The neurosurgery specialty is a lifelong and arduous process that encompasses various challenges. In Turkey, after the completion of a six-year medical school program, physicians face a challenging exam called the “Medical Specialty Exam.” Based on their performance in this assessment, they are granted the opportunity to choose their respective specializations. Nevertheless, this examination must not be regarded as the sole measure of a physician's level of enthusiasm towards the realm of neurosurgery. During the internship period of their six-year medical curriculum, individuals are engaged in the neurosurgery department for approximately one week.
Recently, there has been a global trend of doctors displaying a reluctance towards pursuing surgical specialties (1). This hesitancy can be attributed to several factors such as the extended duration of residency programs, demanding night shifts, instances of workplace harassment, and other issues within the medical education system (2–4). Consequently, the number of students migrating abroad after completing their medical education has increased, and the inclination towards pursuing specialty training within Turkey has declined (5, 6).
Training programs were established to enhance the surgical skills of medical students (7, 8). However, training camps, particularly in the field of neurosurgery, aimed at catering to the requirements of medical students have recently emerged. These initiatives effectively guide students in making informed decisions regarding their specialization choices and provide them with a comprehensive understanding of the intricate process (9–11).
The Turkish Neurosurgery Academy oversaw the organization of the Neurosurgery Training Camp by the Faculty of Medicine at Bursa Uludag University, in collaboration with the Departments of Neurosurgery and Medical Education. This event was specifically designed for medical students and graduate practitioners, with the primary objectives of assessing their knowledge and skills in the field of neurosurgery, aiding them in making informed choices regarding their specializations, facilitating their engagement in simple surgical interventions, and offering them a glimpse into the potential prospects within this department.
Recognizing the aspirations of students who intend to pursue opportunities abroad, pre-graduation training camps within the field of neurosurgery were established. The fundamental reasoning behind this initiative was to motivate these students to remain in Turkey, instill a feeling of optimism regarding their prospects, and expand their horizons in the process.
In this study, we aimed to highlight the importance of hands-on experiences and mentorship in shaping the future workforce of specialized medical professionals via a Neurosurgery Training Camp.
Materials and methodsThe Turkish Neurosurgery Academy, a division of the Turkish Neurosurgical Society, held the second Neurosurgery Training Camp in 2023. The camp took place at the Bursa Uludag University's Good Medical Practices and Simulation Center, and it was attended by 22 faculty members and 41 students from various towns and universities. Before the camp began, all students had to provide motivation letters outlining their interest in neurosurgery, their previous experience in the subject during medical school, and their expectations for the camp.
Students were assessed using open-ended questions about their interest in neurosurgery before and after the camp (Table 1). The students' answers to open-ended questions and the positive and negative changes in their decisions about choosing Neurosurgery as a career were statistically evaluated.
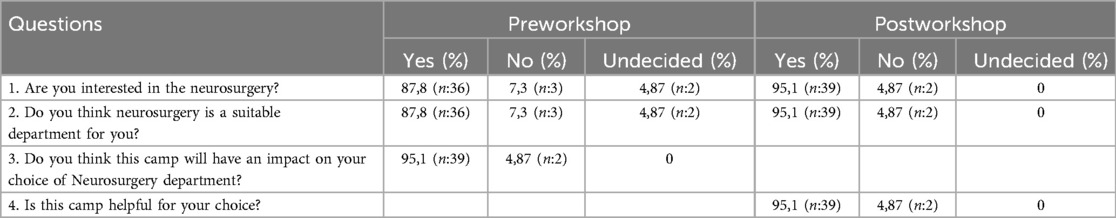
Table 1. Pre and postworkshop questions.
The morning sessions included oral presentations, lectures, and interactive discussion panels. Twenty-two professors discussed their experiences on different subjects with the students (Table 2). At noon, the faculties and students ate together. Each table consisted of 1 professors, a neurosurgery resident from Bursa Uludag University School of Medicine, Department of Neurosurgery, and 6–7 randomly chosen students. At lunch, each student interacted with other students and teachers, exchanging questions and experiences.
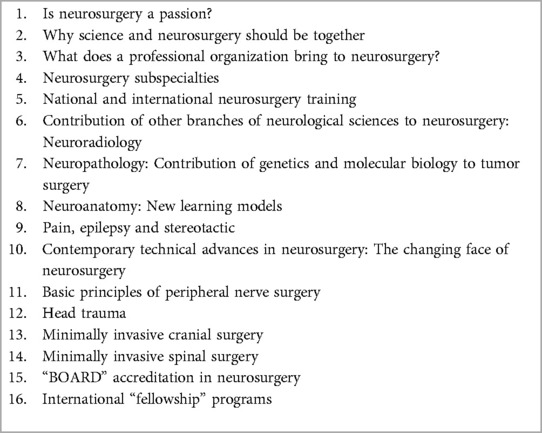
Table 2. Summary of the lectures given.
During the afternoon sessions, students were practically guided by faculty members on utilizing microscopes in neurosurgery, recognizing surgical instruments and devices, and determining locations through stereotactic procedures. This session was subdivided into three segments which were held in different classrooms. During Part 1 of the session, the students performed spinal surgeries such as laminotomy and laminectomy under the guidance of three distinct professors at animal cadaveric spine (sheep). Part 2 of the session involved students receiving hands-on training in surgical knots, dural sutures, microscope use, burr-hole drilling, craniotomy, and scalp-meninges-dura opening at animal cadaveric scalp (sheep). They were supervised by three different instructors. Part 3 of the session covered surgical positions in neurosurgery, characteristics of the surgical table, and utilization of neuronavigation, endoscopes, cavitational ultrasonic surgey aspitators (CUSA), aspirators, and bipolar/unipolar devices (Table 3) (Figure 1A–E).
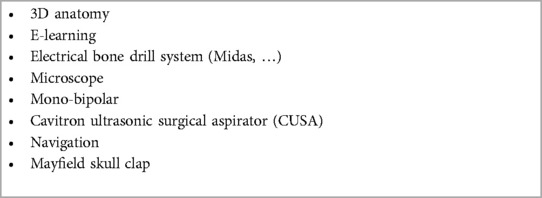
Table 3. Devices/tools used by the students when performing procedures.

Figure 1. Different sections of the camp. (A, B) Section where the microscope and electrical bone drill were used. (C) E-learning section. (D) 3D anatomy section. (E) Students with their program certificate.
All the students were awarded a certificate of participation by the members of the Department of Neurosurgery, Uludag University School of Medicine.
ResultsForty-one students from 10 medical schools participated in our camp. Having participants from 10 different medical schools ensured that there was a diverse range of ideas and experiences, which enhanced the learning atmosphere. The participant gender distribution was balanced (39% women and 61% men) and highlighted the inclusivity of neurosurgical education. At our camp, 46% (n = 19) of the participants were fourth-year students, 19.5% (n = 8) were fifth-year students, and 12.1% (n = 5) were sixth-year students. Approximately 78% of the students were in the final 3 years of their studies (Table 4). The workshop's appeal to a wide range of learners at different stages of their medical education is highlighted by the distribution of students throughout multiple academic years, from first-year to sixth-year students.
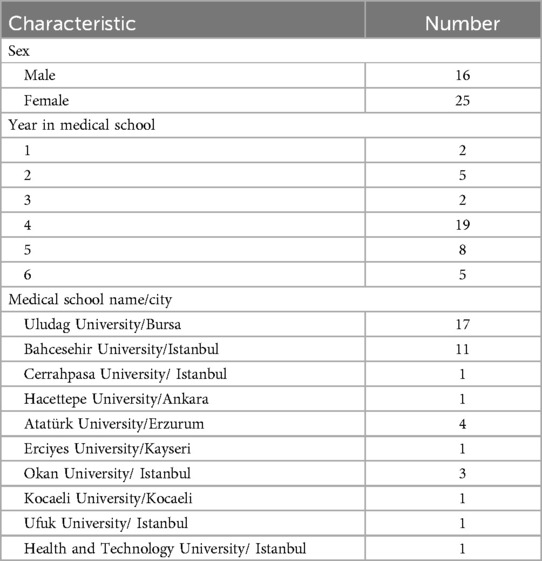
Table 4. Demographic of the attendees.
Post-workshop survey results indicated that 73% (n = 30) of the students chose to pursue a career in neurosurgery following the camp, 21.9% (n = 9) were undecided, and 4.8% (n = 2) decided against pursuing neurosurgery. Two neurosurgery aspirants changed their minds and opted not to pursue the career path after completing the camp. Thus, the camp was beneficial in helping them make a decision.
The postworkshop questionnaire revealed that all students found the camp beneficial in helping them understand what to expect in neurosurgery and making decisions about their career paths.
The answers to the open-ended question highlighted two prominent themes. The first refers to the transmission of knowledge from an expert, while the second pertains to the practical knowledge gained in the specific field of expertise.
One participant expressed that the transfer of experts' experience to career choice had a positive impact. They stated, “Observing the dedication and way of life of faculty members at this level made me reassess everything.” A different attendee highlighted the significance of sharing expertise through presentations and organized discussions at the camp, stating, “Having the opportunity to engage in one-on-one conversations with faculty members during meals and practices and receiving their perspectives was extremely valuable.”
One participant expressed that the transfer of experts' experience to career choice had a positive impact. They stated, “Observing the dedication and way of life of faculty members who have achieved this level made me reassess everything.” Another attendee highlighted the significance of sharing knowledge through presentations and organized discussions at the camp, stating, “Having the opportunity to engage in one-on-one conversations with faculty members during meals and practices and hear their perspectives was extremely valuable.”
The majority of participants concurred that their exposure to medical practices during their specialization period had a positive impact on their career decision. Regarding this matter, a participant expressed, “The practical component of the program proved to be highly beneficial, as it provided us with valuable educational experiences that we may not have encountered prior to completing our studies.” Another participant highlighted the significance of engaging in practical activities during career camps, stating, “I had the chance to explore various technologies, which greatly enhanced my understanding of brain and neurosurgery.”
DiscussionRecently, there has been an increase in unwillingness among medical professionals globally to choose surgical specialties. Factors like extended residency years, rigorous night shifts, workplace harassment, and systemic problems in medical education institutions have led to this pattern (8, 11). Thus, more medical students are looking to migrate abroad after completing their medical education, and their interest in pursuing specialist training in their home countries, such as Turkey, is decreasing.
Events featuring experts and faculty who share their experiences have a significant impact on career choices in medicine. These events provide valuable insights, mentoring, and networking opportunities. Faculty members' reflective narratives can stimulate trainees to engage in introspection and social interaction, motivating them to emulate exemplary figures and mold their professional identities (12). Virtual events, such as webinars and roundtable sessions, are highly effective in enhancing students' exposure to a wide range of specialties, enhancing their understanding of educational pathways, and influencing their decision-making processes regarding their careers demonstrated (13, 14). These events are particularly vital during the COVID-19 pandemic, when traditional face-to-face interactions and clinical exposures are restricted (15). By prioritizing the humanistic aspects of medicine, inclusion has the potential to enhance students' comprehension, empathy, and ultimately impact their career decisions (16, 17).
To address these difficulties and promote the development and retention of skilled individuals in the neurosurgical field, Bursa Uludag University's Faculty of Medicine partnered with the Turkish Neurosurgery Academy to host a Neurosurgery Training Camp. This program was designed to offer medical students and practicing graduates a direct chance to delve into the complexities of neurosurgery, assess their suitability for the specialty, and acquire knowledge regarding the residency process and potential career opportunities in the area.
The camp provided participants with a practical experience, along with mentorship from experienced professionals, to enhance their awareness of the difficulties and benefits of a career in neurosurgery. The communal lunchtime atmosphere allowed professors, neurosurgery residents, and students to network, mentor, and share ideas and experiences. The afternoon sessions involved rotating among seven distinct classes that helped students gain practical experience with various neurosurgical instruments and techniques while being supervised by experts.
The Neurosurgery Training Camp and similar efforts are crucial for integrating academic knowledge with practical implementation. Participants can perform basic surgical procedures under supervision, allowing them to develop confidence and skill.
The postworkshop survey findings demonstrate the camp's significant influence on students' career goals. Approximately 73% of the participants exhibited an interest in pursuing a career in neurosurgery after the camp. This high percentage indicates the workshop's success in inspiring and pushing students to pursue neurosurgery, potentially helping to alleviate workforce shortages and generate interest in a specialized medical field.
Initiatives such as the Neurosurgery Training Camp help medical students and practitioners discover their interests and evaluate their suitability for neurosurgery. This contributes to creating a healthcare workforce that is well-informed and driven. By adopting proactive actions, stakeholders can tackle the issues in medical education and specialist training to maintain a sustainable supply of trained practitioners in essential areas such as neurosurgery.
Study limitationThe short-term thoughts of the students after the camp were learned, but since they had not graduated yet, it could not be evaluated whether the students chose Neurosurgery during the long-term follow-up. Follow-up of students participating in the camp will continue. These camp results will be compared with subsequent groups to obtain comprehensive information. However, only students who wanted to specialize in neurosurgery were included in the camp. This can be considered as an issue that may affect the objectivity of the research.
ConclusionStudents in medical school were effectively inspired and educated about the discipline of neurosurgery via the Neurosurgery Training Camp. The students' career goals and their opinions of neurosurgery were successfully changed by the camp. This was accomplished via a combination of interactive presentations, hands-on experiences, and opportunity to network with other individuals. To adequately foster and support future neurosurgeons, it is vital to continue evaluating and refining educational efforts of this kind. The in-depth analysis of the various components and outcomes of the camp allows us to conclude that the Neurosurgery Training Camp was highly effective in achieving its goals and shaped the students' perceptions on neurosurgery as a career path.
Data availability statementThe raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statementWritten informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributionsHU: Data curation, Formal Analysis, Writing – original draft. MA: Conceptualization, Data curation, Formal Analysis, Investigation, Methodology, Project administration, Writing – review & editing. EB: Formal Analysis, Writing – original draft. PE: Methodology, Project administration, Writing – review & editing. ZA: Supervision, Writing – review & editing, Conceptualization, Data curation, Formal Analysis, Investigation, Methodology, Project administration. MT: Conceptualization, Data curation, Formal Analysis, Investigation, Methodology, Project administration, Writing – review & editing. MK: Formal Analysis, Methodology, Project administration, Software, Writing – review & editing. HK: Methodology, Project administration, Supervision, Writing – review & editing. SD: Methodology, Project administration, Supervision, Writing – review & editing. SY: Methodology, Project administration, Supervision, Writing – review & editing. AB: Methodology, Project administration, Supervision, Writing – review & editing. ZS: Funding acquisition, Methodology, Project administration, Resources, Supervision, Writing – review & editing. KA: Conceptualization, Data curation, Formal Analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Supervision, Validation, Visualization, Writing – review & editing.
FundingThe author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
AcknowledgmentsPreparation for the publication of this article was partly supported by the Turkish Neurosurgical Society. We thank Kaya Aksoy and Nejat Akalan for their insightful discussions and supervisions, as well as the President and members of the Turkish Neurosurgery Academy for their contributions.
Conflict of interestThe authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's noteAll claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References1. Hoffmann H, Dell-Kuster S, Rosenthal R. Medical students’ career expectations and interest in opting for a surgical career. Swiss Med Wkly. (2014) 144:w13932. doi: 10.4414/smw.2014.13932
PubMed Abstract | Crossref Full Text | Google Scholar
2. Boyle E, Healy D, Hill AD, O'Connell PR, Kerin M, McHugh S, et al. Career choices of today’s medical students: where does surgery rank? Ir J Med Sci. (2013) 182(3):337–43. doi: 10.1007/s11845-012-0882-x
PubMed Abstract | Crossref Full Text | Google Scholar
4. McLennan S, Purich K, Verhoeff K, Mador B. Attitudes of Canadian medical students towards surgical training and perceived barriers to surgical careers: a multicentre survey. Can Med Educ J. (2023) 14(5):71–6. doi: 10.36834/cmej.74694
PubMed Abstract | Crossref Full Text | Google Scholar
5. Kaya AE, Aktürk BE, Aslan E. Factors predicting the motivation to study abroad in Turkish medical students: a causal investigation into the problem of brain drain. J Health Sci Med. (2023) 6:526–31. doi: 10.32322/jhsm.1253308
Crossref Full Text | Google Scholar
6. Sancak B, Selek SN, Sarı E. Depression, anxiety, stress levels and five-factor personality traits as predictors of clinical medical students’ migration intention: a cross-sectional study of brain drain. Int J Health Plann Manage. (2023) 38(4):1015–31. doi: 10.1002/hpm.3646
PubMed Abstract | Crossref Full Text | Google Scholar
8. O'Herrin JK, Lewis BJ, Rikkers LF, Chen H. Medical student operative experience correlates with a match to a categorical surgical program. Am J Surg. (2003) 186(2):125–8. doi: 10.1016/s0002-9610(03)00188-0
PubMed Abstract | Crossref Full Text | Google Scholar
9. Radwanski RE, Winston G, Younus I, ElJalby M, Yuan M, Oh Y, et al. Neurosurgery training camp for sub-internship preparation: lessons from the inaugural course. World Neurosurg. (2019) 127:e707–16. doi: 10.1016/j.wneu.2019.03.246
PubMed Abstract | Crossref Full Text | Google Scholar
10. Yearley AG, Ng PR, Gupta S, Cosgrove GR, Mooney MA. Utility of a pilot neurosurgical operative skills boot camp in medical student training. World Neurosurg. (2022) 166:e551–60. doi: 10.1016/j.wneu.2022.07.065
PubMed Abstract | Crossref Full Text | Google Scholar
11. Ashraf M, Ismahel H, Lub S, Gardee A, Evans VE, Middleton EES, et al. Role of a medical student neuro-society organized neurosurgical conference: the Glasgow neuro experience. Surg Neurol Int. (2023) 24(14):70. doi: 10.25259/SNI_755_2022
Crossref Full Text | Google Scholar
12. Khoo SM, Wong XLS. When faculty tell tales: how faculty members’ reflective narratives impact residents’ professional identity formation. Acad Med. (2022) 97(3):385–8. doi: 10.1097/ACM.0000000000004256
PubMed Abstract | Crossref Full Text | Google Scholar
13. Nguyen AX, Pur DR, Lo C, Gottlieb C, Hardy I. Experiences from a national webinar with recently matched Canadian ophthalmology residents for medical students. Can J Ophthalmol. (2022) 57(4):e131–3. doi: 10.1016/j.jcjo.2021.10.004
PubMed Abstract | Crossref Full Text | Google Scholar
14. Hogan D, Geary S, Hennessey DB. The impact of a novel surgical forum, ‘virtual surgical speed dating’, on career perception for medical students: a pilot study. Ir J Med Sci. (2023) 192(6):2987–92. doi: 10.1007/s11845-023-03361-2
PubMed Abstract | Crossref Full Text | Google Scholar
15. Shakir T, Matwala K, Lovett B. SP7.2 Student reported outcomes of a novel virtual medical work experience: results from an international cohort. Br J Surg. (2022) 109:25. doi: 10.1093/bjs/znac247.075
Crossref Full Text | Google Scholar
16. Pirjani R, Rabiei M, Alipour S, Hosseini R, Shahvari Z. Promoting professionalism in practice: using patients’ lived experiences. Med Educ. (2019) 53(5):505. doi: 10.1111/medu.13863
PubMed Abstract | Crossref Full Text | Google Scholar
17. Player E, Gure-Klinke H, North S, Hanson S, Lane D, Culyer G, et al. Humanising medicine: teaching on tri-morbidity using expert patient narratives in medical education. Educ Prim Care. (2019) 30(6):368–74. doi: 10.1080/14739879.2019.1670097
留言 (0)