Polycystic Ovary Syndrome (PCOS) is a chronic disorder prevalent among women of all ages with a global prevalence of about 10 to 13% (1). PCOS can manifest with various symptoms across different life stages, including reproductive, dermatological, metabolic, and psycho-socio-sexual problems (2). Despite this multifaceted nature, the psychological, emotional, and social aspects associated with PCOS often receive inadequate attention in clinical practice, leaving many adolescents and women dissatisfied with the prevailing standard of care (3–6). Consequently, women with PCOS seek personalised healthcare that can address their specific health concerns, especially focusing on psychological and emotional well-being and resilience (7–10).
Several studies have indicated an increasing interest among those affected by PCOS in using various traditional, complementary, and integrative medicine (TCIM), such as yoga, meditation, and mindfulness-based therapies gaining popularity in the last few years (11–13). In a cross-sectional survey, it was reported that approximately 80% of ethnic Indian women worldwide diagnosed with PCOS incorporate some form of TCIM into their management regimen, with yoga being the most commonly adopted practice (12). Therefore, it is essential to explore and understand these practices and their potential implications in mitigating PCOS symptoms.
Meditation, originating from the yoga tradition as the seventh limb termed Dhyana, has rich historical origins spanning over 6,000 years (14). Broadly, meditation involves a diverse range of self-taught, self-focused and self-regulatory practices aimed at auto-regulation of neurobehavioral energy, logical relaxation, and achieving a state of ‘unitive being’, with a primary focus on mental training and awareness (15, 16). Meditation encompasses a range of ancient practices originating from Buddhist, Chinese, and Vedic traditions (17). Lutz categorised meditation into two distinct types: focused attention meditation, characterised by an intentional and prolonged concentration on a selected object, and open monitoring meditation, characterised by non-reactive observation of moment-to-moment experiential content (18). Travis and Shear (2010) introduced a third category of meditation practice, termed automatic self-transcending, to help determine its mechanisms or clinical effects encompassing techniques explicitly designed to surpass their own cognitive and operational activities (19). Each category exhibits unique neural correlates, with automatic self-transcending associated with alpha-1 activity, focused attention with beta/gamma activity, and open monitoring with theta activity, drawing upon various traditions including Tibetan Buddhist, Buddhist, and Chinese (19).
Mindfulness, deeply rooted in Buddhist culture, is the most prevalent form of meditation in contemporary research. John Kabat-Zinn defines mindfulness as “the awareness that emerges through paying attention on purpose, in the present moment, and nonjudgmentally to the unfolding of experience moment to moment” (20). Mindfulness practices, whether formal (e.g., breathing, sitting, walking, body scan) or informal (e.g., mindfulness in daily activities), aim to cultivate a state of mindful awareness (21). Several standardised interventions, such as Mindfulness-based Stress Reduction (MBSR) developed by Jon Kabat-Zinn in 1979, and Mindfulness-based Cognitive Therapy (MBCT) developed by Segal, Teasdale and Williams, along with non-standardized mindfulness programs, such as mindful breathing and body scan (22, 23), are of current interest (24–26).
Meditation practices contribute to adaptive cognitive and affective functioning, enhancing positive traits, behaviours, and overall well-being (27). By promoting awareness and regulating attention, meditation aims to relieve physical, mental and emotional distress (28). A comprehensive review of 191 systematic and meta-analytic reviews highlights the versatility of meditation in addressing various health conditions, including anxiety, depression, stress, quality of life (QoL), fatigue, weight management, sleep quality, daily activities, and behavioural changes (29). Mindfulness-based interventions have demonstrated efficacy in managing pain, and negative emotions, cultivating self-compassion, and enhancing mindfulness, social connections, and positivity (30).
Employing additional strategies beyond the symptomatic treatment of PCOS becomes increasingly important in the holistic management of women with PCOS. Moreover, cost-effective strategies capable of alleviating psychological burdens, promoting healthy behavioural changes, and enhancing overall quality of life are increasingly warranted. Previous systematic reviews have reported inconsistent findings regarding the efficacy of yoga-based meditation and mindfulness in managing PCOS symptoms (11, 31). Meditation was not assessed independently in these reviews, and recent studies have since been published. Therefore, the objective is to provide an updated summary of the evidence pertaining to meditation/mindfulness interventions (MMIs) and their therapeutic potential in optimising PCOS management.
MethodsThe methods employed in this study adhered to a predetermined protocol. The search strategy and methods for extracting data were congruent with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for Scoping Reviews (PRISMA-ScR) checklist. Extensive literature searches were conducted across multiple databases including Medline OVID, Scopus, PubMed, PsychInfo, and CINAHL, spanning from inception to March 2023 for identifying current evidence on MMIs in PCOS. The keywords and search strategies used in Medline are described in Supplementary Table 1, with similar search strategy approaches applied to other databases. Original experimental studies published in English on meditation/mindfulness alone or in combination with other treatments in women diagnosed with PCOS using research designs such as randomised controlled trials (RCTs), quasi-experimental, single-arm, and pre-post were included. No restrictions were imposed regarding participants’ age, PCOS diagnosis criteria or the type or duration of the MMIs used. Excluded from consideration were reviews, case studies/series, qualitative studies, and studies utilising alternative research methodologies. Citations were extracted and duplicates were removed using Endnote (32).
Covidence (33) was used to manage the screening process. VR, JG and APD conducted the abstract and full-text screening in duplication. Any discrepancies that arose from the two screening processes were resolved by discussion and consensus, with consultation among all authors where needed. Data extraction tables were initially developed by one author (VR) and subsequently refined based on feedback from two authors (APD, NC). Data extraction from eligible studies was conducted independently by one author (VR) using Microsoft Excel (version 16.68) and subsequently verified for accuracy and completeness by another author (AJ). Extracted data included study design, participant demographics and settings, intervention characteristics, and any reported adverse events and outcomes related to PCOS features. A narrative descriptive summary of the current evidence was constructed employing the Population, Intervention, Comparison, and Outcome (PICO) method.
ResultsStudy selectionThe search strategy yielded 6742 records, of which 3385 independent studies were eligible for title and abstract screening after the removal of duplicates. Finally, 70 citations were retrieved for full-text screening, out of which 17 citations representing 14 trials (one trial having four citations) satisfied the inclusion criteria and were included in the analysis. The article selection process is visually presented in the PRISMA flow chart (Figure 1).
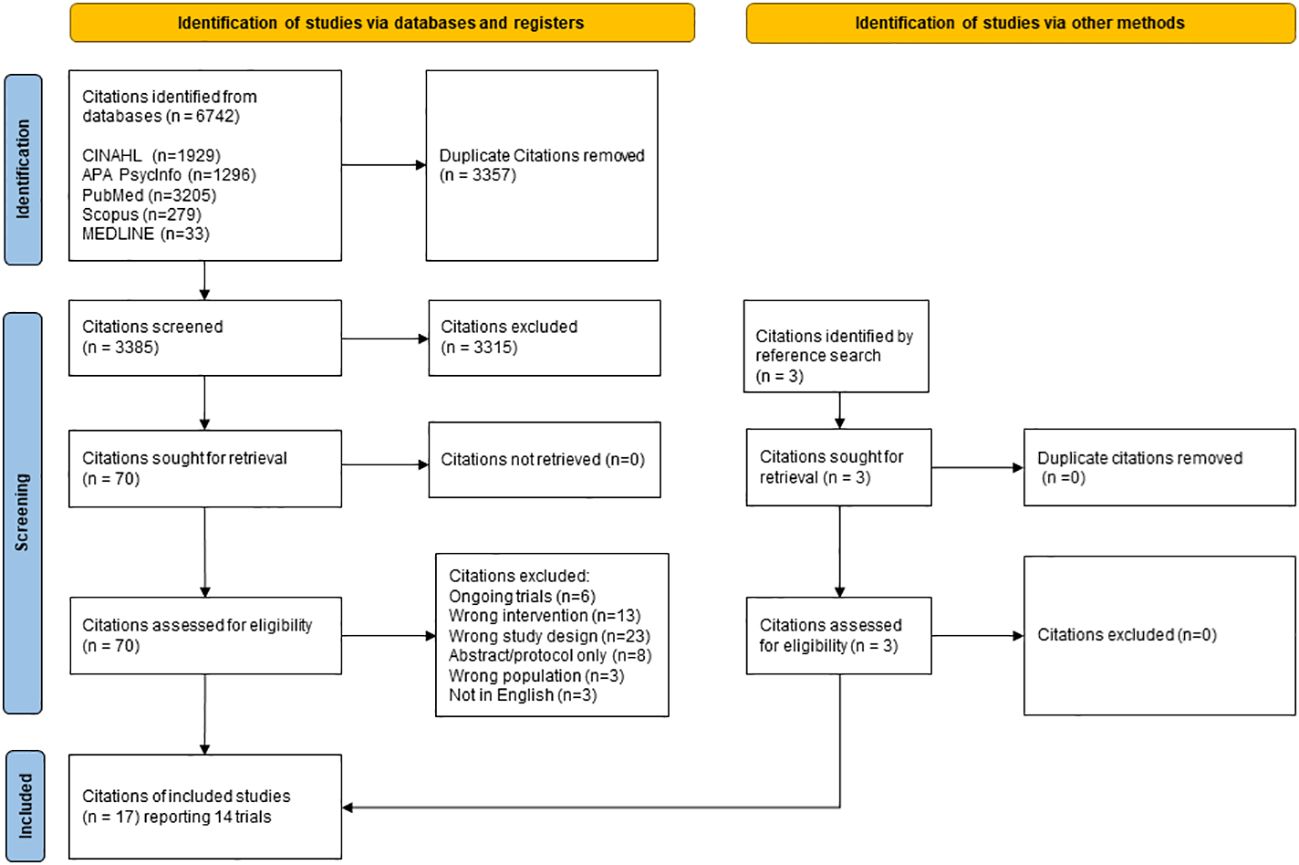
Figure 1 Legend: Flow chart of the study selection process.
Study CharacteristicsAmong the 14 trials, nine trials were RCTs (12 citations) (34–45), four were single-arm trials (46–49) and one was a quasi-experimental trial (50). The distribution of trials across geographical locations included six trials (9 citations) conducted in India (34–37, 39, 44, 46, 47, 49), four in the USA (40, 42, 45, 48), and one each in China (41), Iran (50), Greece (38) and Slovenia (43). Refer to Table 1 for a summary of available evidence.
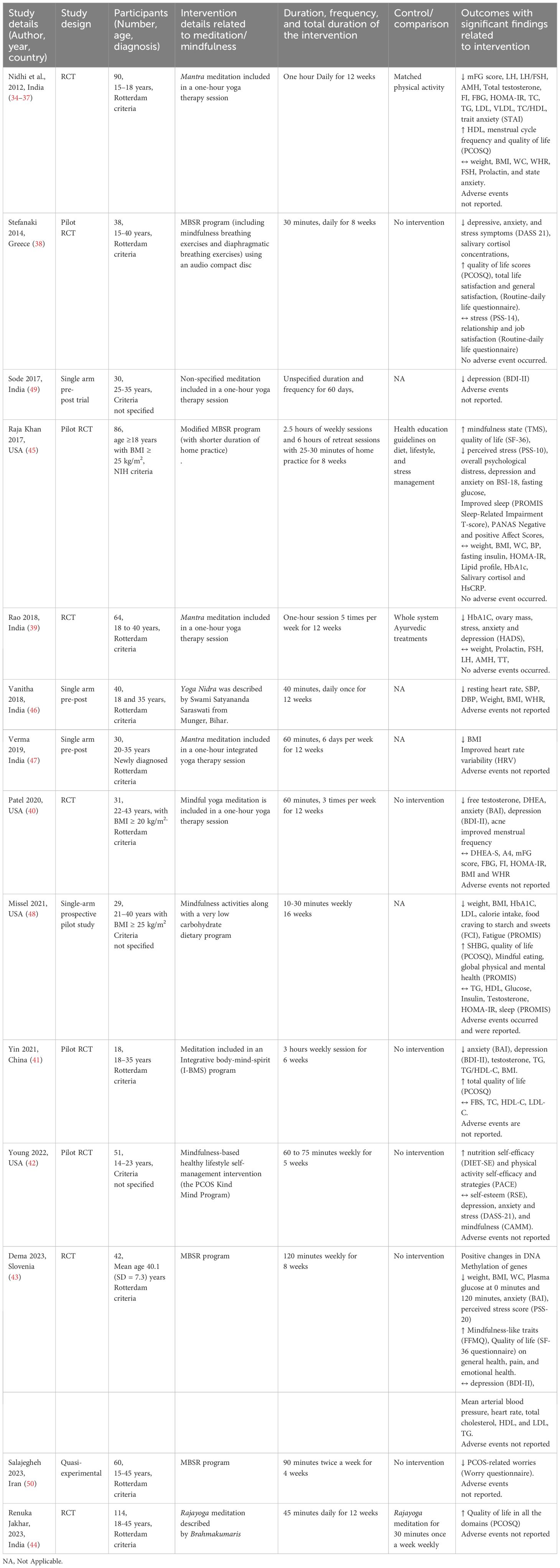
Table 1 Summary of trials investigating the role of meditation and mindfulness in PCOS.
ParticipantsThe collective sample size across the 14 trials comprised 723 participants, with individual trial sample sizes ranging from 18 to 114 participants. Age ranges varied across trials, with one trial specifically involving individuals aged 15 to 18 years (34–37). Three trials involved both adolescent and adult participants, with one study involving individuals aged 15 to 40 years (38), another involving individuals aged 14 to 23 years (42), and a third study involving individuals aged 15 to 45 years (50). The remaining ten trials focused on participants aged 18 and above. Diagnostic criteria for PCOS varied across trials, with one trial using the National Institutes of Health (NIH) criteria (51), three trials not specifying the diagnosis criteria (42, 48, 49), and the remaining 10 trials using the Rotterdam criteria.
InterventionsSeveral meditation practices, such as Rajayoga meditation, described by Brahmakumaris (44), and Yoga Nidra (46), were used. Three trials (6 citations) used OM meditation in holistic yoga therapy, including other components of yoga, such as asana and pranayama (breathing) practices (34–37, 39, 47). Two trials included unspecified forms of meditation (41, 49). Four studies used the MBSR program (38, 43, 50, 51). One trial included mindfulness-based activities, such as mindful eating (48), and another trial employed a mindfulness-based healthy lifestyle self-management program (PCOS kind mind) (42). One trial used mindful yoga (40). Intervention durations ranged from 10 minutes to 2.5 hours per session, spanning study durations of 4 to 16 weeks. Most interventions were administered by trained therapists, with one study comparing different durations of meditation practices (44). Adherence was reported in five trials (39, 41, 42, 48, 51).
Control/comparisonsAmong the 14 trials, four were single-arm trials and thus lacked a control intervention (46–49). Four trials used active interventions (34–37, 39, 44, 51), while the remaining six used control groups without active interventions.
OutcomesThe studies investigated various PCOS-related outcomes, with psychological parameters being the most commonly examined (n=11/14), followed by anthropometric (n=9/14), metabolic (n=7/14) and QoL outcomes (n=7/14). Reproductive outcomes were reported in four trials. Three trials examined the impact of mindfulness-based interventions on participants’ mindfulness. Three trials investigated heart rate variability, two trials studied sleep, two trials studied diet and physical activity-related parameters, and one study explored fatigue.
Various psychological outcomes, including anxiety, depression, stress, PCOS-related worries, and overall psychological distress, were examined. Several subjective questionnaires/tools were used to evaluate these psychological outcomes among participants. The used questionnaires/tools included Beck’s Depression Inventory-II (40, 41, 43, 49), The Depression, Anxiety and Stress Scale - 21 Items (38, 42), Hospital Anxiety and Depression Scale (39), Beck Anxiety Inventory (40, 41, 43), The State-Trait Anxiety Inventory (36), Brief Symptoms Inventory-18 (45), and The Perceived Stress Scale (38, 43, 45). Most trials reported improvement in psychological parameters, except for one 5-week study that indicated the need for an extended follow-up assessment to comprehensively evaluate psychological parameters (42).
The effects on anthropometric parameters were varied. Five of the nine trials showed improvement in anthropometric parameters: weight (43, 46, 48), BMI (41, 43, 46–48), waist-to-hip ratio (46) and waist circumference (43). However, four trials reported no significant improvement in these parameters (37, 39, 40, 51). None of the four trials reporting on reproductive outcomes assessed pregnancy and related outcomes. Among these, two trials reported an improved frequency of the menstrual cycle (34, 40), while one reported a decrease in ovarian mass (39). Two trials reported clinical hyperandrogenism evaluated by the modified Ferriman-Gallwey (mFg) score, with a significant decrease in one trial (34) and no significant changes in another trial (40). Two trials reported decreased biochemical hyperandrogenism – total testosterone (34, 41), free testosterone (40), and dehydroepiandrosterone (40). One trial reported increased levels of sex hormone-binding globulin (48).
Improvement in QoL of life was reported in seven trials (38, 41, 43–45, 48); the Polycystic Ovary Syndrome Quality of Life (PCOSQ) scale and Short Form Survey (SF-36) were used to assess the QoL among the participants. Three trials reported improvement in mindfulness-related traits (43, 48, 51) using the Toronto Mindfulness Scale and Five Facet Mindfulness Questionnaire for evaluating mindfulness. Two trials studied the effect of meditation on heart rate variability (46, 47). One trial studied changes in DNA methylation (43), self-efficacy regarding diet, physical activity, sleep and behavioural changes (42), general and physical health (48), and overall life satisfaction (38). The mindful eating trial observed less calorie intake and reduced cravings for sweets and carbohydrates as improvements associated with mindful eating.
Whilst most trials (n=10) did not mention the occurrence or non-occurrence of adverse events during the study period, three trials specified the absence of adverse events (38, 39, 51). One trial reported the incidence of adverse events, including kidney stone development, continuous muscle cramping and blurry vision (48). It is important to note that this trial was predominantly focused on dietary-dominant mindfulness interventions and the causal relationship between these adverse events and mindfulness remains uncertain.
In sum, psychological outcomes were evaluated using various standardised tools, with most trials reporting improvements in psychological parameters. Improvement in anthropometric parameters varied across trials, with some indicating significant improvements while others showed no significant changes. Reproductive outcomes primarily focused on menstrual cycle frequency and clinical and biochemical hyperandrogenism. Improvement in QoL was reported in seven trials, while three trials reported enhancement in mindfulness-related traits. Adverse events were infrequently reported, with some trials observing their absence while others reported incidents, such as kidney stone development and muscle cramping, albeit with uncertain causal relationships to the interventions.
DiscussionThe study provides a brief description of existing evidence concerning the efficacy of MMIs in alleviating symptoms associated with PCOS. The findings contribute to informing both ongoing and future research in this field. Most of the trials studied the impact of MMIs on psychological parameters, with a noteworthy absence of studies investigating pregnancy and related outcomes. A significant gap was found in the reporting of adherence and adverse events associated with MMIs. The current state of reporting regarding MMI delivery is deemed suboptimal, highlighting the necessity for improvement in future studies.
The concept and utilisation of meditation in the Eastern world transcends its role as a mere disease management tool, including aspects of self-help and spiritual well-being (52). Specific meditative techniques are seamlessly integrated into traditional health approaches in these countries. For example, meditation is included in yoga and Ayurveda (53). The diversity in the forms of MMIs used across various settings is evident. For instance, yogic meditation was the most used in India, while mindfulness-based practices were extensively explored in the USA. This discrepancy could be attributed to the cultural adaptation of meditation practices in Western contexts (54). Thus, it is vital to contextualise these practices when reporting or evaluating their effects. Furthermore, future studies should rigorously document and explain both the characteristics of the intervention provider and the intervention itself.
The implementation of complementary strategies, such as MMIs, holds promise, particularly in high-risk population groups, such as adolescents. This demographic stands to derive substantial benefits from complementary strategies aimed at facilitating weight management, improving lifestyle choices and mitigating the onset of reproductive-endocrine disorders (55). Meditation serves as a practical, cost-effective tool offering both physical and emotional benefits that extend beyond single interventions. Insights derived from studies covering adolescents and women afflicted with PCOS highlight the utility of meditation in facilitating psychological and metabolic outcomes amongst adolescent populations. These outcomes encompassed improvements in self-efficacy across various lifestyle domains. These findings are similar to observations from previous studies examining meditation and mindfulness interventions in non-PCOS adolescent populations, wherein significant reductions in psychological and emotional distress and improvements in self-esteem, mindfulness traits and overall quality of life (56–59) were observed. Furthermore, evidence supports the role of MMIs in mitigating addiction rates, increasing resilience and improving self-efficacy in managing chronic illnesses among this population (60–64). Consequently, early engagement in healthy lifestyle behaviours and MMIs among adolescent girls holds the potential to serve as a cornerstone in the management of PCOS. Future large studies with extended durations and employing appropriate diagnostic criteria among adolescents diagnosed with PCOS, and those at risk of developing PCOS, are warranted to explore the role of MMIs in PCOS management comprehensively.
Psychosocial co-morbidities are highly prevalent amongst women with PCOS and often contribute to reduced QoL (65). The majority of studies included in this review reported that MMIs reduced stress, anxiety and depression associated with PCOS. Similarly, the role of MMIs in improving psychological health, well-being and QoL was evident in non-PCOS individuals with mental health conditions (66–70). Golbery et al. concluded that meditation has results similar to standard treatments, such as psychotherapy for mental health conditions. A recent RCT by Bringmann et al. demonstrated that a meditation-based lifestyle program can help manage mild-moderate depression in the non-PCOS population (71). These findings indicate the potential of MMIs as a psychotherapeutic tool in managing psychological well-being, warranting further investigation in women with PCOS.
Lifestyle modifications are the primary therapeutic approach in the management of PCOS among women (1), primarily aiming at weight management through a combination of dietary modifications, exercise regimens and behavioural changes (72). However, women often encounter several barriers while adopting a healthy lifestyle (73, 74). A significant correlation between obesity, state of mind and food cravings aggravates this challenge, forming a vicious cycle (75). Previous studies involving non-PCOS adults support the effectiveness of MMIs not only in facilitating weight reduction (76, 77), but also in changing obesity-related eating behaviours, such as emotional, binge, and excess eating, thereby facilitating weight management (76, 78–83). Similarly, the study findings suggest that MMIs may improve self-efficacy and promote weight loss among individuals with PCOS (42, 43, 47, 48, 51).
Studies assessing the role of MMIs in eating behaviours suggested improvements in individuals’ relationships with food and reductions in psychological distress among those struggling with obesity (84). For example, mindful eating practices increase awareness of hunger, fullness, cravings, and triggers associated with dietary habits (85). MMIs also directly target ingrained behavioural patterns, such as faulty eating patterns, cravings, and addictions (86, 87). Thus, the exploration of MMIs is proposed as it holds promise in optimising lifestyle modifications and facilitating weight management among women afflicted with PCOS.
Strengths and limitationsThe adoption of the PRISMA-ScR checklist facilitated the identification of studies examining the utilisation of MMIs for managing PCOS. However, it is essential to acknowledge certain limitations that should be considered when interpreting the findings. All included studies were not critically appraised as this was a scoping review. The categorisation of MMIs proved challenging due to the complexity of interventions, which often comprised multifaceted practices, such as yoga therapy, unspecified meditation techniques, and instances where mindfulness overlapped with other forms of meditation. The present study did not aim to examine the efficacy of individual MMIs on specific PCOS features, as it was beyond the scope of the present study.
RecommendationsThis scoping review identified 14 studies investigating the breadth of MMIs for PCOS management. Several areas for future research have been identified to facilitate the translation of the findings presented in this review. These include (1): Future primary studies should explore the role of MMIs in promoting healthy lifestyle habits among adolescents (2); Future primary studies should examine the efficacy of MMIs on weight management and reproductive parameters in women diagnosed with PCOS (3); It is essential to establish clear definitions for the intervention, instructor and meditator, while also outlining proposed outcomes and implementing strategies to improve adherence rates; (4) Determination of therapeutic dosage levels of MMIs is needed to elicit clinically beneficial effects on PCOS features and describe the underlying mechanisms; (5) More rigorous methodologies for monitoring and documenting adverse events are required; (6) Further high-quality research, including attention-matched controls, is required to facilitate the integration of MMIs into clinical practice.
ConclusionsPCOS is a common chronic condition accompanied by significant psycho-social burdens throughout individuals’ lifespans. The rising popularity and accumulating evidence of supporting holistic approaches, such as meditation and mindfulness, have demonstrated their benefits in improving psychological well-being and QoL outcomes. MMIs may serve as a valuable complement to standard PCOS care; however, their efficacy requires further exploration through high-quality research.
Author contributionsVR: Conceptualization, Data curation, Formal Analysis, Investigation, Methodology, Project administration, Resources, Software, Validation, Writing – original draft, Writing – review & editing. AP: Methodology, Supervision, Validation, Writing – review & editing. AJ: Writing – review & editing, Data curation. AP: Data curation, Writing – review & editing, Formal Analysis. JG: Data curation, Writing – review & editing, Formal Analysis. EB: Writing – review & editing. NC: Writing – review & editing. PK: Funding acquisition, Investigation, Methodology, Supervision, Validation, Writing – review & editing.
FundingThe author(s) declare that no financial support was received for the research, authorship, and/or publication of this article. No funding was received for this paper.
Conflict of interestThe authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s noteAll claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary materialThe Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fendo.2024.1295705/full#supplementary-material
AbbreviationsPCOS, Polycystic Ovarian Syndrome; RCT, randomized clinical trial; ↑ significant increase (P ≤ 0.05), ↓ significant decrease (P ≤ 0.05), ↔ no significant change; mFG, modified Ferriman-Gallwey; FI, Fasting insulin; FBG, Fasting blood glucose; HOMA-IR, Homeostatic Model Assessment for Insulin Resistance; TC, Total Cholesterol; TG, Triglyceride; LDL, Low density lipoprotein; VLDL, Very-low-density lipoprotein; HDL, high-density lipoprotein; PCOSQ: BMI, Body mass index; WC, Waist circumference; WHR, Waist-hip ratio; MBSR, Mindfulness Based Stress Reduction; PSS, Perceived Stress Scale; DASS, The depression, anxiety and stress scale; TMS, Toronto Mindfulness Scale; HbA1C, Glycated haemoglobin; SBP, Systolic blood pressure; DBP, Diastolic blood pressure; SHBG, sex hormone binding globulin; SD, Standard deviation; BAI, Beck Anxiety inventory; BDI, Beck depression inventory; FFMQ, Five-Facet Mindfulness Questionnaire; SF-36, Short Form Survey; PROMIS, Patient-Reported Outcomes Measurement Information System; FCI, Food craving inventory; NIH, National Institutes of Health definition; BSI, Brief Symptom Inventory-18; PANAS, Positive and Negative Affect Schedule; CAMM, 10-item Child and Adolescent Mindfulness Measure; DIET-SE, 11-item Diet Self-Efficacy Scale; PACE, Patient-Cantered Assessment and Counselling for Exercise Plus Nutrition; HADS, Hospital Anxiety and Depression Scale; STAI (The state-trait anxiety inventory).
References1. Teede HJ, Tay CT, Laven JJE, Dokras A, Moran LJ, Piltonen TT, et al. Recommendations from the 2023 international evidence-based guideline for the assessment and management of polycystic ovary syndrom Eur J Endocrinology. (2023) 189:G43–64. doi: 10.1093/ejendo/lvad096
CrossRef Full Text | Google Scholar
2. Teede H, Deeks A, Moran L. Polycystic ovary syndrome: a complex condition with psychological, reproductive and metabolic manifestations that impacts on health across the lifespan. BMC Med. (2010) 8:41. doi: 10.1186/1741-7015-8-41
PubMed Abstract | CrossRef Full Text | Google Scholar
3. Gibson-Helm M, Teede H, Dunaif A, AJTJoCE D. Metabolism. Delayed diagnosis and a lack of information associated with dissatisfaction in women with polycystic ovary syndrome. J Clin Endocrinol Metab. (2017) 102(2):604–12. doi: 10.1210/jc.2016-2963
PubMed Abstract | CrossRef Full Text | Google Scholar
4. Rao VS, Cowan S, Armour M, Smith CA, Cheema BS, Moran L, et al. A global survey of Ethnic Indian women living with polycystic ovary syndrome: Co-morbidities, concerns, diagnosis experiences, quality of life, and use of treatment methods. Int J Environ Res Public Health. (2022) 19:15850. doi: 10.3390/ijerph192315850
PubMed Abstract | CrossRef Full Text | Google Scholar
5. Peña AS, Teede H, Hewawasam E, Hull ML, Gibson-Helm M. Diagnosis experiences of adolescents with polycystic ovary syndrome: Cross-sectional study. Clin endocrinology. (2022) 96:62–9. doi: 10.1111/cen.14604
CrossRef Full Text | Google Scholar
6. Elghobashy M, Lau GM, Davitadze M, Gillett CDT, O’Reilly MW, Arlt W, et al. Concerns and expectations in women with polycystic ovary syndrome vary across age and ethnicity: findings from PCOS Pearls Study. Front Endocrinol (Lausanne). (2023) 14:1175548. doi: 10.3389/fendo.2023.1175548
PubMed Abstract | CrossRef Full Text | Google Scholar
7. Ee C, Smith C, Moran L, MacMillan F, Costello M, Baylock B, et al. “The whole package deal”: experiences of overweight/obese women living with polycystic ovary syndrome. BMC women’s Health. (2020) 20:1–9. doi: 10.1186/s12905-020-01090-7
PubMed Abstract | CrossRef Full Text | Google Scholar
8. Pirotta S, Joham AE, Moran LJ, Skouteris H, Lim SS. Implementation of the polycystic ovary syndrome guidelines: A mixed method study to inform the design and delivery of a lifestyle management program for women with polycystic ovary syndrome. Nutr Dietetics. (2021) 78:476–86. doi: 10.1111/1747-0080.12670
CrossRef Full Text | Google Scholar
9. Tay CT, Pirotta S, Teede HJ, Moran LJ, Robinson T, Skouteris H, et al. (2021). Polycystic ovary syndrome models of care: a review and qualitative evaluation of a guideline-recommended integrated care, in: Seminars in Reproductive Medicine, 333 Seventh Avenue, 18th Floor, NY, USA: Thieme Medical Publishers, Inc.
10. Sheikh J, Khalil H, Shaikh S, Hebbar M, Zia N, Wicks S, et al. Emotional and psychosexual well-being is influenced by ethnicity and birthplace in women and individuals with polycystic ovary syndrome in the UK and India. BJOG: Int J Obstetrics Gynaecology. (2023) 130:978–86. doi: 10.1111/1471-0528.17428
CrossRef Full Text | Google Scholar
11. Verma A, Upadhyay V, Saxena V. Effect of yoga therapy on health outcomes in women with polycystic ovary syndrome: A systematic review and meta-analysis. Am J lifestyle Med. (2023) 17:73–92. doi: 10.1177/15598276211029221
PubMed Abstract | CrossRef Full Text | Google Scholar
12. Rao VS, Armour M, Cheema BS, Smith CA, Moran L, Perera RS, et al. Use of traditional and complementary medicine by ethnic Indian women living with polycystic ovary syndrome: a global survey BMC Complementary Med Therapies. (2023) 23:392. doi: 10.1186/s12906-023-04229-9
CrossRef Full Text | Google Scholar
13. Arentz S, Smith CA, Abbott JA, Bensoussan A. A survey of the use of complementary medicine by a self-selected community group of Australian women with polycystic ovary syndrome BMC complementary and alternative. Medicine. (2014) 14:472. doi: 10.1186/1472-6882-14-472
CrossRef Full Text | Google Scholar
15. Cardoso R, de Souza E, Camano L, Roberto Leite J. Meditation in health: an operational definition. Brain Res Protoc. (2004) 14:58–60. doi: 10.1016/j.brainresprot.2004.09.002
CrossRef Full Text | Google Scholar
17. Lutz A, Dunne JD, Davidson RJ. Meditation and the neuroscience of consciousness. In: Cambridge handbook of consciousness. Zelazo P.D., Moscovitch M., Thompson E. (Cambridge: Cambridge University Press), (2007). p. 499–555.
19. Travis F, Shear J. Focused attention, open monitoring and automatic self-transcending: Categories to organize meditations from Vedic, Buddhist and Chinese traditions. Consciousness Cognition. (2010) 19:1110–8. doi: 10.1016/j.concog.2010.01.007
CrossRef Full Text | Google Scholar
20. Kabat-Zinn J. Mindfulness-based interventions in context: past, present, and future. Clinical Psychology: Science and Practice (2003) 10(2):144–56. doi: 10.1093/clipsy/bpg016
CrossRef Full Text | Google Scholar
21. Baer RA Mindfulness training as a clinical intervention: A conceptual and empirical review Clin psychology: Sci practice (2003) 10:125. doi: 10.1093/clipsy/bpg015
CrossRef Full Text | Google Scholar
22. Garland EL, Hanley AW, Riquino MR, Reese SE, Baker AK, Salas K, et al. Mindfulness-oriented recovery enhancement reduces opioid misuse risk via analgesic and positive psychological mechanisms: A randomized controlled trial. J Consulting Clin Psychol. (2019) 87:927. doi: 10.1037/ccp0000390
CrossRef Full Text | Google Scholar
23. Garland EL, Baker AK, Riquino MR, Priddy SE. Mindfulness-oriented recovery enhancement. Handb mindfulness-based program mindfulness. Interv Educ to heal Ther Abingdon. (2019) 13:327–40.
25. White ND. Mindfulness-based cognitive therapy for depression, current episodes, and prevention of relapse. Am J Lifestyle Med. (2015) 9:227–9. doi: 10.1177/1559827615569677
CrossRef Full Text | Google Scholar
26. Van Dam NT, Van Vugt MK, Vago DR, Schmalzl L, Saron CD, Olendzki A, et al. Mind the hype: A critical evaluation and prescriptive agenda for research on mindfulness and meditation. Perspect psychol science. (2018) 13:36–61. doi: 10.1177/1745691617709589
CrossRef Full Text | Google Scholar
27. Orme-Johnson D. Medical care utilization and the transcendental meditation program Psychosomatic Med. (1987) 49(5):493–50. doi: 10.1097/00006842-198709000-00006
CrossRef Full Text | Google Scholar
29. Schlechta Portella CF, Ghelman R, Abdala V, Schveitzer MC, Afonso RF. Meditation: evidence map of systematic reviews. Front Public Health. (2021) 9:1777. doi: 10.3389/fpubh.2021.742715
CrossRef Full Text | Google Scholar
30. Bursky M, Kosuri M, Walsh Carson K, Babad S, Iskhakova A, Nikulina V. The utility of meditation and mindfulness-based interventions in the time of COVID-19: A theoretical proposition and systematic review of the relevant prison, quarantine and lockdown literature. psychol Rep. (2023) 126:557–600. doi: 10.1177/00332941211048734
PubMed Abstract | CrossRef Full Text | Google Scholar
31. Phimphasone-Brady P, Palmer B, Vela A, Johnson RL, Harnke B, Hoffecker L, et al. Psychosocial interventions for women with polycystic ovary syndrome: a systematic review of randomized controlled trials. F&S Rev. (2022) 3:42–56. doi: 10.1016/j.xfnr.2021.11.004
CrossRef Full Text | Google Scholar
32. Reuters T. Thomson reuters Int J Court Admin. (2014) 6(2).
34. Nidhi R, Padmalatha V, Nagarathna R, Amritanshu R. Effects of a holistic yoga program on endocrine parameters in adolescents with polycystic ovarian syndrome: A randomized controlled trial. J Altern Complementary Med. (2012) 19:153–60. doi: 10.1089/acm.2011.0868
CrossRef Full Text | Google Scholar
35. Nidhi R, Padmalatha V, Nagarathna R, Amritanshu R. Effect of yoga program on quality of life in adolescent polycystic ovarian syndrome: A randomized control trial. Appl Res Qual Life. (2013) 8:373–83. doi: 10.1007/s11482-012-9191-9
CrossRef Full Text | Google Scholar
36. Nidhi R, Padmalatha V, Nagarathna R, Amritanshu R. Effect of holistic yoga program on anxiety symptoms in adolescent girls with polycystic ovarian syndrome: A randomized control trial. Int J yoga. (2012) 5:112–7. doi: 10.4103/0973-6131.98223
PubMed Abstract | CrossRef Full Text | Google Scholar
37. Nidhi R, Padmalatha V, Nagarathna R, Ram A. Effect of a yoga program on glucose metabolism and blood lipid levels in adolescent girls with polycystic ovary syndrome. Int J gynaecology obstetrics: Off Organ Int Fed Gynaecology Obstetrics. (2012) 118:37–41. doi: 10.1016/j.ijgo.2012.01.027
CrossRef Full Text | Google Scholar
38. Stefanaki C, Bacopoulou F, Livadas S, Kandaraki A, Karachalios A, Chrousos GP, et al. Impact of a mindfulness stress management program on stress, anxiety, depression and quality of life in women with polycystic ovary syndrome: a randomized controlled trial. Stress (Amsterdam Netherlands). (2015) 18:57–66. doi: 10.3109/10253890.2014.974030
PubMed Abstract | CrossRef Full Text | Google Scholar
39. Vibhuti Rao B, Kashinath Metri B, Shubhashankari Rao B, Nagaratna R. Improvement in biochemical and psychopathologies in women having PCOS through yoga combined with herbal detoxification. J Stem Cells. (2018) 13:213–22.
40. Patel V, Menezes H, Menezes C, Bouwer S, Bostick-Smith CA, Speelman DL. Regular mindful yoga practice as a method to improve androgen levels in women with polycystic ovary syndrome: A randomized, controlled trial. J Am Osteopathic Assoc. (2020) 120(5):323–35. doi: 10.7556/jaoa.2020.050
CrossRef Full Text | Google Scholar
41. Yin MXC, Du LB, Zou XN, Fung YL, Sun YY, Chan CHY, et al. Can psychosocial intervention suppress testosterone and triglycerides among women with polycystic ovary syndrome? A feasibility trial. Front Psychol. (2021) 12
留言 (0)