The term “danger signs” refers to any symptoms or indicators that suggest a pregnant woman may be at risk during pregnancy. They are referred to as obstetric danger signs (ODS) and include symptoms such as loss of consciousness, persistent vomiting, severe persistent abdomen pain, vaginal bleeding, swelling of the face, fingers, and feet, blurred vision, severe recurring frontal headache, and high-grade fever (1, 2).
Every pregnant woman is at risk of experiencing unanticipated, sudden problems related to ODS (1, 3). Pregnancy and its related complications remain one of the major causes of maternal morbidity and mortality worldwide, with over half a million women dying each year due to pregnancy-related causes. Almost all of these (87%) maternal deaths occur in low-income countries (3, 4). Direct obstetric factors, such as severe bleeding, pregnancy-induced hypertension, unsafe abortion, labor and delivery difficulties, and maternal infections, account for approximately 73% of all maternal deaths (3).
Developing countries experience a maternal mortality rate that is 15 times higher than that of developed countries, and the global burden of maternal mortality is concentrated in these regions, with sub-Saharan Africa accounting for 56% of all reported maternal deaths (5). Maternal mortality remains a significant public health concern in low- and middle-income countries, particularly in sub-Saharan Africa, where Ethiopia is located. One of the most effective strategies for reducing maternal mortality is the early identification and management of obstetric danger signs, which are critical indicators of potential complications during pregnancy, childbirth, and the postpartum period (6). Timely recognition of obstetric danger signs allows for prompt intervention, preventing life-threatening complications such as preeclampsia, obstructed labor, and hemorrhage (7).
The Sustainable Development Goal 3 (SDG 3) aims to reduce the global maternal mortality ratio to less than 70 per 100,000 live births by 2030. In addition to this target, each country has the responsibility and commitment to achieve a target of no more than 140 maternal deaths per 100,000 live births (8, 9). Although the maternal mortality ratio is decreasing globally, its reduction in sub-Saharan countries is occurring at a much slower rate. According to the 2019 Ethiopia Demographic Health Survey (EDHS) mini-report, the maternal mortality and morbidity ratio in Ethiopia was 402 per 100,000 live births. Of these deaths, 30% were related to obstetrical danger signs during pregnancy (4).
Maternal mortality remains a critical health challenge in Ethiopia, particularly in rural areas where access to healthcare services is limited. One of the key factors contributing to the high maternal mortality rate is the delay in recognizing and responding to obstetric danger signs. These signs serve as early warning of potential complications during pregnancy, childbirth, and the postpartum period (10).
In the majority of developing countries, including Ethiopia, the underlying cause of maternal death during pregnancy is attributed to three crucial delays, even when ODS occur: delay in identifying danger signs and making the decision to visit the health facility, delay in reaching the health facility, and delay in receiving appropriate and adequate care at the health facility (1, 2).
The majority of women in Ethiopia have a low social status, and the decision-making power regarding access to and use of care is dominated by men. This factor can significantly contribute to adverse pregnancy outcomes (11, 12). A study conducted by Mbizvo and Say analyzed the factors that reduced maternal mortality in Bangladesh, Morocco, and Rwanda. The findings revealed that maternal mortality rates decreased by 20–50% through increased skilled birth attendance and efforts to educate husbands about obstetric danger signs (30).
Several studies conducted in various regions of Africa (including Nigeria, Tanzania, Kenya, and Ethiopia) showed that male partners had a low level of knowledge about obstetric danger signs during pregnancy and childbirth. Only 22.4 to 56.2% of them were able to identify at least two or more of the listed danger signs (2, 13–15).
When husbands fail to recognize the danger signs during pregnancy, it can affect the health of both the mother and the fetus, leading to conditions such as anemia, infections, prematurely ruptured membranes, neonatal morbidity and mortality, abortion, antepartum hemorrhage, and illness or death of the mothers (5, 16). Moreover, a lack of knowledge regarding obstetric danger signs is associated with a delay in the utilization of skilled care, which contributes to an increase in maternal mortality and morbidity (17).
Husbands, particularly in rural Ethiopia, play a key role in influencing the first two delays. As primary decision-makers in many households, they are often responsible for determining when and whether their wives should seek medical care during pregnancy and childbirth (18). If husbands lack knowledge about obstetric danger signs, such as severe vaginal bleeding, convulsions, and prolonged labor, it can lead to significant delays in recognizing complications and deciding to seek timely care, thereby contributing to poor maternal and neonatal outcomes (10).
The World Health Organization (WHO) advocates for the inclusion of men in maternal health strategies as their participation can lead to better care-seeking behaviors, timely interventions, and improved overall maternal well-being (19). Limited awareness of obstetric danger signs among husbands contributes to delays in seeking care, which is a known factor in increasing the risk of maternal mortality in rural Ethiopia. However, maternal deaths are influenced by multiple factors (10, 19).
In Ethiopian cultural practices, men are at the top of the decision-making hierarchy, including decisions regarding the healthcare of their spouses. Therefore, they become a major factor in determining where, when, why, and how many pregnant women can access antenatal care, delivery services, and postpartum care. Husbands’ knowledge of obstetric danger signs, such as severe headache, severe bleeding, convulsions, and prolonged labor, can directly impact the timeliness of seeking care. Husbands with insufficient knowledge of obstetric danger signs may fail to recognize when their wives are in need of urgent medical attention, leading to delays that could result in adverse maternal or neonatal outcomes.
Various studies have been conducted in Ethiopia on male involvement during pregnancy. Despite the acknowledged importance of male involvement in maternal health, there is limited research on husbands’ knowledge of obstetric danger signs. In addition, there is still considerable variation in the variables studied, and no research has been conducted specifically in rural districts such as Raya Kobo.
This study aimed to assess husbands’ knowledge of obstetric danger signs in the Raya Kobo district and to identify the factors associated with this knowledge. Understanding these factors can guide public health interventions aimed at improving male engagement in maternal health and help design targeted educational programs to increase husbands’ awareness of obstetric danger signs, ultimately reducing delays in care-seeking and improving maternal outcomes.
Therefore, incorporating variables, such as distance from nearby health facilities, and sources of information would help assess husbands’ knowledge of obstetric danger signs and the associated factors in the Raya Kobo district.
Methodology Study areaThis study was conducted in the Raya Kobo district, North Wollo Zone, Amara Regional state, Ethiopia, which is 570 Km away from Addis Ababa, the capital city of Ethiopia, and 409 km from Bahir Dar, the capital of the regional state. According to the 2007 Census conducted by the Central Statistical Agency (CSA) of Ethiopia, the district had a total population of 221,958. There were 2,659 pregnant women in the district. The district consists of 37 rural and five urban kebeles. It has 1 hospital, 7 health centers, and 42 health posts. Each health post has two health extension workers (HEWs) (20).
Study design and periodA community-based cross-sectional study was conducted from 29th April to 30th May 2023.
ParticipantsThe source population included all husbands living in the Raya Kobo district whose wives were pregnant or had given birth within the 12 months prior to the study period. The study population consisted of all husbands living in the selected 11 kebeles whose wives were pregnant or had given birth within the 12 months prior to the study period.
Eligibility criteriaInclusion criteria: all husbands living in the Raya Kobo district for 6 months and above were included in this study.
Exclusion criteria: husbands who were critically ill and unable to participate in the interview during the data collection period were excluded from the study.
Sample size determinationThe sample size was determined using a single population proportion formula based on the levels of husbands’ knowledge (p = 44%) from a previous study in the Amara region’s Andede district (35). The sample size was calculated as follows:
vn1=Za/22p.qd2=z2x1−pd2=1.962∗0.44∗0.56/0.052=379
Considering a 1.5 design effect and a 10% non-response rate, the total sample size was calculated to be 626.
The second largest sample size was calculated using EP Info V.7, with a maximum result of 189. Therefore, the overall final sample size was determined by considering the first objective, which was 379, a 1.5 design effect, and a 10% non-response rate, resulting in a total sample size of 626.
Sampling technique and procedureA multi-stage stratified random sampling technique was used to select participants. The district was divided into urban and rural areas, with nine kebeles selected from the rural area and two kebeles from the urban area using random sampling and considering a minimum sample size of 25%. Data on husbands whose wives were pregnant or had given birth within the past 12 months were collected through a survey before the actual data collection. Husbands of mothers who were single, divorced, or widowed in the selected kebeles were excluded from the study. After determining the number of participants, the sample size for each kebele was proportionally allocated, and eligible women were selected using a systematic sampling technique. The interval was determined by dividing the total number of eligible women in the study area, which was estimated to be 1,337, by the sample size of 626, resulting in an interval of 2 (K=N/n, 1,337/626 = 2). The eligible women were initially selected using the lottery method from a list of folders, and after selecting these women, the researchers then proceeded to approach their husbands to administer the questionnaire (Figure 1).
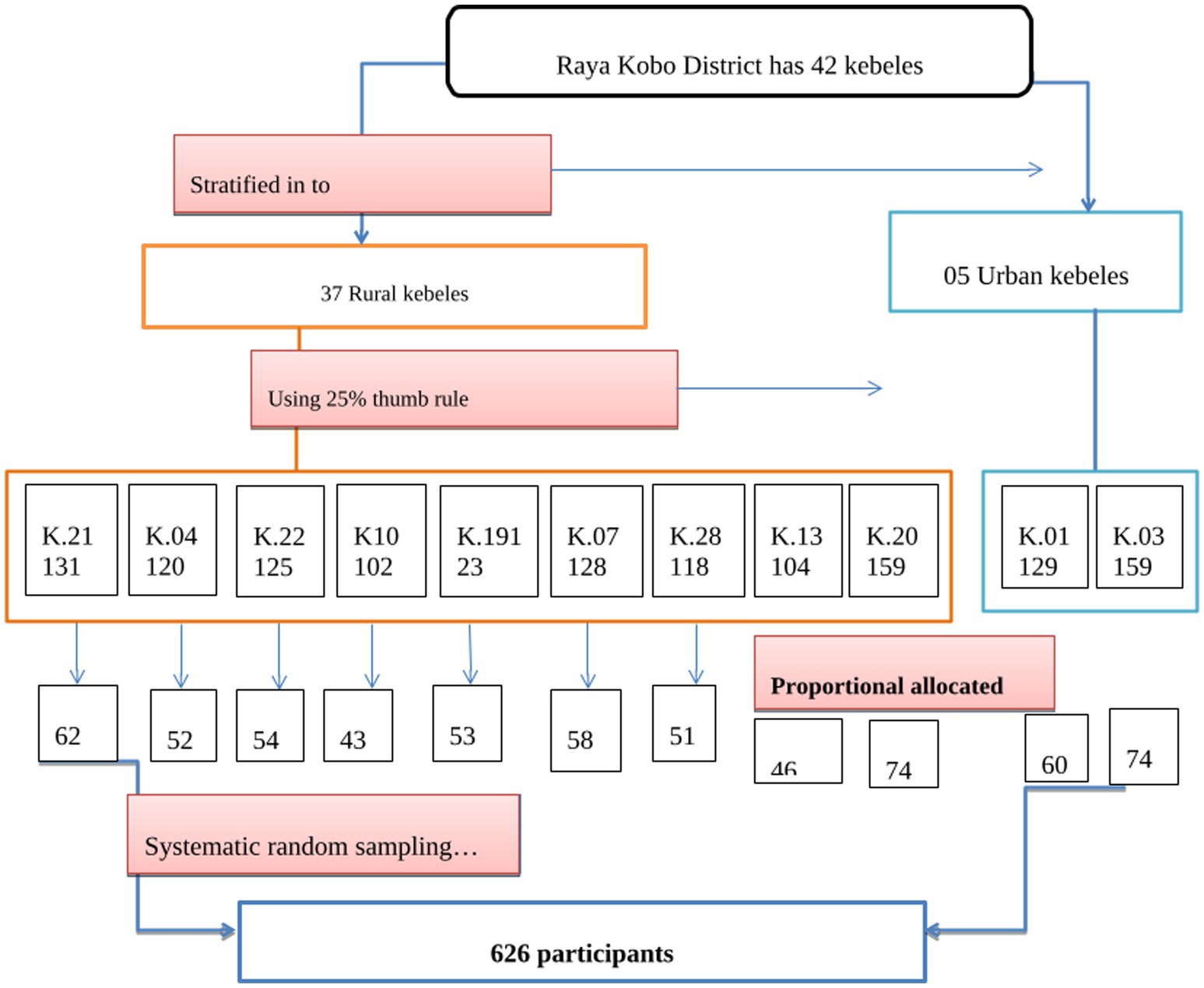
Figure 1. Schematic presentation of the sampling procedure.
Data collection methodData were collected using face-to-face interview techniques and structured questionnaires adapted from various studies (19, 21). The information collected included sociodemographic and economic characteristics (maternal age, husband’s age, residence, income, educational status of the woman/husband, and occupational status), infrastructure (availability of health facilities and distance from a health facility), obstetrical characteristics (gravidity, parity, and place of delivery), and husbands’ awareness of danger signs of obstetric complications at three stages. A total of eight female HEWs and three BSc midwifery graduates were hired as data collectors and were supervised by two MPH students.
Dependent variable: the dependent variable was the husbands’ knowledge of obstetric danger signs.
Independent variables: the independent variables included sociodemographic and socioeconomic characteristics (maternal age, husband’s age, residence, educational status of the woman/husband, occupational status of the woman/husband, and family income), obstetrical characteristics (gravidity, parity, place of delivery, previous history of danger signs, and male involvement in antenatal care (ANC) follow-up), infrastructure (availability of health facilities and distance from a health facility), and sources of information (radio, TV, decision-making by the husband, and health professionals).
Husbands’ good knowledge of obstetrical danger signs: this refers to men who responded to 26 questions about obstetric danger signs during any of the three phases (pregnancy, childbirth, or the post-partum period) and scored above or equal to the median score (20, 22).
Data processing and analysisEach completed questionnaire was checked manually for completeness before data entry. The data were coded and entered into EpiData (V.4.6), cleaned to check for accuracy and consistency, and any errors identified were corrected. The final data were exported to SPSS (IBM-26) for further cleaning and analysis. Logistic regression was performed, and the variables with a 95% CI and a p-value of <0.05 were considered significant. The strength of the statistical association was determined by the adjusted odds ratio (AOR) and 95% CI. The assumptions of multiple logistic regression were fulfilled, and the goodness of fit was tested using the Hosmer–Lemeshow statistical test (0.12). Multicollinearity was assessed based on the maximum number of variables. The important findings’ frequencies, proportions, means, and standard deviations were summarized and presented using tables, figures, and narratives.
Data quality assuranceTo maintain the data quality, a reliability test was performed using Cronbach’s α, which yielded a value of 0.787. A validity test was conducted by a senior expert, and the Pearson correlation coefficient was calculated using SPSS software. Data collectors received training to further uphold the quality of data. A pretest was conducted on 5% of the study participants from a similar population in the Guba Lafto district, located outside the study area. Based on the pretest feedback, some questions were rephrased and inappropriate skipping patterns were corrected. The questionnaires were initially prepared in English, then translated into Amharic (the national language), and subsequently translated back into English by two different language experts to ensure consistency and clarity.
Results Sociodemographic and socioeconomic characteristics of the husbandsData collection was planned for 626 participants, and 620 completed the interviews, resulting in a resonse rate of 99.04%. The mean age of the respondents was 34.68 (SD ± 6.46) years. A total of 270 (43.5%) respondents were between the ages of 26 and 35 years. Among the study participants, 209 (33.7%) had primary education, while only 55 (8.9%) had attended college or higher education. A total of 408 (65.8%) respondents lived in rural areas (Table 1).
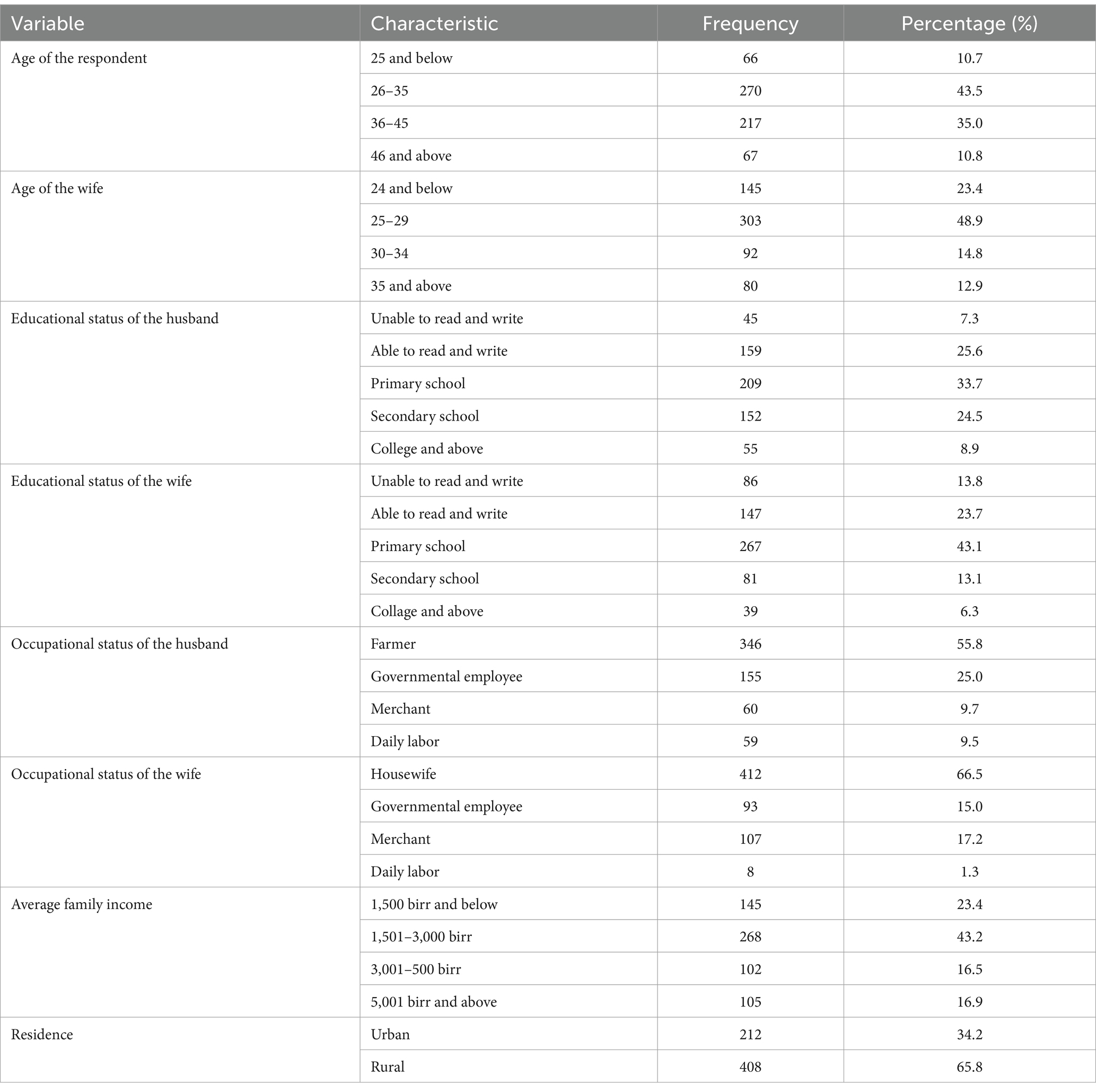
Table 1. Distribution of the respondents and their wives by socio-demographic and economic characteristics in the Raya Kobo district, April 2023 (n = 620).
Obstetric characteristics of the respondentsThe obstetric characteristics of the respondents were determined based on the condition of their wives, as reported by the husbands. Among the respondents’ wives, 492 (79.4%) were pregnant during the data collection. Regarding the number of pregnancies, 511 (82.4%) of the respondents’ wives were multigravida, and 376 (60.6%) husbands helped their wives comply with the instructions received at health institutions during ANC visits. The majority of the respondents, 600(98.6%), reported that there was a health facility available in their kebeles, but only 99 (16.0%) of them lived within 30 min of a health facility. Similarly, 108 (17.4%) of the respondents needed to walk distances greater than 90 min (Table 2).
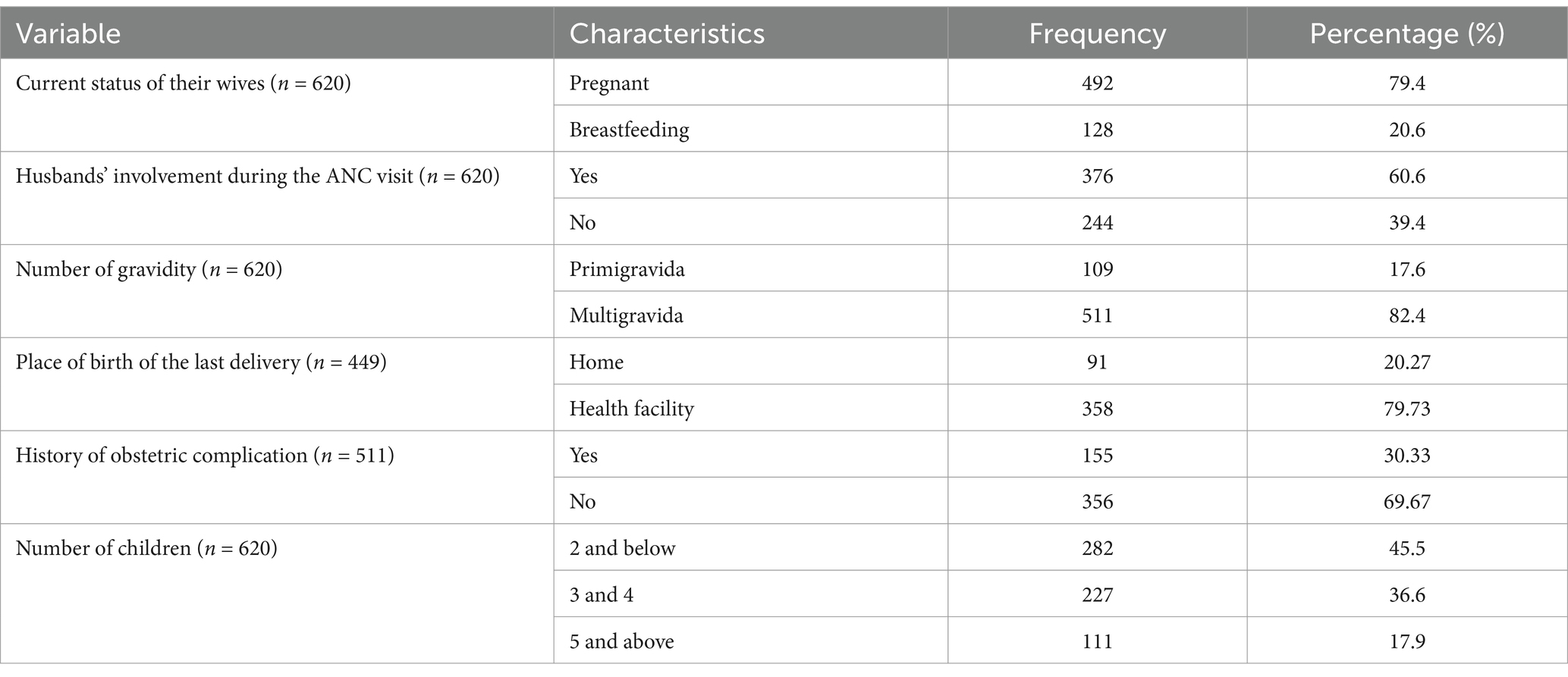
Table 2. Distribution of the respondents and their wives by obstetric characteristics in the Raya Kobo district, April 2023.
Infrastructure-related factorsOf the respondents, 600 (96.8%) reported that health facilities were available in their kebeles, and only 216 (36%) of the respondents reported that it took them less than 30 min to reach the nearest health facility (Table 3).
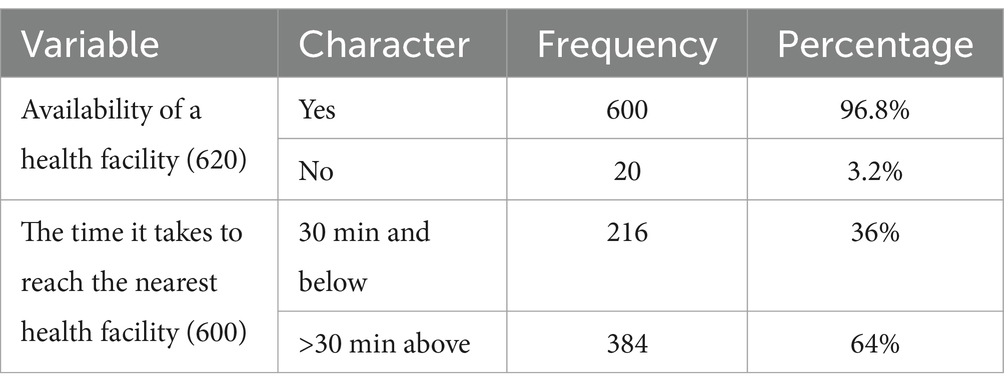
Table 3. Availability of a health facility and the time it takes to reach it in the Raya Kobo district, 2023.
Sources of informationThe findings of this study indicated that the majority of the participants, 247(39.8%), who gathered information about obstetric danger signs received it from health professionals (Figure 2).
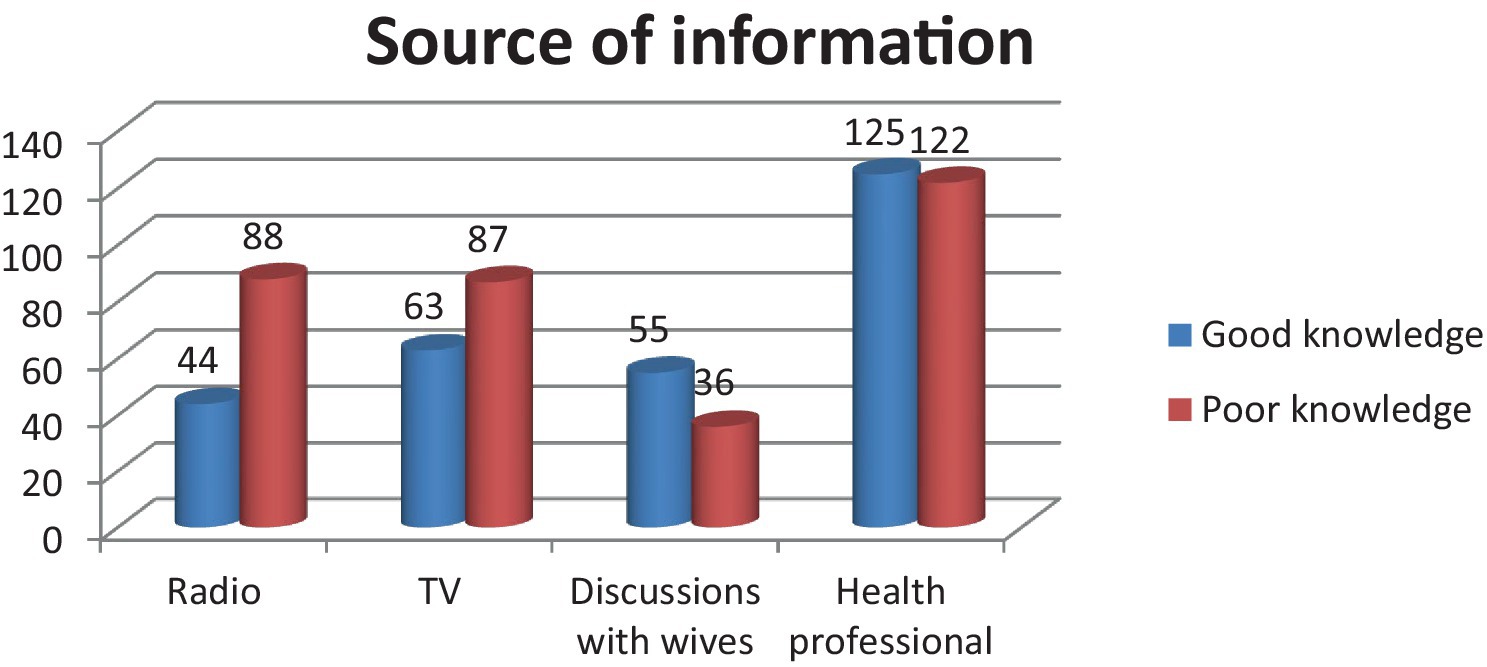
Figure 2. Source of information for the husband on ODS in Raya Kobo district, April (2023).
Knowledge of obstetric danger signsThe knowledge of obstetric danger signs among the respondents was calculated for each period using the median score cut-off point of 34. It was categorized as “good knowledge” when the average score was above the median score, and it was categorized as “poor knowledge” when the average score was below the median score. Of all respondents, 46.3% (95% CI: 42.6–50.3) had good knowledge (Figure 3).
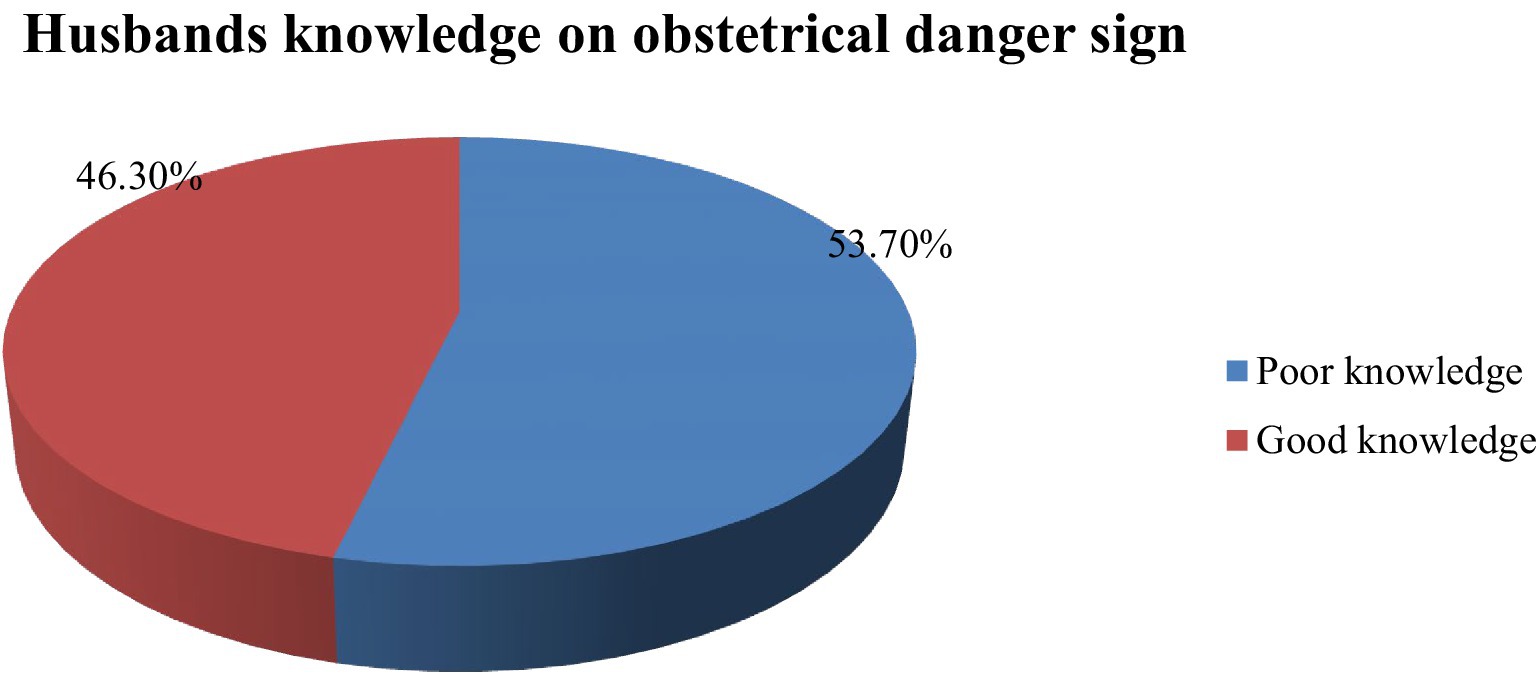
Figure 3. Knowledge of obstetric danger signs among husbands in the Raya Kobo District April 2023.
Knowledge of obstetric danger signs during pregnancy, delivery, and postpartum periodsWhen computing the phase one variable to identify those above the median score, 261 (42.1%) of the respondents, with a 95% CI of (38.1, 46.0), had good knowledge during the postpartum period. In this phase, severe vaginal bleeding after delivery was reported to be a high-scoring obstetric danger sign, mentioned by 348 (56.1%), while severe weakness was reported to be a lower-scoring obstetric danger sign, mentioned by 185 (29.8%). In another computed variable, 36.6% of the respondents had good knowledge throughout pregnancy. A total of 422(68.1%) respondents mentioned membrane rupture before labor and 411 (66.3%) respondents mentioned severe vaginal bleeding as high-scoring obstetric danger signs, while 92 (14.8%) mentioned difficulty breathing as a lower-scoring obstetric danger sign. Lastly, during delivery, 26% of the husbands mentioned in phase two had a median score. A total of 301 (48.1%) identified placenta retention (placenta not detaching before 30 min) as the highest-scoring obstetric danger sign, while 106 (17.1%) mentioned high-grade fever as a lower-scoring danger sign (Table 4).
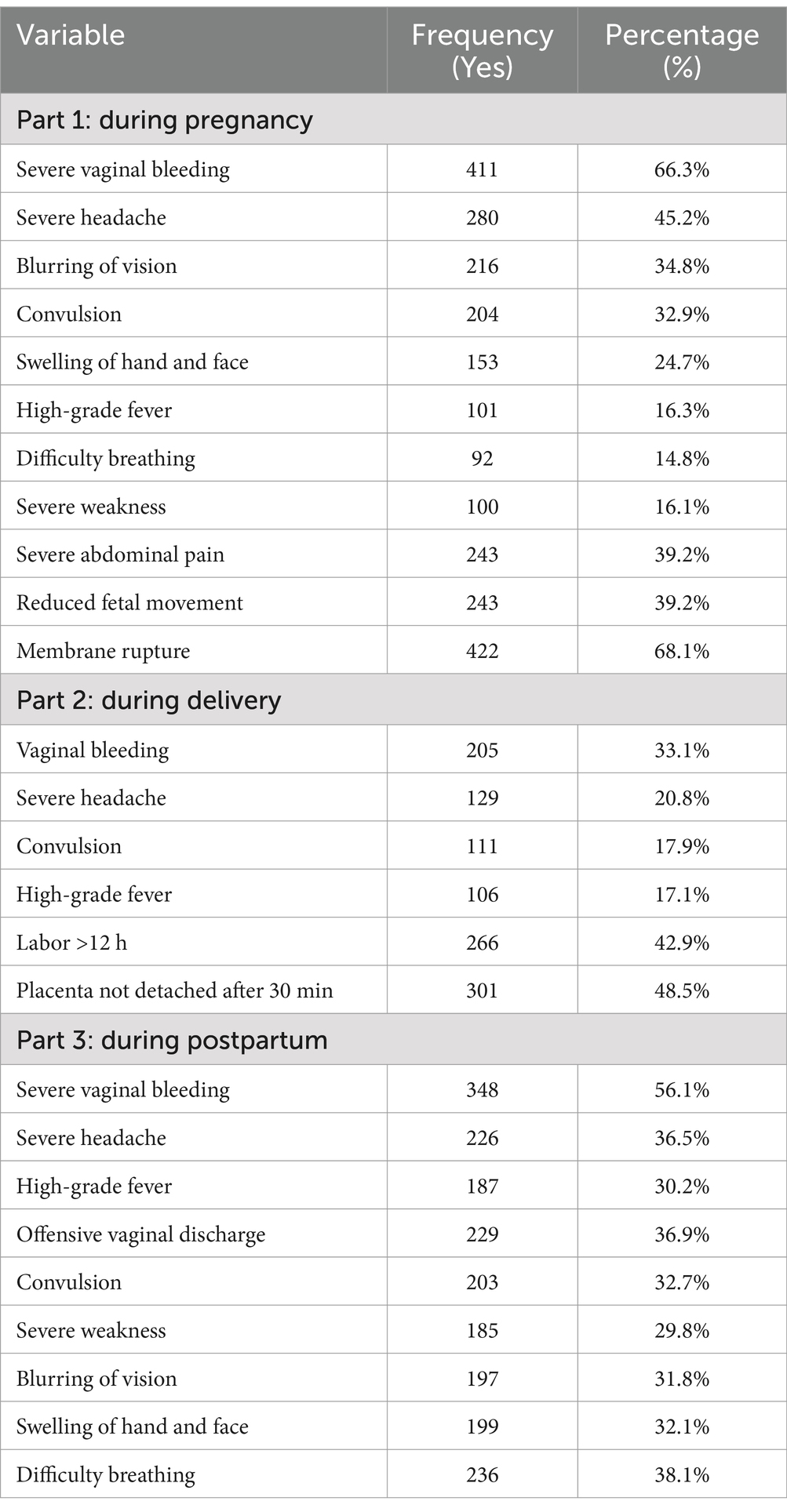
Table 4. Knowledge of obstetric danger signs during pregnancy, delivery, and postpartum periods among the husbands in the Raya Kobo district, April 2023.
Factors associated with the husbands’ knowledge of obstetrical danger signsTo identify the factors associated with the husbands’ knowledge of obstetric danger signs, binary and multivariable logistic regression analyses were conducted with the dependent and independent variables. In the binary logistic regression, the age of the husband, the occupation of the husband, the level of education of the husband, family income, residence, the husband’s involvement in ANC visits, the wife’s history of bad obstetric signs, number of children, and the level of education of the wife were significantly associated with the husbands’ knowledge of obstetric danger signs.
The multivariable analysis was performed to identify independent predictors of the husbands’ knowledge regarding obstetrics danger signs. After controlling for possible confounders, the husband’s education, residence, number of children, and family income were identified as the independent predictors of the husbands’ knowledge of obstetrics danger signs in the Raya Kobo district. These results also showed that the husbands who had secondary school education were 4.8 times (AOR = 4.77, 95% CI, (1.42–16.04)) more likely to have good knowledge of obstetrics danger signs than those who were unable to read and write.
The husbands in families with more than five children were 85% (AOR = 0.15: 95% CI; (0.05–0.46)) less likely to have good knowledge of obstetric danger signs compared to those with fewer than two children. The husbands with an average monthly income of 3,001–5,000 birr were 3.4 times (AOR = 3.35, 95% CI = (1.58, 7.12)) more likely to have good knowledge compared to those with an average monthly income of less than 1,500 birr. The husbands living in urban areas were 3 times (AOR = 3.00, 95%CI = (1.59, 7.57)) more likely to have good knowledge than those living in rural areas (Table 5).
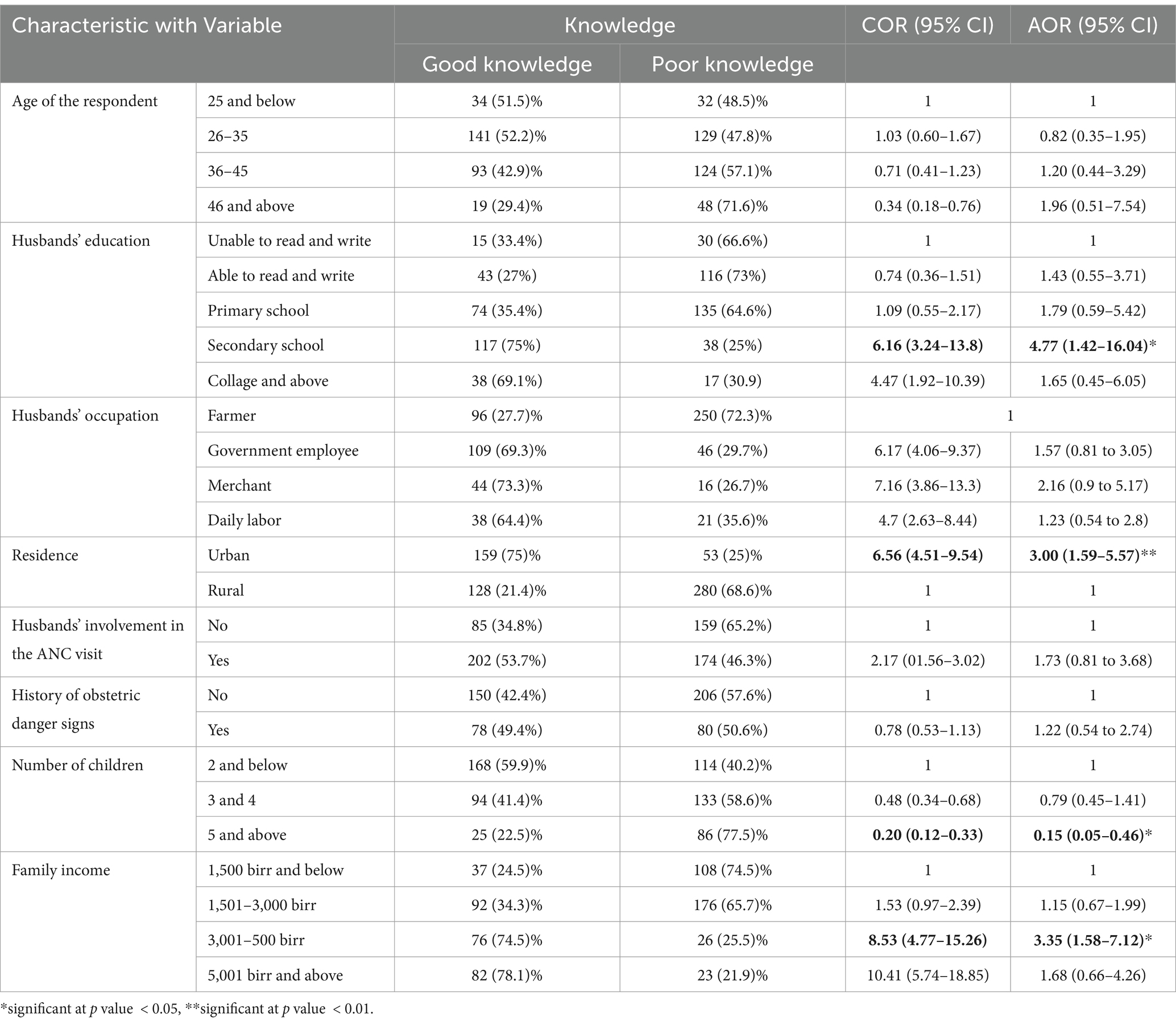
Table 5. Multivariate and bivariate logistic regression analyses showing factors independently associated with the husbands’ knowledge of obstetrics danger signs in the Raya Kobo district, 2023.
DiscussionThe findings of this study indicated that the magnitude of the husbands’ knowledge of obstetric danger signs in the overall combination of three phases (prenatal period, childbirth, and postnatal period) was 46.3%, with a 95% CI of 42.6 to 50.3%. This finding is lower than that in Nigeria, where research conducted in two different study areas found that 53.8 and 51.9% of men had good knowledge of obstetric danger signs in pregnancy, as well as 53.3% in Dessie (12, 21, 22). This variation may be due to socio-economical differences between the studies conducted in Nigeria and this study, where the majority of the participants lived in rural areas that had less access to sources of information about obstetric danger signs and a lower likelihood of wives attending ANC follow-up visits, which would provide opportunities for sharing knowledge on danger signs. However, this finding was higher than the findings of studies conducted in the Musoma district, Mara region, Tanzania (32%) and southern Ethiopia (42.2%) (23).
Possible reasons for the higher prevalence and the differences observed might include healthcare system disparities between the countries, especially the utilization of community mobilization on maternal health in Ethiopia by health extension workers. Additionally, the time gap between studies may have contributed, as wives’ utilization of maternal care may have improved, which in turn could have led to an increase in husbands’ knowledge of danger signs. The study found that the husbands who had completed secondary school were 4.8 times (AOR = 4.77, 95% CI, (1.42–16.04)) more likely to have good knowledge of obstetric danger signs than those who were unable to read and write. This finding is in line with a study conducted in Southwest Nigeria (24). This may be due to the fact that education is an important tool for increasing understanding and access to information about obstetric danger signs and their outcomes through various electronic media. In addition, closer collaboration between schools and local health services may enhance the delivery of reproductive health education. The place of residence was significantly associated with the husbands’ knowledge of obstetric danger signs. The husbands living in urban areas were 3 times (AOR = 3.00, 95%CI = (1.59, 7.57)) more likely to have good knowledge than those living in rural areas. This finding is similar to a study conducted in the Andede district (25). This could be because the respondents living in urban areas in the present study had greater access to information compared to those in rural areas, as most messages are transmitted through various media available in urban settings. However, this finding is in contradiction with a study conducted in the Chencha district, Gamo Gofa Zone, southern Ethiopia, which showed that husbands living in rural areas were 8.4 times more knowledgeable than those living in urban areas (11). This discrepancy may be due to the fact that the husbands living in rural areas in this study had limited sources of information and lower educational backgrounds compared to those living in urban areas.
The number of children in this study was a significant factor associated with the husbands’ awareness. The husbands in families with more than five children were 85% times (AOR = 0.15; 95% CI: 0.05–0.46) less likely to have good knowledge of obstetric danger signs compared to those with fewer than two children. The finding is consistent with a study conducted in Tanzania (26).A possible reason for this is that husbands with many children tend to prioritize income generation, leading to longer working hours and multiple sources of employment (27). This situation leaves them with limited time to attend antenatal care (ANC) visits or to recognize and respond to obstetric danger signs, such as prolonged labor, severe bleeding, or reduced fetal movement, all of which require immediate attention. However, a study conducted in Nigeria showed no significant difference in the knowledge of danger signs regarding the number of children in the family (28). The reason for this discrepancy may be the large sample size used as larger sample sizes increase the probability of detecting associations between variables.
The total average monthly income of the family was also a factor associated with the husbands’ knowledge of obstetric complications. The husbands with an average monthly income of 3,001–5,000 birr were 3.4 times (AOR = 3.35, 95% CI = (1.58, 7.12)) more likely to have good knowledge compared to those with an average monthly income of less than 1,500 birr. This finding is in line with studies conducted in South Ethiopia and Uganda, where economic status was also significantly associated with men’s awareness of danger signs of obstetric complications (28, 29). This may be because men with higher economic status are more likely to be exposed to health education provided by health institutions. In addition, they can afford radios, TVs, and other media to access more information about maternal health. Higher-income households tend to exhibit better health-seeking behaviors and greater engagement in maternal health, as they are less constrained by financial limitations. This access to information and services enables them to pay more attention to their wives’ pregnancies, increasing the likelihood of early recognition and intervention in the case of obstetric danger signs.
Strengths and limitations of this studyThe study was community-based, which allowed it to reflect the experiences of the husbands during the study period. It also utilized a large sample size, making the findings more representative. However, a limitation of the study is the potential for recall bias, even though the recall period was reduced to 1 year. The husbands were asked to remember events that occurred up to 1 year before the study, and the data were collected by having them mention the obstetric danger signs they knew and the activities they had undertaken, without providing them with options to choose from.
ConclusionThe husbands’ knowledge of obstetric danger signs in the Raya Kobo district was limited. Severe vaginal bleeding was the most frequently identified obstetric danger sign during the antepartum, intrapartum, and postpartum periods. The educational status of the husband, average family income, residence, and number of children were significantly associated with the husbands’ knowledge of obstetric danger signs. These findings highlight the importance of addressing knowledge gaps through targeted educational programs aimed at improving awareness of obstetric complications. Enhancing this awareness among husbands could play a crucial role in promoting timely healthcare-seeking behaviors and improving maternal health outcomes in the study area.
Data availability statementThe data sets used or analyzed during the current study are available from the corresponding author upon reasonable request.
Ethics statementThe studies involving humans were approved by the Institutional Review Board (IRB) of Debre Berhan University, Asrat Woldeys Health Science Campus, who granted ethical approval under reference number IRB01/74/2015. The Official letter was written for Amara Public Health Institute to Raya Kobo District health offices and informed verbal consent was taken from individual participants. No form of identifier was included in the questionnaires to maintain confidentiality. Participation was voluntary and participants were informed that they could withdraw from the study at any stage if they desired, without any penalty. At the end of the interview, information was given about the danger signs of obstetric complications at three stages (during pregnancy, labor and childbirth, and the postpartum period). The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributionsJD: Data curation, Project administration, Visualization, Writing – original draft, Writing – review & editing. AY: Conceptualization, Data curation, Formal analysis, Methodology, Writing – original draft, Writing – review & editing. AMi: Conceptualization, Formal analysis, Methodology, Software, Validation, Writing – original draft, Writing – review & editing. AA: Conceptualization, Investigation, Methodology, Supervision, Writing – original draft, Writing – review & editing. AMo: –. NS: Formal analysis, Investigation, Methodology, Visualization, Writing – original draft, Writing – review & editing. BM: Conceptualization, Formal analysis, Investigation, Methodology, Validation, Writing – original draft, Writing – review & editing.
FundingThe author(s) declare that financial support was received for the research, authorship, and/or publication of this article. The study was fully funded by the Amhara National Regional State Health office.
AcknowledgmentsFirst, we would like to thank all study participants for their contribution in providing the necessary information. We also thank data collectors and supervisors for their commitment to the accomplishment of this thesis work. Finally, we would like to thank the Amhara Regional State Health Bureau for their cooperativeness.
Conflict of interestThe authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s noteAll claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
AbbreviationsANC, Antenatal Care; AOR, Adjusted Odds Ratio; BSc, Bachelor of Science; CI, Confidence Interval; CM, Clinical Midwife; COR, Crude Odd Ratio; EDHS, Ethiopia Demographic Health Survey; HEWs, Health Extension Workers; ICPD, International Conference on Population and Development; ODS, Obstetric Danger Signs; OR, Odd Ratio; RH, Reproductive Health; SBA, Skilled Birth Attendant; SDG, Sustainable Development Goal; SPSS, Statistical Package and Services Solution; WHO, World Health Organization.
References1. WHO, U. and W.B. UNFPA. Trends in maternal mortality: 1990 to 2015. Geneva: World Health Organization (2015).
2. Woldeamanuel, GG, Lemma, G, and Zegeye, B. Knowledge of obstetric danger signs and its associated factors among pregnant women in Angolela Tera District, Northern Ethiopia. BMC Res Notes. (2019) 12:1–6. doi: 10.1186/s13104-019-4639-8
Crossref Full Text | Google Scholar
3. Organization, W.H. Trends in maternal mortality 2000 to 2017: Estimates by WHO, UNICEF, UNFPA, World Bank Group and the United Nations population division. Geneva, Switzerland: Executive summary World Health Organization (2019).
4. Brun, M, Monet, JP, Moreira, I, Agbigbi, Y, Lysias, J, Schaaf, M, et al., Implementation manual for developing a national network of maternity units-improving emergency obstetric and newborn care (EmONC), United Nations Population Fund. United Nations Popul Fund. (2020).
5. Stafford-Smith, M, Griggs, D, Gaffney, O, Ullah, F, Reyers, B, Kanie, N, et al. Integration: the key to implementing the sustainable development goals. Sustain Sci. (2017) 12:911–9. doi: 10.1007/s11625-016-0383-3
PubMed Abstract | Crossref Full Text | Google Scholar
6. Organization, W.H. Trends in maternal mortality: 1990 to 2015. Geneva: WHO (2015). 2018 p.
7. Alem, AZ, Yeshaw, Y, Liyew, AM, Tesema, GA, Alamneh, TS, Worku, MG, et al. Timely initiation of antenatal care and its associated factors among pregnant women in sub-Saharan Africa: a multicountry analysis of demographic and health surveys. PLoS One. (2022) 17:e0262411. doi: 10.1371/journal.pone.0262411
PubMed Abstract | Crossref Full Text | Google Scholar
8. Woldegiorgis, MA, Bhowmik, J, and Wubegzier, M. Trends in reproductive health indicators in Ethiopia: 2000–2014. Int J Healthcare. (2017) 3:17–25.
9. Kurji, J. Assessing the determinants of maternal healthcare service utilization and effectiveness of interventions to improve institutional births in Jimma Zone. Ethiopia: Université d'Ottawa/University of Ottawa (2021).
10. Hailu, M, Gebremariam, A, and Alemseged, F. Knowledge about obstetric danger signs among pregnant women in Aleta Wondo District, Sidama Zone, southern Ethiopia. Ethiop J Health Sci. (2010) 20:25–32. doi: 10.4314/ejhs.v20i1.69428
PubMed Abstract | Crossref Full Text | Google Scholar
11. Debiso, AT, Gello, BM, and Malaju, MT. Factors associated with men’s awareness of danger signs of obstetric complications and its effect on men’s involvement in birth preparedness practice in southern Ethiopia, 2014. Adv Public Health. (2015) 2015:1–9. doi: 10.1155/2015/386084
Crossref Full Text | Google Scholar
12. Tadesse, M, Boltena, AT, and Asamoah, BO. Husbands’ participation in birth preparedness and complication readiness and associated factors in Wolaita Sodo town, southern Ethiopia. African J Prim Health Care Fam Med. (2018) 10:1–8.
13. Okoror, CEM, and Omuemu, VO. Knowledge of obstetric danger signs among antenatal clinic attendees in south–South Nigeria. Health Care Women Int. (2021) 44:1363–78. doi: 10.1080/07399332.2021.1941025
Crossref Full Text | Google Scholar
14. Winner, MBF, and Do, M. Knowledge of obstetric danger signs among adolescent and adult mothers in Tanzania: a secondary data analysis. Women's Reprod Health. (2021) 8:279–93. doi: 10.1080/23293691.2021.1976049
Crossref Full Text | Google Scholar
15. Orwa, J, Gatimu, SM, Mantel, M, Luchters, S, Mugerwa, MA, Brownie, S, et al. Birth preparedness and complication readiness among women of reproductive age in Kenya and Tanzania: a community-based cross-sectional survey. BMC Pregnancy Childbirth. (2020) 20:1–9. doi: 10.1186/s12884-020-03329-5
Crossref Full Text | Google Scholar
16. Arefaynie, M, Kefale, B, Yalew, M, Adane, B, Dewau, R, and Damtie, Y. Number of antenatal care utilization and associated factors among pregnant women in Ethiopia: zero-inflated Poisson regression of 2019 intermediate Ethiopian demography health survey. Reprod Health. (2022) 19:1–10. doi: 10.1186/s12978-022-01347-4
Crossref Full Text | Google Scholar
17. Suandi, D, Williams, P, and Bhattacharya, S. Does involving male partners in antenatal care improve healthcare utilisation? Systematic review and meta-analysis of the published literature from low-and middle-income countries. Int Health. (2020) 12:484–98. doi: 10.1093/inthealth/ihz073
PubMed Abstract | Crossref Full Text | Google Scholar
18. Getachew, F, Sintayehu, A, Damitew, S, Endalkachew, F, and Gebeyaw, M. Mens knowledge towards obstetric danger signs and their involvement on birth preparedness in Aneded woreda, Amhara regional state, Northwest Ethiopia. Ethio J Public Health Nutri. (2019) 3:39–45.
19. Organization, W.H. Trends in maternal mortality: 1990–2015: Estimates from WHO, UNICEF, UNFPA, world bank group and the United Nations population division. Geveva, Switzerland: World Health Organization (2015).
20. Yimer, NB, and Liben, ML. Knowledge on intrapartum danger sign influences place of delivery: the case of Raya Kobo District, northeastern Ethiopia. Int J. (2021) 10:44–50. doi: 10.6000/1929-4247.2021.10.02.1
Crossref Full Text | Google Scholar
21. Chattopadhyay, A, and Govil, D. Men and maternal health care utilization in India and in selected less-developed states: evidence from a large-scale survey 2015–16. J Biosoc Sci. (2021) 53:724–44. doi: 10.1017/S0021932020000498
Crossref Full Text | Google Scholar
22. Shitie, A, Dilnessa, T, Ayalew, S, and Tadesse, B. Knowledge and factors associated with obstetric danger signs among married men in Dessie town, south Wollo, north-East Ethiopia: a community-based cross-sectional study. BMJ Open. (2022) 12:e063936. doi: 10.1136/bmjopen-2022-063936
留言 (0)