Urolithiasis is among the most frequently encountered urological conditions. Between 1994 and 2010, the global prevalence of urinary stone disease increased from 5.2% to 8.8% (1). Depending on the size, location, and shape, upper urinary tract stones that cannot be removed on their own (≥6 mm) require different interventions such as percutaneous nephrolithotomy (PCNL), rigid ureteroscopy (rURS), flexible ureteroscopy (fURS), and extracorporeal shock wave lithotripsy (ESWL) (2, 3).
One of the most serious conditions of postoperative infection is systemic inflammatory response syndrome (SIRS). SIRS, if not diagnosed in time, can rapidly progress to septic shock with a relatively high mortality rate. Thus, well prediction and timely treatment of SIRS are important for a better outcome (4). Relevant studies have shown that a preoperative positive urine culture is a major risk factor for postoperative infection, and treatment should be based on the results of the urine culture such as upper urinary tract drainage (5). However, for patients with positive urine culture who require surgery, the factors influencing the postoperative incidence of SIRS are still unclear.
In our study, we analyzed the key information of patients with positive urine culture includes preoperative history, preoperative laboratory examinations, operation time, operation methods, intraoperative findings, postoperative vital signs, and postoperative laboratory examinations. We found out two risk factors, one protective factor, and two predictors of SIRS after upper urinary tract stone surgery of the patients with urine culture-positive stones, which provided new insights in the prevention and prediction of SIRS after infection stone lithotripsy.
2 Materials and methods 2.1 Patient data acquisitionFrom January 2022 to December 2023, patients at Wuhan Union Hospital with a preoperative positive urine culture who underwent minimally invasive uroscopic lithotripsy were retrospectively analyzed. The exclusion criteria were (1) a single surgery utilizing two or more types of minimally invasive uroscopic lithotripsy and (2) missing relevant data. The study was approved by the Institutional Ethics Committee of Wuhan Union Hospital.
2.2 Diagnostic standardPatients were categorized into two groups according to whether they developed SIRS after surgery or not. SIRS was defined as the presence of any two or more of the following four criteria: (1) temperature >38°C or <36°C; (2) heart rate >90 /min; (3) respiratory rate >20 /min or PaCO2 < 32 mmHg (4.3 kPa); (4) white blood cell count >12*109 /L or <4*109 /L or >10% immature bands (4).
2.3 Statistical analysisContinuous variables that were not normally distributed with heterogeneous variance were expressed as median (IQR) and compared using the Mann-Whitney test and Kruskal-Wallis test. Categorical variables were compared using the χ2 test or Fisher exact test. Variables selected in multivariate logistic regression analysis were based on past findings and clinical experience. Correlation analysis of continuous variables that were not normally distributed with heterogeneous variance was performed using Spearman's Rank Correlation Analysis. In all the analyses, p < 0.05 was considered statistically significant.
3 Results 3.1 Basic information of the included patientsA total of 393 patients with preoperative positive urine culture were eligible for our study, while 52 (13.23%) of them developed SIRS postoperatively. The incidence rates for PCNL, rURS, and fURS were 14.74%, 8.42%, and 14.82%, respectively. Among all characteristics, surgical duration, preoperative WBC in urinalysis, preoperative nitrites in urinalysis, and hemoglobin drop showed significant differences between the SIRS and non-SIRS group. Their detailed information was shown in Table 1.
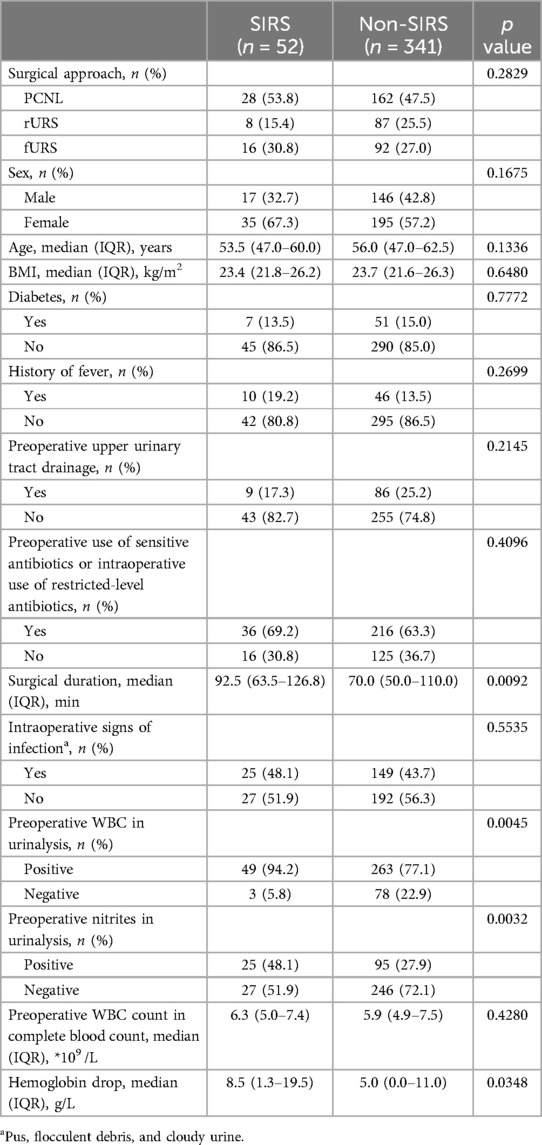
Table 1. Participant characteristics.
3.2 Risk factors and protective factorsBased on previous studies and clinical experience, the following were selected for multivariate logistic regression analysis: history of fever, preoperative upper urinary tract drainage, preoperative use of sensitive antibiotics or intraoperative use of restricted-level antibiotics (such as vancomycin, meropenem, imipenem, teicoplanin, linezolid, and tigecycline), preoperative positive WBC in urinalysis, and a hemoglobin drop exceeding 5 g/L (3, 4). The variables included will ensure independence from each other so that there is no correlation between the two variables. For instance, preoperative WBC in urinalysis and preoperative nitrites may have a strong correlation, we only selected preoperative WBC in urinalysis as one of the regression variables. Furthermore, considering that the factors affecting the surgical duration are multifactorial, related to the location and size of the stone, the power of the laser, etc. Besides, the prolonged surgical duration brings uncertainty in the results. For example, prolonged surgical duration resulting from severe obstruction is a risk factor for SIRS, whereas prolonged surgical duration due to carefully operating is a protective factor. Therefore, we did not include the surgical duration in the regression analysis. The results of multivariate logistic regression analysis were presented in Table 2. Risk factors of postoperative SIRS include preoperative WBC in urinalysis and hemoglobin drop exceeds 5 g/L, while protective factor contains preoperative upper urinary tract drainage.
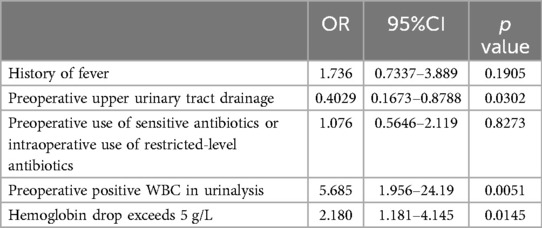
Table 2. Multivariate logistic regression analysis of SIRS (risk factors and protective factors).
3.3 Predictive factorsSimilarly, postoperative C-reactive protein (CRP), procalcitonin (PCT), and serum creatinine were included in the multivariate logistic regression analysis. The results of multivariate logistic regression analysis were presented in Table 3. It showed that postoperative CRP and PCT could be effective predictors of postoperative SIRS.

Table 3. Multivariate logistic regression analysis of SIRS (predictive factors).
3.4 Factors affecting the decrease in hemoglobinKruskal–Wallis test was performed on the postoperative hemoglobin drop of all three surgical procedures PCNL, rURS, and fURS, while the results showed no statistically significant difference (H = 2.879, p = 0.2371). However, the correlation analysis between surgical duration and the decrease in hemoglobin showed a weak correlation with statistically significant difference (r = 0.1589, p = 0.0016).
As for PCNL, the size of the nephrostomy sheath did not have a direct impact on the operative time (r = 0.1058, p = 0.1462) and the hemoglobin drop (r = 0.1229, p = 0.0913), while the use of EMS could effectively shorten the operative time (U = 1,080, p = 0.0062) without significant hemoglobin drop (U = 2,160, p = 0.1338).
4 DiscussionSIRS, which lacks a specific treatment regimen, marks the early stage of urosepsis and often persists throughout its progression, posing significant risks to both morbidity and mortality (3). Similar to previous studies, our data also identified several factors associated with SIRS after lithotripsy for infectious urinary stones. These include risk factors such as preoperative WBC in urinalysis, protective factors such as preoperative upper urinary tract drainage, and predictive factors such as CRP and PCT in the postoperative complete blood count (5–7). In addition, relevant studies have shown that people with positive preoperative nitrites on are more likely to develop septic shock (8). However, since positive leukocytes in the urinalysis were included in the multivariate logistic regression analysis, positive nitrites, which correlate with positive leukocytes, were excluded to maintain variable independence.
Interestingly, to date, no literature has suggested an association between postoperative hemoglobin drop and SIRS, which our multivariate logistic regression analysis identified. The result may be attributed to intraoperative vascular wall injury, which subsequently leads to the entry of infectious bacteria attached to stone particles into the bloodstream. However, this also awaits a clearer causality and needs more detailed evidence, as sometimes severe infections can also lead to a hemoglobin drop. We further analyzed the potentially influential factors for the decrease in postoperative hemoglobin and found no significant differences among the three surgical approaches. However, the surgical duration showed a weak correlation with the decrease in postoperative hemoglobin. This suggests that while the correlation between these two variables is not strong, an underlying association might exist that requires a larger sample size and more precise data for accurate measurement. Regarding PCNL, we found no statistically significant difference in the impact of nephrostomy sheath size on hemoglobin drop. Besides, whether or not using EMS had no significant effect on hemoglobin drop, but the use of EMS could effectively shorten the operative time. This may be due to the higher energy level of EMS, which accelerate the surgery but not causing more injury of kidney (9).
Although our data found a slightly higher incidence of SIRS after PCNL and fURS than rURS, the difference was not statistically significant. And the coverage of PCNL and fURS, which mainly target renal stones and some upper ureteral stones, does not overlap with that of rURS. The factors most closely associated with the occurrence of SIRS were preoperative positive urine WBC and postoperative hemoglobin drop. Besides, the preoperative placement of a double J-stent or nephrostomy tube could reduce the incidence of SIRS. Perhaps in the case of patients with infectious stones, whose urinalysis suggests a large number of leukocytes and CT suggests severe obstruction, drainage should be performed in advance in all patients. And more attention should be paid to minimize vascular wall injury to reduce the possibility of SIRS. In addition, the patient's CRP and PCT should be monitored in the postoperative period, which are good predictors of SIRS. Combining preoperative and intraoperative conditions, if they are abnormally elevated in the 12 h after the surgery or even earlier, it is necessary to choose sensitive antibiotics in a timely manner to prevent septic shock. Furthermore, for larger stones requiring longer surgical duration, the use of EMS can effectively shorten the operative time and improve the stone clearance rate (9, 10). And the 22Fr nephrostomy sheath that is suitable for EMS wouldn't cause an extra hemoglobin drop.
However, our study does have some limitations. Our sample size is still relatively small and lacks more precise data. The number of people who developed SIRS after all three surgical procedures was small, especially after rURS, and the number of people who developed SIRS after rURS was less than 10. Therefore, performing multivariate regression analysis of the risk factors for SIRS in the subgroups of the different surgical procedures would result in statistical error. Additionally, there are certain influential factors that we were unable to consider, such as the surgeon's experience, intrarenal pressure, stone location, severity of hydronephrosis, and duration of obstruction.
In a nutshell, our study has identified several factors associated with SIRS following lithotripsy for infectious urinary stones. Preoperative positive WBC in urinalysis and postoperative hemoglobin drop were found to be significantly associated with SIRS. Preoperative upper urinary tract drainage appears to mitigate the risk of SIRS. Monitoring postoperative CRP and PCT levels can help predict the occurrence of SIRS. Future studies with larger cohorts and comprehensive data collection are needed to validate these results and explore other potential influencing factors. Overall, our findings suggest strategies for reducing the risk of SIRS and improving outcomes in patients undergoing lithotripsy for infectious urinary stones.
Data availability statementThe raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statementThe studies involving humans were approved by Ethics Committee of Wuhan Union Hospital. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributionsXL: Formal Analysis, Investigation, Writing – original draft. YZ: Writing – original draft, Writing – review & editing. HR: Conceptualization, Writing – review & editing. XZ: Conceptualization, Writing – review & editing. LL: Conceptualization, Writing – review & editing.
FundingThe author(s) declare financial support was received for the research, authorship, and/or publication of this article. This study was funded by the Key Research and Development Plan in China (Grant No. 2017YFB1303100), National Natural Science Foundation of China (Grant No. 82102787), and Shenzhen Medical Research Fund (Grant No. B2302054).
Conflict of interestThe authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's noteAll claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References2. Da Silva Ferreira D, Bhattu AS, Adam A. Miniaturizing the approach to upper tract renal calculi: is smaller always better? A narrative review. Curr Urol. (2023) 17(4):280–5. doi: 10.1097/CU9.0000000000000210
PubMed Abstract | Crossref Full Text | Google Scholar
3. Ye S, Wang W, Yu Z, Luo J. Risk factors for systemic inflammatory response syndrome after endoscopic lithotripsy for upper urinary calculi. BMC Urol. (2023) 23(1):59. doi: 10.1186/s12894-023-01230-9
PubMed Abstract | Crossref Full Text | Google Scholar
4. Wang C, Xu R, Zhang Y, Wu Y, Zhang T, Dong X, et al. Nomograms for predicting the risk of SIRS and urosepsis after uroscopic minimally invasive lithotripsy. Biomed Res Int. (2022) 2022:6808239. doi: 10.1155/2022/6808239
PubMed Abstract | Crossref Full Text | Google Scholar
6. Yuan Q, Guo J, He L, Chen Q, Zou X, Yang S, et al. Retrospective analysis of the risk factors and drug resistance of pathogenic bacteria in systemic inflammatory response syndrome after ureteroscopic holmium Laser lithotripsy for impacted ureteral calculi. Int J Gen Med. (2022) 15:3923–31. doi: 10.2147/IJGM.S356540
PubMed Abstract | Crossref Full Text | Google Scholar
7. Tan D, Wu F, Huo W. Clinical characteristics and risk factors of systemic inflammatory response syndrome after flexible ureteroscopic lithotripsy. Arch Esp Urol. (2022) 75(7):618–23. doi: 10.56434/j.arch.esp.urol.20227507.89
PubMed Abstract | Crossref Full Text | Google Scholar
8. Liu Y, Sun Q, Long H, Qiu Z, Zhang D, Zhang H, et al. The value of IL-6, PCT, qSOFA, NEWS, and SIRS to predict septic shock after percutaneous nephrolithotomy. BMC Urol. (2024) 24(1):116. doi: 10.1186/s12894-024-01502-y
PubMed Abstract | Crossref Full Text | Google Scholar
9. Cauni VM, Tanase F, Mihai B, Gorecki GP, Ples L, Sima RM, et al. Single-center experience with Swiss LithoClast(®) trilogy for kidney stones. Diagnostics (Basel). (2023) 13(8):1372. doi: 10.3390/diagnostics13081372
PubMed Abstract | Crossref Full Text | Google Scholar
10. Ozbir S, Atalay HA, Canat HL, Culha MG, Cakır SS, Can O, et al. Factors affecting fluoroscopy time during percutaneous nephrolithotomy: impact of stone volume distribution in renal collecting system. Int Braz J Urol. (2019) 45(6):1153–60. doi: 10.1590/s1677-5538.ibju.2019.0111
留言 (0)