Since February 2020, over 104 million people in the United States have been diagnosed with SARS-CoV-2 infection, or COVID-19, with over 8.5 million, or 28,812 per hundred thousand population, reported in the state of Texas (1). The risk of SARS-CoV-2 exposure, progression to clinical disease, and severe outcomes such as hospitalization and death depend on both individual and societal factors (2–6). However, there is increasing recognition of significant rates of severe COVID-19 outcomes and post-acute syndromes, including long COVID, among populations previously thought to be ‘low-risk’ (7–9). Furthermore, the absolute risk of outcomes, such as hospitalization and death, have changed over time as novel SARS-CoV-2 variants emerged, vaccinations increased, and public health policies adapted to local epidemic dynamics (10–12).
As the pandemic progressed, social determinants of health, including demographic, financial, and social factors, emerged as significant contributors to adverse COVID-19 outcomes. Investigations have highlighted the risk of SARS-CoV-2 exposure among low-income, minority, and immigrant populations (13), and the impracticality of quarantine and isolation guidelines in high-density housing and other communal settings (14). Additionally, disparities in healthcare utilization among members of different socioeconomic groups were well documented before and during the COVID-19 pandemic (15–17). Hospital visits, especially unplanned readmissions, are important metrics not only of patient health, but also of healthcare practices, population health, and care costs (18, 19).
While increasing age and comorbidity burden have been identified as independent risk factors for COVID-19-related hospitalization and readmission, the relationship between readmission across healthcare systems and social determinants of health in the United States has been described in only a few studies (4, 20, 21). Therefore, the current study aimed to investigate 30, 60, and 90-day readmission outcomes among patients with a COVID-19-associated inpatient hospitalization encounter identified within a regional health information exchange between February 1, 2020, to December 1, 2022.
2 Methods 2.1 Health information exchangeGreater Houston Healthconnect (GHH) is the regional health information exchange (HIE) for Southeast Texas. GHH collects prospective and retrospective health data from approximately 15.5 million unique patients from more than 75 Texas counties and 40 Louisiana parishes through partnerships with more than 150 member hospitals, over 2,000 ambulatory practices, and several local public health departments. In practice, HL7 version 2 real-time feeds and Consolidated Continuity of Care Documents (C-CDA) are converted to a relational database with individual patients’ longitudinal electronic health data. While the primary objective of any HIE is to facilitate clinical care by supporting the efficient exchange of clinical information, these large EHR datasets are increasingly being utilized for treatment, payment, and operations-related research (22, 23).
2.2 Identification of COVID-19 casesCOVID-19 cases were defined as any patient with either: A COVID-19 diagnosis identified through ICD-10 or SNOMED CT codes (see Supplementary 1 for the codeset); A positive diagnostic laboratory test for SARS-CoV-2, including nucleic acid amplification tests and antigen tests (antibody tests were excluded); And a case report documented by local public health departments. Patients for whom a COVID-19 identification date could not be determined were excluded.
2.3 Study populationThe study area for this investigation covered most of Southeast Texas and included Brazoria, Burleson, Chambers, Fort Bend, Galveston, Grimes, Hardin, Harris, Jasper, Jefferson, Liberty, Madison, Matagorda, Montgomery, Nueces, Orange, Polk, San Jacinto, San Patricio, Walker, Waller, and Wharton counties, where a high proportion of hospitals are GHH members. Patients’ residential addresses were extracted at the time of the initial data pull (December 2022). Patients with an ‘inpatient’ encounter beginning within 7 days (+/−) of any COVID-19 identification date who resided within the study area were eligible for inclusion in the COVID-19 inpatient cohort. ‘Emergency Room’ type encounters were not included in the inpatient cohort.
2.4 Exclusion criteriaPediatric patients (<18 years of age), patients who were pregnant or delivering at their index encounter, patients who expired during their index encounter, and patients residing outside of the study area were excluded from readmission analyses. Pregnant patients were excluded from readmission analyses due to the likelihood of subsequent hospital encounters unrelated to COVID-19, i.e., labor and delivery encounters.
2.5 Study outcomesThe primary outcome was all-cause readmission, defined as any subsequent inpatient hospital encounter beginning within 90 days from discharge from the index encounter. Patients for whom readmission status could not be determined (e.g., a post-discharge encounter that was not clearly a readmission) were excluded from this analysis.
2.6 Study exposuresPatient demographics, including age at index encounter admission, sex, race, and ethnicity, were extracted directly from the EHR. The Charlson Comorbidity Index (CCI) was calculated as a measure of overall comorbidity burden (24, 25); individual CCI components were extracted by searching ICD-10-CM (26) and SNOMED CT (27) diagnosis codes associated with the index encounter as well as up to 3 years prior to the index encounter. Peaks in Texas COVID-19 incidence were used to categorize COVID-19 admissions to further reflect local epidemic dynamics (28).
2.7 Geographic informationCOVID-19 patient hospitalization data were collected for the state of Texas from publicly available Department of State Health Services (DSHS) datasets. Publicly available geographic information system (GIS) datasets were collected from the Texas Parks and Wildlife Department, the Texas Department of Transportation, the US Census repository, and DSHS. Ecological measures of socioeconomic disadvantage, including the Area Deprivation Index (ADI), which measures relative deprivation between all census block groups by state (29, 30) and the Social Vulnerability Index (SVI), which measures relative vulnerability to disaster among all census tracts in the state (31) were calculated from the geocoded patient-provided home addresses collated and analyzed December 2022. Heat maps were created by calculating kernel density estimates from patients’ residential addresses; low-density values (<15th quantile) were truncated to preserve patient privacy. All geospatial analyses were performed on ArcGIS Pro version 3.1.1 (ESRI, Redlands, CA).
2.8 Statistical analysesDemographic and clinical data were reported as frequencies and proportions for categorical variables and as the median and interquartile range (IQR) for continuous variables. Logistic regression modeling was performed to identify risk factors for readmission at 30, 60, and 90 days from discharge; crude and adjusted odds ratios and 95% confidence intervals are provided as estimates of risk for each outcome. Variable selection for the multivariable models was based on a priori clinical importance. For survival analyses, time zero was the date of discharge from the index encounter, event time was the date of first readmission, and data were censored at 90 days. All analyses were performed on Stata MP version 17.0 (StataCorp LLC, College Station, TX, United States). A p-value of <0.05 was considered nominally significant; a conservative, Bonferroni-corrected statistical significance threshold of 0.00625 was utilized in model-building.
2.9 Ethics statementThis retrospective registry-based study was approved by the Western Institutional Review Board as a quality improvement study and granted a waiver of informed consent (#1–1,053,411-1).
3 Results 3.1 Study populationFrom February 1, 2020, to December 1, 2022, 1,011,024 patients were identified as COVID-19 cases by diagnosis, laboratory testing, or local public health case reporting, of whom 133,298 (13%) had an inpatient hospital encounter within 7 days (+/−) of a COVID-19 identification date (Figure 1). Of these, 104,196 had a residential address within the study area, making-up the COVID-19 inpatient cohort (Figure 2). Of the inpatients, 80,253 were identified as COVID-19 cases during their index hospitalization. In this COVID-19 inpatient cohort, trends in inpatient admissions mirrored total COVID-19 incidence and total COVID-19 hospitalizations for the state of Texas (Figure 3). The median age at admission was 57.4 (IQR: 40.4–71.0), and 51,062 (49%) scored zero on the CCI (Table 1).
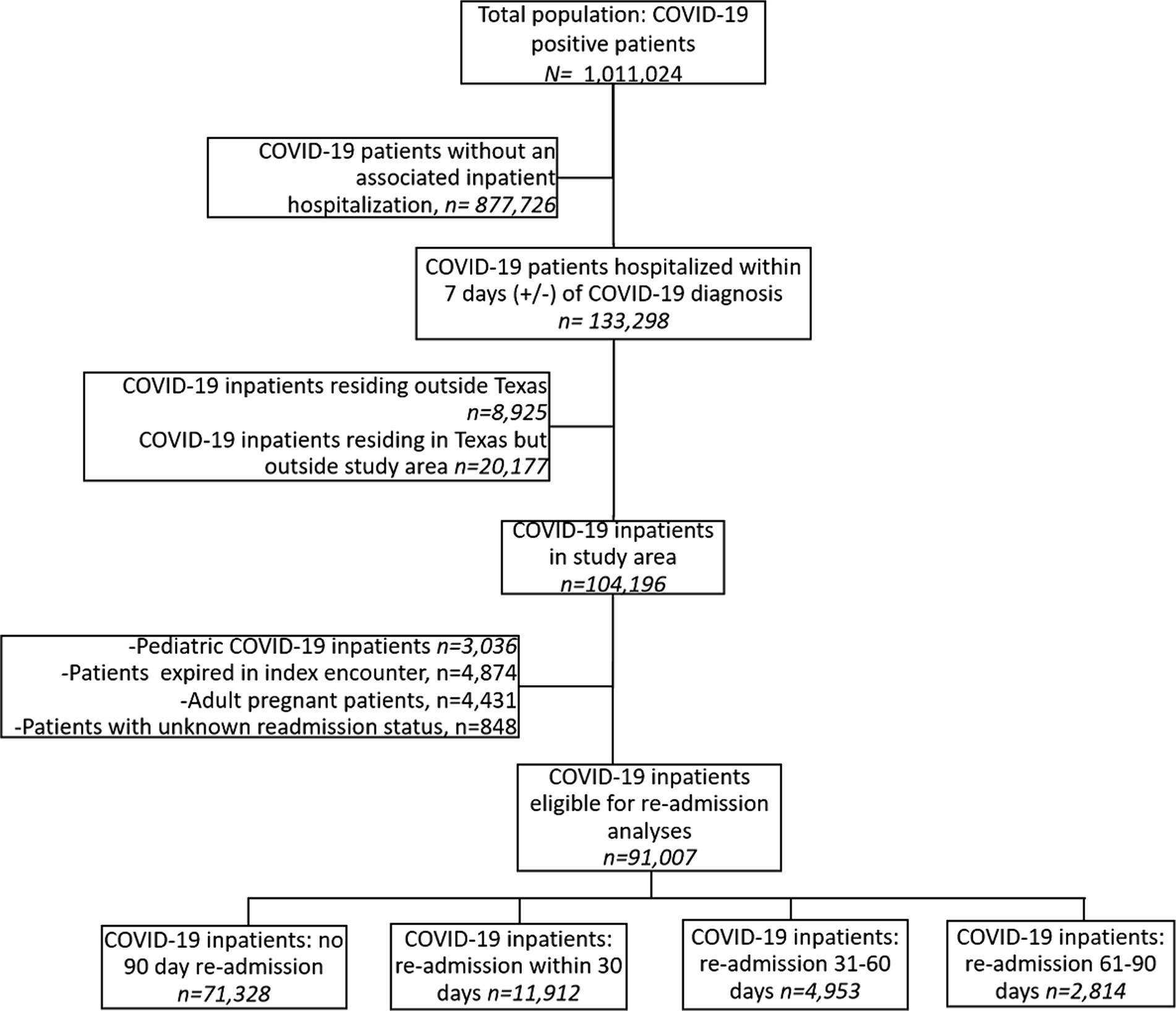
Figure 1. Study flowchart.
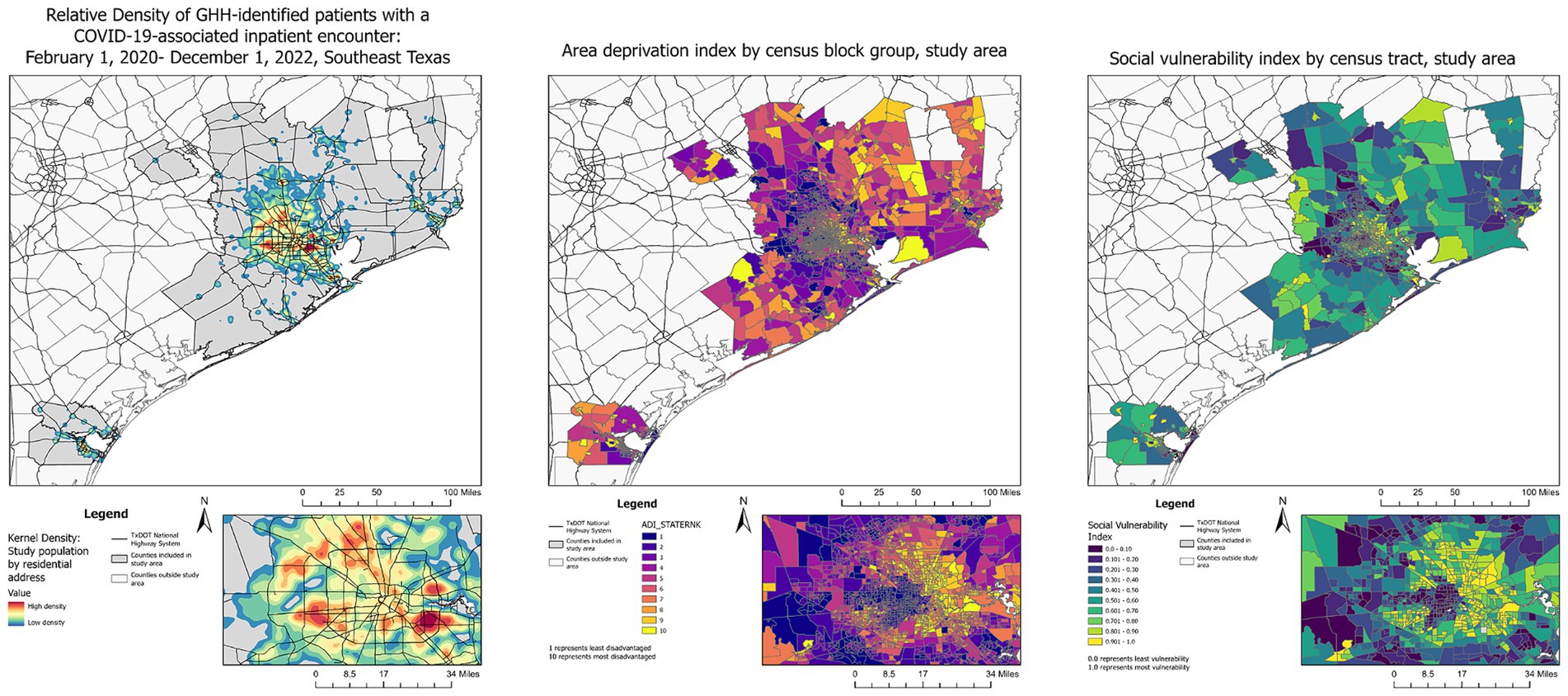
Figure 2. Relative density of GHH-identified patients with a COVID-19-associated inpatient encounter: February 1, 2020–December 1, 2022.
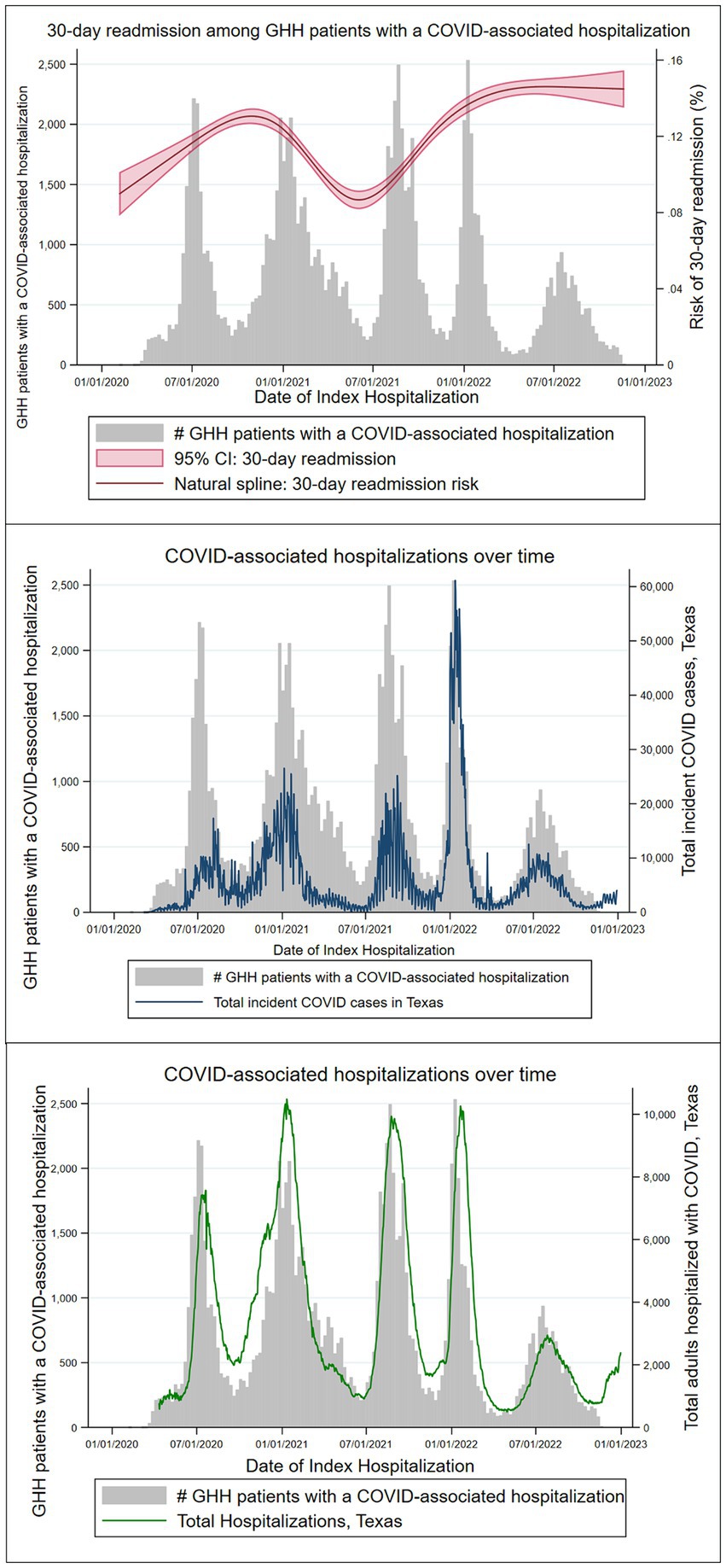
Figure 3. GHH patients with a COVID-19-associated hospitalization.
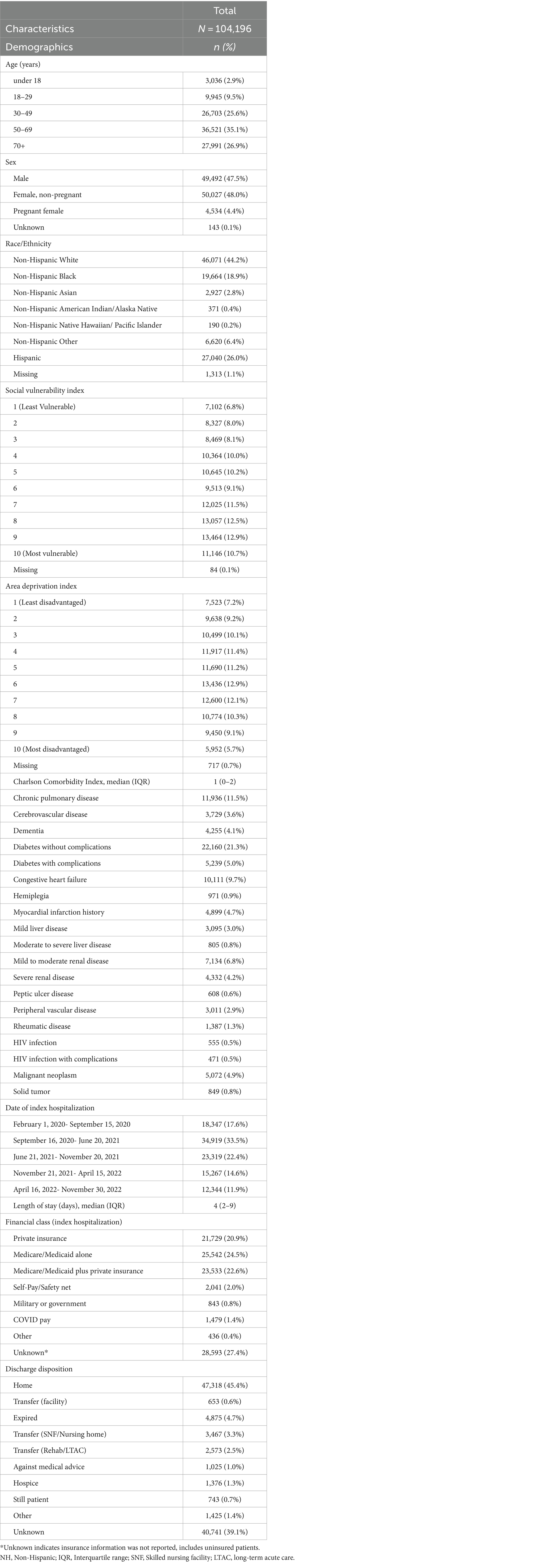
Table 1. Characteristics of GHH patients with a COVID-19-associated inpatient hospitalization.
At their index hospital encounter, 21% of patients were privately insured, 47% were Medicare or Medicaid clients, and 27% had no payer information available (Table 1). Index inpatient encounters that noted the death of the patient occurred 4,875 (5%) times and were excluded from these readmission analyses. In total, 91,007 adult inpatients were included in these readmission analyses, of whom 11,912 (13%) were readmitted within 30 days of discharge from their index encounter (Figure 1). Additionally, 14,479 (74%) of readmitted patients returned to the same hospital, while 5,200 (26%) were admitted to a different hospital from their index encounter. Of the 19,679 patients who were readmitted within 90 days, 822 (4%) expired during their first readmission encounter. Diagnoses associated with index and readmission encounters are shown in Supplementary 2.
3.2 Readmission analysesUnivariable logistic regression analyses for 30, 60, and 90-day readmission are shown in Table 2, and Kaplan–Meier survival curves for time to readmission are shown in Figures 4 5. Patients who expired during the observation period without a readmission (n = 2,499 patients) were excluded from Kaplan–Meier analyses. In multivariable logistic regression analysis, increasing age at encounter was significantly associated with 30, 60, and 90-day readmission (Table 3). Hispanic and non-Hispanic Asian patients were less likely to be readmitted within 90 days (aOR: 0.8, 95% CI: 0.7–0.9, and aOR: 0.8, 95% CI: 0.8–0.8), while non-Hispanic Black patients were more likely to be readmitted (aOR: 1.1, 95% CI: 1.0–1.1, p = 0.002), compared to non-Hispanic White patients. Living in neighborhoods with higher relative disadvantage was a significant risk factor in 30, 60, and 90-day readmission models. Increasing CCI scores were a risk factor in all readmission models. Medicare/Medicaid clients and patients without a named payor were more likely to be readmitted compared to patients with commercial insurance (aOR: 1.4, 95% CI: 1.3–1.5, and aOR: 1.3, 95% CI: 1.2–1.3), while patients with index encounters primarily covered by special COVID-19 funds were less likely to be readmitted within 90 days (aOR: 0.7, 95% CI: 0.5–0.8). Length of stay <2 days or ≥ 10 days were both risk factors for 90-day readmission compared to stays 4 to 5 days long (aOR: 2.0, 95% CI: 1.9–2.1, and aOR: 1.1, 95% CI: 1.0–1.1). To address the problem of competing risks of mortality and readmission and identify possible survivorship biases, we conducted additional analyses of 30-day mortality and readmission as a composite outcome (Supplementary 3). Receiver operating characteristic curves are displayed in Supplementary 4; area under the curve for each multivariable regression model are presented in the table legend (Figure 5).
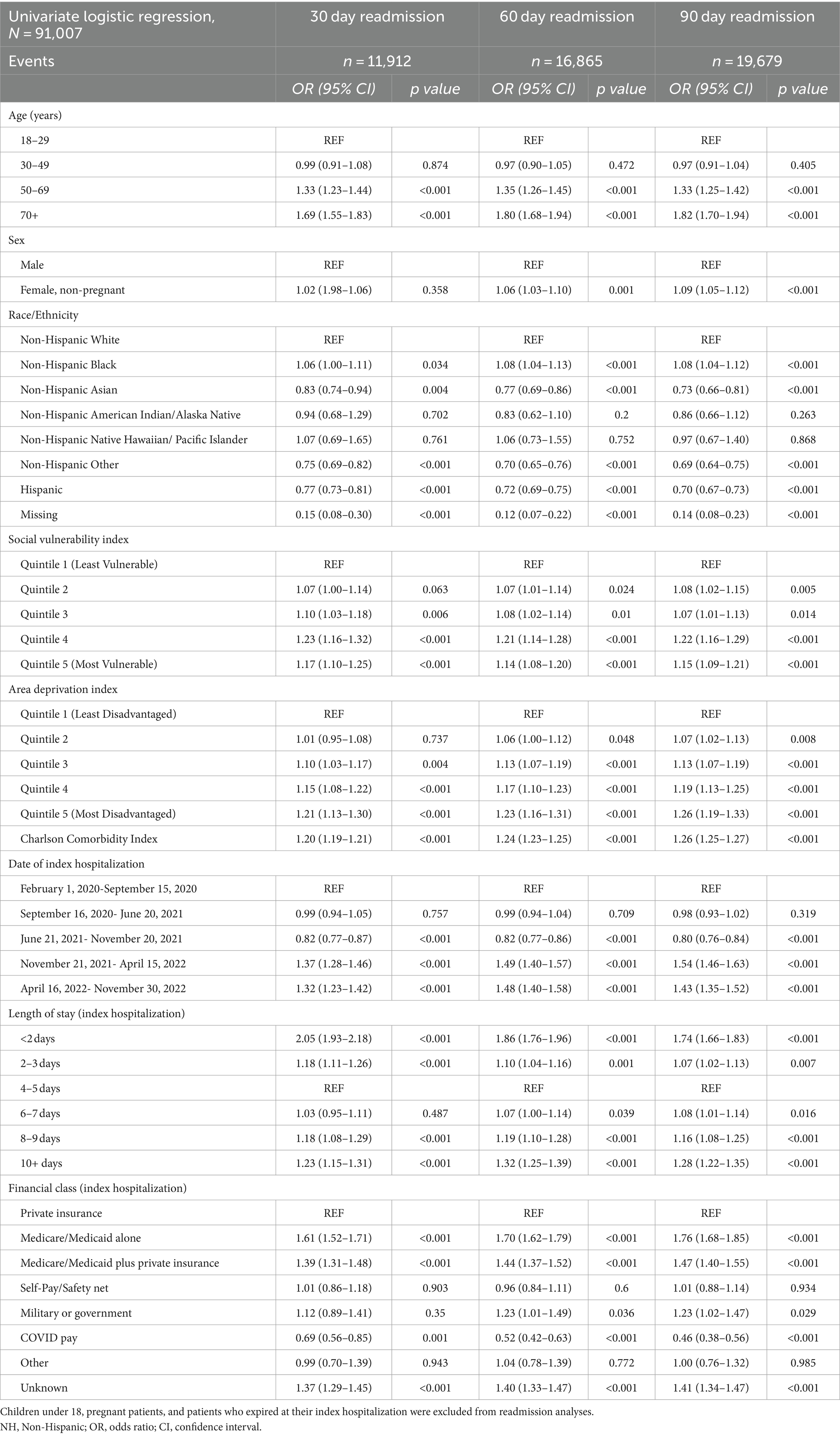
Table 2. Univariate logistic regression: readmission among patients with a COVID-19-associated inpatient hospitalization.
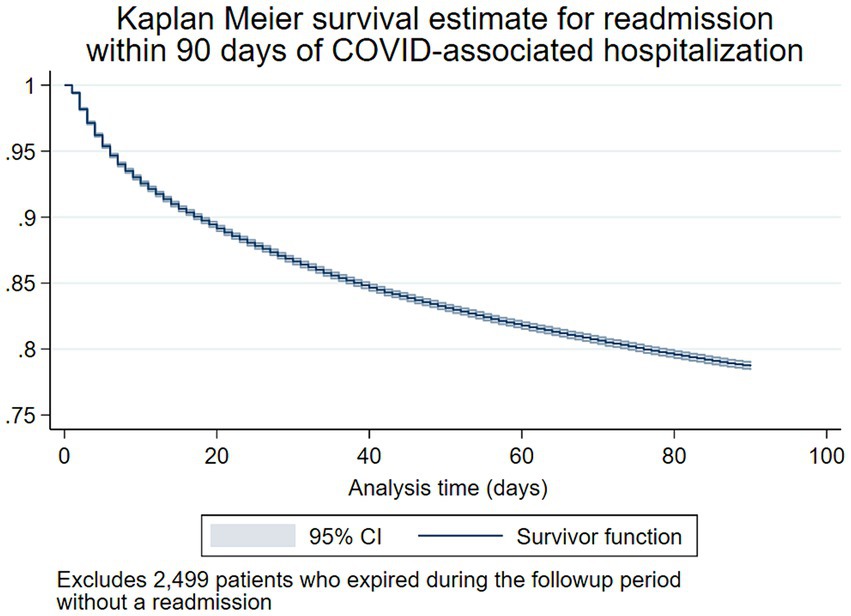
Figure 4. Kaplan–Meier survival estimate for 90-day readmission following COVID-19-associated hospitalization.
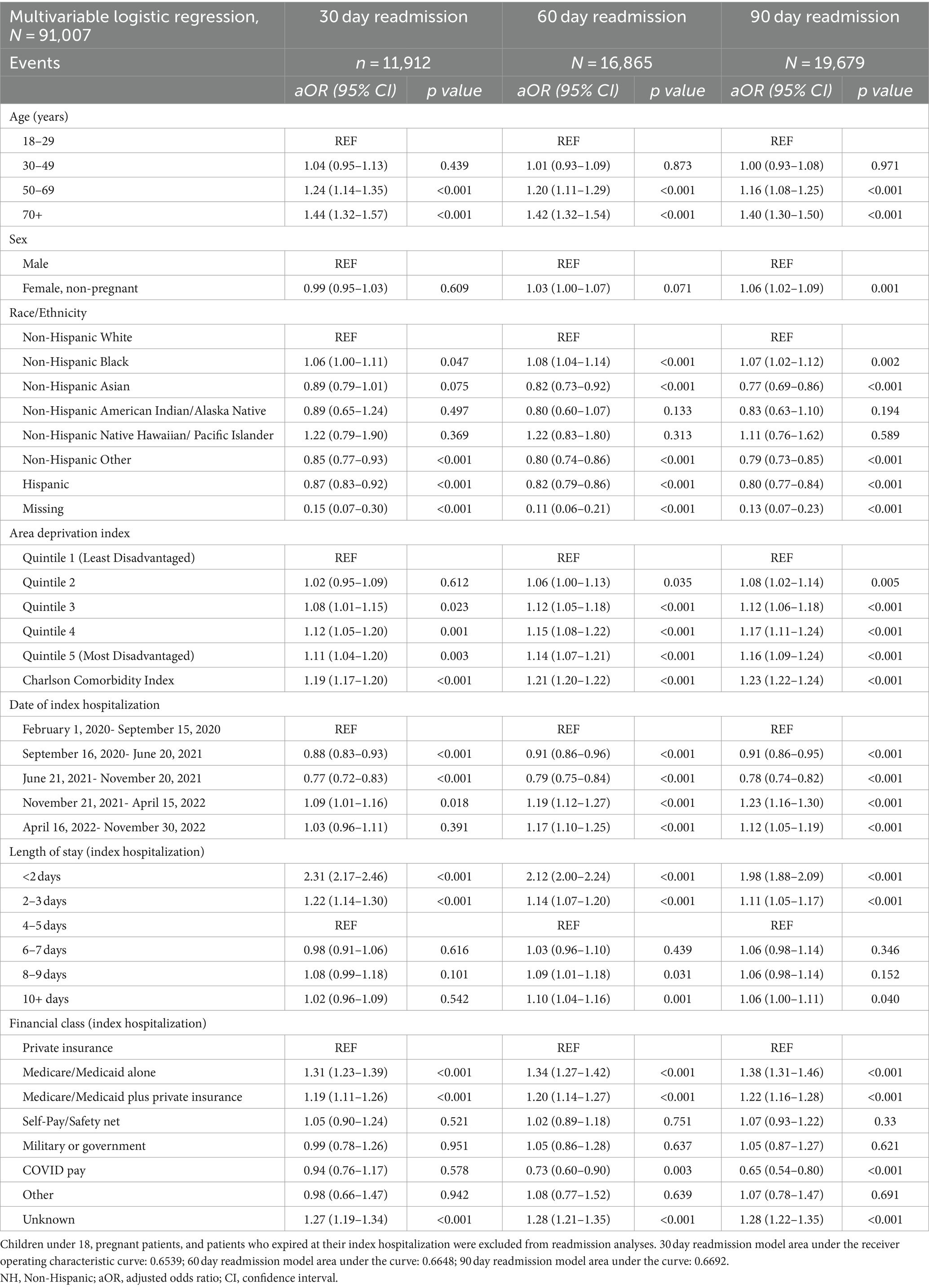
Table 3. Multivariable logistic regression: readmission among patients with a COVID-19-associated inpatient hospitalization.
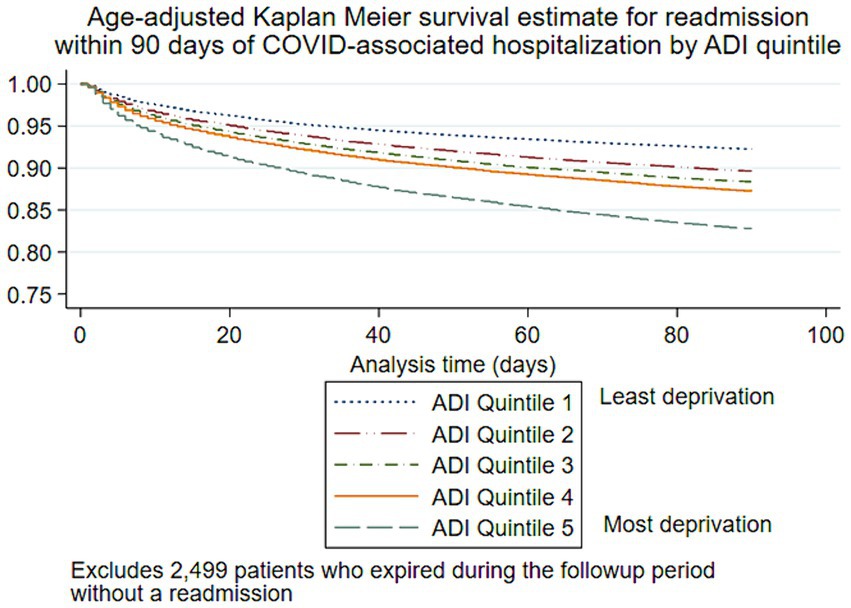
Figure 5. Age-adjusted Kaplan–Meier survival estimate for 90-day readmission following COVID-19-associated hospitalization by area deprivation index.
4 DiscussionIn this cohort of 91,007 adult patients with a COVID-19-associated hospitalization, over 21% were readmitted to the hospital within 90 days of their initial visit (n = 19,679), and 13% were readmitted within the first 30 days (n = 11,912). While this study did not seek to determine the cause of admission or readmission, the relative frequencies of diagnoses such as pneumonia, acute respiratory failure, and hypoxia are characteristics of a population of patients with severe COVID-19. Total 30-day readmission risk varied significantly across time points, falling during the period of July 2021 through November 2021, when Delta was the dominant circulating variant and then peaking during the period of December 2021 to December 2022, as Omicron group variants became dominant.
The measured social determinants of health, including race/ethnicity, relative neighborhood disadvantage (ADI), and insurance status, were all associated with readmission risk. Non-Hispanic Black patients were more likely to be readmitted at 30, 60, and 90 days, while Hispanic patients were less likely to be readmitted at all time points, compared to non-Hispanic White patients. However, when mortality and readmission were considered as a composite outcome, Hispanic patients were not at greater risk, which may indicate a survivorship bias among certain subgroups. Likewise, increasing neighborhood disadvantage displayed a clear dose–response relationship to readmission in age-adjusted time-to-event analysis and logistic regression models. While communities of color bore disproportionate COVID-19-related mortality early in the pandemic (32, 33), the demographic proportions of COVID-19 cases, hospitalizations, and deaths have varied widely across each wave of the pandemic (1). The observed associations between race, ethnicity, socioeconomic status, and poor health outcomes are unlikely biological in origin. As COVID-19 transitions into an endemic condition, further research is needed to elucidate the specific barriers to accessing quality, timely care for COVID-19 and to develop interventions to curb preventable readmissions within vulnerable communities.
The readmission rate demonstrated in this study is high relative to the extant literature, especially given the proportion of patients under 50 years of age (34%; 31,267/91,007) and patients with a zero score on the Charlson Comorbidity Index (47%; 42,413/91,007) (34, 35). This gap could be explained by the capacity of the health information exchange to identify encounters across institutions and hospital systems: 26% of readmission encounters were to a different hospital or hospital system from the index hospitalization encounter. Increasing length of stay is often used as a proxy of disease severity at the index encounter (36, 37), but in this study, the length of stay of the index encounter displayed a parabolic effect: readmission risk was highest in patients whose index encounter was either less than 2 days or 10 or more days. These results suggest some patients may have either been discharged prematurely or decompensated quickly after transitioning to outpatient care, possibly due to overburdened hospital and primary care facilities during epidemic peaks.
The breadth and depth of the HIE data facilitated accurate patient tracking across time and between facilities and enabled investigators to correctly determine readmission status, regardless of whether patients returned to the same hospital. Our analyses are further strengthened by the addition of neighborhood-level measures of disadvantage and encounter-specific insurance information. As we utilized neighborhood-level socioeconomic measures that have been normalized across United States national and state populations, our findings will be valuable in comparative analyses across regions. We chose to exclude pregnant patients from readmission analyses, as they likely represent a population of incidentally captured subclinical COVID-19 cases who are inherently at high risk for readmission. However, future studies are needed to investigate COVID-19-related maternal and fetal outcomes, as well as healthcare utilization among pregnant COVID-19 patients. The primary outcome was all-cause readmission; patients with readmissions due to causes unrelated to COVID-19 were likely included in this analysis. Additionally, due to a high number of index encounters with missing discharge disposition data, we analyzed readmission risk for living patients irrespective of discharge status, which may have resulted in the misclassification of some transfer encounters as readmissions. However, the proportion of transferred patients was relatively low (<7%) and consistent with other studies in the region (38, 39). As with all EHR-based research, events occurring outside of the healthcare system, including death outside of a hospital facility, are challenging to collect. While we were able to collect date of death from some patients who expired in the community, some patients who died after leaving their index encounter may have been classified as non-readmissions. Despite these limitations, our study adds to the growing body of evidence characterizing social determinants of COVID-19 healthcare utilization and disease outcomes throughout 3 years of the pandemic.
More than 20% of patients in this large, HIE-based cohort with a COVID-19-associated hospitalization were readmitted within 90 days of their index encounter, demonstrating the lasting impact of COVID-19 infection, especially among members of marginalized communities, and the increasing burden of COVID-19 morbidity on the healthcare system. Multiple investigations throughout the pandemic reported COVID-19 patients suffering substantial and long-lasting health changes, including decreased respiratory and cardiovascular function, ongoing symptoms requiring clinical intervention, and decreased quality of life in the months or even years following even apparently mild COVID-19 episodes (40–42). Our findings further illustrate the ongoing changes in patients’ experiences of COVID-19 over 3 years of the pandemic and emphasize the need for transitional care for COVID-19 patients leaving the hospital. As growing numbers face the specter of long COVID, health authorities must ensure all patients have access to quality care, build trust in the health system among vulnerable populations, and ensure institutions have the capacity to provide care in the post-acute period.
Data availability statementThe datasets presented in this article are not readily available because clinical data cannot be shared publicly because of patient confidentiality concerns as imposed by the University of Texas Health Science Center at Houston Committee for the Protection of Human Subjects. Requests to access de-identified data can be made to cphs@uth.tmc.edu which will be evaluated on a case by case basis in line with institutional policies. Requests to access the datasets should be directed to Committee for the Protection of Human Subjects: cphs@uth.tmc.edu.
Ethics statementThe studies involving humans were approved by the Western Institutional Review Board as a quality improvement study and granted a waiver of informed consent. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation was not required from the participants or the participants’ legal guardians/next of kin in accordance with the national legislation and institutional requirements.
Author contributionsMS: Writing – review & editing, Writing – original draft, Visualization, Formal analysis, Conceptualization. JM: Writing – review & editing, Validation, Data curation. MF: Writing – review & editing, Validation, Data curation. GT: Writing – review & editing, Validation, Data curation, Conceptualization. TC: Writing – review & editing, Supervision, Methodology, Formal analysis. RR: Writing – review & editing, Formal analysis. JH: Writing – review & editing, Supervision, Resources. EB: Writing – review & editing, Writing – original draft, Supervision, Resources, Conceptualization.
FundingThe author(s) declare that financial support was received for the research, authorship, and/or publication of this article. The Southeast Texas COVID cohort was supported by the Cullen Foundation, Cullen Trust for Health Care, 249 Elkins Foundation and John P. McGovern Foundation. The funders of the study had no role in study design, data collection, data analysis, data interpretation, or writing of the report. The corresponding author had full access to all the data in the study and had final responsibility for the decision to submit for publication.
AcknowledgmentsThe authors would like to thank the Cullen Foundation, Cullen Trust for Health Care, Elkins Foundation, and John P. McGovern Foundation for their generous support of the Southeast Texas COVID cohort. We would also like to thank the healthcare institutions of Southeast Texas for their support of treatment, payment and operations-related research.
Conflict of interestThe authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s noteAll claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary materialThe Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2024.1352240/full#supplementary-material
Footnotes References2. Rossen, LM, Branum, AM, Ahmad, FB, Sutton, P, and Anderson, RN. Excess deaths associated with COVID-19, by age and race and ethnicity—United States, January 26–October 3, 2020. Morb Mortal Wkly Rep. (2020) 69:1522–7. doi: 10.15585/mmwr.mm6942e2
PubMed Abstract | Crossref Full Text | Google Scholar
3. Hutchins, HJ, Wolff, B, Leeb, R, Ko, JY, Odom, E, Willey, J, et al. COVID-19 mitigation behaviors by age group—United States, April–June 2020. Morb Mortal Wkly Rep. (2020) 69:1584–90. doi: 10.15585/mmwr.mm6943e4
PubMed Abstract | Crossref Full Text | Google Scholar
4. Schold, JD, King, KL, Husain, SA, Poggio, ED, Buccini, LD, and Mohan, S. COVID-19 mortality among kidney transplant candidates is strongly associated with social determinants of health. Am J Transplant. (2021) 21:2563–72. doi: 10.1111/ajt.16578
PubMed Abstract | Crossref Full Text | Google Scholar
5. MacIntyre, CR, Nguyen, PY, Chughtai, AA, Trent, M, Gerber, B, Steinhofel, K, et al. Mask use, risk-mitigation behaviours and pandemic fatigue during the COVID-19 pandemic in five cities in Australia, the UK and USA: a cross-sectional survey. Int J Infect Dis. (2021) 106:199–207. doi: 10.1016/j.ijid.2021.03.056
PubMed Abstract | Crossref Full Text | Google Scholar
6. Utych, SM, and Fowler, L. Age-based messaging strategies for communication about COVID-19. Journal of Behavioral. Public Adm. (2020) 3:151. doi: 10.30636/jbpa.31.151
Crossref Full Text | Google Scholar
7. Cunningham, JW, Vaduganathan, M, Claggett, BL, Jering, KS, Bhatt, AS, Rosenthal, N, et al. Clinical outcomes in young US adults hospitalized with COVID-19. JAMA Intern Med. (2021) 181:379–81. doi: 10.1001/jamainternmed.2020.5313
PubMed Abstract | Crossref Full Text | Google Scholar
9. Crook, H, Raza, S, Nowell, J, Young, M, and Edison, P. Long covid—mechanisms, risk factors, and management. BMJ. (2021) 374:1648. doi: 10.1136/bmj.n1648
Crossref Full Text | Google Scholar
10. Mohiuddin, MD, and Kasahara, K. Investigating the aggressiveness of the COVID-19 omicron variant and suggestions for possible treatment options. Respir Med. (2022) 191:106716. doi: 10.1016/j.rmed.2021.106716
PubMed Abstract | Crossref Full Text | Google Scholar
12. Sandoval, M, Nguyen, DT, Huang, HJ, Yi, SG, Ghobrial, RM, Gaber, AO, et al. COVID-19 mortality may be reduced among fully vaccinated solid organ transplant recipients. PLoS One. (2022) 17:e0279222. doi: 10.1371/journal.pone.0279222
PubMed Abstract | Crossref Full Text | Google Scholar
13. Ryan, BJ, Coppola, D, Canyon, DV, Brickhouse, M, and Swienton, R. COVID-19 community stabilization and sustainability framework: an integration of the Maslow hierarchy of needs and social determinants of health. Disaster Med Public Health Prep. (2020) 14:623–9. doi: 10.1017/dmp.2020.109
PubMed Abstract | Crossref Full Text | Google Scholar
14. Thakur, N, Lovinsky-Desir, S, Bime, C, Wisnivesky, JP, and Celedón, JC. The structural and social determinants of the racial/ethnic disparities in the US COVID-19 pandemic. What’s our role? Am J Respir Crit Care Med. (2020) 202:943–9. doi: 10.1164/rccm.202005-1523PP
PubMed Abstract | Crossref Full Text | Google Scholar
15. Baker, MC, Alberti, PM, Tsao, TY, Fluegge, K, Howland, RE, and Haberman, M. Social determinants matter for hospital readmission policy: insights from new York City: study examines social determinants and hospital readmissions. Health Aff. (2021) 40:645–54. doi: 10.1377/hlthaff.2020.01742
PubMed Abstract | Crossref Full Text | Google Scholar
16. Grunwell, JR, Opolka, C, Mason, C, and Fitzpatrick, AM. Geospatial analysis of social determinants of health identifies neighborhood hot spots associated with pediatric intensive care use for life-threatening asthma. J Allergy Clin Immunol Pract. (2022) 10:981–991.e1. doi: 10.1016/j.jaip.2021.10.065
Crossref Full Text | Google Scholar
17. Chen, M, Tan, X, and Padman, R. Social determinants of health in electronic health records and their impact on analysis and risk prediction: a systematic review. J Am Med Inform Assoc. (2020) 27:1764–73. doi: 10.1093/jamia/ocaa143
PubMed Abstract | Crossref Full Text | Google Scholar
18. Amrollahi, F, Shashikumar, SP, Meier, A, Ohno-Machado, L, Nemati, S, and Wardi, G. Inclusion of social determinants of health improves sepsis readmission prediction models. J Am Med Inform Assoc. (2022) 29:1263–70. doi: 10.1093/jamia/ocac060
PubMed Abstract | Crossref Full Text | Google Scholar
19. 30-Day Readmission Rates to U.S. Hospitals. Agency for Healthcare Research and Quality. Rockville, MD: Trafo (2018).
20. Wiley, Z, Kulshreshtha, A, Li, D, Kubes, J, Kandiah, S, Leung, S, et al. Clinical characteristics and social determinants of health associated with 30-day hospital readmissions of patients with COVID-19. J Investig Med. (2022) 70:1406–15. doi: 10.1136/jim-2022-002344
PubMed Abstract | Crossref Full Text | Google Scholar
21. Ge, D, Vatson, JS, Andrews, T, Regunathan, A, Nesbitt, D, and Hussain, S. Impact of the pandemic: screening for social determinants of health in the ICU setting. B47 Covid Manag Outcomes. (2022):A2951. doi: 10.1164/ajrccm-conference.2022.205.1
Crossref Full Text | Google Scholar
22. Shapiro, JS, Mostashari, F, Hripcsak, G, Soulakis, N, and Kuperman, G. Using health information exchange to improve public health. Am J Public Health. (2011) 101:616–23. doi: 10.2105/AJPH.2008.158980
PubMed Abstract | Crossref Full Text | Google Scholar
23. Lenert, L, and McSwain, BY. Balancing health privacy, health information exchange, and research in the context of the COVID-19 pandemic. J Am Med Inform Assoc. (2020) 27:963–6. doi: 10.1093/jamia/ocaa039
PubMed Abstract | Crossref Full Text | Google Scholar
24. Charlson, ME, Pompei, P, Ales, KL, and MacKenzie, CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. (1987) 40:373–83. doi: 10.1016/0021-9681(87)90171-8
PubMed Abstract | Crossref Full Text | Google Scholar
25. Charlson, ME, Carrozzino, D, Guidi, J, and Patierno, C. Charlson comorbidity index: a critical review of clinimetric properties. Psychother Psychosom. (2022) 91:8–35. doi: 10.1159/000521288
PubMed Abstract | Crossref Full Text | Google Scholar
26. Quan, H, Li, B, Couris, CM, Fushimi, K, Graham, P, Hider, P, et al. Updating and validating the Charlson comorbidity index and score for risk adjustment in hospital discharge abstracts using data from 6 countries. Am J Epidemiol. (2011) 173:676–82. doi: 10.1093/aje/kwq433
PubMed Abstract | Crossref Full Text | Google Scholar
27. Fortin, SP, Reps, J, and Ryan, P. Adaptation and validation of a coding algorithm for the Charlson comorbidity index in administrative claims data using the SNOMED CT standardized vocabulary. BMC Med Info Decision Making. (2022) 22:1–2. doi: 10.1186/s12911-022-02006-1
Crossref Full Text | Google Scholar
31. Flanagan, BE, Gregory, EW, Hallisey, EJ, Heitgerd, JL, and Lewis, B. A social vulnerability index for disaster management. J Homeland Security Emerg Manag. (2011) 8:792. doi: 10.2202/1547-7355.1792
Crossref Full Text | Google Scholar
32. Sotoodeh Ghorbani, S, Taherpour, N, Bayat, S, Ghajari, H, Mohseni, P, and Hashemi Nazari, SS. Epidemiologic characteristics of cases with reinfection, recurrence, and hospital readmission due to COVID-19: a systematic review and meta-analysis. J Med Virol. (2022) 94:44–53. doi: 10.1002/jmv.27281
PubMed Abstract | Crossref Full Text | Google Scholar
33. Lavery, AM, Preston, LE, Ko, JY, Chevinsky, JR, DeSisto, CL, Pennington, AF, et al. Characteristics of hospitalized COVID-19 patients discharged and experiencing same-hospital readmission—United States, march–august 2020. Morb Mortal Wkly Rep. (2020) 69:1695–9. doi: 10.15585/mmwr.mm6945e2
PubMed Abstract | Crossref Full Text | Google Scholar
34. Vahidy, FS, Drews, AL, Masud, FN, Schwartz, RL, Boom, ML, and Phillips, RA. Characteristics and outcomes of COVID-19 patients during initial peak and resurgence in the Houston metropolitan area. JAMA. (2020) 324:998–1000. doi: 10.1001/jama.2020.15301
PubMed Abstract | Crossref Full Text | Google Scholar
35. Mude, W, Oguoma, VM, Nyanhanda, T, Mwanri, L, and Njue, C. Racial disparities in COVID-19 pandemic cases, hospitalisations, and deaths: a systematic review and meta-analysis. J Glob Health. (2021) 11:11. doi: 10.7189/jogh.11.05015
Crossref Full Text | Google Scholar
36. Horn, SD, Sharkey, PD, Buckle, JM, Backofen, JE, Averill, RF, and Horn, RA. The relationship between severity of illness and hospital length of stay and mortality. Med Care. (1991) 29:305–17. doi: 10.1097/00005650-199104000-00001
Crossref Full Text | Google Scholar
37. Iuliano, AD, Brunkard, JM, Boehmer, TK, Peterson, E, Adjei, S, Binder, AM, et al. Trends in disease severity and health care utilization during the early omicron variant period compared with previous SARS-CoV-2 high transmission periods—United States, December 2020–January 2022. Morb Mortal Wkly Rep. (2022) 71:146–52. doi: 10.15585/mmwr.mm7104e4
留言 (0)