Internet Gaming Disorder (IGD) is listed for further study in the Fifth Edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) (1) and as an addictive disorder in the 11th revision of the International Statistical Classification of Diseases and Related Health Problems (ICD-11) (2). Despite the inclusion of IGD as a clinical diagnosis, there has been slow progress in the development of effective treatment for IGD. IGD is a growing public health concern, affecting both adults (0.3–2.4%) and 7.3% of adolescents (male, 6.8%> female, 1.3%) and globally 2.47% (1.46%–4.16%) (3, 4), while another scoping review reported that IGD prevalence varied from 0.21–57.50% in general populations, 3.20–91.00% in clinical populations, and 50.42–79.25% in populations undergoing intervention for severe cases (5). Adolescents experience hyperactivity, inattention, lower self-esteem, social support, and life satisfaction (6). Hyperactivity/inattention and self-esteem problems seem to be important for the development of IGD, and IGD could prospectively contribute to a deterioration of adolescent mental health (7). Young adults with IGD reported symptoms of depression, anxiety, and stress, lower life satisfaction and elevated motor and attentional impulsivity (8).
Previous reviews of treatment studies (9–12) have several limitations, including problems in the measurement of use and lack of randomized controlled clinical trials. Lampropoulo et al. (13) evaluated treatment interventions in children and adolescents and found that CBT is a widely used intervention; however, for cases with comorbidity, such as depression or attention-deficit/hyperactivity disorder (ADHD), pharmacological intervention proved effective. Danielsen et al. (14) examined treatment studies and proposed a positive impact of therapeutic interventions on gaming disorder, limited by small-study effects, potential publication bias, a restricted study sample, and a lack of standardization. Dong et al. (15) reviewed treatment studies, including established approaches like CBT and newer options like pharmacotherapies and non-invasive brain stimulation (NIBS). They have suggested that CBT is the most extensively researched treatment for IGD and advice cautious implementation of medication-based approaches. In this narrative review, we evaluate the impact of various treatments on IGD behavior, with a particular emphasis on brain imaging findings and recent developments in both psychological and non-invasive treatment options.
2 MethodsWe conducted searches on PubMed/Medline and Scopus using the keywords ‘Internet Gaming Disorder’, ‘Online Gaming’, ‘Brain Imaging’, and ‘Treatment/Intervention’. This yielded 75 studies, out of which 22 were included (10 RCT, 5 new treatments, 7 brain imaging studies). We specifically focused on randomized controlled trials (RCTs) for psychological and pharmacological treatments for IGD. Both authors screened each citation independently, and discrepancies were addressed in the discussion.
3 Results3.1 Psychological treatment- CBT interventionsSeveral studies (Table 1) support CBT as a treatment for IGD. CBT and bupropion were more effective than bupropion alone after 8 weeks of intervention (16). A 6-week study found that both CBT and counselling reduced IGD severity, with no significant difference between the two treatments (17). A single-session implicit training to avoid gaming cues reduced automatic approach tendencies (18). CBT and virtual reality therapy reduced gaming addiction scores (19). A 15-week CBT treatment was more effective than a waiting-list control group in reducing IGD symptoms (20). Additionally, addressing and improving life satisfaction as a secondary outcome measure in this study has been shown to enhance long-term treatment effects and prevent relapse in internet use disorders (21). Training with a stimulus-response-compatibility (SRC) was superior to a pseudo-modification group (22). Finally, a large multicenter RCT with at-risk adolescents found that CBT effectively reduced IGD and unspecified internet use disorder symptoms over 12 months without impacting incidence rates (23). Overall, CBT, medications, and targeted behavioral interventions show promise for treating IGD.
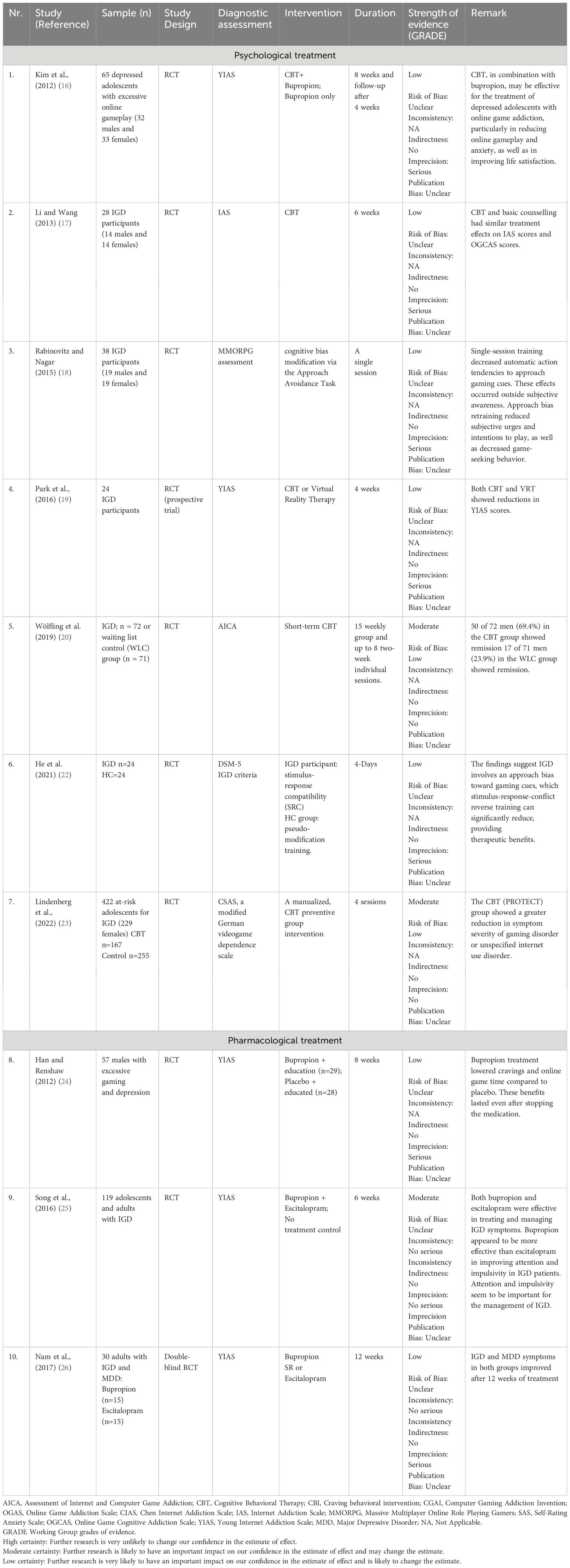
Table 1 Summary of findings: List of studies included psychological and pharmacological treatment for IGD.
3.2 Pharmacological treatment for comorbid IGD and psychiatric disordersThere is evidence for comorbidity of IGD with anxiety disorder and major depressive disorder (MDD). In a 12-week, double-blind RCT, 50 males with IGD and major depressive disorder (MDD) were assigned to bupropion + education or placebo + education groups (24) see Table 1. During active treatment, the bupropion group showed a reduction in Internet Addiction scores, gaming time and Depression Inventory (BDI) scores versus placebo. During the 4-week follow-up, bupropion’s benefits on gaming persisted, but depression recurred, suggesting it may temporarily improve comorbid depression and internet gaming disorder (24). A subsequent 6-week study among adolescents and adults with IGD compared the effects of bupropion and escitalopram to no medication, and both medication groups showed improvement in clinical symptoms versus no medication group, with bupropion being more effective in improving attention and impulsivity (25). In a 12-week, double-blind trial by Nam et al. (26) involving 30 patients with IGD and MDD, treatment with bupropion or escitalopram improved depressive and IGD symptoms in both groups, but bupropion showed greater efficacy in reducing impulsivity and attentional symptoms.
3.3 Emerging treatment approaches3.3.1 Transcranial direct current stimulationTranscranial direct current stimulation (tDCS) targeting the dorsolateral prefrontal cortex (dlPFC) reduces substance use and addictive behaviors, possibly by enhancing inhibitory control over addiction-related triggers. Lee et al. (27) administered tDCS over the DLPFC to 15 online gamers 3 times a week for 4 weeks. They reported decreased weekly hours spent on games, and Internet Addiction Test scores restored the symmetry of DLPFC metabolism. Wu et al. (28) investigated this possibility in 33 males with IGD who underwent active tDCS (1.5 mA for 20 minutes) and sham treatment 1 week apart, randomly assigned, to evaluate inhibitory control over gaming-related distractors and pre- and post-stimulation cravings. Active tDCS reduced interference from gaming distractors but did not affect cue-induced craving. This study was limited by small size and lack of addiction behavior assessments for tDCS.
3.3.2 Repetitive transcranial magnetic stimulationCuppone et al. (29) reported on a 21 young male university student with excessive online gaming activity who received high-frequency rTMS over the left dorsolateral prefrontal cortex (DLPFC), resulting in reduced addictive symptoms and improved executive control, suggesting rTMS may represent an effective treatment for IGD.
3.3.3 Electro-acupunctureRecent studies have shown efficacy in using electro-acupuncture (EA) to treat IGD. Yang et al. (30) studied 32 adolescents with IGD who were randomly assigned to receive either EA (16 participants) or 16 receiving CBT, and 16 healthy volunteers were included as a control group. All adolescents underwent a 45-day intervention. Barratt Impulsiveness Scale (BIS-11) scores, Young’s Internet Addiction Test (IAT), as well as the ratio of brain N-acetyl aspartate (NAA) to creatine (NAA/Cr) and choline (Cho) to creatine (Cho/Cr), were measured by magnetic resonance spectroscopy before and after intervention. Both EA and CBT groups exhibited a decrease in IAT and BIS-11 total scores after treatment. However, the NAA/Cr and Cho/Cr ratios improved in the EA group after treatment but not in the CBT group, indicating that EA might offer benefits over CBT regarding impulsivity control and neuronal protection for individuals with IGD. Peng et al. (31) used electropuncture (EA), psychological intervention (PI), and comprehensive intervention (CI) for the treatment of depression in Internet addiction disorder (IAD). The study involved 120 subjects diagnosed with IAD who were randomly assigned to EA, PI, or CI groups for 40 days. All three treatments effectively reduced scores on IAT, SDS, and HAMD. However, the CI was most effective, followed by EA, and then PI. RCTs conducted by Wu et al. (28) and Yang et al. (30) show promise for tDCS and electro-acupuncture, respectively, while in the prospective single-arm study by Lee et al. (27) the absence of a control group limits the conclusion about its effectiveness; Cuppone et al. (29) offer insights on rTMS for behavioral addiction but lacks generalizability due to the case study format and the absence of a control group.
4 Assessment of the quality of the evidence using GRADE method.Quality of evidence assessments were carried out using Grading of Recommendations Assessment, Development and Evaluation (GRADE) approaches (32). GRADE assessed each study on risk of bias, inconsistency, indirectness, imprecision, and publication bias. An overall high, moderate, low rating was assigned to the body of evidence for each intervention (Table 1). Overall, the quality of evidence for treating IGD is moderate for psychological interventions (mainly CBT) but low to moderate for pharmacological approaches (bupropion and escitalopram). While two large, well-designed RCTs support CBT (20, 23), most other studies for both intervention types suffer from limitations like small sample sizes and potential bias.
5 Discussion5.1 Psychological treatment for IGDCBT is a robust and validated intervention for IGD, only 6 RCTs have evaluated CBT to treat IGD. Han et al. (33) found CBT superior to supportive therapy, with a 66.3% improvement rate and greater reduction in internet addiction, anxiety, impulsivity, and social avoidance. Others have used a more specific treatment for impulsivity; for example, Zheng et al. (34) compared the effects of a single rash impulsiveness intervention (SRC) or behavioral reward sensitivity intervention versus a combined intervention among IGD participants. They reported that the behavioral training of Go/No-go and SRC effectively improved rash impulsiveness and reward sensitivity in IGD, respectively. Still, the intervention effect of the combined training was better than that of the single training. André et al. (35) evaluated relapse prevention as an IGD treatment in an RCT with Swedish adolescents. Both the treatment and control groups showed lower game addiction scale scores at follow-up, but the treatment group had greater improvement compared with treatment as usual. Integrating CBT, motivation, and relapse prevention can also improve treatment for IGD. Sharma et al. (36) reported improvement in 33 individuals with IGD after a 10-session (8-week) intervention combining motivational enhancement, cognitive restructuring, behavioral techniques and relapse prevention. Abstinence is also considered as a potential treatment for IGD. King et al. (11) piloted a voluntary 84-hr abstinence protocol in 24 online gamers, including 9 with IGD. Brief voluntary abstinence successfully reduced gaming hours, maladaptive cognitions, and IGD symptoms. At the 28-day follow-up, 75% of the IGD group showed clinical improvement, and 63% had reduced maladaptive gaming cognitions. Li et al. (37) reported an 8-week mindfulness-based treatment for 30 adults with IGD or problematic gaming, compared to a support group control. Participants in mindfulness treatment had substantial reductions in IGD symptoms meeting DSM-5 criteria, craving, and maladaptive cognitions that were maintained at a 3-month follow-up. Li et al. (38) reported that changes in maladaptive gaming cognitions mediated the beneficial effects of mindfulness for IGD. These findings suggest mindfulness can be an effective approach for targeting cognitive and behavioral symptoms of IGD. Sakuma et al. (39) reported on an intensive 9-day therapeutic residential camp for 10 adolescent males with IGD in South Korea, which comprises psychotherapy, psychoeducational therapy, and CBT components. Months after the camp, participants showed reduced total gaming time, problem recognition related to IGD, and increased self-efficacy for positive change. Finally, Nielsen et al. (40) evaluated family therapy for IGD in 30 adolescents meeting at least 5 DSM-5 IGD criteria, randomized to 12 receiving family therapy or 18 receiving treatment as usual in Switzerland. Over one year, both groups showed decreased IGD prevalence and fewer criteria met, with family therapy outperforming treatment as usual. However, there was no effect on total gaming time. These findings suggest family-based interventions may be beneficial for reducing core IGD symptoms among adolescents beyond standard treatment, though impacts on actual gaming behaviors require further study.
5.1.1 Brain imaging studies of treatment of IGDBrain imaging techniques such as fMRI have provided valuable insights into the neural mechanism underlying IGD and the effects of various treatments. Multiple studies have utilized fMRI to evaluate cue reactivity and craving in individuals with IGD pre and post-interventions, such as craving behavioral intervention (CBI) and acupuncture (Table 2). Zhang et al. (41, 42) found that CBI reduced cue-induced craving, insula activation, and insula connectivity with regions involved in visual processing and attention. Wang et al. (43) reported that recovered individuals exhibited reduced brain activity in the anterior cingulate cortex and lentiform nucleus when exposed to gaming cues, suggesting improved control over cravings. Wang et al. (44) used multi-voxel pattern analysis to identify brain regions involved in successful CBI treatment outcomes. Liu et al. (45) found CBI improved connectivity within the default-mode network, salience and executive control networks in IGD. Regarding acupuncture, Wang et al. (46) observed a reduction in resting-state functional connectivity between the ventral rostral putamen and cortical regions after treatment, correlating with alleviated internet cravings. Another study by Wang et al. (47) showed that acupuncture modulated functional connectivity within the frontal-parietal network and between subcortical nuclei and this network, with symptom improvement correlating with decreased connectivity in specific regions. These imaging studies provide insights into the neural mechanism underlying IGD and the potential therapeutic effects of interventions like CBI and acupuncture. All these studies using fMRI to evaluate brain activity in individuals with IGD employed valid methodologies with control groups selected prior to the studies. However, a limitation is that these studies were not RCTs, which methodologically limits the generalizability and strength of their findings.
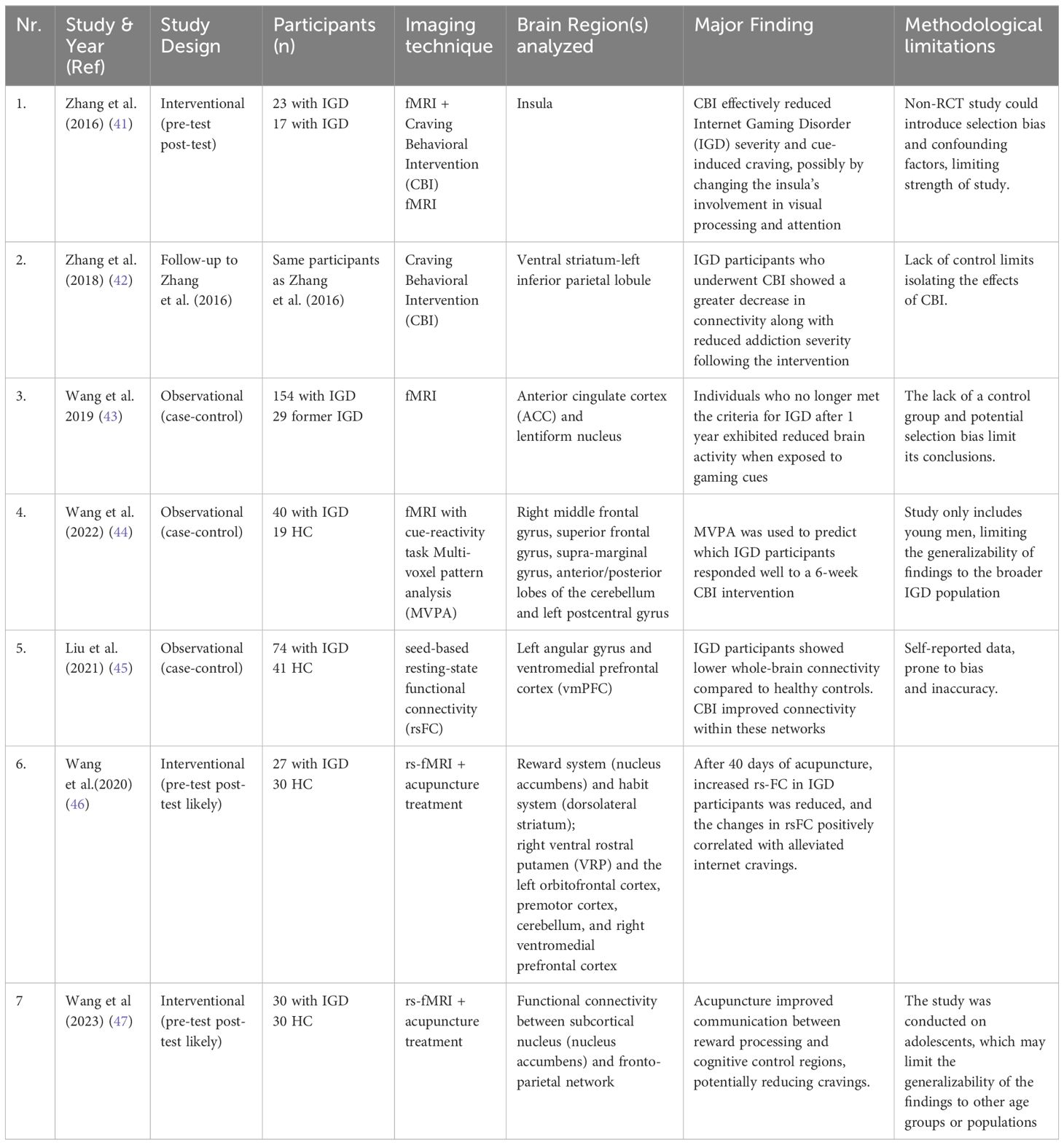
Table 2 Summary of imaging studies.
6 Consideration for treatment of IGDMachado et al. (48) investigated gender differences among 115 adults (20 women, 95 men) seeking treatment for problematic internet use in Brazil. Women showed higher rates of psychiatric comorbidity like mood disorders, anxiety disorders, obsessive-compulsive disorder, post-traumatic stress disorder, and bulimia nervosa compared to men. Women exhibited greater severity in certain behavioral addictions, such as compulsive buying and disordered eating. Gender differences were observed in personality traits, with women scoring higher on impulsivity, novelty seeking, and self-transcendence.
7 Limitations and future directionsThe study addresses a few limitations, including small sample sizes limiting generalizability, lack of long-term follow-up hindering evaluation of treatment durability, inconsistency in diagnostic criteria and assessment measures across studies, potential publication bias inflating treatment effects, and the need to consider co-occurring conditions like anxiety depression and ADHD that might confound results. Further limitations include cultural influences since most studies are carried out in Asian countries. In future research, we emphasize the importance of larger, diverse samples, longer follow-up periods, standardized diagnostic tools, comprehensive literature searches, and addressing co-morbidities. Public health initiatives involving policymakers, healthcare systems, educators and gaming industry stakeholders are critical for preventing and facilitating appropriate treatment access.
8 Ethical and legal issuesThe treatment of IGD presents ethical concerns around informed consent, autonomy, and ensuring confidentiality. Legal issues like data protection and protecting minors’ rights also require attention. Pharmacological risk needs evaluation, and discrimination, stigma, and accessibility issues must be addressed.
9 ConclusionIGD is a growing public health concern that demands attention and effective treatment strategies. This review has examined the current landscape of treatment approaches, including psychosocial interventions, pharmacological interventions, and multimodal strategies.
Author contributionsRS: Writing – original draft, Writing – review & editing. AW: Writing – original draft, Writing – review & editing.
FundingThe author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interestThe authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The author(s) declared that they were an editorial board member of Frontiers, at the time of submission. This had no impact on the peer review process and the final decision.
Publisher’s noteAll claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References1. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition. Arlington, VA: American Psychiatric Association (2013). doi: 10.1176/appi.books.9780890425596
CrossRef Full Text | Google Scholar
2. World Health Organization. ICD-11: International Statistical Classification of Diseases and Related Health Problems. 11th revision. Geneva: World Health Organization (2022). Available at: https://icd.who.int/en.
3. Pan YC, Chiu YC, Lin YH. Systematic review and meta-analysis of epidemiology of internet addiction. Neurosci Biobehav Rev. (2020) 118:612–22. doi: 10.1016/j.neubiorev.2020.08.013
PubMed Abstract | CrossRef Full Text | Google Scholar
5. Darvesh N, Radhakrishnan A, Lachance CC, Nincic V, Sharpe JP, Ghassemi M, et al. Exploring the prevalence of gaming disorder and Internet gaming disorder: A rapid scoping review. Syst Rev. (2020) 9:68. doi: 10.1186/s13643-020-01329-2
PubMed Abstract | CrossRef Full Text | Google Scholar
6. Teng Z, Pontes HM, Nie Q, Xiang G, Griffiths MD, Guo C. Internet gaming disorder and psychosocial well-being: A longitudinal study of older-aged adolescents and emerging adults. Addict Behav. (2020) 110:106530. doi: 10.1016/j.addbeh.2020.106530
PubMed Abstract | CrossRef Full Text | Google Scholar
7. Wartberg L, Kriston L, Zieglmeier M, Lincoln T, Kammerl R. A longitudinal study on psychosocial causes and consequences of Internet gaming disorder in adolescence. Psychol Med. (2019) 49:287–94. doi: 10.1017/S003329171800082X
PubMed Abstract | CrossRef Full Text | Google Scholar
8. Bargeron AH, Hormes JM. Psychosocial correlates of internet gaming disorder: Psychopathology, life satisfaction, and impulsivity. Comput Hum Behav. (2017) 68:388–94. doi: 10.1016/j.chb.2016.11.029
CrossRef Full Text | Google Scholar
9. Zajac K, Ginley MK, Chang R. Treatments of internet gaming disorder: a systematic review of the evidence. Expert Rev Neurother. (2020) 20:85–93. doi: 10.1080/14737175.2020.1671824
PubMed Abstract | CrossRef Full Text | Google Scholar
10. Zajac K, Ginley MK, Chang R, Petry NM. Treatments for Internet gaming disorder and Internet addiction: A systematic review. Psychol Addict Behav. (2017) 31:979–94. doi: 10.1037/adb0000315
PubMed Abstract | CrossRef Full Text | Google Scholar
11. King DL, Kaptsis D, Delfabbro PH, Gradisar M. Effectiveness of brief abstinence for modifying problematic internet gaming cognitions and behaviors. J Clin Psychol. (2017) 73:1573–85. doi: 10.1002/jclp.22460
PubMed Abstract | CrossRef Full Text | Google Scholar
12. King DL, Delfabbro PH. Internet gaming disorder treatment: A review of definitions of diagnosis and treatment outcome. J Clin Psychol. (2014) 70:942–55. doi: 10.1002/jclp.22097
PubMed Abstract | CrossRef Full Text | Google Scholar
13. Lampropoulou P, Siomos K, Floros G, Christodoulou N. Effectiveness of available treatments for gaming disorders in children and adolescents: A systematic review. Cyberpsychol Behav Soc Netw. (2022) 25:5–13. doi: 10.1089/cyber.2021.0067
PubMed Abstract | CrossRef Full Text | Google Scholar
14. Danielsen PA, Mentzoni RA, Låg T. Treatment effects of therapeutic interventions for gaming disorder: A systematic review and meta-analysis. Addict Behav. (2024) 149:107887. doi: 10.1016/j.addbeh.2023.107887
PubMed Abstract | CrossRef Full Text | Google Scholar
15. Dong GH, Dai J, Potenza MN. Ten years of research on the treatments of internet gaming disorder: A scoping review and directions for future research. J Behav Addict. (2024) 13:51–65. doi: 10.1556/2006.2023.00071
PubMed Abstract | CrossRef Full Text | Google Scholar
16. Kim SM, Han DH, Lee YS, Renshaw PF. Combined cognitive behavioral therapy and bupropion for the treatment of problematic on-line game play in adolescents with major depressive disorder. Comput Hum Behav. (2012) 28:1954–9. doi: 10.1016/j.chb.2012.05.015
CrossRef Full Text | Google Scholar
17. Li H, Wang S. The role of cognitive distortion in online game addiction among Chinese adolescents. Child Youth Serv Rev. (2013) 35:1468–75. doi: 10.1016/j.childyouth.2013.05.021
CrossRef Full Text | Google Scholar
18. Rabinovitz S, Nagar M. Possible end to an endless quest? Cognitive bias modification for excessive multiplayer online gamers. Cyberpsychol Behav Soc Netw. (2015) 18:581–7. doi: 10.1089/cyber.2015.0173
PubMed Abstract | CrossRef Full Text | Google Scholar
19. Park SY, Kim SM, Roh S, Soh MA, Lee SH, Kim H, et al. The effects of a virtual reality treatment program for online gaming addiction. Comput Methods Programs Biomed. (2016) 129:99–108. doi: 10.1016/j.cmpb.2016.01.015
PubMed Abstract | CrossRef Full Text | Google Scholar
20. Wölfling K, Müller KW, Dreier M, Ruckes C, Deuster O, Batra A, et al. Efficacy of short-term treatment of internet and computer game addiction: A randomized clinical trial. JAMA Psychiatry. (2019) 76:1018–25. doi: 10.1001/jamapsychiatry.2019.1676
PubMed Abstract | CrossRef Full Text | Google Scholar
21. Müller KW, Dreier M, Beutel ME, Ruckes C, Batra A, Mann K, et al. The impact of life satisfaction in the treatment of gaming disorder and other internet use disorders: Results from a randomized controlled trial. J Behav Addict. (2023) 12:159–67. doi: 10.1556/2006.2022.00091
PubMed Abstract | CrossRef Full Text | Google Scholar
22. He J, Pan T, Nie Y, Zheng Y, Chen S. Behavioral modification decreases approach bias in young adults with internet gaming disorder. Addict Behav. (2021) 113:106686. doi: 10.1016/j.addbeh.2020.106686
PubMed Abstract | CrossRef Full Text | Google Scholar
23. Lindenberg K, Kindt S, Szász-Janocha C. Effectiveness of cognitive behavioral therapy-based intervention in preventing gaming disorder and unspecified internet use disorder in adolescents: A cluster randomized clinical trial. JAMA Netw Open. (2022) 5:e2148995. doi: 10.1001/jamanetworkopen.2021.48995
PubMed Abstract | CrossRef Full Text | Google Scholar
24. Han DH, Renshaw PF. Bupropion in the treatment of problematic online game play in patients with major depressive disorder. J Psychopharmacol. (2012) 26:689–96. doi: 10.1177/0269881111400647
PubMed Abstract | CrossRef Full Text | Google Scholar
25. Song J, Park JH, Han DH, Roh S, Son JH, Choi TY, et al. Comparative study of the effects of bupropion and escitalopram on Internet gaming disorder. Psychiatry Clin Neurosci. (2016) 70:527–35. doi: 10.1111/pcn.12429
PubMed Abstract | CrossRef Full Text | Google Scholar
26. Nam B, Bae S, Kim SM, Hong JS, Han DH. Comparing the effects of bupropion and escitalopram on excessive internet game play in patients with major depressive disorder. Clin Psychopharmacol Neurosci. (2017) 15:361–8. doi: 10.9758/cpn.2017.15.4.361
PubMed Abstract | CrossRef Full Text | Google Scholar
27. Lee SH, Im JJ, Oh JK, Choi EK, Yoon S, Bikson M, et al. Transcranial direct current stimulation for online gamers: A prospective single-arm feasibility study. J Behav Addict. (2018) 7:1166–70. doi: 10.1556/2006.7.2018.107
PubMed Abstract | CrossRef Full Text | Google Scholar
28. Wu LL, Potenza MN, Zhou N, Kober H, Shi XH, Yip SW, et al. Efficacy of single-session transcranial direct current stimulation on addiction-related inhibitory control and craving: A randomized trial in males with internet gaming disorder. J Psychiatry Neurosci. (2021) 46:E111–8. doi: 10.1503/jpn.190137
PubMed Abstract | CrossRef Full Text | Google Scholar
29. Cuppone D, Perez LJG, Cardullo S, Cellini N, Sarlo M, Soldatesca S, et al. The role of repetitive transcranial magnetic stimulation (rTMS) in the treatment of behavioral addictions: Two case reports and review of the literature. J Behav Addict. (2021) 10:361–70. doi: 10.1556/2006.2021.00032
PubMed Abstract | CrossRef Full Text | Google Scholar
30. Yang Y, Li H, Chen X-X, Zhang L-M, Huang B-J, Zhu T-M. Electro-acupuncture treatment for internet addiction: Evidence of normalization of impulse control disorder in adolescents. Chin J Integr Med. (2017) 23:837–44. doi: 10.1007/s11655-017-2765-5
PubMed Abstract | CrossRef Full Text | Google Scholar
31. Peng W, Wang Y, Hao Q, Wang J, Chen Y, Qiu M, et al. Effects of electroacupuncture combined with psychological intervention on depressive status and contingent negative variation in patients with internet addiction disorder: A randomized controlled trial. Front Psychiatry. (2021) 12:722422. doi: 10.3389/fpsyt.2021.722422
PubMed Abstract | CrossRef Full Text | Google Scholar
34. Zheng Y, He J, Fan L, Qiu Y. Reduction of symptom after a combined behavioral intervention for reward sensitivity and rash impulsiveness in internet gaming disorder: A comparative study. J Psychiatr Res. (2022) 153:159–66. doi: 10.1016/j.jpsychires.2022.06.056
PubMed Abstract | CrossRef Full Text | Google Scholar
35. André F, Kapetanovic S, Einarsson I, Trebbin Harvard S, Franzén L, Möttus A, et al. Relapse prevention therapy for internet gaming disorder in Swedish child and adolescent psychiatric clinics: a randomized controlled trial. Front Psychiatry. (2023) 14. doi: 10.3389/fpsyt.2023.1256413
PubMed Abstract | CrossRef Full Text | Google Scholar
36. Sharma M, Bhargav H, Kumar A, Digambhar V, Alka Mani T. Mindfulness-based interventions: Potentials for management of internet gaming disorder. Int J Yoga. (2021) 14:244. doi: 10.4103/ijoy.ijoy_46_21
PubMed Abstract | CrossRef Full Text | Google Scholar
37. Li W, Garland EL, Mcgovern P, O’brien JE, Tronnier C, Howard MO. Mindfulness-oriented recovery enhancement for internet gaming disorder in U.S. adults: A stage I randomized controlled trial. Psychol Addict Behav. (2017) 31:393–402. doi: 10.1037/adb0000269
PubMed Abstract | CrossRef Full Text | Google Scholar
38. Li W, Garland EL, Howard MO. Therapeutic mechanisms of Mindfulness-Oriented Recovery Enhancement for internet gaming disorder: Reducing craving and addictive behavior by targeting cognitive processes. J Addict Dis. (2018) 37:5–13. doi: 10.1080/10550887.2018.1442617
PubMed Abstract | CrossRef Full Text | Google Scholar
39. Sakuma H, Mihara S, Nakayama H, Miura K, Kitayuguchi T, Maezono M, et al. Treatment with the Self-Discovery Camp (SDiC) improves Internet gaming disorder. Addict Behav. (2017) 64:357–62. doi: 10.1016/j.addbeh.2016.06.013
PubMed Abstract | CrossRef Full Text | Google Scholar
40. Nielsen P, Christensen M, Henderson C, Liddle HA, Croquette-Krokar M, Favez N, et al. Multidimensional family therapy reduces problematic gaming in adolescents: A randomised controlled trial. J Behav Addict. (2021) 10:234–43. doi: 10.1556/2006.2021.00022
PubMed Abstract | CrossRef Full Text | Google Scholar
41. Zhang JT, Yao YW, Potenza MN, Xia CC, Lan J, Liu L, et al. Effects of craving behavioral intervention on neural substrates of cue-induced craving in Internet gaming disorder. NeuroImage Clin. (2016) 12:591–9. doi: 10.1016/j.nicl.2016.09.004
PubMed Abstract | CrossRef Full Text | Google Scholar
42. Zhang JT, Ma SS, Li CSR, Liu L, Xia CC, Lan J, et al. Craving behavioral intervention for internet gaming disorder: remediation of functional connectivity of the ventral striatum. Addict Biol. (2018) 23:337–46. doi: 10.1111/adb.12474
PubMed Abstract | CrossRef Full Text | Google Scholar
43. Wang M, Zhang J, Du X, Dong GH, Potenza MN. Functional neural changes and altered cortical–subcortical connectivity associated with recovery from Internet gaming disorder. J Behav Addict. (2019) 8:692–702. doi: 10.1556/2006.8.2019.75
PubMed Abstract | CrossRef Full Text | Google Scholar
44. Wang ZL, Potenza MN, Song KR, Fang XY, Liu L, Ma SS, et al. Neural classification of internet gaming disorder and prediction of treatment response using a cue-reactivity fMRI task in young men. J Psychiatr Res. (2022) 145:309–16. doi: 10.1016/j.jpsychires.2020.11.014
PubMed Abstract | CrossRef Full Text | Google Scholar
45. Liu L, Potenza MN, Lacadie CM, Zhang JT, Yip SW, Xia CC, et al. Altered intrinsic connectivity distribution in internet gaming disorder and its associations with psychotherapy treatment outcomes. Addict Biol. (2021) 26:e12917. doi: 10.1111/adb.12917
PubMed Abstract | CrossRef Full Text | Google Scholar
46. Wang Y, Qin Y, Li H, Yao D, Sun B, Li Z, et al. The modulation of reward and habit systems by acupuncture in adolescents with internet addiction. Neural Plast. (2020) 2020:7409417. doi: 10.1155/2020/7409417
PubMed Abstract | CrossRef Full Text | Google Scholar
47. Wang Y, Qin Y, Li H, Yao D, Sun B, Gong J, et al. Acupuncture modulates the functional connectivity among the subcortical nucleus and fronto-parietal network in adolescents with internet addiction. Brain Behav. (2023) 13:e3241. doi: 10.1002/brb3.3241
留言 (0)