Trigeminal neuralgia (TN) can be defined as a neurological disorder characterized by sudden, unilateral, temporary, electric shock-like neuropathic facial pain in one or more distributions of the fifth cranial nerve. Although this definition was primarily based on expert opinions, TN can be classified into two forms: one that is “purely paroxysmal” and the other that is “with concomitant persistent facial pain” (1). There are also three types of TN: essential, idiopathic, and classical. Blood vessels compressing the trigeminal nerve root as it enters the brain stem is the cause of nearly all occurrences of trigeminal neuralgia (2). It has been demonstrated that not all patients with TN had vascular compression, and vice versa. Although neurovascular compression accounts for most TN cases, primary demyelination disorders, such as multiple sclerosis (MS), can also lead to TN symptoms (2–4). It is often known that women have trigeminal neuralgia at higher rates than men do (5). It has been well documented that patients with MS are at a higher risk of developing neuropathic pain and are estimated to be 20 times more likely to develop TN than the general population (6).
Due to the potential severity of the pain, debilitating effects of TN on the social life of the depressed patient, either physically, mentally, or socioeconomically, have been well documented in numerous studies (7, 8). TN can cause episodes of severe pain up to 50 times per day, which typically last for only a few seconds to 2 min (9). These TN episodes, which refer to the duration of repeated attacks, can vary from days to months, but they can also have lengthy remission intervals. The condition most commonly affects people over the age of 50 years, and women are more frequently affected than men (10). Non-neurologists such as dentists, general practitioners, internists, anesthesiologists, and neurosurgeons often treat individuals with trigeminal neuralgia. The patient's medical history and pain characteristics are the only factors used in the diagnosis. Due to a vast range of clinical symptomatology, delays or incorrect diagnoses frequently occur (11).
The symptoms of TN can be exacerbated by daily activities such as touching the skin lightly, washing, shaving, tooth brushing, blowing the nose, drinking hot or cold beverages, encountering a light breeze, applying makeup, smiling, and talking (12). The pathophysiology of TN is still mostly unclear. The current consensus on the underlying etiology of TN, also known as classical TN, is that it is caused by localized demyelination of the trigeminal nerve root entrance zone induced by compression from an aberrant artery or vein. Furthermore, it has been proven that TN is more common in patients with multiple sclerosis, leading to bilateral symptomatic or secondary TN (STN). Few published studies support a possible inheritance pattern of trigeminal neuralgia, implying that genetics may play a role in TN pathophysiology (13, 14).
Most previous studies revealed that the mandibular division was most commonly engaged, while the ophthalmic division was less frequently involved. The maxillary division persisted between the mandibular and ophthalmic divisions (15, 16). Some researchers have reported that atypical TN causes pain in the second and third divisions of the trigeminal nerve (16, 17). However, research ought to focus on pinpointing the precise causes of the affected side and the involvement of nerve branches. Previous literature reviews in this area are limited to specific involvement of the trigeminal nerve branch and the side of the face involved. Therefore, investigation of the affected nerve branches in trigeminal neuralgia might have paramount importance for early diagnosis and appropriate management. The aim of this systematic review was to answer the focused question, “What is the commonly affected nerve branch and the side of the face involved in trigeminal neuralgia?”
Methods and materials Search strategy and study inclusion criteriaThe searches were carried out by three independent authors (AA, ND, and BK) using the PubMed electronic database and Google scholar. In PubMed, we used the advanced search option to select relevant Medical Subject Headings (MeSH) terms. To obtain many results, we used the explode function, included all subheadings, and conducted a keyword search for each term using the multi-purpose (mp) function. Boolean operators combined the search terms. The results were limited to English language articles and studies conducted on humans (Table 2). AA and MA visually screened the titles and abstracts of the search results for eligibility according to the predefined criteria. The full text of the selected articles was then assessed to confirm eligibility. Articles that did not fulfill the criteria were excluded. In cases of ambiguous ideas, eligibility for inclusion was determined after a full-text review and discussion with the third party (YM, MT).
The terms ((“trigeminal neuralgia”[MeSH Terms] OR (“trigeminal”[All Fields] AND “neuralgia”[All Fields]) OR “trigeminal neuralgia”[All Fields]) AND (((“trigeminal nerve”[MeSH Terms] OR (“trigeminal”[All Fields] AND “nerve”[All Fields]) OR “trigeminal nerve”[All Fields]) AND (“branch”[All Fields] OR “branch s”[All Fields] OR “branche”[All Fields] OR “branched”[All Fields] OR “branches”[All Fields] OR “branching”[All Fields] OR “branching”[All Fields] OR “branches”[All Fields])) OR (“trigeminal nerve”[MeSH Terms] OR (“trigeminal”[All Fields] AND “nerve”[All Fields]) OR “trigeminal nerve”[All Fields] OR (“fifth”[All Fields] AND “cranial”[All Fields] AND “nerve”[All Fields]) OR “fifth cranial nerve”[All Fields]) OR (“5th”[All Fields] AND (“cranial nerves”[MeSH Terms] OR (“cranial”[All Fields] AND “nerves”[All Fields]) OR “cranial nerves”[All Fields] OR (“cranial”[All Fields] AND “nerve”[All Fields]) OR “cranial nerve“[All Fields])))) AND (fft[Filter]) were used in various combinations as primary search keywords.
Studies that provided information about the distribution of pain, the side of the face involved, clear descriptions regarding the diagnosis modalities, and the clearly identified trigeminal nerve branch involved in TN were included. However, studies that did not provide any specific report, consensus documents, or articles published before 2000 G.C. were excluded.
Data extractionAfter removing duplicates, title and abstract screening was conducted by three authors independently. After applying the selection criteria, all eligible studies with full texts were read, and the relevant references were checked manually. Three researchers independently extracted the data according to the inclusion and exclusion criteria, and the extracted data include the author's name, year of study, country, sample size, study design, frequency of the involved nerve branch, and the side of the face involved. When there was a difference of opinion, discussions with another author (GW) occurred until an agreement was reached. The extra reviewer confirmed the extracted data for accuracy.
Quality and risk-of-bias assessmentThe modified version of a quality assessment tool validated in a previous study was used to assess the qualities of the included studies. Three reviewers (AT, MM, and AWA) independently assessed the quality of the included studies. This review addressed the key domains of trigeminal neuralgia, including the side of the face involved, the affected trigeminal nerve branch, and the number of patients investigated. The discrepancies between three reviewers were resolved through discussion and there are articles that were included after consensus. The quality of the studies was assessed using the Newcastle-Ottawa Quality Assessment Scale (NOS). Based on the results of the quality assessment tool, the maximum score obtained from all questions was considered as having a low risk of bias. Total scores of 0–3, 4–6, and 7–9 were classified as low, moderate, and high risk of bias, respectively (28) (Table 1).
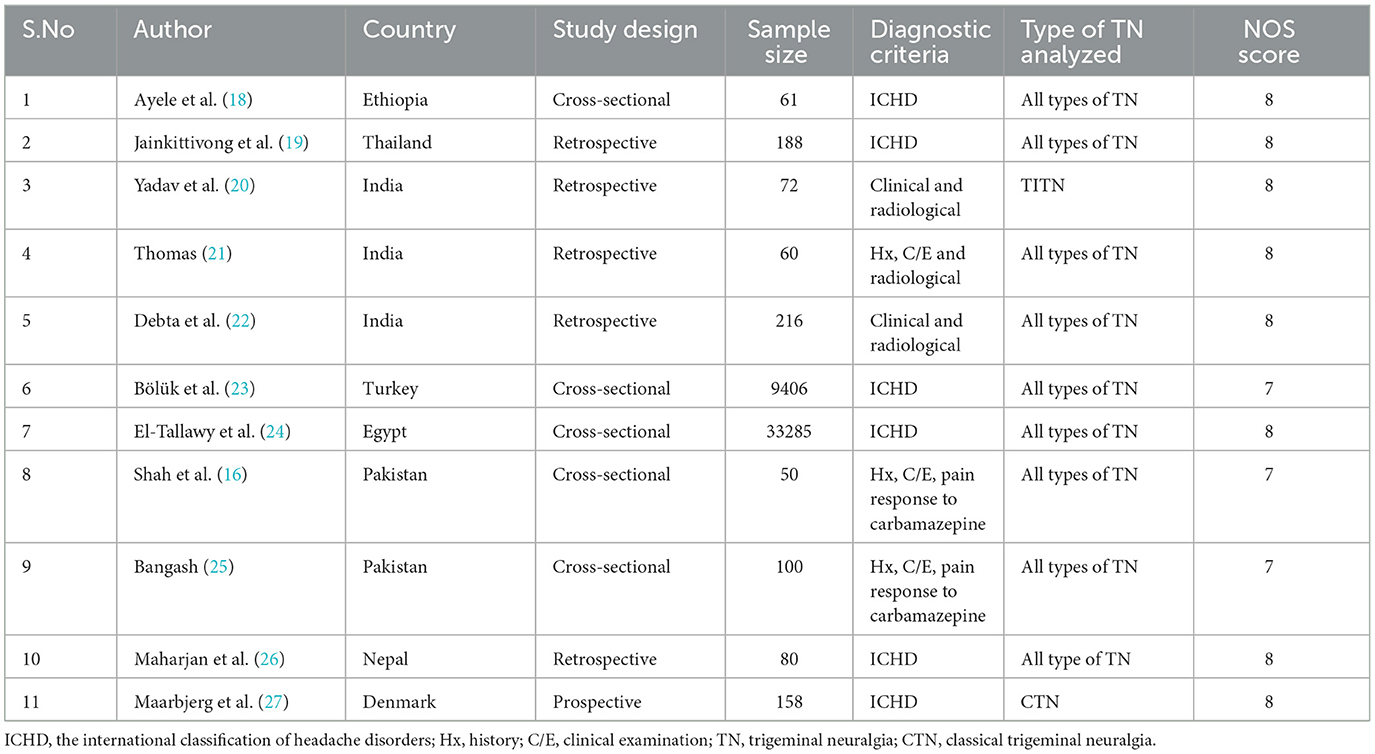
Table 1. Basic characteristics of the included studies.
Statistical analysisIt was impossible to perform an appropriate meta-analysis because of the lack of research data among the studies related to this subject.
Results Study selection and identificationPublications addressing the examination of the frequency of occurrence in different nerve branches and the side of the face involved in trigeminal neuralgia are included in this systematic review. A search of the database yielded 132 items in all. After the removal of articles due to duplications and other reasons, only 79 articles remained. After reading the abstract and the title, additional screening was conducted, and 40 articles were eliminated. Due to a lack of eligibility and non-retrieval of reports, 28 surviving items were again eliminated. As seen in the PRISMA flow diagram, 11 possible articles were ultimately included for qualitative synthesis (Figure 1).

Figure 1. PRISMA flow diagram of article selection for systematic review on the frequency of occurrence in different nerve branches and the side of the face involved in trigeminal neuralgia.
Characteristics of the included studiesThree of the 10 included studies were conducted in India (20–22), two studies were from Pakistan (16, 25), and one study each was conducted in Ethiopia (18), Turkey (23), Nepal (26), Egypt (24), Denmark (27), and Thailand (19). All of the included studies analyzed all types of TN, except for one study conducted in India that specifically analyzed idiopathic typical trigeminal neuralgia (ITTN) (20). A total of 43,676 study participants were included in the review. The studies contain a minimum and a maximum sample size of 50 and 33,285 participants, respectively. Regarding the diagnosis method of TN, all of the included studies relied on history, clinical examination, and radiological imaging as per the International Classification of Headache Disorders, 3rd edition, from the International Headache Society (ICHD-3/IHS) (10) (Table 1).
Occurrence of trigeminal nerve branches and the side of the face involvedAccording to a study conducted in Ethiopia, it was found that TN affected the left side of the face in 29.5% of patients, the right side in 68.9% of patients, and both sides of the face in 1.6% of patients. The maxillary and mandibular branches (V2 + V3) were affected in 34.4% of the patients, while the mandibular branch (V3) was affected in half of the patients. No patient showed any evidence of a single ophthalmic branch involvement (V1) (18). Another retrospective study in Thailand showed that the mandibular division of the trigeminal nerve was shown to be the most commonly affected (30.3%) division, followed by the maxillary division alone (25%) and the combined maxillary and mandibular divisions (29.3%) (19).
The most commonly implicated branch was the mandibular division. Neuralgic discomfort limited to the mandibular distribution of the face was experienced by 56.9% of respondents. Of the patients who reported mandibular division involvement, 38.89% indicated involvement of the inferior alveolar nerve, and 18.05% experienced neuralgic pain limited to the mental nerve's distribution. Furthermore, 37.5% of patients experienced neuralgic pain in the maxillary nerve distribution, with all cases including the infraorbital nerve involvement, while 5.6% of patients experienced involvement of both the infraorbital and maxillary divisions on the same side as involvement of the mental and mandibular nerves (20).
Moreover, another study in Nepal assessed 100 TN patients and found that the right side of the face was found to be involved in 64% of them, while 36% of them had involvement on the left side. No case presented with bilateral involvement. The mandibular division was most commonly involved, accounting for 55%, followed by the maxillary (39%) and ophthalmic divisions (6%). The combination of V2 and V3 was seen in only 9% of patients. The combined involvement of all three divisions was not seen in this study (25).
Furthermore, a study conducted in Turkey using a large sample size found that 60% of cases had right-side involvement and 40% had left-side TN. It was also found that 20% of the patients had isolated maxillary involvement, 20% had isolated mandibular involvement, and 60% had combined maxillary and mandibular nerve involvement (23). Except for one study conducted in India (21) that found 60% of TN patients were affected by the maxillary nerve division, all other included studies reported that the mandibular division was the most commonly involved nerve, and the right side of the face was predominantly affected in all included studies (Table 2).

Table 2. Summary of different studies showing the frequency of occurrence in different nerve branches and the side of the face involved in trigeminal neuralgia.
DiscussionAlthough it is uncommon, TN lowers a person's quality of life when it does occur. Facial pain is the main TN symptom, which can make daily tasks such as eating and drinking difficult. The type and frequency may negatively influence a patient's quality of life and intensity of their pain, and pain may be linked to depression (11, 29, 30).
Our systematic review investigated the available evidence on the frequency of occurrence in trigeminal nerve branches, diagnosis modalities, and the sidedness of the face involved in trigeminal neuralgia. A lack of evidence about the commonest branches of the trigeminal nerve and the sidedness of the face involved in TN were confirmed as we reviewed the literature.
Furthermore, our determination of the frequency of occurrence in nerve branches, diagnosis modalities, and the sidedness of the face involved was hindered due to the complexity of identification and the variability of disease characteristics. In addition, we discovered that, due to these complications, it was not possible to have a comprehensive understanding of the phenomenon in a few studies that were restricted to reporting some variables rather than quantifying the occurrence of common nerve branches and the sidedness of the face involved.
Based on the reviewed literature, TN is diagnosed based on clinical grounds; therefore, a thorough clinical history, with special attention to the patient's description of symptoms, is the first essential step in the diagnosis process (31). The majority of research studies that have been published indicated that the ocular division (V1) was less frequently exhibited and that the mandibular division (V3) was most frequently implicated, followed by the maxillary division (10, 18, 19, 23, 32, 33). Furthermore, this systematic review revealed that the right side of the face is more frequently affected than the left side in 90% of the included articles, and this could be due to the fact that the foramen rotundum and foramen ovale on the right are narrower than those on the left (32).
This systematic review highlights the variability in the diagnosis modalities and summarizes the frequency of affected trigeminal nerve branches and involved facial sides that have been treated using medical and surgical interventions for TN by clinicians to date.
It is important to note that this review has a few shortcomings. Initially, very few studies fulfilled the strict requirements. Second, most of the reviewed studies were based on the retrospective study design. There is no meta-analysis in this review, which could offer stronger support than a systematic review alone. Therefore, more epidemiologic research with verified TN diagnostic standards and meta-analyses are necessary.
Data availability statementThe original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Author contributionsAT: Writing – review & editing, Writing – original draft, Software, Methodology, Formal analysis, Conceptualization. GW: Writing – review & editing, Methodology, Formal analysis. BA: Writing – original draft, Supervision, Investigation. NB: Conceptualization, Methodology, Software, Writing – review & editing. AAA: Writing – original draft, Supervision, Investigation, Data curation. MM: Conceptualization, Methodology, Supervision, Writing – original draft. TY: Methodology, Supervision, Writing – original draft. AG: Writing – review & editing, Supervision, Methodology, Conceptualization. ES: Writing – review & editing, Methodology, Data curation, Conceptualization. YM: Supervision, Writing – review & editing, Conceptualization, Methodology. MT: Conceptualization, Supervision, Writing – review & editing. AWA: Writing – review & editing, Supervision, Methodology, Conceptualization.
FundingThe author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interestThe authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's noteAll claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References1. Maarbjerg S, Gozalov A, Olesen J, Bendtsen L. Concomitant persistent pain in classical trigeminal neuralgia–evidence for different subtypes. Headache. (2014) 54:1173–83. doi: 10.1111/head.12384
PubMed Abstract | Crossref Full Text | Google Scholar
2. Islam J, Elina K, Park YS. Recent update on trigeminal neuralgia. J Korean Soc Ster Func Neurosurg. (2022) 18:9–19. doi: 10.52662/jksfn.2022.00150
Crossref Full Text | Google Scholar
3. Maarbjerg S, Di Stefano G, Bendtsen L, Cruccu G. Trigeminal neuralgia–diagnosis and treatment. Cephalalgia. (2017) 37:648–57. doi: 10.1177/0333102416687280
Crossref Full Text | Google Scholar
4. Sindou M, Howeidy T, Acevedo G. Anatomical observations during microvascular decompression for idiopathic trigeminal neuralgia (with correlations between topography of pain and site of the neurovascular conflict). Prospective study in a series of 579 patients. Acta Neurochir. (2002) 144:1–13. doi: 10.1007/s701-002-8269-4
PubMed Abstract | Crossref Full Text | Google Scholar
5. De Stefano G, Litewczuk D, Mollica C, Di Pietro G, Galosi E, Leone C, et al. Sex differences in trigeminal neuralgia: a focus on radiological and clinical characteristics. Neurol Sci. (2023) 44:4465–72. doi: 10.1007/s10072-023-06923-5
PubMed Abstract | Crossref Full Text | Google Scholar
6. Di Stefano G, Maarbjerg S, Truini A. Trigeminal neuralgia secondary to multiple sclerosis: from the clinical picture to the treatment options. J Headache Pain. (2019) 20:1–10. doi: 10.1186/s10194-019-0969-0
PubMed Abstract | Crossref Full Text | Google Scholar
8. O'Callaghan L, Floden L, Vinikoor-Imler L, Symonds T, Giblin K, Hartford C, et al. Burden of illness of trigeminal neuralgia among patients managed in a specialist center in England. J Headache Pain. (2020) 21:1–10. doi: 10.1186/s10194-020-01198-z
PubMed Abstract | Crossref Full Text | Google Scholar
9. Cruccu G, Finnerup NB, Jensen TS, Scholz J, Sindou M, Svensson P, et al. Trigeminal neuralgia: new classification and diagnostic grading for practice and research. Neurology. (2016) 87:220–8. doi: 10.1212/WNL.0000000000002840
PubMed Abstract | Crossref Full Text | Google Scholar
10. De Toledo IP, Conti Réus J, Fernandes M, Porporatti AL, Peres MA, Takaschima A, et al. Prevalence of trigeminal neuralgia: a systematic review. J Am Dent Assoc. (2016) 147:570–6.e2. doi: 10.1016/j.adaj.2016.02.014
Crossref Full Text | Google Scholar
11. Bendtsen L, Zakrzewska JM, Abbott J, Braschinsky M, Di Stefano G, Donnet A, et al. European academy of neurology guideline on trigeminal neuralgia. Eur J Neurol. (2019) 26:831–49. doi: 10.1111/ene.13950
PubMed Abstract | Crossref Full Text | Google Scholar
12. Montano N, Conforti G, Di Bonaventura R, Meglio M, Fernandez E, Papacci F. Advances in diagnosis and treatment of trigeminal neuralgia. Ther Clin Risk Manag. (2015) 11:289. doi: 10.2147/TCRM.S37592
Crossref Full Text | Google Scholar
13. Tronnier VM, Rasche D, Hamer J, Kienle AL, Kunze S. Treatment of idiopathic trigeminal neuralgia: comparison of long-term outcome after radiofrequency rhizotomy and microvascular decompression. Neurosurgery. (2001) 48:1261–8. doi: 10.1227/00006123-200106000-00014
PubMed Abstract | Crossref Full Text | Google Scholar
14. Burchiel KJ, Baumann TK. Pathophysiology of trigeminal neuralgia: new evidence from a trigeminal ganglion intraoperative microneurographic recording: case report. J Neurosurg. (2004) 101:872–3. doi: 10.3171/jns.2004.101.5.0872
PubMed Abstract | Crossref Full Text | Google Scholar
15. Oyetola E, Adewale A, Elijah O, Theophilus Agho E, Taofeek A, Owotade FJ. Patterns of presentation of trigeminal neuralgia in patients attending the oral medicine clinic in a Nigerian Tertiary Hospital. Af J Oral Maxillofac Pathol Med. (2018) 4:40–5.
16. Shah SA, Murad N, Alaar A, Iqbal N. Trigeminal neuralgia: analysis of pain distribution and nerve involvement. Pakistan Oral Dent J. (2008) 28:37–41.
17. Santo Neto H, Camilli JA, Marques MJ. Trigeminal neuralgia is caused by maxillary and mandibular nerve entrapment: greater incidence of right-sided facial symptoms is due to the foramen rotundum and foramen ovale being narrower on the right side of the cranium. Med Hypotheses. (2005) 65:1179–82. doi: 10.1016/j.mehy.2005.06.012
PubMed Abstract | Crossref Full Text | Google Scholar
18. Ayele BA, Mengesha AT, Zewde YZ. Clinical characteristics and associated factors of trigeminal neuralgia: experience from Addis Ababa, Ethiopia. BMC Oral Health. (2020) 20:1–7. doi: 10.1186/s12903-020-01227-y
PubMed Abstract | Crossref Full Text | Google Scholar
20. Yadav S, Mittal H-C, Sachdeva A, Verma A, Dhupar V, Dhupar A. A retrospective study of 72 cases diagnosed with idiopathic trigeminal neuralgia in indian populace. J Clin Exp Dent. (2015) 7:e40. doi: 10.4317/jced.51771
PubMed Abstract | Crossref Full Text | Google Scholar
21. Thomas R. Clinical and radiological profile of trigeminal neuralgia-a retrospective study. J Clin Diagn Res. (2020) 14. doi: 10.7860/JCDR/2020/46782.14261
Crossref Full Text | Google Scholar
22. Debta P, Sarode G, Sarode S, Gadbail A, Debta FM, Swain SK, et al. Natural history of trigeminal neuralgia—a hospital-based retrospective study. Oral Dis. (2020) 26:647–55. doi: 10.1111/odi.13263
PubMed Abstract | Crossref Full Text | Google Scholar
23. Bölük C, Türk Börü Ü, Taşdemir M. The prevalence of trigeminal neuralgia in Turkey: a population-based study. Neurol Res. (2020) 42:968–72. doi: 10.1080/01616412.2020.1794372
Crossref Full Text | Google Scholar
24. El-Tallawy HN, Farghaly WM, Rageh TA, Shehata GA, Abdel Hakeem M N, Badry R, et al. Prevalence of trigeminal neuralgia in Al-Quseir city (Red sea Governorate), Egypt. Clin Neurol Neurosurg. (2013) 115:1792–4. doi: 10.1016/j.clineuro.2013.04.014
PubMed Abstract | Crossref Full Text | Google Scholar
26. Maharjan IK, Rimal J, Subedi A, Regmee P. Clinical profile and treatment outcome of patients with trigeminal neuralgia: a retrospective study in a tertiary hospital of Eastern Nepal. J Nepal Soc Periodontol Oral Implantol. (2022) 6:85–90. doi: 10.3126/jnspoi.v6i2.53010
Crossref Full Text | Google Scholar
27. Maarbjerg S, Gozalov A, Olesen J, Bendtsen L. Trigeminal neuralgia–a prospective systematic study of clinical characteristics in 158 patients. Headache. (2014) 54:1574–82. doi: 10.1111/head.12441
PubMed Abstract | Crossref Full Text | Google Scholar
28. Hoy D, Brooks P, Woolf A, Blyth F, March L, Bain C, et al. Assessing risk of bias in prevalence studies: modification of an existing tool and evidence of interrater agreement. J Clin Epidemiol. (2012) 65:934–9. doi: 10.1016/j.jclinepi.2011.11.014
PubMed Abstract | Crossref Full Text | Google Scholar
29. Di Stefano G, Yuan J-H, Cruccu G, Waxman SG, Dib-Hajj SD, Truini A. Familial trigeminal neuralgia–a systematic clinical study with a genomic screen of the neuronal electrogenisome. Cephalalgia. (2020) 40:767–77. doi: 10.1177/0333102419897623
PubMed Abstract | Crossref Full Text | Google Scholar
31. Alshukry A, Salburgo F, Jaloux L, Lavieille J-P, Montava M. Trigeminal neuralgia (TN): A descriptive literature analysis on the diagnosis and management modalities. J Stomatol Oral Maxillofac Surg. (2017) 118:251–4. doi: 10.1016/j.jormas.2017.06.010
PubMed Abstract | Crossref Full Text | Google Scholar
33. Prasetya M, Adidharma P, Sulistyanto A, Inoue T, Arham A. Characteristics of patients with trigeminal neuralgia referred to the Indonesian National Brain Center Neurosurgery Clinic. Front Surg. (2022) 8:697. doi: 10.3389/fsurg.2021.747463
留言 (0)