Hypertension is a major worldwide health concern that leads to increased risk of cardiovascular disease and premature death (1, 2). The use of classic psychedelics – naturally-occurring or derived serotonin 2A receptor agonists that can elicit non-ordinary states of consciousness (3) – has been identified as a potential protective factor for hypertension (4); although, direct investigations of this matter have never been conducted and thus this link remains an open question for future research. Examples of classic psychedelics include psilocybin (the active compound in “magic mushrooms”), lysergic acid diethylamide (LSD), and peyote (a cactus with psychoactive properties).
Despite the possible protective associations between classic psychedelic use and hypertension, there is a need to explore if race and ethnicity might affect these associations for two reasons. First, research on classic psychedelics has suffered from a lack of inclusion and focus on racial and ethnic minorities, limiting the generalizability of prior findings suggesting that these substances may share protective associations with hypertension. Second, there are long documented differences in risk levels for hypertension across different races and ethnicities that may affect the associations that psychedelics share with hypertension as well (5–7). Additionally, there are well-known health disparities in hypertension outcomes for racial and ethnic minorities (8, 9) that may also cause associations between psychedelic use and hypertension to differ for these populations. Thus, the goal of this investigation is to examine if race and ethnicity moderate the associations between classic psychedelic use and hypertension.
Although there is preliminary evidence that classic psychedelics may share protective associations with hypertension, this research suffers from a lack of focus on racial and ethnic minorities and is preliminary. First, Simonsson and colleagues used data from the National Survey on Drug Use and Health (NSDUH) (10) and found protective associations between lifetime classic psychedelic use and hypertension, even after controlling for a host of other potential confounds (e.g., demographic factors, lifetime use of other substances, etc.) (4). Although this work laid an essential foundation for better understanding the link between classic psychedelics and hypertension, this research also did not examine how race and ethnicity may moderate these associations, inviting further investigation into this research domain. Additionally, as psychedelics can also cause transient increases in blood pressure, cardiovascular disease is an exclusion criteria for many psychedelic trials (11); relatedly, there have been no in-depth clinical investigations into the impact of psychedelic use on hypertension. Thus, there is generally a need for more research within this domain, including how race/ethnicity might play a role in the link between psychedelics and hypertension.
Second, healthy lifestyle changes can have a considerable impact on hypertension outcomes (12, 13) and comprehensive reviews have described a number of studies that indicate classic psychedelics can promote such changes (14). However, there is a dearth of research on whether race and ethnicity might affect potential lifestyle changes associated with classic psychedelics. For example, in a study with over 340 participants who stopped or reduced alcohol consumption or misuse after a psychedelic experience, over 60% of the individuals reported improved diet and over 50% reported increased exercise as a result of their experience with psychedelics (15). Yet, nearly 90% of participants in this study were White and only 5.8% were Hispanic, sharply limiting the generalizability of these results. In a similar vein, a study by Anderson et al. (16) found that spontaneous health behavior changes such as improved eating habits and increased exercise were associated with microdosing classic psychedelics. Although these researchers recruited from over a dozen countries, they nevertheless acknowledge that their sample was predominantly “middle class, white, male, and heterosexual”, illustrating that the lack of racial diversity in psychedelic research is pervasive and exists even when one samples within different cultural contexts.
Third, although there is evidence that classic psychedelics may treat mental health disorders that confer increased risk of hypertension, this research has suffered from a lack of diversity as well (17). Classic psychedelics have demonstrated efficacy for treating internalizing disorders such as anxiety and depression – disorders that are known risk factors for hypertension (18, 19) – in a number of high-impact clinical trials (20–23). However, in a comprehensive review of foundational psychedelic trials that have been conducted in recent years, over 80% of participants in these trials were White whereas under 5% of participants were Black or Hispanic (24). Amidst this lack of diversity, there is a clear need to investigate whether prior results on psychedelics and adverse mental health outcomes that put one at risk for hypertension might generalize to diverse populations.
Furthermore, there is preliminary evidence suggesting that associations between psychedelics and adverse health outcomes may differ for racial and ethnic minorities (25, 26), inviting further inquiries into whether such differences exist for associations involving hypertension.
Using data from the National Survey of Drug Use and Health (NSDUH), Jones and Nock (26) and Jones (25) demonstrated that race and ethnicity significantly moderate the associations that psychedelics share with psychological distress, suicidality, and depression. For White participants, both MDMA/ecstasy and psilocybin conferred decreased odds of the aforementioned outcomes. However, for racial and ethnic minorities, there were far fewer of such associations (25, 26). For White participants in Jones & Nock (26), MDMA/ecstasy and psilocybin shared lowered odds of distress and suicidality, but for Black, Hispanic, and Multiracial participants, these associations were non-existent. Additionally, in Jones (25) and for White participants, psilocybin once again conferred lowered odds of depression but did not for Black and Multiracial participants; additionally, for Hispanic participants, psilocybin and MDMA/ecstasy were associated with lowered odds of just one of three depression outcomes, and for Indigenous participants, MDMA/ecstasy was associated with increased odds of depression for two of three outcomes. Additionally, Jones et al. (27) found that psilocybin conferred lower odds of crime arrests for all racial and ethnic groups aside from Black and Hispanic individuals. These results have important implications for psychedelic research as they suggest limits to the generality of existing findings on psychedelics.
Thus, in light of the above findings, the goal of this study is to examine whether race and ethnicity moderate the associations between classic psychedelics and hypertension in a population-based survey sample. This investigation is also a follow-up study to Simonsson et al. (4), which previously found protective associations between classic psychedelics and hypertension (4). Although our investigation cannot be used to make causal claims about the impact of race and ethnicity on the effects of psychedelics, it can make important advancements in our understanding of the associations among identity, psychedelic use, and health.
MethodsData are from the National Survey on Drug Use and Health (2005–2014), an annual survey that aims to collect information on drug use and health outcomes in a nationally-representative sample of the U.S. population. The NSDUH recruits participants by reaching out to a randomly selected, nationally-representative assortment of household addresses across the United States, and collects data via a computer-assisted self-interviewing paradigm wherein field-interviewers administer the survey for participants to complete in their homes. The NSDUH collects data from individuals aged 12 years and older across all 50 states and the District of Columbia. Additionally, the NSDUH survey does not collect data from individuals without a fixed household address, such as active duty military members and homeless individuals who do not reside in shelters. We used data from 2005–2014 as these are all of the years in the NSDUH survey for which there are data on our dependent variable of interest (self-reported hypertension). Lastly, we included all participants aged 18+ years and older in the current study.
This study was exempt from Harvard Institutional Review Board (IRB) review as all data for this project are publicly available at the following web address: https://www.datafiles.samhsa.gov/data-sources.
Analysis planOur analysis plan consists of three main steps. For each step, we conducted survey weighted logistic regression models, allowing us to incorporate the survey design and weighting from the NSDUH into our analyses.
Step 1. First, we assessed the associations that each of the four individual classic psychedelics (psilocybin, peyote, mescaline, and LSD) shared with past-year hypertension. Given that Simonsson et al. found lifetime tryptamine use (i.e., psilocybin) in particular conferred lowered odds of hypertension, we hypothesized that psilocybin would be the substance that conferred lowered odds of hypertension in this follow-up study. This hypothesis was further driven by prior cross-sectional population-based studies demonstrating that tryptamines share the strongest protective associations with health outcomes (e.g., distress, suicidality) compared with other types of psychedelics (28), suggesting that we might see similar results in the current study.
Step 2. After identifying the substance(s) that conferred lowered odds of hypertension, we planned to test whether race and ethnicity significantly moderate the associations that psychedelics share with hypertension.
Putative Moderator. In line with prior research in this domain (25, 26), we used a three level race and ethnicity variable for our moderation analyses (Non-Hispanic White [N = 242,527], Non-Hispanic Participant of Color [N = 79,677], Hispanic [N = 59,478]), reduced from the seven level race/ethnicity variable included in the NSDUH (Non-Hispanic White, Black [N = 46,896], Native American/Alaska Native [N = 5,702], Native Pacific Islander/Hawaiian [N = 1,923], Asian [N = 14,688], Multiracial [N = 10,468], Hispanic). We reduced the number of levels of our moderator a priori for statistical parsimony and to reduce the number of interaction tests in our study, ultimately reducing the likelihood of a Type 1 error (false positive). In interpreting our interactions, we were not concerned with the specific beta values yielded by this model, but simply whether any of the tests were significant, as any positive test would serve to justify the next step of our study.
Step 3. Finally, if our moderation tests yielded any significant results, we planned to break down our sample by race and ethnicity and assess associations between relevant psychedelics and hypertension for individual racial and ethnic groups. This approach allows us to incorporate the unique demographic and substance use profiles of each demographic group into our analyses and generate specific assessments of how the protective associations between psychedelics and hypertension vary across groups.
Dependent Variable (yes/no). Self-reported hypertension in the past year served as the dependent variable for our analyses. Additionally, one’s self-report of hypertension was based on whether a medical professional had diagnosed a given participant with this condition in the past year.
Independent Variable (yes/no). Lifetime use of any of four classic psychedelics (psilocybin, peyote, mescaline, and LSD) served as the independent variable for our study.
Covariates. In line with our prior population based survey research on race and psychedelics (25, 26), we used the following covariates in our analyses: sex, age, income, educational attainment, marital status, survey year, and lifetime use of various substances (MDMA/ecstasy, PCP, inhalants, cocaine, heroin, tranquilizers, stimulants, sedatives, pain relievers, and marijuana).
ResultsThe demographics of our sample, broken down by race and ethnicity, are presented in Table 1. Rates of hypertension were significantly lower amongst Hispanic participants than they were among Non-Hispanic White and Non-Hispanic Participants of Color. In contrast, rates of classic psychedelic use were higher among Non-Hispanic White participants than among the other racial and ethnic groups in the study.
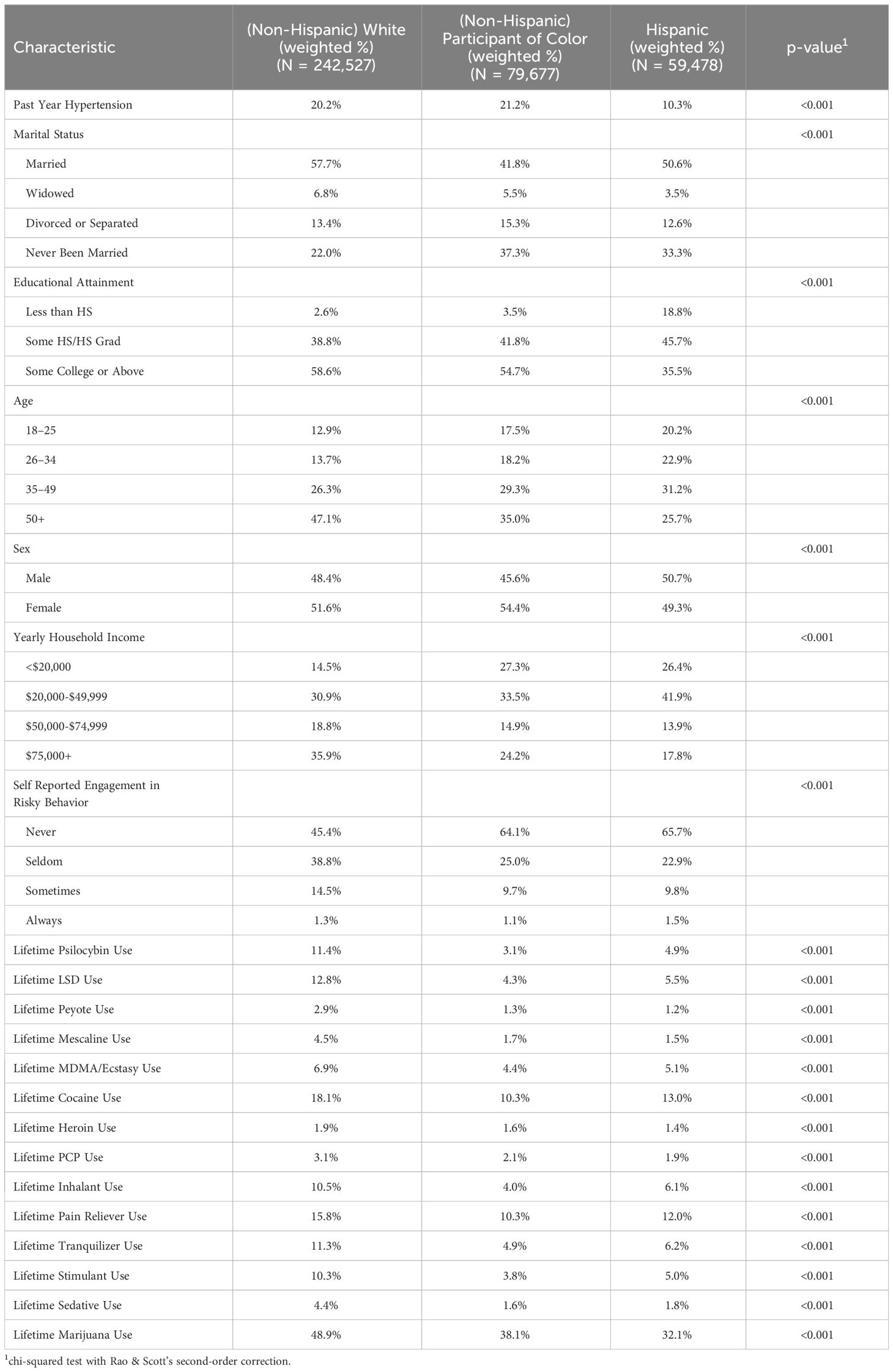
Table 1 Sample demographics and prevalence of past year hypertension and past year substance use, broken down by race and ethnicity.
The results of our preliminary assessment of the associations between the four most commonly used classic psychedelics (psilocybin, peyote, mescaline, and LSD) are presented in Table 2. In line with our hypothesis, psilocybin was the sole classic psychedelic substance that conferred lowered odds of hypertension among the four we assessed. Thus, lifetime psilocybin use served as the independent variable within our analyses.

Table 2 Associations between lifetime use of individual classic psychedelics and past year hypertension.
The results of our interaction tests are presented in Table 3. Overall, the “Hispanic” category interacted significantly with psilocybin for predicting past year hypertension. Given that one of our interaction tests was significant, we proceeded with breaking down our sample by race and ethnicity and assessing the associations that psilocybin shared with hypertension for each racial and ethnic group.
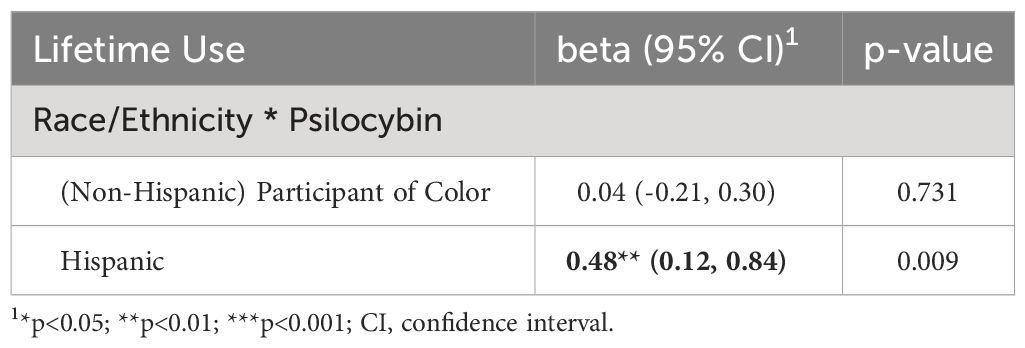
Table 3 Interaction test between race and ethnicity and lifetime psilocybin use for predicting past year hypertension.
The associations between classic psychedelics and hypertension, broken down by race and ethnicity, are presented in Table 4. Psilocybin conferred lowered odds of hypertension only for Non-Hispanic White participants (aOR: 0.83; 95% CI [0.75, 0.92]). There were no other significant associations between psilocybin and hypertension.
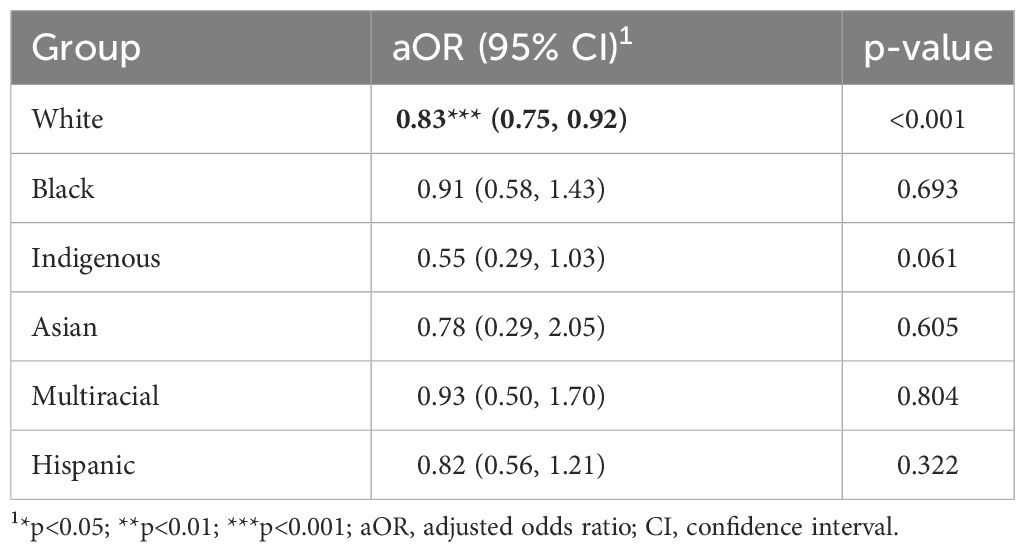
Table 4 Associations between lifetime psilocybin use and past year hypertension, broken down by race and ethnicity.
LimitationsThis study features a number of limitations that are important to state clearly. First and foremost, our study is based on cross-sectional data, meaning that our findings cannot be used to make definitive causal claims. Future longitudinal studies and clinical trials will be needed to address these limitations and determine whether there are causal links between race and ethnicity, psychedelic use, and hypertension.
Second, there are limitations due to the large sample size in this study and our ability to detect small effects as significant. The significant odds ratios in this study are not much lower than 1 (with an OR of 1 representing an independent variable having no significant association with a given dependent variable), suggesting that the associations between psilocybin use and hypertension may be minimal. Future replication studies can address this limitation and determine whether the aforementioned associations exist within other samples.
Third, due to the nature of our main independent variable – lifetime psilocybin use – we could not assess a number of important dosing parameters within this study, such as frequency, dosage, and recency of use. Future studies that include more granular measures of psychedelic use will be needed to overcome this limitation.
Fourth, given that the NSDUH is based on self-report, underreporting represents another potential limitation. This limitation is especially relevant for this study as racial and ethnic minorities are at increased risk of criminal repercussions due to illicit substance use, given the racialized nature of the criminal justice system (29). If racial and ethnic minorities report psychedelic use less frequently than Non-Hispanic White participants, this underreporting may potentially contribute to differences in the associations between psilocybin and hypertension. Follow-up work can assess whether there are differences in the response rates for questions on illegal substances, and subsequently test whether these differences may impact the associations between psychedelics and adverse outcomes.
Fifth, this study used broad, imprecise categories to assess racial and ethnic identity (White, Black, Indigenous, Asian, Multiracial, and Hispanic). Furthermore, the “Hispanic” category has particular limitations, given that this is an ethnic category that includes individuals with a diverse range of racial identities. These limitations stem from the seven-level race/ethnicity variable included in the NSDUH (Non-Hispanic White, Non-Hispanic Black, Non-Hispanic Asian, Non-Hispanic Native American, Non-Hispanic Native Hawaiian/Pacific Islander, Non-Hispanic Multiracial, and Hispanic), which limits our ability to assess identity in more granular ways in this study. There are more comprehensive and flexible ways to assess race and ethnicity in future work (e.g., more detailed race/ethnicity variables, qualitative assessments, assessments of perceived racial identity, etc.). Additionally, it is also likely that a complex interplay of identity factors (i.e., gender, immigration status, socioeconomic status) impact the associations between psychedelic use and hypertension as well. Future investigations should therefore take a more nuanced approach to studying the impact of identity on psychedelics and health, as such investigations can shed further light on our observed findings.
Finally, another potential limitation is that the interaction test for Non-Hispanic racial and ethnic minorities was not significant and the confidence intervals for White participants and some racial and ethnic minority groups overlap, calling into question the validity of our observed differences. However, we do not believe this limitation to hinder our findings. Given that our interaction tests involve pooling the variance from White and Non-White participants to conduct a test of differences, one is disproportionately weighting the model terms of the interaction around White participants. Such a test therefore represents a stringent assessment of differences, meaning that one null result should not prevent further exploration of potential differences between groups using complementary statistical methods. Additionally, our study featured a robust number of participants of color, instilling confidence that our models yielded accurate estimates of the associations between psilocybin and hypertension for each racial and ethnic group. Nevertheless, future longitudinal research and studies featuring even larger sample sizes can address this limitation.
DiscussionWe found that race and ethnicity significantly moderate the previously observed protective association between classic psychedelics – specifically, psilocybin – and hypertension. More specifically, this protective association existed only for Non-Hispanic White participants. These results extend prior research examining the associations between classic psychedelics and hypertension (4), while also replicating recent findings demonstrating fewer protective associations between psychedelics and adverse outcomes for those from racial and ethnic minority groups (25, 26).
Potential explanations for the observed findingsDespite the above limitations, our study makes a significant contribution to the literature by demonstrating the associations between psychedelic use and hypertension vary by racial and ethnic identity. Furthermore, we believe there are a few potential explanations for our results.
Third Variable Factors. Third variable factors may underlie the observed results, as prior research suggests there may be important pre-drug differences between those who have versus have not used psychedelics that may contribute to the associations between these substances and health outcomes. For instance, Johnstad (30) analyzed a sample of 319 individuals who use psychedelics and found that they scored significantly higher on each of the Big Five personality traits except for extraversion (agreeableness, openness, conscientiousness, and neuroticism) (30). Furthermore, a 2017 study by Nour, Evans, and Carhart-Harris found that lifetime psychedelic use was positively associated with a number of potential pre-drug factors, such as affinity with nature, openness, and liberal political views (31). Lastly, there is also evidence that personality factors contribute to a diagnosis of hypertension as well (32, 33), lending further credence to third variable factors as an explanation of our findings. Future investigations can explore a range of third-variable factors as potential mediators of the observed moderation effect in this study.
Additionally, in our study there may be additional demographic differences that exist within and between racial groups that contribute to the observed findings. For example, rates of hypertension are known to increase with age (34), and in our study, there is a higher proportion of 50+ Non-Hispanic White participants (~48% of White participants are aged 50+) than there are for Hispanic participants (~28% of Hispanic participants are aged 50+). Although we controlled for age in all of our analyses, there may be third variable demographic differences that we did not control for that may have driven these results. Other potential third-variable demographic factors that may have driven our results include parental education, level of religiosity, rural vs. urban status, and household ownership status; these factors remain purely speculative, however. Future research can explore how additional third variable demographic factors impact the associations between psilocybin, race, and hypertension.
Racial disparities in hypertension. Second, there are many disparities in hypertension outcomes that exist for communities of color; downstream, such disparities may contribute to our findings in this study demonstrating fewer protective associations between psilocybin use and hypertension. Existing research indicates that racial and ethnic minorities – especially Black Americans and Hispanic Americans – have poorer hypertension outcomes across a host of dimensions (8, 9). Compared to Non-Hispanic White individuals, Hispanic adults have also been noted to have lower levels of hypertension awareness and blood pressure control (35–37). Furthermore, the prevalence of hypertension, as well as hypertension-related deaths, is also elevated for American Indians as compared to many other racial and ethnic groups (38, 39). A 2011–2012 study additionally noted Non-Hispanic Asian individuals had lower awareness of their hypertensive status as well as lower treatment rates for hypertension than did adults from other racial and ethnic groups (39, 40). Lastly, there are generally pervasive disparities in access to healthcare treatment for communities of color (41) which may exacerbate differences in hypertension outcomes for communities of color compared to White populations.
If psilocybin use does share a direct or indirect relationship to reductions in hypertension, such disparities may weaken protective associations that may exist in this domain. Although there is suggestive evidence of potential causes that may underlie these disparities (e.g., differing treatment effects across racial groups, body-mass index differences, dietary factors), no single factor has been identified to explain differences in hypertension outcomes for racial and ethnic minorities (42). Therefore, future research should further explore the causes and conditions that give rise to hypertension disparities, as well as the potential biological mechanisms that may link psilocybin use to lowered odds of hypertension, as these inquiries may shed further light on our observed findings.
Potential health implications of our resultsWhile we cannot make definitive causal claims based on the results in this study, they nevertheless may have important implications for population health and future clinical investigations in this research area.
The odds ratios (ORs) being lower than 1.0 for the relationship between psilocybin use and hypertension in this study indicates that there may be a protective effect of naturalistic psilocybin use on hypertension. It is important to note that effects in our study were small, with the significant ORs ranging between 0.82–0.83 and the non-significant ORs ranging between 0.55–0.93; these ORs are within the range of those observed within prior work in this area, which found ORs of 0.80–0.86 for the associations between psilocybin use and hypertension (4). Despite the small effects, these results still may have important implications for health if they are causal. Foundational health research indicates that small effect sizes can have a large impact in key contexts (43), such as when small effects are applied to large groups. Accordingly, as this study is a large-scale investigation featuring over 380,000 participants, these small effect sizes may indicate a slight, diffuse protective effect of psilocybin use on hypertension at the population-level. However, further research is needed to substantiate this claim.
Furthermore, the significant moderation effect of race/ethnicity on the link between psilocybin and hypertension may have important implications for clinical research as well. If these results apply to causal and experimental contexts, it may imply that psilocybin may vary in its efficacy as a treatment for hypertension depending on one’s racial or ethnic background. Such interpretations are tentative and much further research is needed to validate this possibility. Yet, the clear results in this study – whereby a protective association between psilocybin use and hypertension existed only for Non-Hispanic White participants – certainly invite further inquiry.
A “call to action” for future researchTherefore, we recommend that these findings serve as a “call to action” that motivates additional inquiries into the link between race/ethnicity, psychedelic use, and hypertension. Specifically, we recommend four areas of future research. First, we recommend additional cross-sectional studies, using databases like the NSDUH, to better understand the epidemiology of psychedelic use and hypertension for racial and ethnic minority communities. For instance, future analyses can assess trends in psychedelic use for minority communities and see if trends may differ for those with versus without hypertension. Such studies can start to shed light on the differential patterns of psychedelic use within diverse populations and provide additional context for the results in this study. Second, future qualitative work is essential as well. Qualitative work on the intersection of race/ethnicity, hypertension, and psychedelic use may provide invaluable information about the lived experiences of individuals of color who use psychedelics, and why such lived experiences may have resulted in the differential findings between populations of color versus White populations in the observed work. Third, we recommend longitudinal studies as well. Future studies can recruit large, diverse samples of psychedelic users and matched controls, and document how hypertension changes over time for populations of color compared to White populations. Such findings would enable future causal investigations of our results. And finally, clinical trials can provide definitive answers about whether psychedelics like psilocybin may hold potential for alleviating hypertension and whether these effects may differ for different communities.
ConclusionThis study assessed the moderating role of race and ethnicity on the protective associations that classic psychedelics – specifically psilocybin – share with hypertension. Protective associations between psilocybin use and hypertension existed only for Non-Hispanic White participants. These findings may be explained by third variable factors or racial and ethnic disparities in hypertension outcomes. Additional cross-sectional and qualitative studies can provide more context for our results; furthermore, longitudinal and clinical studies also represent a propitious next step in this line of research, as such studies can assess whether these findings are causal. Overall, this study advances our understanding of the impact that identity may have on the associations between psychedelic use and health, and tees up future research in this domain of inquiry.
Data availability statementPublicly available datasets were analyzed in this study. This data can be found here: https://www.samhsa.gov/data/data-we-collect/nsduh-national-survey-drug-use-and-health.
Ethics statementThe requirement of ethical approval was waived by Harvard University Institutional Review Board for the studies involving humans because the data are publicly available. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation was not required from the participants or the participants’ legal guardians/next of kin because the data are publicly available.
Author contributionsGJ: Conceptualization, Formal analysis, Writing – original draft. JR: Writing – original draft, Writing – review & editing. MN: Writing – original draft, Writing – review & editing.
FundingThe author(s) declare financial support was received for the research, authorship, and/or publication of this article: atai Fellowship (Grant Jones)
Conflict of interestThe authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s noteAll claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References4. Simonsson O, Hendricks PS, Carhart-Harris R, Kettner H, Osika W. Association between lifetime classic psychedelic use and hypertension in the past year. Hypertension. (2021) 77:1510–6. doi: 10.1161/HYPERTENSIONAHA.120.16715
PubMed Abstract | CrossRef Full Text | Google Scholar
6. Douglas JG, Bakris GL, Epstein M, Ferdinand KC, Ferrario C, Flack JM, et al. Management of high blood pressure in African Americans: Consensus statement of the Hypertension in African Americans Working Group of the International Society on Hypertension in Blacks. Arch Internal Med. (2003) 163:525–41. doi: 10.1001/archinte.163.5.525
CrossRef Full Text | Google Scholar
7. Chan Q, Stamler J, Elliott P. Dietary factors and higher blood pressure in African-Americans. Curr Hypertension Rep. (2015) 17:1–8. doi: 10.1007/s11906-014-0517-x
CrossRef Full Text | Google Scholar
12. Drevenhorn E, Kjellgren KI, Bengtson A. Outcomes following a programme for lifestyle changes with people with hypertension. J Clin Nurs. (2007) 16:144–51. doi: 10.1111/j.1365-2702.2005.01493.x
PubMed Abstract | CrossRef Full Text | Google Scholar
13. Ozemek C, Tiwari S, Sabbahi A, Carbone S, Lavie CJ. Impact of therapeutic lifestyle changes in resistant hypertension. Prog Cardiovasc Dis. (2020) 63:4–9. doi: 10.1016/j.pcad.2019.11.012
PubMed Abstract | CrossRef Full Text | Google Scholar
14. Teixeira PJ, Johnson MW, Timmermann C, Watts R, Erritzoe D, Douglass H, et al. Psychedelics and health behaviour change. J Psychopharmacol. (2021) 32:12–9. doi: 10.1177/02698811211008554
CrossRef Full Text | Google Scholar
15. Garcia-Romeu A, Davis AK, Erowid F, Erowid E, Griffiths RR, Johnson MW. Cessation and reduction in alcohol consumption and misuse after psychedelic use. J Psychopharmacol. (2019) 33:1088–101. doi: 10.1177/0269881119845793
PubMed Abstract | CrossRef Full Text | Google Scholar
16. Anderson T, Petranker R, Christopher A, Rosenbaum D, Weissman C, Dinh-Williams L-A, et al. Psychedelic microdosing benefits and challenges: An empirical codebook. Harm Reduction J. (2019) 16:1–10. doi: 10.1186/s12954-019-0308-4
CrossRef Full Text | Google Scholar
17. George JR, Michaels TI, Sevelius J, Williams MT. The psychedelic renaissance and the limitations of a White-dominant medical framework: A call for indigenous and ethnic minority inclusion. J Psychedelic Stud. (2020) 4:4–15. doi: 10.1556/2054.2019.015
CrossRef Full Text | Google Scholar
18. Stein DJ, Scott K, Abad JMH, Aguilar-Gaxiola S, Alonso J, Angermeyer M, et al. Early childhood adversity and later hypertension: Data from the World Mental Health Survey. Ann Clin Psychiatry. (2010) 22:19.
PubMed Abstract | Google Scholar
19. Kretchy IA, Owusu-Daaku FT, Danquah SA. Mental health in hypertension: Assessing symptoms of anxiety, depression and stress on anti-hypertensive medication adherence. Int J Ment Health Syst. (2014) 8:1–6. doi: 10.1186/1752-4458-8-25
PubMed Abstract | CrossRef Full Text | Google Scholar
20. Davis AK, Barrett FS, May DG, Cosimano MP, Sepeda ND, Johnson MW, et al. Effects of psilocybin-assisted therapy on major depressive disorder: A randomized clinical trial. JAMA Psychiatry. (2020) 78:481-9. doi: 10.1001/jamapsychiatry.2020.3285
CrossRef Full Text | Google Scholar
21. Goldberg SB, Pace BT, Nicholas CR, Raison CL, Hutson PR. The experimental effects of psilocybin on symptoms of anxiety and depression: A meta-analysis. Psychiatry Res. (2020) 284:112749. doi: 10.1016/j.psychres.2020.112749
PubMed Abstract | CrossRef Full Text | Google Scholar
22. Carhart-Harris R, Giribaldi B, Watts R, Baker-Jones M, Murphy-Beiner A, Murphy R, et al. Trial of psilocybin versus escitalopram for depression. New Engl J Med. (2021) 384:1402–11. doi: 10.1056/NEJMoa2032994
PubMed Abstract | CrossRef Full Text | Google Scholar
23. Raison CL, Sanacora G, Woolley J, Heinzerling K, Dunlop BW, Brown RT, et al. Single-dose psilocybin treatment for major depressive disorder: A randomized clinical trial. JAMA. (2023) 330:843–53. doi: 10.1001/jama.2023.14530
PubMed Abstract | CrossRef Full Text | Google Scholar
24. Michaels TI, Purdon J, Collins A, Williams MT. Inclusion of people of color in psychedelic-assisted psychotherapy: A review of the literature. BMC Psychiatry. (2018) 18:245. doi: 10.1186/s12888–018-1824–6
PubMed Abstract | CrossRef Full Text | Google Scholar
25. Jones GM. Race and ethnicity moderate the associations between lifetime psychedelic use (MDMA/ecstasy and psilocybin) and major depressive episodes. J Psychopharmacol. (2022) 37:61-9. doi: 10.1177/02698811221127304
PubMed Abstract | CrossRef Full Text | Google Scholar
26. Jones GM, Nock MK. Race and ethnicity moderate the associations between lifetime psychedelic use (MDMA and psilocybin) and psychological distress and suicidality. Sci Rep. (2022) 12:16976. doi: 10.1038/s41598–022-18645–3
PubMed Abstract | CrossRef Full Text | Google Scholar
27. Jones G, Al-Suwaidi M, Castro-Ramirez F, McGuire TC, Mair P, Nock MK. Race and ethnicity moderate the associations between lifetime psilocybin use and crime arrests. Front Psychiatry. (2023) 14:1169692. doi: 10.3389/fpsyt.2023.1169692
PubMed Abstract | CrossRef Full Text | Google Scholar
28. Sexton JD, Nichols CD, Hendricks PS. Population survey data informing the therapeutic potential of classic and novel phenethylamine, tryptamine, and lysergamide psychedelics. Front Psychiatry. (2020) 10:896. doi: 10.3389/fpsyt.2019.00896
PubMed Abstract | CrossRef Full Text | Google Scholar
29. Rosenberg A, Groves AK, Blankership KM. Comparing black and white drug offenders: implications for racial disparities in criminal justice and reentry policy and programming. J Drug Issues. (2017) 47:132–42. doi: 10.1177/0022042616678614
PubMed Abstract | CrossRef Full Text | Google Scholar
30. Johnstad PG. The psychedelic personality: personality structure and associations in a sample of psychedelics users. J Psychoactive Drugs. (2021) 53:97–103. doi: 10.1080/02791072.2020.1842569
PubMed Abstract | CrossRef Full Text | Google Scholar
32. Irvine MJ, Garner DM, Olmsted MP, Logan AG. Personality differences between hypertensive and normotensive individuals: Influence of knowledge of hypertension status. Psychosomatic Med. (1989) 51:537–49. doi: 10.1097/00006842–198909000–00005
CrossRef Full Text | Google Scholar
33. García-Vera MP, Sanz J, Espinosa R, Fortún M, Magán I. Differences in emotional personality traits and stress between sustained hypertension and normotension. Hypertension Res. (2010) 33:Article 3. doi: 10.1038/hr.2009.210
CrossRef Full Text | Google Scholar
36. Redmond N, Baer HJ, Hicks LS. Health behaviors and racial disparity in blood pressure control in the national health and nutrition examination survey. Hypertension (Dallas Tex: 1979). (2011) 57:383–9. doi: 10.1161/HYPERTENSIONAHA.110.161950
PubMed Abstract | CrossRef Full Text | Google Scholar
38. Centers for Disease Control and Prevention (CDC). Vital signs: Avoidable deaths from heart disease, stroke, and hypertensive disease—United States 2001–2010. MMWR Morbidity Mortality Weekly Rep. (2013) 62:721–7.
39. Balfour PC, Rodriguez CJ, Ferdinand KC. The role of hypertension in race-ethnic disparities in cardiovascular disease. Curr Cardiovasc Risk Rep. (2015) 9:1–8. doi: 10.1007/s12170-015-0446-5
CrossRef Full Text | Google Scholar
40. Nwankwo T, Yoon SS, Burt V, Gu Q. Hypertension among adults in the United States: National Health and Nutrition Examination Survey 2011–2012. NCHS Data Brief. (2013) 133:1–8.
41. Riley WJ. Health disparities: gaps in access, quality and affordability of medical care.
留言 (0)