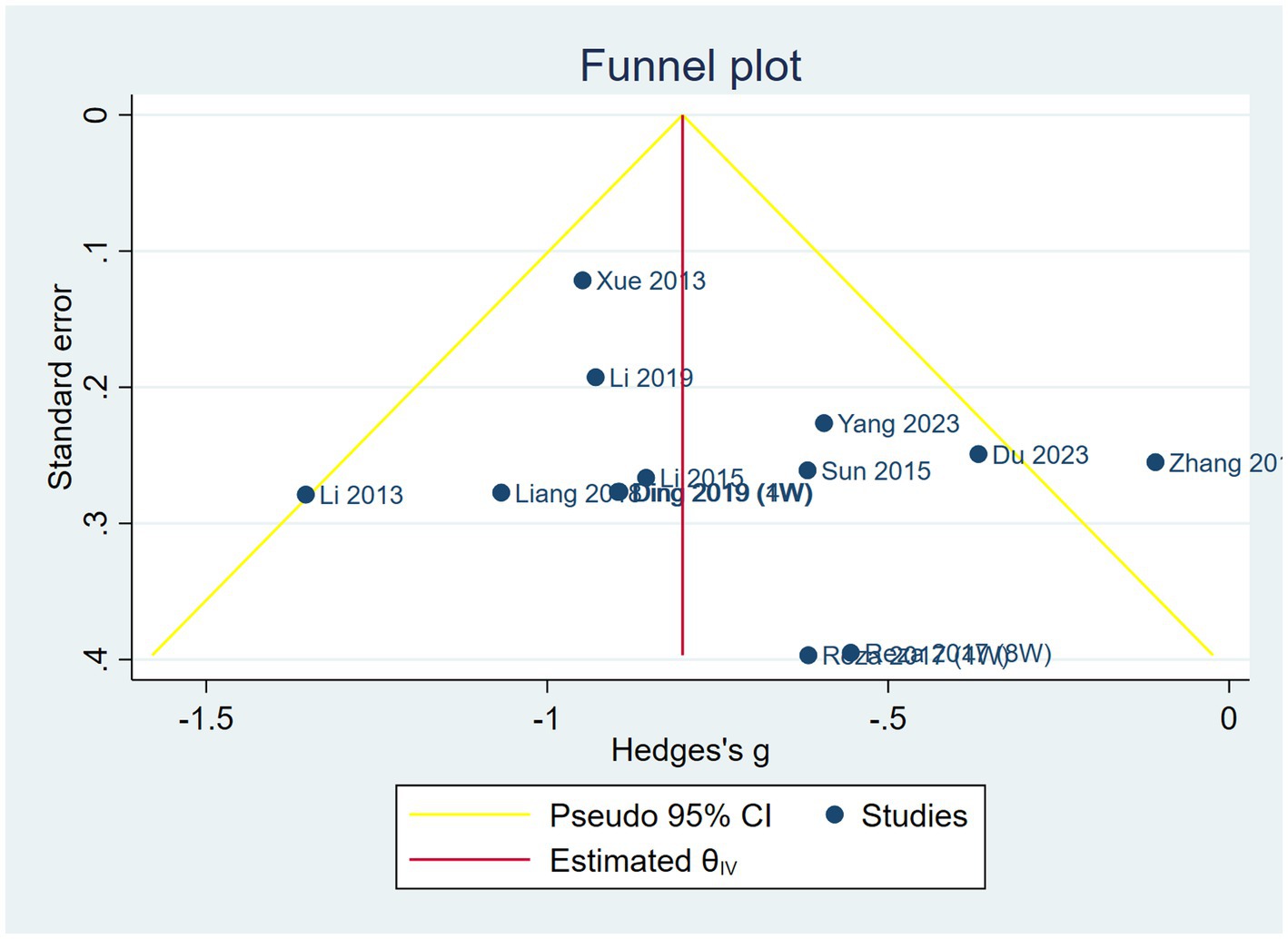
Figure 7. Funnel plots of SET on the VAS score.
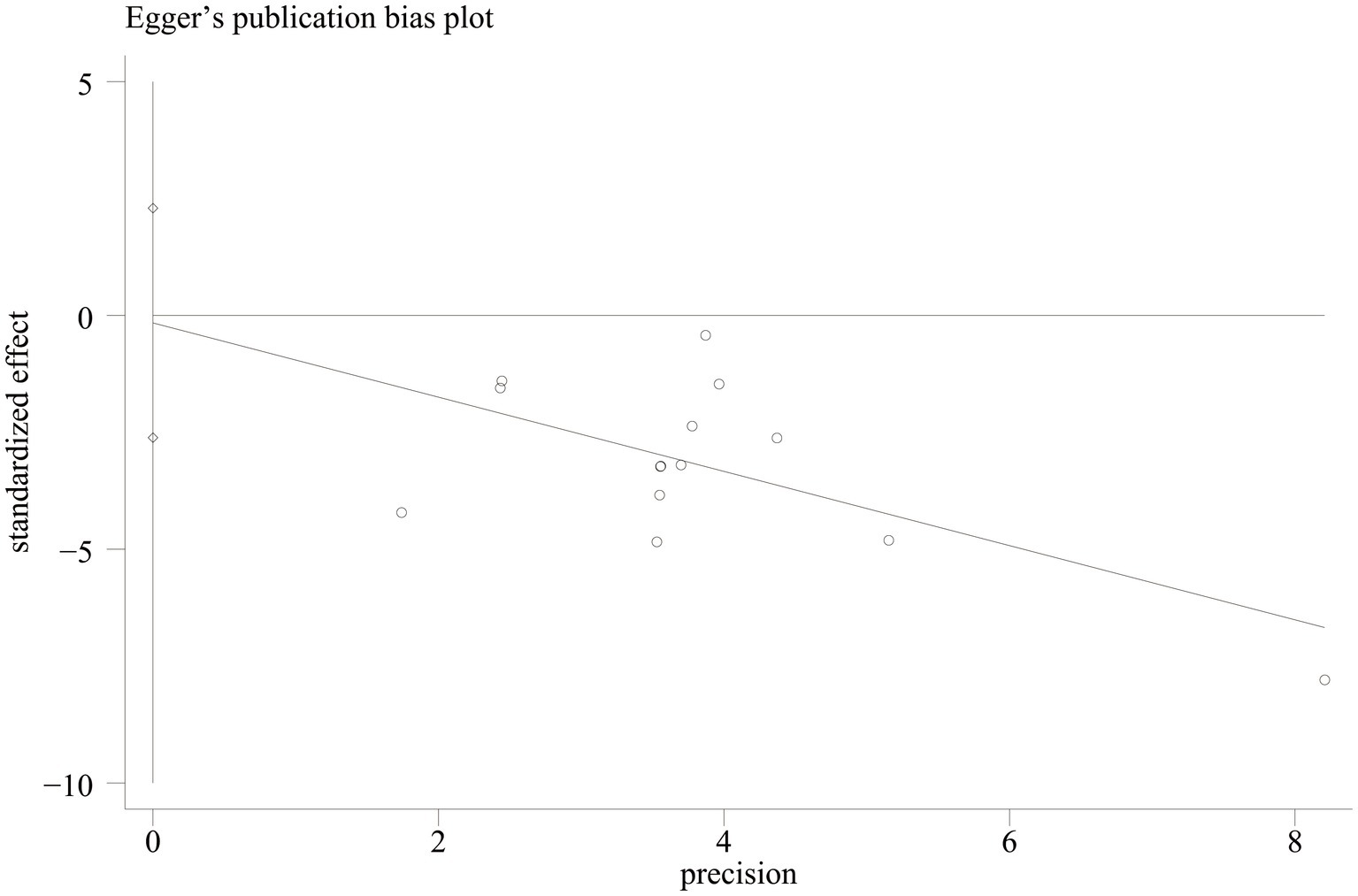
Figure 8. Egger’s publication bias plot for the VAS score.
4 DiscussionTo the best of our knowledge, this is the first meta-analysis that evaluates the efficacy of suspension exercise training in the treatment of LDH, focusing particularly on its effect on patients with lumbar disk herniation. A total of 11 studies involving 943 patients with lumbar disk herniation were included in this meta-analysis. The results indicated that suspension exercise training significantly improved the VAS, JOA, and ODI scores among the patients with LDH. Subgroup analyses revealed that the combined modality of suspension exercise training was the main source of heterogeneity in the JOA scores.
The VAS score (17) is a valid scoring method for measuring pain, represented on a straight line of 10 cm length, where one end signifies 0 for no pain and the other end signifies 10 for the most severe pain. This allows testers to assess the level of pain according to their own sensations; the lower the score, the lesser the pain, while the higher the score, the greater the pain. The results of this study showed that suspension exercise training significantly reduced the VAS scores among the patients with lumbar disk herniation, which is consistent with a previous study (31). However, unlike the previous study, which showed that suspension exercise training reduced the VAS score by 4.37 points, this overview showed that SET only reduced it by 0.96 points. This difference is mainly due to the lack of a control group in the study as the VAS scores do not represent the mean difference between the experimental and control groups. Suspension exercise training can significantly reduce the VAS scores of patients with LDH for three main reasons. Firstly, suspension exercise training increases the lumbar intervertebral space by stretching the spinal column, which reduces the compression of lumbar disks on the nerves (32). Secondly, it can improve the microcirculation of lumbar soft tissues and accelerate the subsidence of inflammatory substances (33), thus reducing the production of pain factors. Finally, it can enhance the strength and coordination of the trunk muscle groups and improve the stability of the lumbar spine, thus reducing pain in patients with LDH (22).
The JOA score (18) is an effective scoring method for assessing the neurological functional status and daily living ability of patients with lumbar spine disease. It includes 25 scoring items, covering subjective symptoms, clinical symptoms, and daily living ability; the higher the score, the more obvious the functional improvement. The results of this overview showed that suspension exercise training significantly improved the JOA scores among the patients with lumbar disk herniation, which is consistent with a previous study (34). However, unlike the previous study, which showed that suspension exercise training improved the JOA scores by 5.28 points compared to traditional massage therapy, our study indicated that it only improved the scores by 3.29 points. We believe that this difference is mainly due to the intervention modality as suspension exercise training is not the only variable in the experimental and control groups. Suspension exercise training significantly improved the JOA scores among the patients with LDH. We believe that, on the one hand, suspension exercise training stimulates the neuromuscular coordination of contractions between the trunk muscles and major muscle groups of the body, thereby improving neuromuscular function (35). On the other hand, suspension exercise training enhances the stability of the spine by strengthening the strength and coordination of the trunk muscle groups, thereby improving the body’s balance, control, and stabilization during exercise (27). However, although suspension exercise training significantly improved the JOA scores among the patients with LDH, the study results showed a high degree of heterogeneity, which was significantly reduced after the deletion of one study (28). We believe this may be attributed to the intervention of suspension exercise training combined with pharmacotherapy. The subgroup analyses showed that suspension exercise training combined with traditional Chinese medicine had a better effect on improving the JOA scores among the patients with LDH. Therefore, future studies need to further validate the therapeutic effects of suspension exercise training combined with traditional Chinese medicine to determine the optimal combination modality.
The ODI score (19) is a validated scale commonly used to evaluate dysfunction related to lower back pain. There are a total of 10 scoring components, covering a variety of aspects such as pain level, daily living ability, walking, and standing, with higher scores indicating more severe dysfunction. The results of this study showed that suspension exercise training significantly reduced the ODI scores among the patients with LDH, which is consistent with a previous study (36). This is mainly due to the fact that suspension training addresses gravity with the help of adjustable slings and ropes, placing the patient on an unstable plane. This increases the stimulation of proprioceptive input in the lumbar core stabilizing muscle groups through safe, stepwise training, activates and recruits more motor units to enhance the muscle strength of target muscle groups, rebuilds the normal muscle movement pattern, and strengthens the stability of the spine, ultimately improving lumbar spine function (26) and reducing the ODI scores of patients with LDH. However, the results of the study showed a high degree of heterogeneity, which was significantly reduced after the deletion of one study (28), although there was no valid reason to delete this study. The subgroup analyses of the intervention duration and treatment modalities did not reveal a source of heterogeneity. We believe that the combined modality of suspension exercise training, the location of lumbar disk herniation, and the population affected by it might have been the sources of heterogeneity, which need to be further investigated in future studies. On the other hand, only five studies were included in the ODI scores of this review, and the small number of studies might have contributed to the high heterogeneity.
5 LimitationsThis study has the following three limitations. First, the number of studies included and their reliability need further improvement. Second, the VAS, JOA, and ODI scores rely on subjective evaluation scales. Finally, the meta-analyses of the JOA and ODI scores showed high heterogeneity.
6 ConclusionIn conclusion, suspension exercise training significantly improved the VAS, JOA, and ODI scores of the patients with lumbar disk herniation; however, there was a high degree of heterogeneity in the JOA and ODI scores Further validation is needed in the future for different populations with lumbar disk herniation, the specific locations of its occurrence, and the combined modalities of suspension exercise training.
Data availability statementThe original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
Author contributionsYL: Methodology, Writing – original draft, Conceptualization. SH: Data curation, Writing – review & editing. XZ: Software, Writing – review & editing. HL: Data curation, Writing – review & editing. WL: Supervision, Visualization, Writing – review & editing. ZZ: Supervision, Visualization, Writing – review & editing.
FundingThe author(s) declare that financial support was received for the research, authorship, and/or publication of this article. This study was supported by Pearl River-Xijiang River Economic Beit Development Institute, Guangxi Normal University (ZX2020015), and Project on Enhancement of Basic Research Ability of Young and Middle-aged Teachers in Guangxi Universities (2022KY0020).
Conflict of interestThe authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s noteAll claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary materialThe Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fneur.2024.1455505/full#supplementary-material
References1. Zhang, AS, Xu, A, Ansari, K, Hardacker, K, Anderson, G, Alsoof, D, et al. Lumbar disc herniation: diagnosis and management. Am J Med. (2023) 136:645–51. doi: 10.1016/j.amjmed.2023.03.024
Crossref Full Text | Google Scholar
2. Yang, X, and Wu, H. Analysis of the therapeutic effect and postoperative complications associated with 3-dimensional computed tomography navigation-assisted intervertebral foraminoscopic surgery in lumbar disc herniation in the elderly: a retrospective cohort study. Quant Imaging Med Surg. (2023) 13:7180–93. doi: 10.21037/qims-23-319
PubMed Abstract | Crossref Full Text | Google Scholar
3. Li, JX, Hsu, TJ, Hsu, SB, and Lin, YH. Strong association of lumbar disk herniation with diabetes mellitus: a 12-year nationwide retrospective cohort study. Front Endocrinol. (2023) 14:1260566. doi: 10.3389/fendo.2023.1260566
PubMed Abstract | Crossref Full Text | Google Scholar
4. Prisilla, AA, Guo, YL, Jan, YK, Lin, CY, Lin, FY, Liau, BY, et al. An approach to the diagnosis of lumbar disc herniation using deep learning models. Front Bioeng Biotechnol. (2023) 11:1247112. doi: 10.3389/fbioe.2023.1247112
PubMed Abstract | Crossref Full Text | Google Scholar
5. Huang, Z, Xu, B, Liu, Y, Chen, H, Cai, X, Zhang, L, et al. The efficacy and safety of condoliase for lumbar disc herniation: a systematic review and meta-analysis. Front Pharmacol. (2023) 14:1151998. doi: 10.3389/fphar.2023.1151998
PubMed Abstract | Crossref Full Text | Google Scholar
6. Moradi, Z, Shahali, S, Ahmadi, F, and Montazeri, A. Correlates of sexual function in women with acute lumbar disc herniation in Iran: a cross-sectional study. Sci Rep. (2024) 14:6430. doi: 10.1038/s41598-024-57274-w
PubMed Abstract | Crossref Full Text | Google Scholar
7. Martin, BI, Mirza, SK, Spina, N, Spiker, WR, Lawrence, B, and Brodke, DS. Trends in lumbar fusion procedure rates and associated hospital costs for degenerative spinal diseases in the United States, 2004 to 2015. Spine (Phila Pa 1976). (2019) 44:369–76. doi: 10.1097/brs.0000000000002822
PubMed Abstract | Crossref Full Text | Google Scholar
8. Ge, L, Li, J, Shang, W, and Xing, X. Non-operative treatments for lumbar disc herniation: an evidence-based practice guideline. Chin J Evid Based Med. (2024) 24:125–48. doi: 10.7507/1672-2531.202309143
Crossref Full Text | Google Scholar
9. Mao, L, Wang, K, Zhu, W, Shen, ZC, Zhang, XJ, Xie, ZY, et al. Repeat surgery after percutaneous endoscopic lumbar discectomy for adolescent lumbar disc herniation: a multicenter observational study. Orthop Surg. (2024) 16:1336–43. doi: 10.1111/os.14042
PubMed Abstract | Crossref Full Text | Google Scholar
10. Wu, X, and Yuan, W. Progress on treatment and prevention of complications of lumbar disc herniation. China J Orthopaed Traumatol. (2024) 3:219–21. doi: 10.12200/j.issn.1003-0034.20240123
Crossref Full Text | Google Scholar
11. Qin, X, Sun, K, Xu, W, Gao, J, Jiang, H, Chen, W, et al. An evidence-based guideline on treating lumbar disc herniation with traditional Chinese medicine. J Evid Based Med. (2024) 17:187–206. doi: 10.1111/jebm.12598
PubMed Abstract | Crossref Full Text | Google Scholar
12. Chen, Z, Zheng, Q, Chen, S, and Lin, Z. Effect of suspension exercise therapy on lumbar function in patients with chronic nonspecific lower back pain. Rehabil Med. (2022) 32:533–8. doi: 10.3724/SP.J.1329.2022.06009
Crossref Full Text | Google Scholar
13. Li, K, Li, Y, Tang, L, and Yang, Y. The efficacy of using surface myoelectric analysis suspension in the treatment of bilateral muscle imbalances in elderly patients with lumbar disc herniation. Chin J Gerontol. (2020) 40:4987–90. doi: 10.3969/j.issn.1005-9202.2020.23.018
Crossref Full Text | Google Scholar
14. Liu, M, Ai, K, Yi, X, and Li, Q. Clinical efficacy of trunk control training based on children's sling exercise therapy system in the treatment of spastic cerebral palsy. Chinese J Rehabil Med. (2023) 38:490-494+499. doi: 10.3969/j.issn.1001-1242.2023.04.009
Crossref Full Text | Google Scholar
15. Moher, D, Liberati, A, Tetzlaff, J, and Altman, DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. (2009) 339:b2535. doi: 10.1136/bmj.b2535
PubMed Abstract | Crossref Full Text | Google Scholar
16. Higgins, JP, Altman, DG, Gøtzsche, PC, Jüni, P, Moher, D, Oxman, AD, et al. The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. BMJ. (2011) 343:d5928. doi: 10.1136/bmj.d5928
PubMed Abstract | Crossref Full Text | Google Scholar
17. Hu, Y, and Wu, X. Clinical progress of percutaneous laser disc decompression for lumbar disc herniation. Chinese J General Practice. (2013) 11:286–8. doi: 10.16766/j.cnki.issn.1674-4152.2013.02.050
Crossref Full Text | Google Scholar
18. Fujiwara, A, Kobayashi, N, Saiki, K, Kitagawa, T, Tamai, K, and Saotome, K. Association of the Japanese Orthopaedic Association score with the Oswestry disability index, Roland-Morris disability questionnaire, and short-form 36. Spine (Phila Pa 1976). (2003) 28:1601–7. doi: 10.1097/01.BRS.0000077510.95462.39
PubMed Abstract | Crossref Full Text | Google Scholar
19. Fairbank, JC, and Pynsent, PB. The Oswestry disability index. Spine (Phila Pa 1976). (2000) 25:2940–53; discussion 2952. doi: 10.1097/00007632-200011150-00017
Crossref Full Text | Google Scholar
20. Ding, Y, Guo, C, and Li, L. Clinical study on the treatment of lumbar disc herniation by suspension massage exercise technique. Rehabil Med. (2019) 29:33–8. doi: 10.3724/SP.J.1329.2019.01033
Crossref Full Text | Google Scholar
21. Du, X, Cheng, H, and Ma, Y. Effects of respiratory training combined with suspension exercises on lumbar spine function in patients after percutaneous lumbar interbody laminectomy. Chinese J Phys Med Rehabil. (2023) 45:1017–20. doi: 10.3760/cma.j.issn.0254-1424.2023.11.014
Crossref Full Text | Google Scholar
22. Khanzadeh, R, Mahdavinejad, R, and Borhani, A. The effect of suspension and conventional core stability exercises on characteristics of intervertebral disc and chronic pain in office staff due to lumbar herniated disc. Arch Bone Joint Surg. (2020) 8:445–53. doi: 10.22038/abjs.2019.40758.2102
PubMed Abstract | Crossref Full Text | Google Scholar
23. Li, L, Feng, Z, and Sun, J. Clinical observation of sling exercise therapy and meridian plucking manipulation on lumbar disc herniation. Rehabil Med. (2015) 25:10–3. doi: 10.3724/SP.J.1329.2015.04010
Crossref Full Text | Google Scholar
24. Li, L, Wang, Q, Feng, Z, Sun, J, and Lu, H. Study on the therapeutic mechanism of lumbar disc herniation treated by sling and massage exercise technique. Rehabil Med. (2019) 29:13–16+21. doi: 10.3724/SP.J.1329.2019.03013
Crossref Full Text | Google Scholar
25. Li, Z, Liu, Q, and Chao, Z. Observation on the curative effect of suspension exercise therapy on patients with lumbar disc herniation. Chinese J Phys Med Rehabil. (2013) 35:393–5. doi: 10.3760/cma.j.issn.0254-1424.2013.05.017
Crossref Full Text | Google Scholar
26. Liang, Z, Yu, Q, Li, D, Gong, J, Huang, Y, Lin, L, et al. The effects of sling exercise training on patients with lumbar discherniation by activating the weak-link muscles. J Jinan Univ. (2018) 39:345–9. doi: 10.11778/j.jdxb.2018.04.009
Crossref Full Text | Google Scholar
27. Sun, T, Chen, X, Fang, L, and Tang, J. Clinical study of the mulligan maneuver combined with suspension training in the treatment of lumbar disc herniation. Chinese J Rehabil Med. (2015) 30:831–3. doi: 10.3969/j.issn.1001-1242.2015.08.020
Crossref Full Text | Google Scholar
28. Xue, KJ, Zhang, L, Jiang, JL, Yang, H, Jing, PJ, Wang, Z, et al. Combined efficacy of Pregabalin and suspension system in lumbar disc herniation and its impact on JOA and ODI score. Indian J Pharm Sci. (2023) 85:144–8. doi: 10.36468/pharmaceutical-sciences.spl.751
Crossref Full Text | Google Scholar
29. Yang, G, Song, Y, Xue, L, and Zhao, F. Comparative analysis of the clinical efficacy of McGill's method combined with suspension in the treatment of lumbar disc herniation. Chinese J Rehabil Med. (2023) 38:1435–9. doi: 10.3969/j.issn.1001-1242.2023.10.018
Crossref Full Text | Google Scholar
30. Zhang, J, Li, L, Xu, Q, Li, F, Ding, Y, and Wang, N. Effect observation of the sling exercise therapy combined with shock wave on lumbar disc herniation. Rehabil Med. (2018) 28:43–46+51. doi: 10.3724/SP.J.1329.2018.06043
Crossref Full Text | Google Scholar
31. Sun, JL, and Li, L. The efficacy of suspension exercise training in the treatment of lumbar intervertebral disc herniation Chinese. J Rehabil Med. (2014) 29:374–6. doi: 10.3969/j.issn,1001-1242.2014.04.020
留言 (0)