The expansion of artery lumen by 50% in relation to the adjacent part of the vessel presents an aneurysm.[5] When infrarenal dilatation of the aorta is in question, it is an AAA. Such change is in most cases without symptoms, until the aneurysm progresses to rupture. The greatest risk for the occurrence of aneurysm occurs in men at the beginning of geriatric age (65 years); the ratio male to female is approximately 10:3. Thoracic aortic aneurysm exhibits no gender difference and it is more prevalent in younger individuals.[6]
Because there are no effective medical therapies, current clinical intervention for large aneurysm includes two options: Endovascular repair (EVAR) and open surgical repair. EVAR is used for both elective repair and at a ruptured case; a bifurcated or tubular stent-graft over the AAA excludes the aneurysm from arterial circulation. This procedure is superior to open surgical repair. Type II endoleak, with an occurrence rate of 20-30%, is the most common complication after EVAR.[7] Elective EVAR results in lower perioperative mortality than traditional open repair, but after 4 years the EVAR survival advantage is not seen; the results of two European trials have also shown worse long-term outcomes with EVAR than with open repair.[8]
A time for the repair has been recommended when the infrarenal aorta diameter becomes larger than 5.5 cm in men and 5.0 cm in women, due to high incidence of ruptures in non-operated aneurysms.[9] This opinion is based on the data obtained 2002 which show a 9% risk of rupture for aneurysms of 5.5-5.9 cm in diameter within 1 year, compared with 19% for those measuring 6.0-7.0 cm, and 33% for > 7.0 cm in diameter. However, recent studies have questioned this because the incidence of rupture in patients with an AAA <7.0 cm diameter was < 5% per 1 year.[10] This finding gives enough time to many patients for improvement of the pre-existing medical conditions before surgical intervention. With AAA diameter above 7.0 cm, a patient faces much higher risk of rupture. The U.S. Preventive Services Task Force recommends that men with a history of smoking who are 65 to 75 years of age should undergo one-time abdominal aortic aneurysm screening with ultrasonography.
Proper control of hypertension, tobacco smoking, diabetes, and blood lipids may partially slow down AAA growth. However, ACE inhibitors should not be used for blood pressure control in such patients. It is better to use one of the ARB (e.g. losartan, irbesartan, valsartan), because ACE also acts as a kininase. In fact, ACE and kininase II (Figure 1) are the same enzyme.[11,12] Therefore, administration of an ACE inhibitor has a dual action, it decreases angiotensin II and increases bradykinin levels. The latter peptide may stimulate aneurysm’s expansion.
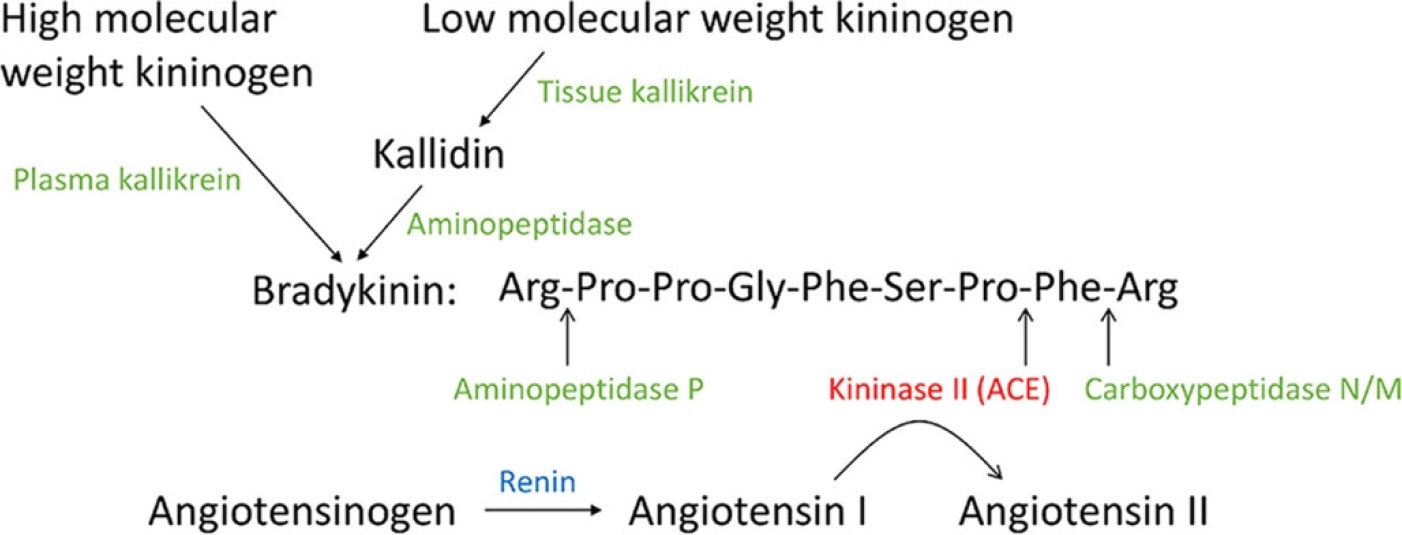
Figure 1:
The peptides and peptidases in the Kallikrein-Kinin System (KKS) and Renin Angiotensin System (RAS). The enzymes in the KKS are shown in green, and renin is shown in blue; ACE (kininase II) is shown in red.
The loss of vascular smooth muscle cells and degradation of the extracellular matrix leads to formation of AAA. New experimental approaches for medical treatment are promising; mouse aneurysm models are frequently used-such as angiotensin II induced abdominal aortic aneurysm in male apolipoprotein E knockout mice (Apoe-/-).[13,14] Pentamethyl quercetin, which inhibits angiotensin II-induced abdominal aortic aneurysm formation by binding to C/EBPβ at Lys253, and reduces the incidence of AAA rupture in mice.[15] Asiatic acid, a triterpene compound, has also been investigated due to its strong anti-inflammatory property. This compound induces aortic remodeling and is useful against blood vessel dissection in the murine model.[16]
留言 (0)