Primary pericardial mesothelioma is a neoplastic proliferation of mesothelial cells of pericardial origin and is responsible for a fraction of mesotheliomas.1 It is an extremely rare tumour with a prevalence of about 0.0022% in an autopsy series.2 Unlike pleural mesotheliomas, which have a strong relation with exposure to asbestos, pericardial mesotheliomas do not show such association; with only 14% of patients reporting exposure to asbestos. Patients with pericardial mesothelioma can have varied presentations including pericarditis, pericardial effusion with cardiac tamponade, congestive cardiac failure and conduction disturbances.3
THE CASEA middle-aged man with diabetes and hypertension presented with dry cough and dyspnoea for 6 months, initially, New York Heart Association Class II, which progressed to Class III. The patient had a coronary angiogram done about a year before presentation in view of a positive stress test and was noted to have normal epicardial coronaries. The patient had no previously diagnosed respiratory ailments. The patient did not smoke and had no occupational or incidental exposure to asbestos or other carcinogens. He had no previously diagnosed malignancy and no history of having received radiation therapy in the past. The patient’s medications included telmisartan, cilnidipine, metformin and insulin. The patient had received symptomatic treatment for the cough and dyspnoea; however, his symptoms persisted. Six months after his symptoms began, a moderate-to-large pericardial effusion was detected on computed tomography and was referred to us for further management.
On examination, the patient had a regular pulse of 100 beats/ minute and blood pressure was 130/80 mmHg. Jugular venous pressure was elevated with minimal bilateral pitting pedal oedema. Initial evaluation showed a normal electrocardiogram and cardiomegaly on chest X-ray (Fig. 1). An echocardiogram done showed a large pericardial effusion (Fig. 2) with a mass within the pericardial cavity (Fig. 3). The mass was lobulated with cystic areas and was seen predominantly over the lateral aspect of the heart. The patient gave no history of fever or weight loss. Clinically, there was no evidence of cardiac tamponade, and pericardiocentesis was deferred until further evaluation. The patient was then subjected to cardiac MRI, which showed a large pericardial mass predominantly arising from the visceral pericardium with few parietal pericardial deposits (Fig. 4). There were areas of focal non-ischaemic pattern of enhancement in the myocardium suggestive of possible infiltration by the tumour. The patient later underwent a positron emission tomography/ computed tomography to look for any other source of primary or metastasis. It revealed an intense fluorodeoxyglucose avid ill-defined hypodense lesion in the pericardial region with gross pericardial effusion and involvement of mediastinal lymph nodes. There was no evidence of tumour anywhere else.
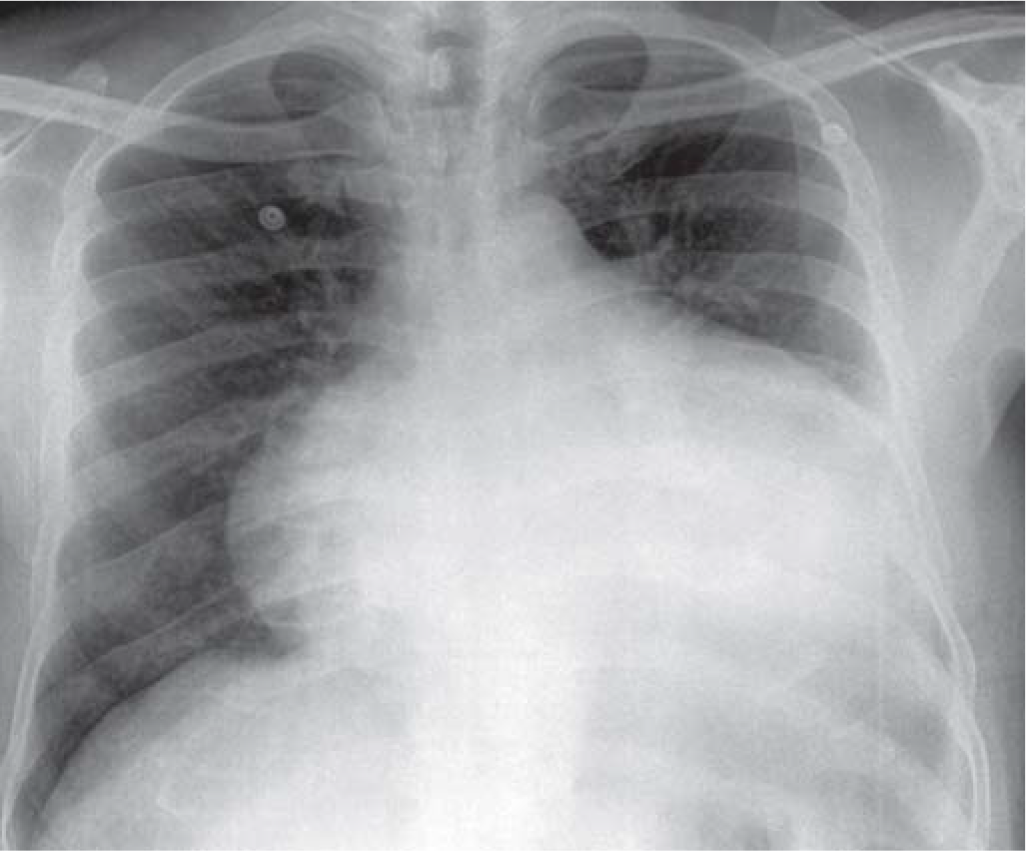
FIG 1.: Chest X-ray showing gross cardiomegaly
Export to PPT
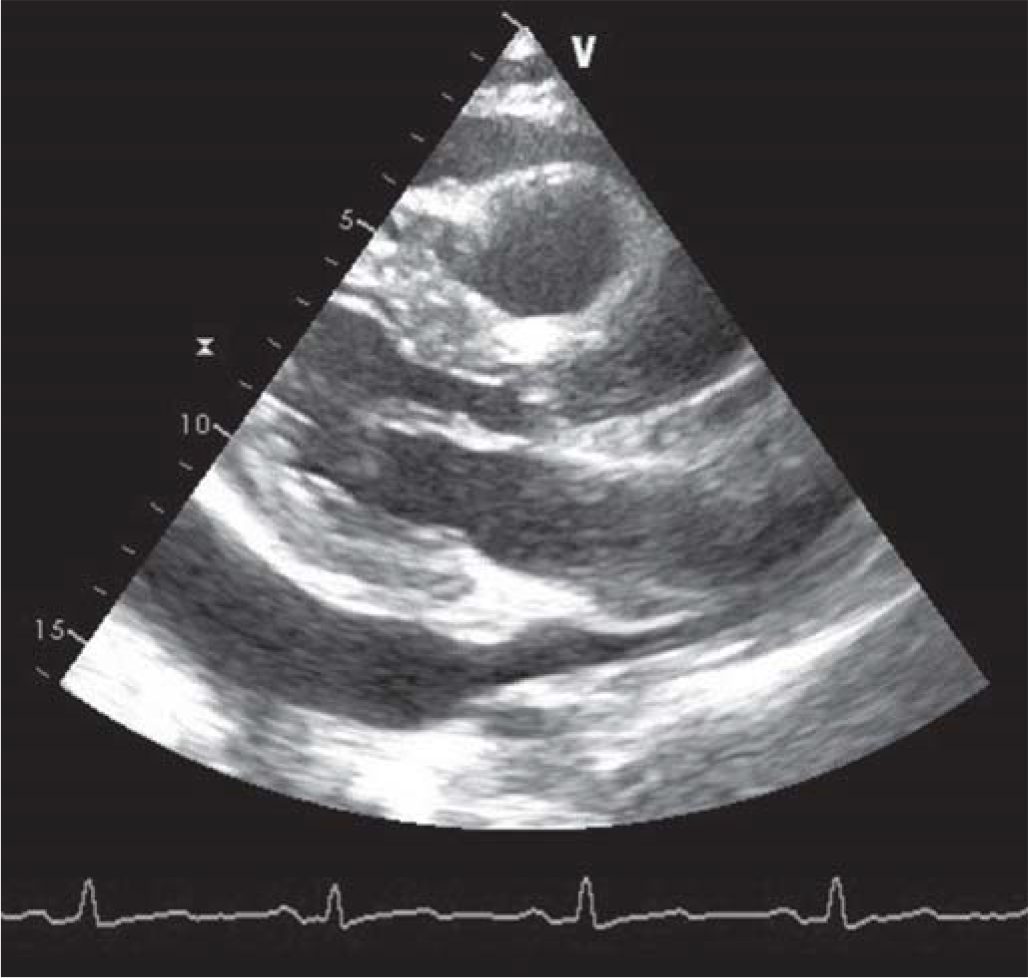
FIG 2.: Large pericardial effusion
Export to PPT
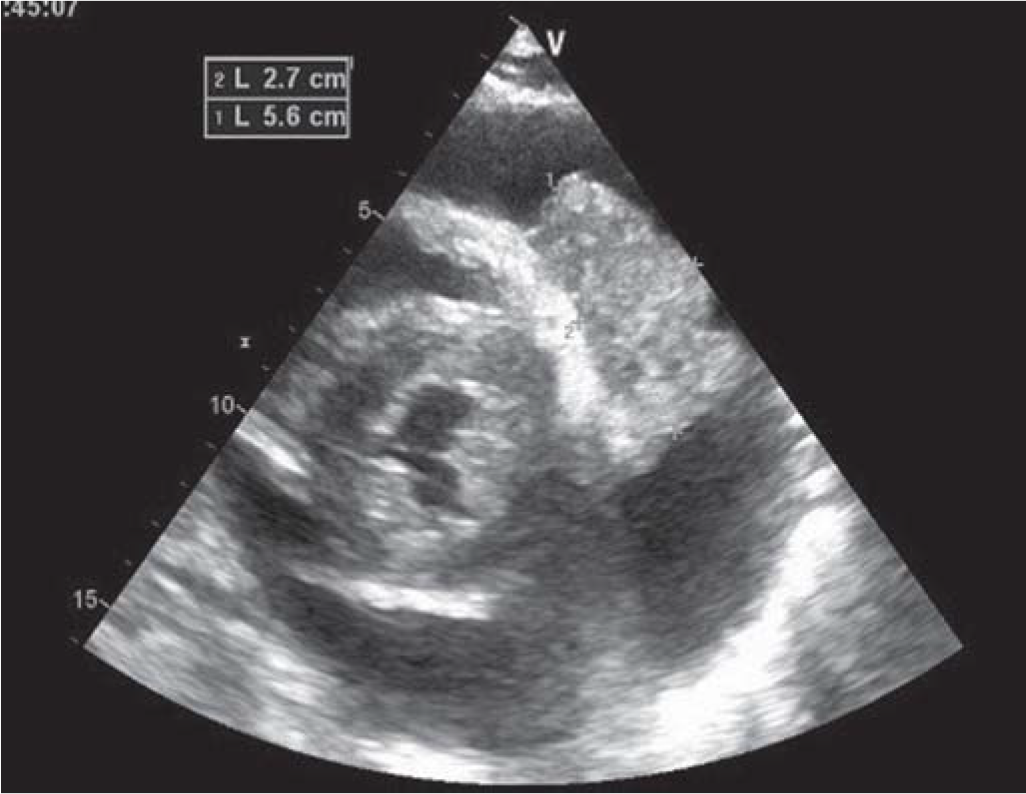
FIG 3.: Mass in pericardial cavity
Export to PPT
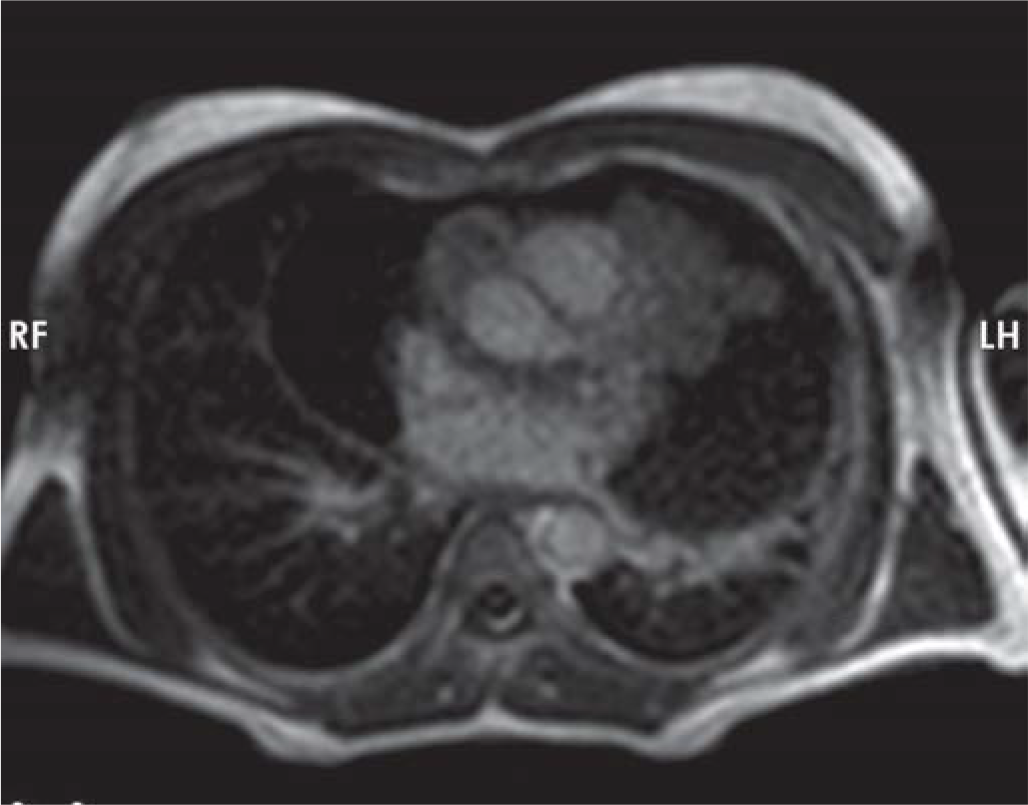
FIG 4.: Cardiac MRI showing the mass encasing the vessels
Export to PPT
The patient was then taken up for pericardiectomy and an open biopsy was done (Fig. 5). Histopathological examination of the tissue revealed a neoplasm with cells arranged in sheets and patternless configuration. Multiple tumour giant cells were observed interspersed with large areas of necrosis. Immunohistochemistry revealed that the neoplastic cells were positive for CK5/6, calretinin, Bcl2, vimentin, and negative for cytokeratin, smooth muscle actin, CD31, s100, desmin, epithelial membrane antigen and CD 117. With the above pattern, a diagnosis of mesothelioma arising from the pericardium was made. Based on the above diagnosis, the patient was started on chemotherapy with pemetrexed and carboplatin three weekly regimens. However, the patient succumbed to the illness about 7 months after diagnosis.
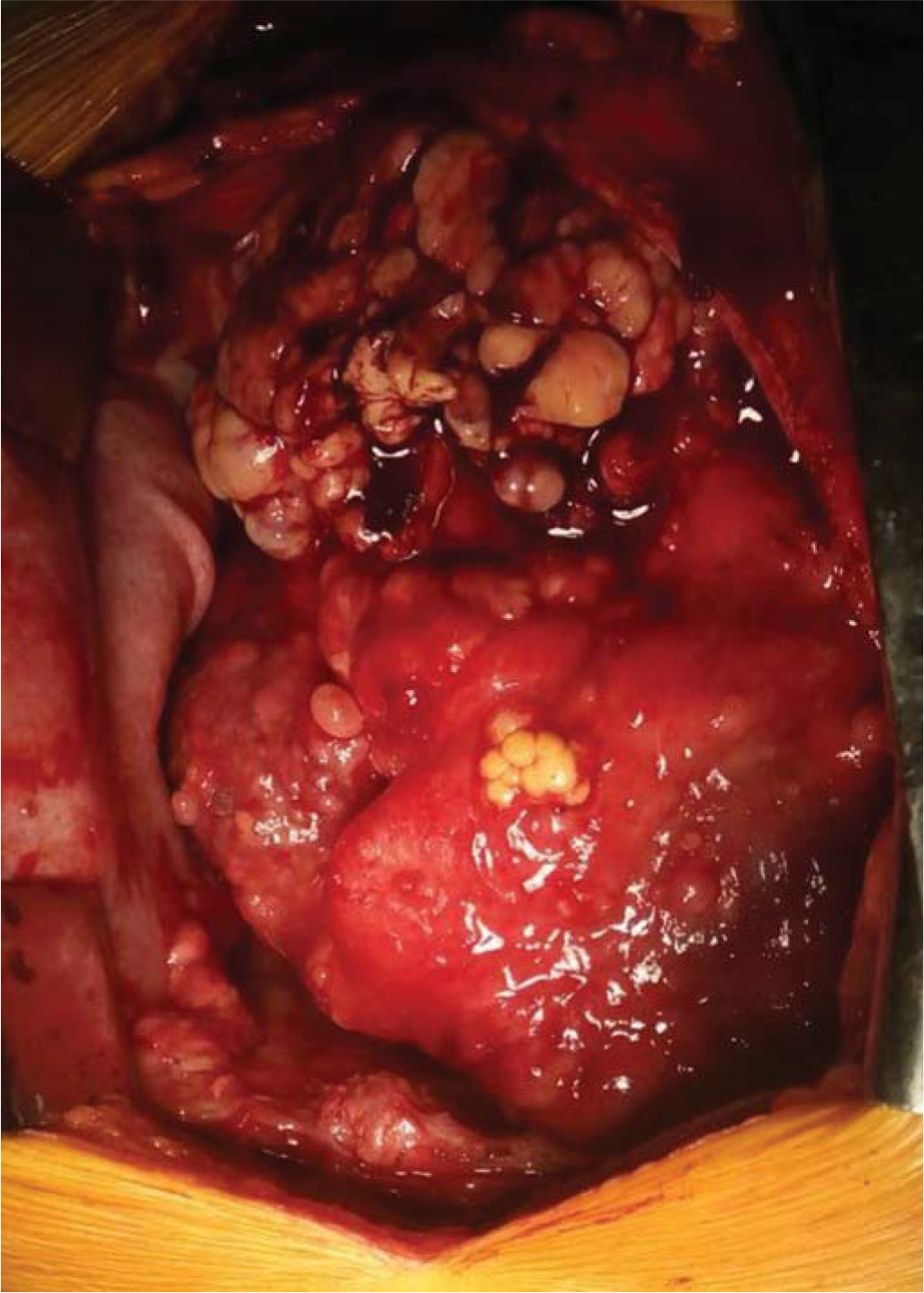
FIG 5.: Intraoperative image of the mass within the pericardium
Export to PPT
DISCUSSIONPrimary pericardial mesothelioma is an extremely rare tumour with preponderance among men. The preponderance among men is 2:1 in pericardial mesotheliomas compared to 3.5:1 in pleural mesotheliomas.4 Mesotheliomas are tumours arising from the mesothelial lining seen in the pleura, pericardium, peritoneum or testes. Pericardial mesotheliomas contribute only 0.7% of the cases, while the majority of the cases are from the pleural cavity.5 The aetiology of pericardial mesotheliomas remains unclear. There has been no definitive correlation between asbestos exposure and pericardial mesotheliomas, unlike pleural and peritoneal mesotheliomas. The relative rarity of pericardial mesotheliomas is partly responsible for the inability to establish a definitive aetiological role for asbestos. One patient developed pericardial mesothelioma 15 years after he underwent pericardial dusting with asbestos.6 Hence, the role of asbestos cannot be completely ruled out. The role of Simian virus 40 as a possible aetiological factor has also been studied.
Patients with malignant pericardial mesothelioma have been reported in a broad age range of 2–78 years with the mean age at diagnosis being 46 years. It is generally difficult to diagnose, given its non-specific symptoms and signs. Patients may present with dyspnoea, chest pain, heart failure, features of constrictive pericarditis, pericardial effusion or cardiac tamponade.7 Our patient had cough and dyspnoea for 6 months before diagnosis. Adequate evaluation, especially if symptoms are not responding to usual treatment, is of importance.
Anderson and Hansen proposed criteria to diagnose malignant primary pericardial mesothelioma. These included: localization of the tumour in the pericardial sac, metastasis only to a lymph node, no other tumour and complete autopsy to be done in case of death.8
The differential diagnosis between pericardial mesotheliomas and other primary or secondary malignancies of the pericardium is difficult owing to their similar appearance and clinical presentation. A common benign pericardial lesion is a pericardial cyst. Pericardial lipoma, fibroma and haemangiomas are some of the benign tumours commonly encountered in the pericardium. Among malignant tumours, metastases to the pericardium are seen more commonly than primary tumours. The most common primary pericardial tumour is pericardial mesothelioma followed by pericardial sarcoma, pericardial lymphoma, epithelioid angiosarcoma, adenomatoid tumour among others. The pericardium is a common site for secondaries from the breast, lung and melanoma. Tuberculous pericarditis should be considered in all patients with blood-stained pericardial fluid.
Histologically, the tumour may be epithelial, sarcomatoid or mixed type. Mixed type is the most common constituting over 75% of cases. Metastasis may be seen in 30%–50% of cases and are generally of the regional lymph nodes.
Pericardial mesothelioma has a poor prognosis and various modalities of treatment such as surgery, radiotherapy and chemotherapy have been used with minimal benefits.9 Prognosis is generally poor, as 50%–60% of patients succumb to the illness within 5–6 months. This calls for a high index of suspicion and early recognition and prompt treatment of this highly malignant neoplasm.
In most patients, palliation would be the main strategy of management, and care should be taken to keep diagnostic procedures to a minimum and as non-invasive as possible, and also intervening only to alleviate patients’ symptoms and improve quality of life. We can consider percutaneous balloon pericardiotomy or instillation of chemotherapeutic agents such as cisplatin or bleomycin into the pericardial space to reduce the accumulation of pericardial effusion as a palliative procedure.10
留言 (0)