The International Working Group on the Diabetic Foot (IWGDF) Guidelines define a diabetes-related foot ulcer (DFU) as a foot ulcer in a person with current or previously diagnosed diabetes mellitus, and usually accompanied by peripheral neuropathy and/or peripheral artery disease in the lower extremity (1). DFU is associated with reduced quality of life, increased hospitalization and mortality (2–6), and subsequently, costs to the health care service are high. In fact, surveys in Sweden, where health care cost levels and demographics are comparable to Norway, estimated the total cost of one non-amputation DFU to nearly USD 25,000, rising to more than USD 40,000 in the case of amputation (7). In line with these results a more recent systematic review covering five other European countries has revealed substantial costs associated with the diabetic foot and its complications (8).
The reported prevalence of DFU among people with diabetes in developed countries has varied widely from 16.6% in Belgium, to 1.5% in Australia (4). Zhang and colleagues examined the global disability burden for diabetes-related lower-extremity complications and estimated that, in 2016, 131 million people had diabetes-related lower-extremity complications (1.8% of the population) (9). Given the elevated risks of infection, hospitalization, and amputation, the prevention of DFU and recurrent ulcer is one of the most important challenges in the current approach to diabetic foot disease (10), and updated international standards are striving to improve DFU prevention and care. However, there is limited knowledge with high-quality population-based studies on change in the point prevalence, and/or change in lifetime prevalence (defined as “the proportion of people who have had the disease in question at any point in their life (up to the time of assessment)”) of DFU (2). Although relevant micro- and macrovascular complication rates have declined substantially in high-income countries over the past 30 years (11, 12), it is not known whether this is also the case for DFU. Cardiovascular risk reduction is a major part of diabetes care, and it is likely that peripheral arterial disease and microvascular sclerosis associated with DFU reflects established arterial disease elsewhere in the body (13). A possible decrease in CVD risk factors could impact DFU prevalence.
The Trøndelag Health Study (HUNT) (https://www.ntnu.edu/hunt) is an ongoing population-based study in a large region in Norway. Our primary aim was to examine the trend in lifetime DFU prevalence using data from HUNT2 (1995–1997), HUNT3 (2006-2008), and HUNT4 (2017-2019). Secondly, we aimed to examine the trends in lifetime prevalence of other micro- and macrovascular complications among those with and without a DFU.
Materials and methodsThe Trøndelag health studyHUNT is an ongoing longitudinal study which includes several comprehensive cross-sectional health surveys conducted at 10-year intervals between 1984 and 2019. All inhabitants ≥20 years old in the Trøndelag region were invited to participate (14). All HUNT studies include extensive questionnaire data, clinical measurements, and samples, collected by specially trained health personnel. Non-fasting blood samples were collected and handled according to appropriate standards. More details on data collection may be found in previous publications (14), and all questionnaires may be found at https://www.ntnu.edu/hunt/data/que.
Study populationIn the current study, we used data from HUNT2, HUNT3, and HUNT4, conducted in 1995-1997, 2006-2008, and 2017-2019. A total of 65,228 (69.5% of those invited) participated in HUNT2, 50,800 (54.1% of those invited) participated in HUNT3, and 56,044 (54.0% of those invited) participated in HUNT4. In addition to completing the main questionnaire, those who reported having diabetes (HUNT2 = 2,028, HUNT3 = 2,264, and HUNT4 = 3,334) received an additional diabetes-specific questionnaire. In HUNT2, HUNT3, and HUNT4, 1,630 (80.4%), 1,824 (80.5%), and 2,393 (71.8%) participants completed the diabetes-specific questionnaire, respectively, and were included in the study population in the current analyses. Supplementary Figure 1 presents the number of individuals who participated in 1) all three health surveys (HUNT2-HUNT4), 2) both HUNT2 and HUNT3, and 3) both HUNT3 and HUNT4.
Data materialType of diabetesType of diabetes (type 1 or type 2 diabetes) was defined using glutamic acid decarboxylase antibodies (GADA) and age at diabetes diagnosis. In HUNT2 and HUNT3, the unit of measure for GADA was antibody index (ai), while HUNT4 used international units per millimeter (IU/mL) (15). GADA was measured in serum samples and analyzed by immunoprecipitation radioligand assay using translation labelled 3H-GAD65 as a labelled reagent. Type 2 diabetes was defined as GADA <5 IU/mL (<0.08 ai) and age at diagnosis ≥30 years. Type 1 diabetes was defined as GADA ≥5 IU/mL (≥0.08 ai) and/or age at diagnosis <30 years. If data on GADA and/or age at diagnosis were missing, we collected this information from a previous HUNT survey, if available. If the participants only had information on either GADA or age at diagnosis, we used the available information to classify them according to type of diabetes. Information was missing for a total of 20 participants on both GADA and age at diagnosis: 13 participants in HUNT2, 2 in HUNT3, and 5 in HUNT4. These participants were excluded from statistical analyses stratified by type of diabetes. An overview of the percentage of missing data may be found in Supplementary Table 1.
Sociodemographic and health-related variablesSelf-reported information on sociodemographic and health-related variables was obtained from the main questionnaires, including the following sociodemographic variables: age at participation, education level (highest achieved education (education <10 years, yes/no)), living alone (yes/no), and occupational status (currently employed, yes/no). The highest attained education level from HUNT2 and HUNT4 was used to classify education level in HUNT3 as this information was missing (not included in the questionnaire).
Information on the following health-related variables was also retrieved: body mass index (BMI), current daily smoking (yes/no), blood pressure (mmHg), use of antihypertensive drugs (yes/no), and physical activity (<1 hour a week). Height and weight were measured by trained personnel and BMI (weight in kilograms divided by the squared value of height in meters) was calculated. Self-reported physical activity was assessed by average hours of light or hard physical activity during one week in the last year (HUNT2), and also, how often they exercised (HUNT3 and HUNT4). By using these data, we categorized physical activity as <1 hour a week and ≥1 hour a week. Blood pressure was measured, by trained personnel, in a sitting position after two minutes of rest. Three measurements were taken, one minute apart, of which the mean value of the second and third measurement was used. Lastly, we retrieved information on the use of insulin and other diabetes medications (yes/no), and on duration of diabetes using (years), year of diagnosis and year of participation.
Primary outcomeWe define lifetime prevalence of DFU as the proportion who have had the disease in question at any point in their life up to the point of the assessment (16), and used the following question from the diabetes-specific questionnaire to assess the self-reported lifetime prevalence: “Did you ever have a foot ulcer that did not heal in three weeks?” (HUNT2 and HUNT3), and “Did you ever have a foot ulcer on a toe, foot or ankle that did not heal in three weeks?” (HUNT4) (16). Lifetime prevalence is distinct from what is referred to as lifetime morbid risk, which is the proportion of people who will eventually develop the disease at some time in their entire life span (17).
Secondary outcomesDiabetes eye problems were self-reported by asking “Do you have problems with your vision that your doctor has said are related to your diabetes?” (HUNT2-3), and “Has an ophthalmologist found diabetic changes on the retina/fundus” (HUNT4). Chronic kidney disease was defined as estimated glomerular filtration rate (eGFR) <60 mL/min/1.73 m2 (eGFR categories G3-G5), while kidney failure was defined as eGFR <30 mL/min/1.73 m2 (eGFR categories G4-G5) (18). eGFR was estimated using the Chronic Kidney Disease Epidemiology Consortium (CKD-EPI) formula (19).
Statistical analysesSociodemographic status and health characteristic of the study population were described using frequencies and percentages for categorical variables and means and standard deviations (SD) for continuous variables.
The lifetime prevalence of DFU and other complications of diabetes were evaluated using cross-sectional data from all three HUNT surveys and calculated as the proportion of the population with diabetes who, at some point in their life (up until the time of assessment), had ever had a foot ulcer that required more than three weeks to heal. Lifetime prevalence in each survey was calculated for the total sample, by age group (20-49, 50-74, and ≥75 years), sex, and diabetes type with 95% confidence intervals. The lifetime prevalence of other micro- and macrovascular complications was defined as the proportion of the diabetes population who, at some point in life, had (or have) any of the following diseases: diabetes eye problems, stroke, MI, and/or angina pectoris. The prevalence of eGFR was assessed as prevalence at time of participation (point prevalence). Trends in the lifetime prevalence of other micro- and macrovascular complications of diabetes are presented with stratification according to diabetes type and presence of DFU.
Prevalence ratios for HUNT3 vs. HUNT2 and HUNT4 vs. HUNT2 were calculated using modified Poisson regression because of convergence problems with log-binomial regression (20). A binary variable for DFU was used as the dependent variable and a three-category variable for HUNT survey was used as independent variable with HUNT2 as the reference category. Prevalence ratios were obtained by exponentiating the regression coefficients. Clustered robust standard error was used to account for repeated participation. All estimates of the prevalence ratios are presented as 1) unadjusted (Model 1), 2) adjusted for age and sex (Model 2), and 3) adjusted for age, sex, education level, living situation, BMI, systolic blood pressure, smoking, use of insulin, eGFR, and HbA1c (Model 3). Variables in model 3 are known risk factors for DFU and other micro- and macrovascular complications and are considered mediators for the association between year of survey and risk of DFU and complications (2). Multiple imputation by chained equations (MICE) was used to impute missing data (21). Less than 5% was missing for the majority of the variables. In HUNT3, all participants with diabetes were invited to a follow-up study, HbA1c was only measured among those with diabetes who also participated in this follow-up after HUNT3, yielding missing HbA1c values for 40.2% of the participants. Persons with missing HbA1c were significantly older than persons with valid HbA1c-measurements, and missing HbA1c was more frequent among women, those living alone and among smokers, indicating some selection in participation. Given that information on age, gender, living situation and smoking was included in imputation models and adjusted for in regression models we consider missing data to be missing at random (MAR) for all variables, including HbA1c. We imputed missing values for the following variables: DFU, education level, living situation, work situation, BMI, systolic blood pressure, total cholesterol, smoking, use of insulin, eGFR, previous MI, previous angina pectoris and HbA1c. Logistic regression was used as the imputation model for binary variables, and linear regression was used for continuous variables. Age and sex were included as auxiliary variables in the imputation equations in addition to the above- mentioned variables. For each missing value, we obtained 50 imputed values. Convergence of the imputation models were evaluated by visual inspection of trace plots of average of imputed values versus number of imputations (Supplementary Figure 2). Plausibility of imputed values for HbA1c was evaluated by distribution plots for each imputed dataset (Supplementary Figure 3). Imputed HbA1c values had a plausible range with a slightly higher mean compared to observed values, compatible with a MAR-mechanism where persons with missing values get a higher imputed value because of higher age, higher occurrence of living alone and more current smoking. The level of significance was defined as <0.05 in all analyses.
Analyses were performed using Stata software (StataCorp, 2019, Stata Statistical Software: Release 16, College Station, TX: StataCorp LLC).
EthicsThis study was approved by the Regional Committees for Medical Research and Health Research Ethics in Norway (74975) and the Norwegian Centre for Research Data (150393). All participants gave written informed consent.
ResultsPopulation characteristicsSociodemographic status and health characteristics of the total diabetes population in HUNT2, HUNT3, and HUNT4 are shown in Table 1. Approximately 85% of the study population was classified as having type 2 diabetes. Age at participation was stable across the three health surveys (66.2, 64.7, and 65.6 years, respectively). Comparing the participants in HUNT4 with those in HUNT2 showed an increase in participants with a higher education level and fewer people reported to be currently smoking. There was a notable decrease in people with systolic blood pressure >140 mmHg, and, at the same time, an increase in the use of antihypertensive drugs from 41.8% to 71.0%. HbA1c decreased from HUNT2 to HUNT4, while there was an increase in participants with BMI >30 (Table 1).
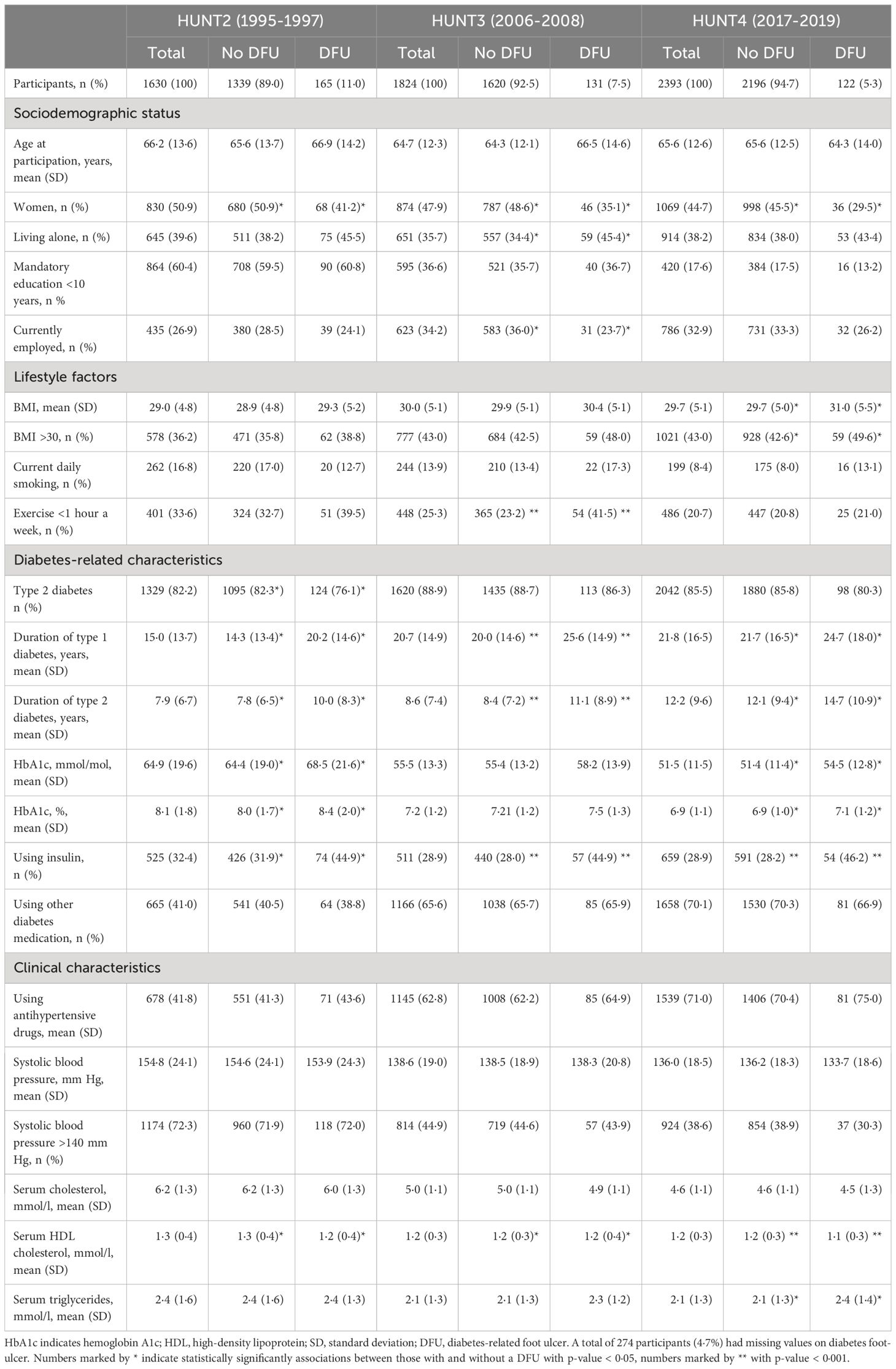
Table 1 Sociodemographic status and health characteristics among participants with diabetes in HUN2-HUNT4, stratified by diabetes foot ulcer (DFU).
We found that the characteristics of the foot ulcer population in HUNT changed during the study period (Table 1). Compared to those without a DFU, the proportion of people with BMI >30 increased more among those with a DFU. Furthermore, in those with a DFU, the percentage of people currently smoking remained stable during the study period. In contrast, the percentage of current smokers was more than halved in those without a DFU. The decrease in HbA1c from HUNT2 to HUNT4 did not differ in those with and without a DFU.
Trends in the lifetime prevalence of diabetes-related foot ulcersIn the total diabetes population, the lifetime prevalence of a DFU requiring three or more weeks to heal was respectively 11.0% (95% CI: 9.-12.) in HUNT2, 7.5% (95% CI: 6.3-8.8) in HUNT3, and 5.26% (95% CI: 4.4-6.3) in HUNT4 (Figure 1, Table 2). A total of 165, 131, and 122 participants reported to ever have had a DFU, respectively. The decreasing lifetime prevalence of a DFU was statistically significant at all three measurement points (HUNT2 vs HUNT3, HUNT2 vs HUNT4, and HUNT3 vs. HUNT4). The clear trend of a decreasing lifetime prevalence of DFU from HUNT2 to HUNT4 was observed in both men and women, although men (12.8%, 9.3%, and 6.7%) in general had a higher lifetime prevalence of DFU than women (9.1%, 5.5%, and 3.5%) (p < 0.001). The lifetime prevalence of a DFU decreased in all age groups, with the largest decrease among the oldest (≥75 years). Overall, the lifetime prevalence of a DFU was 30% lower in HUNT3 compared to HUNT2, and 50% lower in HUNT4 compared to HUNT2 (Table 2). After adjusting for age, sex, education level, living situation, BMI, systolic blood pressure, smoking, use of insulin, eGFR, and HbA1c using multiple imputation to account for missing values, the estimates did not differ markedly. Results were also similar in complete case analyses (Supplementary Table 2).
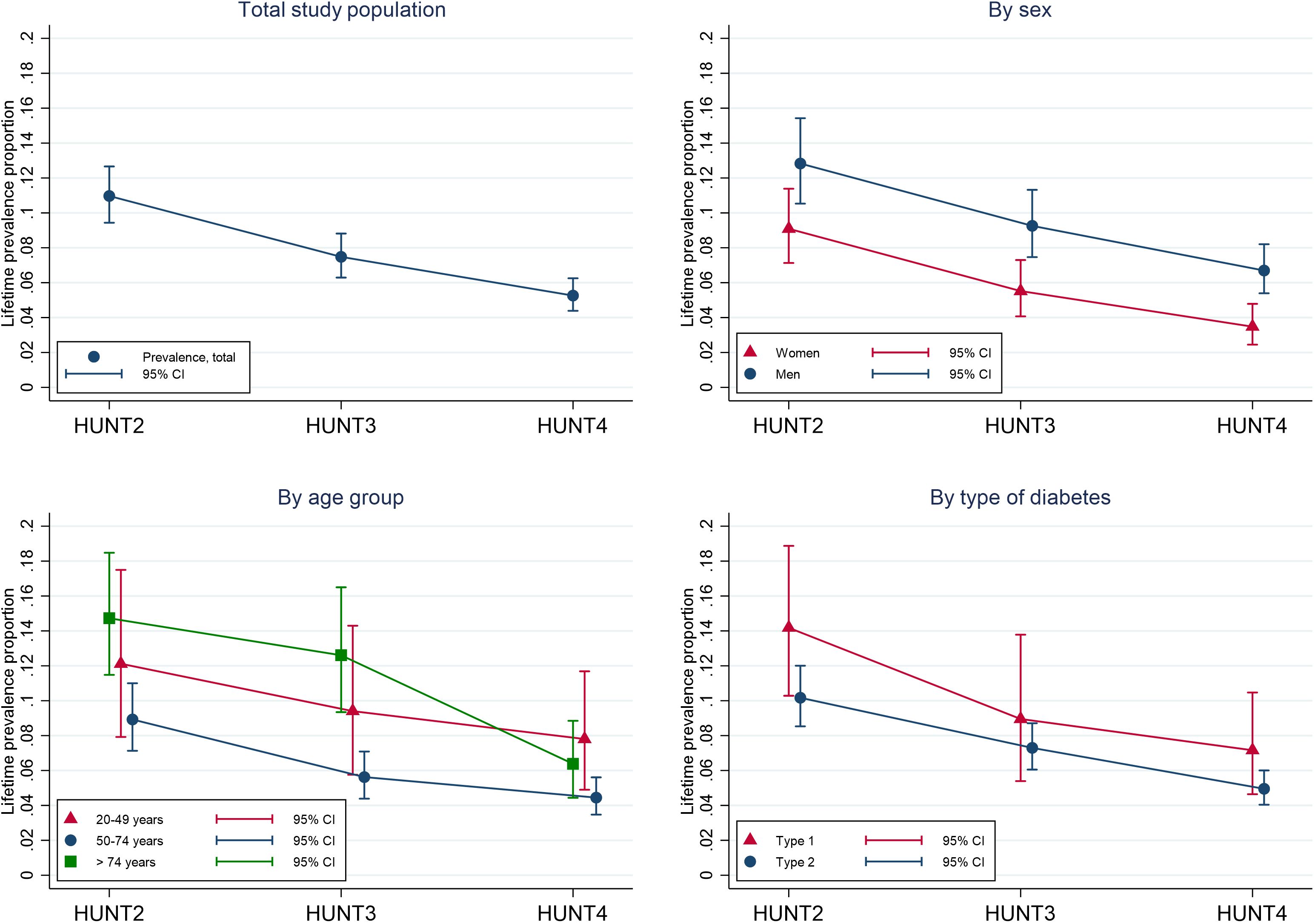
Figure 1 Trends in lifetime prevalence of diabetes-related foot ulcers among participants in HUNT2 (1995-1997), HUNT3 (2006-2008) and HUNT4(2017-2019), in total, and stratified by age, sex and type of diabetes. CI indicates confidence interval.
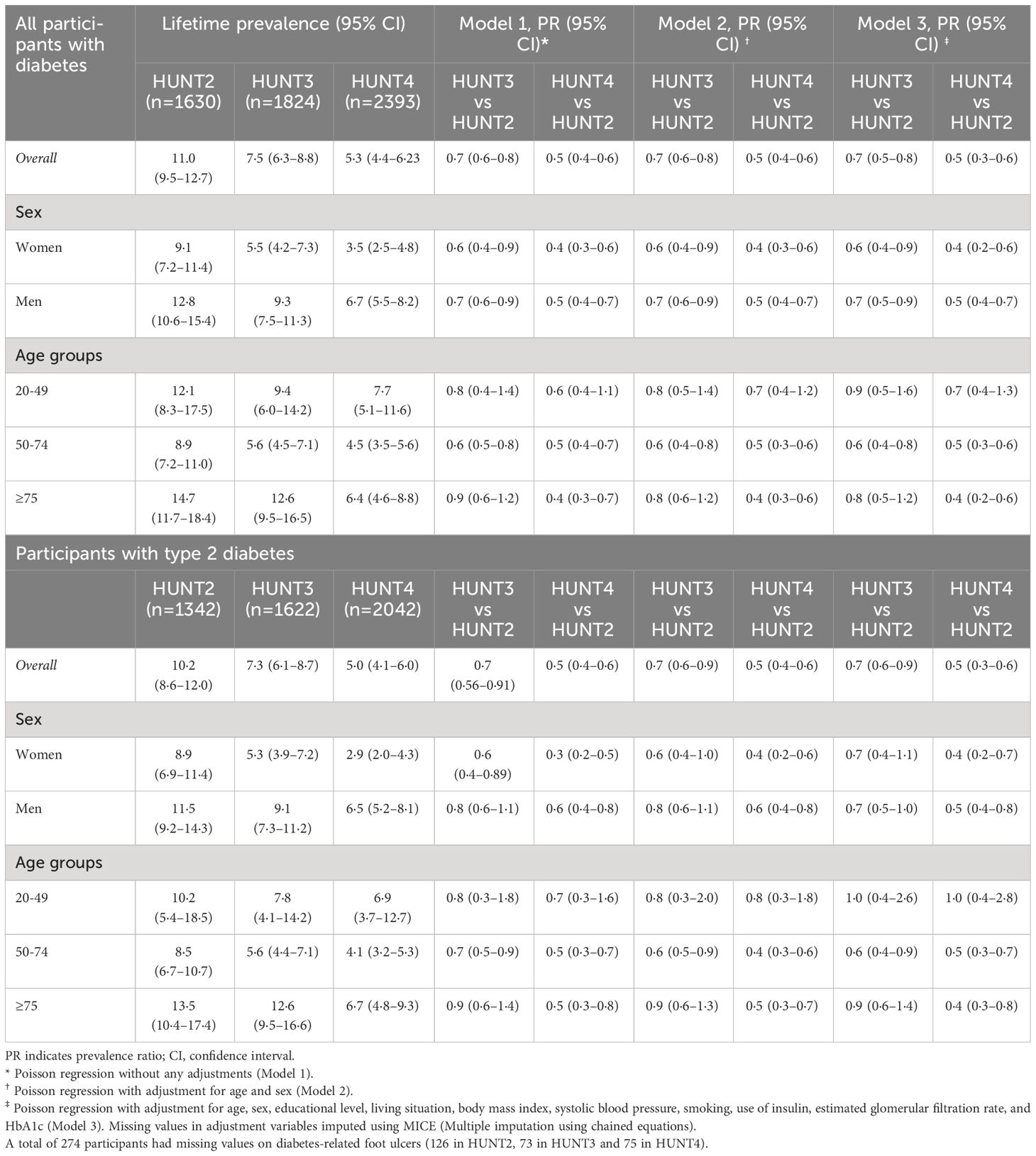
Table 2 Lifetime prevalence (%) and prevalence ratio (PR) of a diabetes-related foot ulcer according to diabetes type in HUNT2-HUNT4, stratified by sex and age.
In individuals with type 2 diabetes, the lifetime prevalence of a DFU was 10.2% (95% CI: 8.7-12.0) in HUNT2, 7.3% (95% CI: 6.2-8.8) in HUNT3, and 5.0.% (95% CI: 4.1-6.0) in HUNT4 (Table 2). The trends in DFU lifetime prevalence among men and women and the different age groups were similar to those in the total diabetes population. The prevalence ratio of a DFU was 50% lower in HUNT4 compared to HUNT2: 60% lower in women and 50% lower in men (Table 2). Adjustment for known risk factors had minimal impact on the results. The lifetime prevalence of a DFU in those with type 1 diabetes was 14.2% (95% CI: 10.5-18.8), 9.0% (95% CI: 5.6-13.8), and 7.2% (95% CI: 4.8-10.5), respectively (Figure 1 (numbers not shown in table)).
Trends in the lifetime prevalence of other micro- and macrovascular diabetes complicationsThe changes in lifetime prevalence of micro- and macrovascular diabetes complications from HUNT2 to HUNT4 stratified by diabetes-related foot ulcer are reported in Table 3 and Supplementary Table 3. These complications were found to significantly relate to DFU. Those with a DFU reported more diabetes eye problems, kidney disease, stroke, MI, and angina pectoris than those without a DFU. In HUNT4, more than twice as many participants with a DFU reported having diabetes eye problems compared to those without a DFU. The same was seen for stroke. There was no significant trend in changes in micro- or macrovascular diabetes complications among individuals with a DFU from HUNT2 to HUNT4.
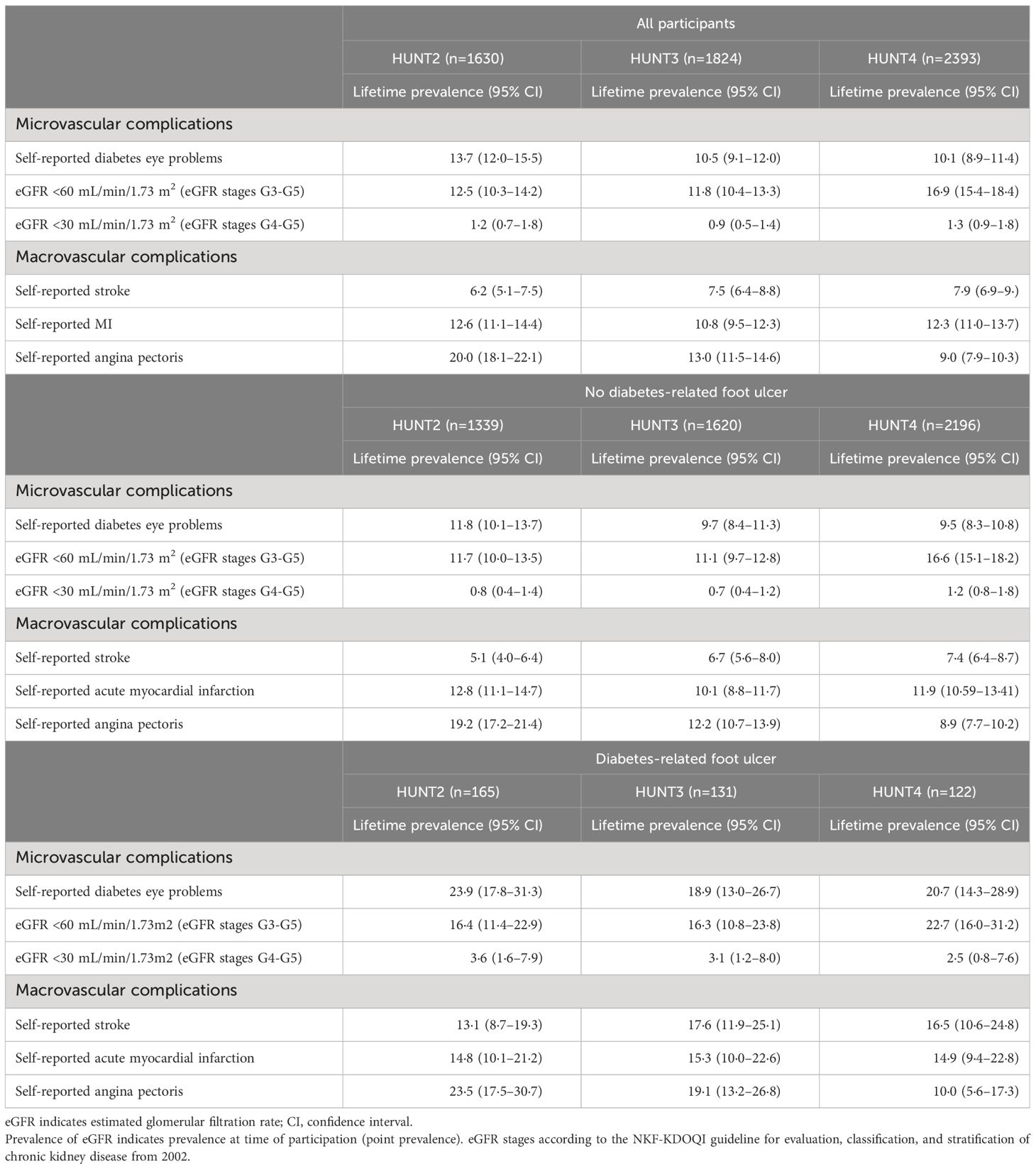
Table 3 Trends in lifetime prevalence (%) of other micro- and macrovascular diabetes complications in participants in HUNT2-HUNT4, stratified by diabetes-related foot ulcer.
In the total diabetes population, the lifetime prevalence of self-reported eye problems was numerically lower in HUNT2 compared to HUNT4 (13.7% to 10.1%). The prevalence of eGFR <60 mL/min/1.73 m2, indicating chronic kidney disease (eGFR stages G3-G5), increased during the same period ((from 12.5% to 16.9%) Table 3). Participants in HUNT4 had an almost 40% increased prevalence (PR 1.4 (95% CI 1.1-1.7)) of chronic kidney disease compared to participants in HUNT2 (Supplementary Table 4).
Small changes were observed in the lifetime prevalence of MI and stroke from HUNT2 to HUNT4. The lifetime prevalence of angina pectoris changed substantially (from 20.0% to 9.0%), corresponding to a risk reduction of 30% (PR 0.7; 95% CI 0.6-0.8) and 50% (PR 0.5; 95% CI 0.4-0.6) from HUNT2 to HUNT3, and from HUNT2 to HUNT4, respectively. There was an increased lifetime prevalence of stroke in HUNT4 compared to HUNT2 (PR 1.2; 95% CI 0.9-1.6), while the lifetime prevalence of MI remained unchanged (Table 3; Supplementary Table 4). The same associations were found among those with type 2 diabetes.
DiscussionIn this population-based study from Norway, there was a more than 50% decrease in lifetime prevalence of DFU from 1995 to 2019. The decrease was observed for both men and women, and for all age groups. Decreasing trends in type 1 and type 2 diabetes were similar, but the highest lifetime prevalence of DFU was found among those with type 1 diabetes.
A review by McDermott and colleagues from 2022 (2) highlights the need for high-quality population-based studies of DFU incidence and prevalence. They also state that despite fluctuations in DFU incidence, the patterns of DFU prevalence have remained stable. To our knowledge, this is the first large population-based study with more than two points of measurement documenting a substantial decrease in the lifetime prevalence of DFU over 25 years. Our results align well with a Danish study assessing time trends in DFU incidence (22), which found that the DFU incidence in type 2 diabetes dropped from 8.1% in 2002 to 2.6% in 2014. The corresponding figures for those with type 2 diabetes were 17.0% and 8.7%, respectively. Another Danish study found decreasing incidence trends of distal symmetric polyneuropathy from 1996 to 2018 in both type 1 and type 2 diabetes (23). The results from these two Danish studies are, however, not directly comparable to ours as we report lifetime prevalence and not incidence.
The systematic review by Zhang et al. found higher DFU prevalence in patients with type 2 diabetes (6.4%) than patients with type 1 diabetes (5.5%) (4). This contrasts with the current study where the lifetime prevalence of DFU tended to be higher in type 1 diabetes. Foot ulceration is a major complication of both type 1 and type 2 diabetes, but the higher lifetime prevalence of DFU in type 1 diabetes observed in the current study may be related to the duration of diabetes, which is closely related to age. As expected, mean diabetes duration was higher among those with type 1 diabetes compared to those with type 2 (HUNT2 15.0 vs 7.9 years, HUNT3 20.7 vs 8.6 years, HUNT4 21.8 vs 12.2 years).
During the study period, we found significant improvements in DFU risk factors in the total diabetes population, such as better glycemic and metabolic control. After adjusting for these risk factors, we still observed small changes in DFU lifetime prevalence, indicating that the decrease in DFU prevalence in Norway may not only be explained by enhanced management of DFU risk factors. In line with our results, several recent studies have showed decreasing risk of diabetes risk factors. For instance, a recent publication from Denmark showed a reduction in incidence of neuropathy in both type 1 and type 2 diabetes (23), and a Norwegian study reported moderate improvements in overall control of risk factors such as HbA1c, blood pressure and total cholesterol (24). Nevertheless, advances in clinical and preventive care, as well as improvements in the performance of the health care system may possibly have contributed more to the decrease in DFU prevalence than changes in risk factors. Both national and international guidelines during the last 20 year have been more precise and explicit regarding prevention and treatment of DFU, such as the recommendations for an annual comprehensive foot examinations for all patients with diabetes (2). Furthermore, the increasing prevalence of diabetes (new and existing cases of disease) might also have influenced our results. It is therefore possible that the decrease in the lifetime prevalence of DFU in the current study reflects the larger diabetes population (denominator) with better glycemic and metabolic control.
We found that the prevalence trends of other micro- and macrovascular complications varied during the study period. There was a clear decrease for angina pectoris and an increase of reduced kidney function (eGFR stages G3-G5), which is in line with previous studies (25, 26). The overall mean years lived with diabetes has increased due to a combination of decreasing mortality and increasing diabetes prevalence, which could lead to a range of diabetes co-morbidities, including high rates of renal disease. Overall, those with a DFU in the current study reported a higher prevalence of diabetes eye problems, kidney disease, stroke, MI, and angina pectoris compared to participants without a DFU. This is in line with factors associated with the at-risk foot (27, 28), reflecting the severity of diabetes in the DFU population.
Diabetes-related lower-extremity complication, including DFU, have a significant impact on global disease burden and targeted strategies are needed to help diabetes management, as well a specific DFU strategies such as interdisciplinary foot care services (9). Although a decrease in DFU lifetime prevalence is found in the current study, awareness is needed as the increase in diabetes prevalence and improved survival in people with diabetes can turn the positive trend of decreasing DFU prevalence in Norway. Future research is expected to closely monitor these trends and identify strategies to maintain or further reduce the prevalence of DFUs. Further research may focus on the impact of new treatment approaches, the role of technology in monitoring and early detection of DFUs, and the effectiveness of initiatives intended to raise awareness and improve foot care among individuals with diabetes.
The present study has several strengths. First, these health surveys were large population-based studies. Secondly, we had access to a range of variables on somatic illness, medications, lifestyle, and health-related characteristics measured at three different time points over a period of 25 years. Thirdly, type 1 and type 2 diabetes were verified by GADA measurements (15), and we were consequently able to assess differences in DFU lifetime prevalence between these two types of patients.
However, as with all large-scale-epidemiological studies, this study also has inherent short comings. First, DFU was self-reported and not clinically verified as it was derived from population-based survey data. As such it was not feasible to clinically validate the diagnosis. Self-reported diabetes has shown high validity in HUNT with a specificity of 99.5% and a sensitivity of 81% (14). The specificity of all data related to self-reported cardiovascular disease used in the current study was found to be high (>99%). The sensitivity was lower; 34% for angina pectoris, 76% for acute myocardial infarction, and 59% for heart failure (14). Secondly, the participants in HUNT are recruited from Trøndelag county, a specific geographical area in Norway with few large cities. The population is relatively homogeneous with less than 3% non-Caucasians. Selection bias is a threat for voluntary health surveys in general. Studies examining the non-participants in HUNT [e.g., 15] have shown that they have lower socioeconomic status and have poorer health than the participants, which is in line with other epidemiological studies (29).
ConclusionDFU still constitute a substantial burden for people with diabetes. Data from the HUNT Study (1995-2019) allowed changes to be identified in the lifetime prevalence of DFU in people with type 1 and type 2 diabetes. We observed a promising decrease in the lifetime prevalence of DFU over a 25-year period. More studies are needed to investigate this trend in other populations, as well as to elicit the underlying reasons for the decline, with the aim of individualized care further improving outcomes for people with diabetes.
Data availability statementThe datasets presented in this article are not readily available because the data that support the findings of this study are available from HUNT, but restrictions apply to the availability of these data, which were used under license for the current study and therefore are not publicly available. Anonymous data are however available from the authors upon reasonable request and with permission from HUNT and the Regional Committees for Medical and Health Research Ethics in Norway. Requests to access the datasets should be directed to HR, hkrr@hvl.no.
Ethics statementThe studies involving humans were approved by Regional Committees for Medical Research and Health Research Ethics in Norway (74975) and the Norwegian Centre for Research Data (150393). The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributionsHR: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Resources, Software, Supervision, Visualization, Writing – original draft, Writing – review & editing. JI: Data curation, Formal analysis, Methodology, Software, Writing – review & editing. MG: Conceptualization, Funding acquisition, Writing – review & editing. AH: Conceptualization, Funding acquisition, Writing – review & editing. TØ: Writing – review & editing, Conceptualization, Funding acquisition. ES: Writing – review & editing, Conceptualization, Funding acquisition. MH: Conceptualization, Funding acquisition, Writing – review & editing. SC: Data curation, Writing – review & editing. BÅ: Conceptualization, Data curation, Funding acquisition, Writing – review & editing. MI: Conceptualization, Funding acquisition, Project administration, Writing – review & editing.
FundingThe author(s) declare financial support was received for the research, authorship, and/or publication of this article. The first author, HR, received a scholarship from Western Norway Regional Health Authority (Helse Vest, project number F-12131) for a 2.5-year postdoctoral position. HUNT is a collaboration between HUNT Research Centre (Faculty of Medicine and Health Sciences, NTNU -Norwegian University of Science and Technology), Trøndelag County Council, Central Norway Regional Health Authority and the Norwegian Institute of Public Health. The analyses of GADA were financed by the Swedish Research Council (Grant number 2018-02035).
Conflict of interestAH has received a lecture honorary from Novo Nordisk and Abbott.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The author(s) declared that they were an editorial board member of Frontiers, at the time of submission. This had no impact on the peer review process and the final decision.
Publisher’s noteAll claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary materialThe Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fendo.2024.1354385/full#supplementary-material
References1. van Netten JJ, Bus SA, Apelqvist J, Chen P, Chuter V, Fitridge R, et al. Definitions and criteria for diabetes-related foot disease (IWGDF 2023 update). Diabetes Metab Res Rev. (2023) 40(3):e3654. doi: 10.2337/dci22-0043
PubMed Abstract | CrossRef Full Text | Google Scholar
2. McDermott K, Fang M, Boulton AJM, Selvin E, Hicks CW. Etiology, epidemiology, and disparities in the burden of diabetic foot ulcers. Diabetes Care. (2023) 46:209–21. doi: 10.2337/dci22-0043
PubMed Abstract | CrossRef Full Text | Google Scholar
3. Iversen MM, Tell GS, Riise T, Hanestad BR, Ostbye T, Graue M, et al. History of foot ulcer increases mortality among individuals with diabetes: ten-year follow-up of the Nord-Trondelag Health Study, Norway. Diabetes Care. (2009) 32:2193–9. doi: 10.2337/dc09-0651
PubMed Abstract | CrossRef Full Text | Google Scholar
4. Zhang P, Lu J, Jing Y, Tang S, Zhu D, Bi Y. Global epidemiology of diabetic foot ulceration: a systematic review and meta-analysis (dagger). Ann Med. (2017) 49:106–16. doi: 10.1080/07853890.2016.1231932
PubMed Abstract | CrossRef Full Text | Google Scholar
5. Khunkaew S, Fernandez R, Sim J. Health-related quality of life among adults living with diabetic foot ulcers: a meta-analysis. Qual Life Res. (2019) 28:1413–27. doi: 10.1007/s11136-018-2082-2
PubMed Abstract | CrossRef Full Text | Google Scholar
6. Lazzarini PA, Cramb SM, Golledge J, Morton JI, Magliano DJ, Van Netten JJ. Global trends in the incidence of hospital admissions for diabetes-related foot disease and amputations: a review of national rates in the 21st century. Diabetologia. (2023) 66:267–87. doi: 10.1007/s00125-022-05845-9
PubMed Abstract | CrossRef Full Text | Google Scholar
7. Tennvall GR, Apelqvist J, Eneroth M. Costs of deep foot infections in patients with diabetes mellitus. Pharmacoeconomics. (2000) 18:225–38. doi: 10.2165/00019053-200018030-00003
PubMed Abstract | CrossRef Full Text | Google Scholar
8. Tchero H, Kangambega P, Lin L, Mukisi-Mukaza M, Brunet-Houdard S, Briatte C, et al. Cost of diabetic foot in France, Spain, Italy, Germany and United Kingdom: A systematic review. Ann Endocrinol (Paris). (2018) 79:67–74. doi: 10.1016/j.ando.2017.11.005
PubMed Abstract | CrossRef Full Text | Google Scholar
9. Zhang Y, Lazzarini PA, McPhail SM, van Netten JJ, Armstrong DG, Pacella RE. Global disability burdens of diabetes-related lower-extremity complications in 1990 and 2016. Diabetes Care. (2020) 43:964–74. doi: 10.2337/dc19-1614
PubMed Abstract | CrossRef Full Text | Google Scholar
11. Gregg EW, Li Y, Wang J, Burrows NR, Ali MK, Rolka D, et al. Changes in diabetes-related complications in the United States, 1990-2010. N Engl J Med. (2014) 370:1514–23. doi: 10.1056/NEJMoa1310799
PubMed Abstract | CrossRef Full Text | Google Scholar
12. Davis WA, Gregg EW, Davis TME. Temporal trends in cardiovascular complications in people with or without type 2 diabetes: The fremantle diabetes study. J Clin Endocrinol Metab. (2020) 105. doi: 10.1210/clinem/dgaa215
PubMed Abstract | CrossRef Full Text | Google Scholar
13. Chin BZ, Lee P, Sia CH, Hong CC. Diabetic foot ulcer is associated with cardiovascular-related mortality and morbidity - a systematic review and meta-analysis of 8062 patients. Endocrine. (2024). doi: 10.1007/s12020-024-03696-5
PubMed Abstract | CrossRef Full Text | Google Scholar
14. Åsvold BO, Langhammer A, Rehn TA, Kjelvik G, Grøntvedt TV, Sørgjerd EP, et al. Cohort profile update: the HUNT study, Norway. Int J Epidemiol. (2022) 52(1):e80-91. doi: 10.1093/ije/dyac095
CrossRef Full Text | Google Scholar
15. Sorgjerd EP, Skorpen F, Kvaloy K, Midthjell K, Grill V. Time dynamics of autoantibodies are coupled to phenotypes and add to the heterogeneity of autoimmune diabetes in adults: the HUNT study, Norway. Diabetologia. (2012) 55:1310–8. doi: 10.1007/s00125-012-2463-y
PubMed Abstract | CrossRef Full Text | Google Scholar
16. Bhopal RS. Concepts of Epidemiology : Integrating The Ideas, Theories, Principles, And Methods Of Epidemiology. 3rd ed. New York: Oxford University Press (2016). 441 p.
17. Kessler RC, Petukhova M, Sampson NA, Zaslavsky AM, Wittchen HU. Twelve-month and lifetime prevalence and lifetime morbid risk of anxiety and mood disorders in the United States. Int J Methods Psychiatr Res. (2012) 21:169–84. doi: 10.1002/mpr.1359
PubMed Abstract | CrossRef Full Text | Google Scholar
18. Inker LA, Astor BC, Fox CH, Isakova T, Lash JP, Peralta CA, et al. KDOQI US commentary on the 2012 KDIGO clinical practice guideline for the evaluation and management of CKD. Am J Kidney Dis. (2014) 63:713–35. doi: 10.1053/j.ajkd.2014.01.416
PubMed Abstract | CrossRef Full Text | Google Scholar
19. Levey AS, Stevens LA, Schmid CH, Zhang YL, Castro AF 3rd, Feldman HI, et al. A new equation to estimate glomerular filtration rate. Ann Intern Med. (2009) 150:604–12. doi: 10.7326/0003-4819-150-9-200905050-00006
PubMed Abstract | CrossRef Full Text | Google Scholar
22. Rasmussen A, Almdal T, Anker Nielsen A, Nielsen KE, Jorgensen ME, Hangaard S, et al. Decreasing incidence of foot ulcer among patients with type 1 and type 2 diabetes in the period 2001-2014. Diabetes Res Clin Pract. (2017) 130:221–8. doi: 10.1016/j.diabres.2017.05.025
PubMed Abstract | CrossRef Full Text | Google Scholar
23. Mizrak HI, Hansen TW, Rossing P, Curovic VR, Vistisen D, Amadid H, et al. Declining incidence rates of distal symmetric polyneuropathy in people with type 1 and type 2 diabetes in Denmark, with indications of distinct patterns in type 1 diabetes. Diabetes Care. (2023) 46(11):1997–2003. doi: 10.2337/dc23-0312
PubMed Abstract | CrossRef Full Text | Google Scholar
24. Bakke Å, Cooper JG, Thue G, Skeie S, Carlsen S, Dalen I, et al. Type 2 diabetes in general practice in Norway 2005–2014: moderate improvements in risk factor control but still major gaps in complication screening. BMJ Open Diabetes Res Care. (2017) 5:e000459. doi: 10.1136/bmjdrc-2017-000459
PubMed Abstract | CrossRef Full Text | Google Scholar
25. Will JC, Yuan K, Ford E. National trends in the prevalence and medical history of angina: 1988 to 2012. Circ Cardiovasc Qual Outcomes. (2014) 7:407–13. doi: 10.1161/CIRCOUTCOMES.113.000779
PubMed Abstract | CrossRef Full Text | Google Scholar
26. Warren B, Rebholz CM, Sang Y, Lee AK, Coresh J, Selvin E, et al. Diabetes and trajectories of estimated glomerular filtration rate: A prospective cohort analysis of the atherosclerosis risk in communities study. Diabetes Care. (2018) 41:1646–53. doi: 10.2337/dc18-0277
PubMed Abstract | CrossRef Full Text | Google Scholar
27. ElSayed NA, Aleppo G, Aroda VR, Bannuru RR, Brown FM, Bruemmer D, et al. 12. Retinopathy, neuropathy, and foot care: Standards of care in diabetes—2023. Diabetes Care. (2022) 46:S203–S15. doi: 10.2337/dc23-SO12
CrossRef Full Text | Google Scholar
28. Boyko EJ, Zelnick LR, Braffett BH, Pop-Busui R, Cowie CC, Lorenzi GM, et al. Risk of foot ulcer and lower-extremity amputation among participants in the diabetes control and complications trial/epidemiology of diabetes interventions and complications study. Diabetes Care. (2022) 45:357–64. doi: 10.2337/dc21-1816
PubMed Abstract | CrossRef Full Text | Google Scholar
29. Drivsholm T, Eplov LF, Davidsen M, Jorgensen T, Ibsen H, Hollnagel H, et al. Representativeness in population-based studies: a detailed description of non-response in a Danish cohort study. Scand J Public Health. (2006) 34:623–31. doi: 10.1080/14034940600607616
留言 (0)