Disclaimer: Early release articles are not considered as final versions. Any changes will be reflected in the online version in the month the article is officially released.
Author affiliations: Centers for Disease Control and Prevention, Atlanta, Georgia, USA (F.A. Tobolowsky, Z. Gilani, J.F. Gidudu); African Field Epidemiology Network, Kampala, Uganda (F. Nsubuga); Uganda National Expanded Program on Immunizations, Kampala (F. Nsubuga, D. Kyabayinze); World Health Organization, Kampala (A. Kisakye); National Drug Authority, Kampala (H. Ndagije)
To eliminate the risk for vaccine-related paralysis, live attenuated Sabin-strain oral poliovirus vaccine type 2 was withdrawn from routine use in a globally coordinated manner in 2016. However, because of decreased population immunity (1) and pathogenic reversion of vaccine virus persisting in communities or introduced during outbreak response vaccinations, circulating vaccine-derived poliovirus type 2 outbreaks have emerged across the World Health Organization (WHO) African Region, particularly during 2019‒2021 (2–4). In November 2020, to reduce the risk for new type 2 emergences, WHO granted Emergency Use Listing of a more genetically stable vaccine, novel oral poliovirus vaccine type 2 (nOPV2) (BioFarma, https://www.biofarma.co.id). Initial use began in March 2021 in a limited number of qualifying countries and subsequently expanded (3,5; https://extranet.who.int/pqweb/vaccines/polio-vaccine-novel-oral-nopv-monovalent-type-2).
Full vaccine licensure requires robust safety data and postdeployment monitoring (6). Although initial phase 1 and 2 clinical trials demonstrated that nOPV2 is well tolerated, those studies enrolled a small number of persons and were unlikely to detect rare adverse events; safety data were only collected actively for 7 days after vaccination (7,8). During initial use, passive and active safety surveillance implementation was not standardized, and data gaps persisted. In October 2021, after early promising safety data in large-scale use, nOPV2 rollout was expanded as recommended by the WHO Strategic Advisory Group of Experts on Immunization (9).
In response to 2 confirmed detections of circulating vaccine-derived poliovirus type 2 in Uganda in November 2021, a nationwide supplemental immunization activity using nOPV2 was planned for children <5 years of age. To further clarify the safety profile of nOPV2, we designed a multipronged safety evaluation using the passive surveillance system in Uganda, active hospital-based surveillance, acute flaccid paralysis (AFP) surveillance, and a cohort event monitoring system to monitor for adverse events following immunization (AEFI) and adverse events of special interest (AESI).
We conducted a safety evaluation in Uganda after the first round of the nationwide supplemental immunization activity in January 2022. We used the country’s passive safety surveillance system to identify AEFI from any data source (e.g., telephone call, short messaging service, Open Data Kit, District Health Information System 2). We conducted active hospital-based surveillance for AESI in 18 sentinel sites. We included events that occurred within 42 days after vaccine administration (10). We defined AEFI as any untoward medical occurrence after immunization that did not necessarily have a causal relationship with the use of the vaccine (11). We defined AESI as prespecified medically significant events that have the potential to be causally associated with a vaccine product that needs to be carefully monitored and confirmed by further special studies (https://polioeradication.org/wp-content/uploads/2022/06/nOPV2-AESI-surveillance.pdf). AESI included anaphylaxis, aseptic meningitis or encephalitis, acute disseminated encephalomyelitis, Guillain-Barré syndrome/Fisher’s syndrome, myelitis/transverse myelitis, AFP, and unexplained deaths. We used the Brighton Collaboration case definitions for validation of cases (https://brightoncollaboration.us/category/pubs-tools/case-definitions) before causality assessment by an independent national AEFI committee. We recorded vaccination status by finger marking or verbal recall for events and cases.
AFP surveillance is ongoing in Uganda through passive, active, and community-based systems. AFP was defined as limb weakness in a child <15 years of age reported during and after the nOPV2 campaign to a surveillance officer or clinician; suspected cases were investigated and adjudicated by the national polio expert committee. We included AFP cases in children <5 years of age with symptom onset <42 days after nOPV2 administration.
We developed a cohort event monitoring system to prospectively monitor children for any AEFI occurring after vaccine administration. We systematically selected households in designated enumeration areas to create a nationally representative sample. We offered enrollment for all eligible children in each household; eligible children were those 0–59 months of age who had been vaccinated with the first dose of nOPV2 in the supplemental immunization activity, who would reside in the selected community for >42 days after the initial nOPV2 vaccination, who had written informed caregiver consent, who demonstrated no acute signs or symptoms at the time of vaccination, and who had a caregiver with access to a telephone. We followed vaccinated children through telephone interviews with caregivers starting on the day of vaccine administration (day 0) and on days 3, 7, 14, 28, and 42. Caregivers reported any signs or symptoms by onset date; healthcare-seeking behavior and hospitalizations were recorded. We combined and harmonized data from all 4 surveillance systems to identify any duplication.
We defined a nonspecified serious event as an event that resulted in death, required hospitalization, or resulted in persistent or major disability (11). For any serious event, clinicians and healthcare workers conducted detailed investigations, and the National AEFI Causality Committee of country experts used the clinical data provided to classify each event for association into 5 categories, according to global guidelines: vaccine product–related, vaccine quality–related, immunization error–related, immunization anxiety–related, indeterminate, or coincidental (12). We completed descriptive data analyses using Excel (Microsoft, https://www.microsoft.com) and SAS version 9.4 (SAS Institute, Inc., https://www.sas.com). The protocol received a nonresearch determination by the Uganda AIDS Support Organization Research Ethics Committee and the Uganda National Council of Science and Technology; this activity was reviewed by the Centers for Disease Control and Prevention and was conducted consistent with applicable federal law and center policy (see e.g., 45 C.F.R. part 46.102(l) (2), 21 C.F.R. part 56; 42 U.S.C. §241(d); 5 U.S.C. §552a; 44 U.S.C. §3501 et seq.).
Figure
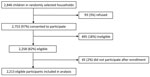
Figure. Cohort event monitoring enrollment after novel oral poliovirus vaccine type 2 administration, Uganda, 2022. Ineligible children included those who were >59 months of age, demonstrated acute signs or symptoms at...
In the first round of the nationwide vaccination campaign in Uganda during January 14‒21, 2022, a total of 9,768,697 doses of nOPV2 were administered to children <5 years of age. During January 14–March 11, 2022, an initial total of 1,159 AEFI were identified across all 4 safety surveillance systems (Table). Passive surveillance identified 43 AEFI; 2 (5%) of those events were serious. Through prospective active hospital-based surveillance, 8 AESI were detected; in 5 (62.5%) of those events, patients reported that they had received nOPV2 vaccination within 42 days. Among 159 AFP cases in children <5 years of age identified through the country’s active AFP surveillance, 128 (80.5%) patients reported nOPV2 receipt, and 81 (50.9%) cases were defined as serious events after investigation. Cohort event monitoring enrolled 2,213 participants (Figure); during follow-up, we found 952 AEFI, of which 22 (2%) were serious. Of the 110 conditions that were classified as serious, 6 (5.5%) were classified into the vaccine product–related reactions category, diagnosed as gastroenteritis (n = 3), acute disseminated encephalomyelitis (n = 1), encephalitis (n = 1), and acute febrile illness (n = 1).
Through the multipronged surveillance system, ≈6% of serious conditions were classified by the causality committee as vaccine product–related reactions; no concerning safety signals were noted. Previous data reported from countries using nOPV2 support this finding; a similar proportion (60/1529; 4%) of events were classified as vaccine product–related reactions, and no major safety concerns have been identified outside of this evaluation in phase 3 trials (13–15).
The first limitation of this evaluation is that AEFI identified through passive surveillance were likely underreported. Conversely, soliciting events through caregivers during cohort event monitoring and active AFP surveillance might have led to overreporting. Recall bias could have occurred with reported vaccination status and in cohort event monitoring, especially with later timepoints after vaccination. Last, the COVID-19 pandemic led to delays in implementation, investigations, and timely review of conditions by the causality committee.
Our evaluation adds to the growing evidence that no safety signals are associated with nOPV2 use among persons <5 years of age. With a robust multipronged approach, safety surveillance can be strengthened for vaccines with limited safety profiles that are introduced in resource-limited settings during public health emergencies, especially while awaiting full licensure.
Dr. Tobolowsky is a Future Leaders in Infections and Global Health Threats (FLIGHT) officer and medical epidemiologist in the Global Immunization Division, Global Health Center, Centers for Disease Control and Prevention. Her primary research interests include the epidemiology of and outbreak response for communicable diseases of public health importance.
留言 (0)