Crippling hand injuries are one of the greatest challenges facing hand microsurgeons (1–3), Re-implantation of severed fingers is undoubtedly the best option for restoring function, especially when multiple fingers are involved, and improvements in microsurgical techniques and effective postoperative monitoring have led to an increasing survival rate of reimplantation (4, 5). However, as medical technology continues to advance, the challenge is not only to restore blood circulation to the fingers but also to better restore hand function (6).
Therefore, in the treatment of crippling hand injuries, it is of utmost importance to restore a working finger and to restore normal joint movement and motor stability, as well as sensory sensitivity in the fingers (7). With advances in microsurgery and medicine, a variety of finger reconstruction techniques have been developed and ectopic fostering techniques have matured; however, each technique has its limitations, including simple toe grafts and finger reconstruction are aesthetically unpleasant (8); Prosthetic fingers can physically replace fingers, but not sensorimotor functions (9, 10); Connected bilateral second toes for long finger reconstruction are associated with poor function and appearance (11). In this trend, the concept of holomorphic reconstruction was born (3, 12), finger reconstruction has been widely carried out at home and abroad.
Fully shaped reconstruction of a severed finger combined with ectopic banking is an innovative technique for the repair of residual hand injuries that can compensate for the limitations of previous approaches. Although heterotopic fostering composite repair has been in use for many years, few reports have focused on the clinical outcomes of ectopic banking composite repair in disfiguring hand injuries. Here, we report a complex case of disfiguring hand injury treated with heterotopic fostering of a severed finger and reconstructed fingers from a pedicle, and evaluate the existing literature.
Case reportThe patient signed a paper version of the informed consent form, and it was approved by the Ethics Committee of the PLA General Hospital.
General informationA male patient, 43 years old, was admitted to the hospital with a “Meat grinder injured left hand for three hours.” She was admitted to the hospital on an emergency basis after three hours of severe destruction of her left hand due to the inadvertent operation of a meat grinder at home. x-ray examination showed multiple metacarpal and phalangeal fractures of the left hand and poor alignment of the carpometacarpal and metacarpophalangeal joints (Figure 1).
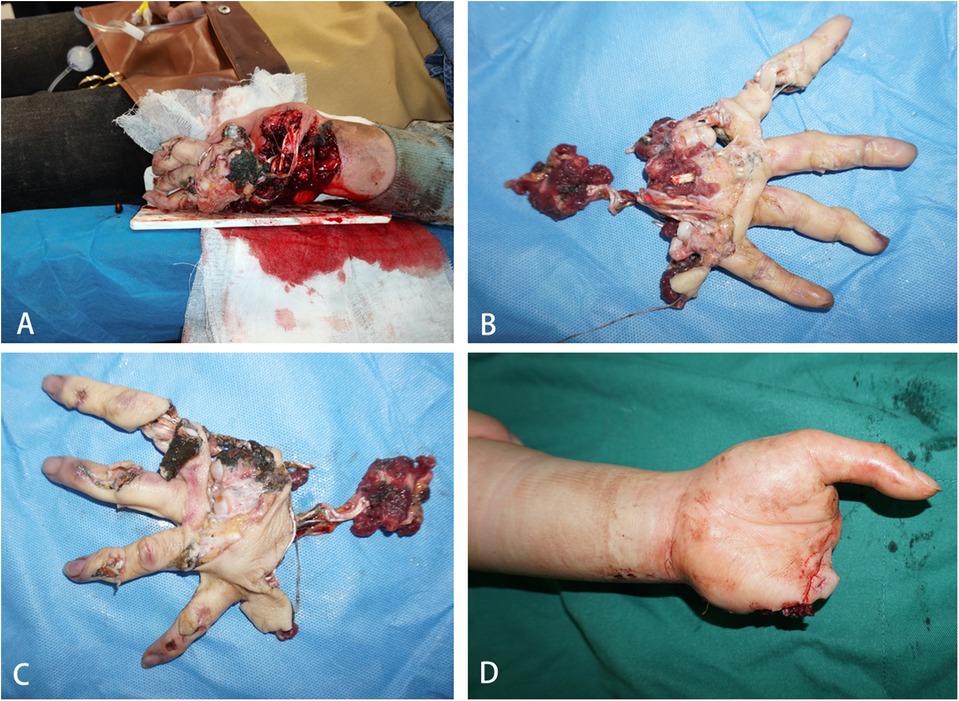
Figure 1. (A–D) on admission, examination revealed severe damage to the left index, middle, ring, and little fingers. The distal ends showed no blood circulation, and there was extensive damage beyond the mid-palm level, accompanied by multiple wounds and exposure of tendons and metacarpal bones.
TreatmentsGiven the complexity of the patient's injury and the severe damage to the palm, primary replantation is not suitable. After thorough discussion, our surgical team has decided to adopt a treatment plan involving the ectopic replantation of the severed finger to the foot. This will be followed by a secondary procedure to repair the bone and flap in the palm and simultaneously transplant the replanted finger back to the hand (Figure 2).
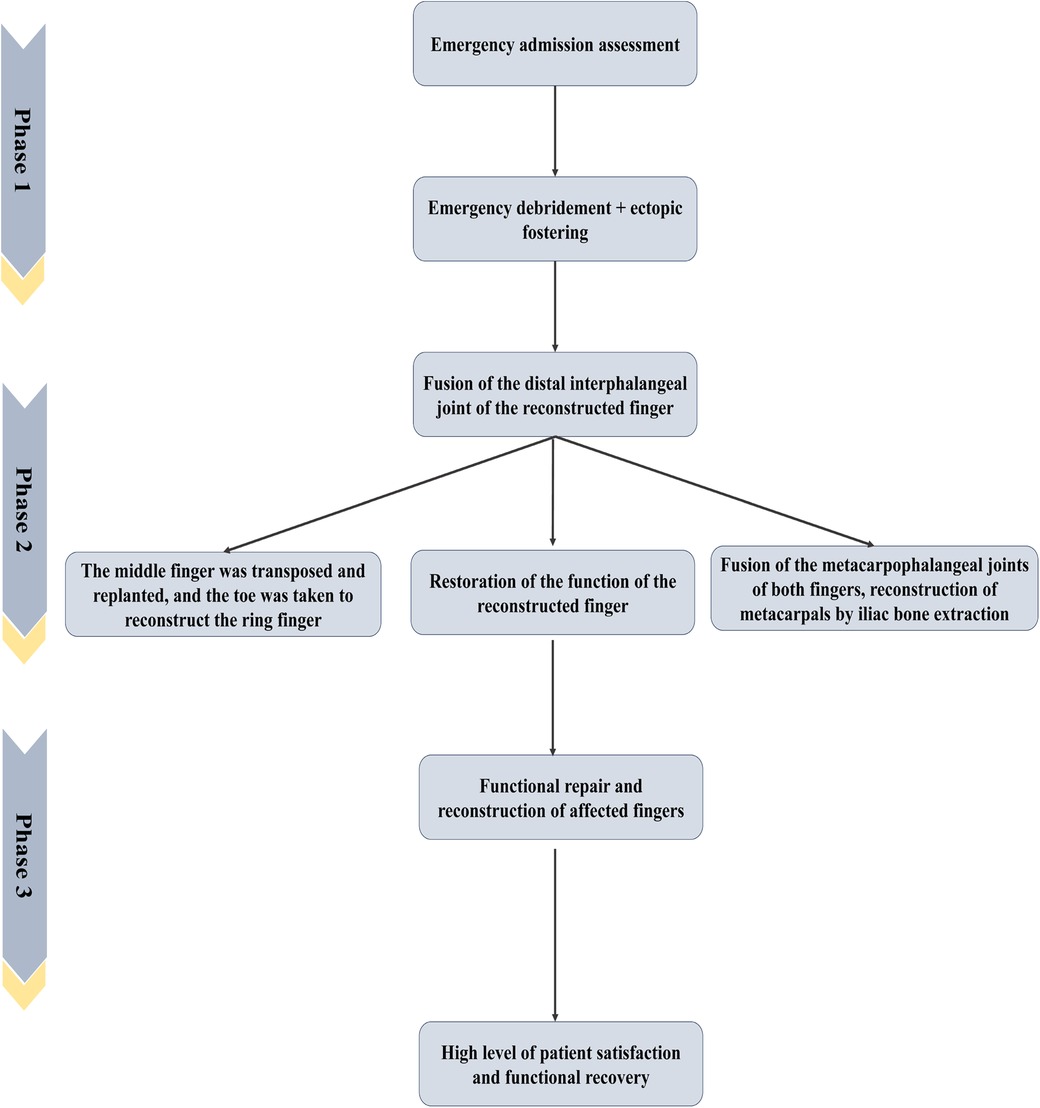
Figure 2. Disposal procedure and surgical plan.
Treatment process and results Phase 1: ectopic fosteringAfter completing the relevant preoperative preparations, we carefully assessed the patient's severed fingers and the condition of the remaining blood vessels. For the primary procedure, we opted for debridement and heterotopic finger grafting, placing each of the four fingers on the dorsum of the feet. Under general anesthesia, we thoroughly debrided the wound on the left hand and skillfully utilized the dorsal pedis vessels (particularly the dorsal pedal artery) as anastomosis sites to graft the severed fingers onto the dorsum of the feet. Postoperatively, we followed the standard care protocol for finger reattachment (Figure 2). After one month of meticulous care, the blood supply to the middle finger grafted on the left foot was satisfactory, while the other three fingers underwent necrosis. The patient was able to fully bear weight and walk ten days after the surgery and was successfully discharged.
Phase 2: replantation of the middle finger and reconstruction of the ring finger using a ToeSix weeks post-trauma, we plan to perform the second stage of surgery. Considering that only the middle finger has survived, a hand with just the thumb and middle finger would not have good grasping functionality. Additionally, if we proceed with a staged approach, where the fostered finger transplant is done first followed by reconstruction, the blood supply during the fostering phase will have already established connections with the first dorsal metatarsal artery, thereby increasing the risk of staged surgery. Therefore, we innovatively decided to perform the foster finger transplant and finger reconstruction simultaneously. This includes the relocation and replantation of the middle finger, as well as the reconstruction of the index finger using a toe from the foot. The procedure was performed as described below (Figure 3).

Figure 3. (A–C) One-phase surgery was performed for debridement and ectopic fostering of the severed fingers, with each of the four fingers being fostered in both feet; (D–F) after a month of careful care, the middle finger of the left foot was foster was in good hematological condition, while the remaining three fingers were necrotic; (G) post-operative DSA examination.
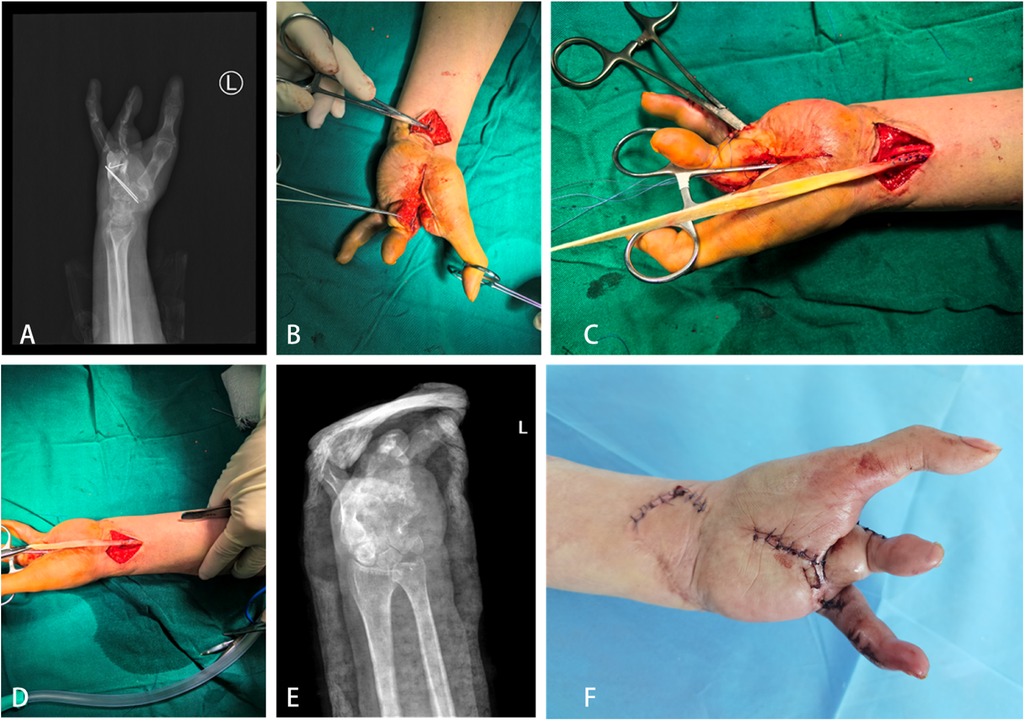
The palmar defect was reconstructed using a 3.5 × 4 cm iliac bone graft. The reconstructed index finger was formed by combining skin from the great toe, the interphalangeal joint of the second toe, and part of the iliac bone, along with the fostered finger. Additionally, a composite tissue flap from the dorsal foot, including a long pedicle (comprising the dorsal foot artery and its accompanying veins, as well as the great saphenous vein), was meticulously anastomosed to the deep branch of the radial artery and the cephalic vein. This approach allowed us to reconstruct the patient's palmar defect and restore the morphology of the index and middle fingers simultaneously. The donor site on the foot was repaired using a contralateral anterolateral thigh flap. Due to the prolonged surgical time and the extensive tendon defects, the motor function of the reconstructed index and middle fingers was not restored during this procedure. Three weeks post-surgery, the transplanted fostered finger and the reconstructed index finger had survived well. The patient then began passive movement of the thumb, gradually progressing to active movement over the next six weeks (Figure 4).
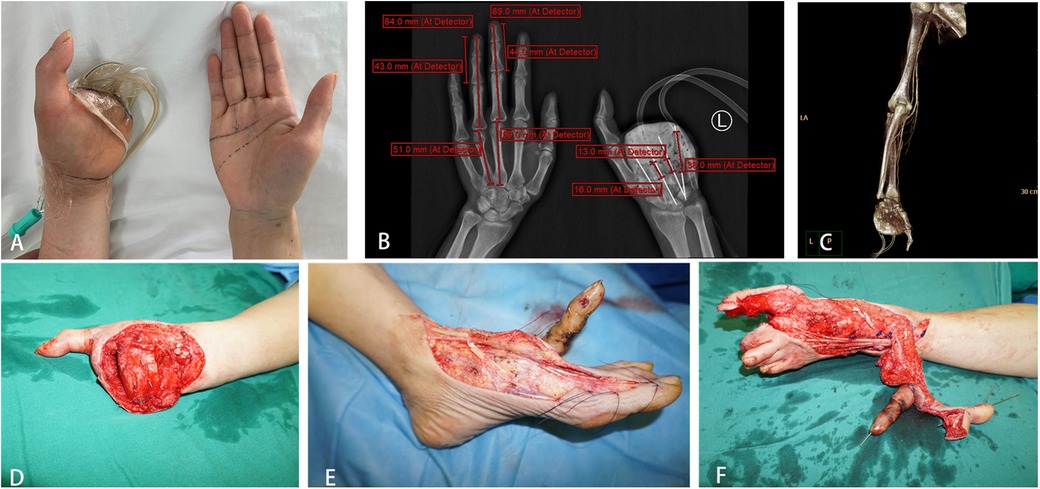
Figure 4. (A–C) precise pre-operative planning; (D–F) replantation of the middle finger and reconstruction of the ring finger by removal of the toe.
Phase 3: hand function reconstructionIn the subsequent treatment, we focused on the functional reconstruction of the patient's left hand. Through multiple surgeries, the patient underwent exploration and allograft tendon transplantation for the extensor and flexor tendons of the left hand's index and middle fingers. Additionally, we performed thinning of the left foot flap, exposed phalanx removal, debridement, and suturing. We successfully restored partial function to the patient's left hand. After seven months of treatment and rehabilitation, the survival of the reconstructed index and middle fingers (toe-to-hand transfer) was satisfactory. Although there were limitations in movement, the overall recovery outcome was considered satisfactory (Appendix A1).
Treatment outcomes, follow-up, and prognosisThroughout the treatment, we consistently monitored the patient's feedback and satisfaction (13). Monthly follow-ups were conducted according to the rehabilitation plan, documenting complications, limb mobility, patient-reported satisfaction, Visual Analog Scale (VAS) scores (14), Short Form-36 (SF-36) scores (15, 16), and imaging data. One year after the first-stage surgery, VAS scores indicated a significant improvement, with the patient's pain level decreasing from 8 before surgery to 2 postoperatively. This suggests a marked reduction in pain and discomfort. Additionally, the SF-36 health survey results demonstrated high scores in physical functioning, mental health, and overall health status (Table 1). These positive outcomes not only validate the effectiveness of our treatment plan but also provide valuable experience and reference for future cases.

Table 1. Short form-36 health survey questionnaire results.
In conclusion, the complex hand injury case, managed with dislocated finger transplantation and complete reconstruction, achieved satisfactory results. The successful application of this innovative technique highlights our expertise in hand surgery and offers new insights and directions for treating similar cases.
DiscussionThe main difference between this case report and previous cases is the first successful combined application of ectopic parasitosis, finger reconstruction, and flap grafting for hand reconstruction. This innovative technique has achieved a breakthrough in the field of hand surgery, providing a new way of thinking about the treatment of complex hand injuries and achieving satisfactory clinical results and patient satisfaction.
Complex disfiguring injuries to the hand have been a great challenge in hand surgery (2). Conventional in situ reimplantation surgery is not optimal in some cases due to the need for significant shortening of the severed finger and the low success rate. In this case, the challenges we faced included not only the complexity of the surgery itself, but also how to apply a combination of ectopic banking, toe reconstruction, and fully shaped reconstruction to achieve optimal restoration of hand function.
By analyzing the existing literature and clinical judgment, we chose ectopic banking as the initial management, followed by the reconstruction of finger and iliac bone harvesting reconstruction, combined with foot-free flap repair. This three-stage repair plan is relatively rare in the existing literature but has a solid theoretical and practical basis. The ultimate goal of surgical reimplantation is not only to achieve successful revascularisation but more importantly the restoration of hand function and patient satisfaction (17–19). Heterotopic replantation offers significant advantages in patients with extensive soft tissue loss or severe contamination requiring radical debridement. However, there is no consensus on the indications for surgery, the ideal location and duration of ectopic banking, the approach and timing of soft tissue management, and the management of complex microvascular secondary reimplantation (20, 21). In reported cases of primary ectopic banking, the reimplanted portion is usually transferred to the correct position within a few weeks after the initial ectopic banking, an approach that is effective in restoring hand function. Bakhach et al (22) demonstrated the effectiveness of ectopic banking in hand reconstruction by performing ectopic banking in four patients, after stump reconstruction, the ingers were microsurgically transplanted to the hand, and functional pinching was eventually restored. In addition, alloplastic reconstruction achieves the goal of “how much is missing, how much is being replaced”, which makes the repair and reconstruction of finger defects precise, but does not emphasize the control of damage to the donor area (23). Holomorphic reconstruction, proposed by Wang Zengtao in 2011, emphasizes the design and assembly of a functionally and cosmetically near-normal finger according to the structure and shape of the healthy finger, while preserving the length and most of the function and shape of the toes (24). This technique allows for more precise repair and reconstruction of finger defects. It is currently the optimal solution for finger reconstruction.
Fully shaped reconstruction of a severed finger combined with Ectopic banking presented in this case is an innovative surgical approach that emphasizes the design and assembly of a finger that is functionally and cosmetically close to normal based on the structure and shape of a healthy finger while preserving as much as possible the length, function, and morphology of the pedicle. Compared with conventional finger replantation techniques, ectopic parasitism combined with holomorphic reconstruction of severed fingers is not only more precise in terms of surgical design, but also better able to preserve the function and appearance of the finger. It has been mentioned in the literature that although the ectopic fostering technique has been used for many years, there are relatively few reports of combining it with alloplastic reconstruction for the management of complex hand disfigurement. This paper demonstrates the effectiveness of this innovative technique through the successful treatment of complex hand disfigurement injuries. The clinical significance of this technique lies in the fact that it provides a new treatment option for complex hand disfigurement injuries that are difficult to treat by traditional surgical methods.
Of course, the technique of ectopic banking has matured and the technique of alloplastic reconstruction is increasingly being applied. The innovation of this case lies in the combination of ectopic banking and fully shaped reconstruction to repair the hand injury, and the difficulty involves simultaneous grafting of blood vessels for reconstruction and the need for simultaneous surgeries, which makes the surgery difficult and requires a very high level of demands on the surgical team. To the best of our knowledge, this is the first case in the world where this combined technique has been successfully applied for hand reconstruction. After overcoming all stages of surgical difficulty, we achieved remarkable clinical success, providing valuable experience and new ideas for the treatment of similar complex hand injuries.
Fully shaped reconstruction of a severed finger combined with ectopic banking is a difficult multi-stage microvascular procedure, while combined reconstruction complicates the difficulty of the procedure and should only be considered for very valuable sites (25). The risk of potentially serious complications (e.g., sepsis and hemorrhage) exists when salvaging a crippled hand trauma by allografting. Therefore, this technique should only be considered if performed by a high-level reconstruction team in a microsurgical setting. In addition, the success of ectopic banking relies on meticulous postoperative management and a rigorous rehabilitation program to ensure the survival and functional recovery of the transplanted tissue.
With the development of technology and more clinical experience, the combined application of fully shaped reconstruction of a severed finger with ectopic banking is expected to be further optimized to improve the success rate of hand reconstruction surgery and the quality of life of patients. Future studies should focus on the refinement of surgical indications, management of postoperative complications, and assessment of long-term functional recovery to provide more comprehensive treatment options in the field of hand surgery.
ConclusionFully shaped reconstruction of a severed finger combined with ectopic banking is a difficult multistage microvascular procedure. This case report demonstrates the value of ectopic parasitism with pedicle reconstructive fingers in finger reconstruction. It not only validates the feasibility and effectiveness of this innovative surgical approach but also provides a valuable reference for the treatment of similar cases in the future.
Data availability statementThe datasets presented in this article are available upon reasonable request. Requests to access the datasets should be directed to emhlbmdmZW5namlhMzAxQDE2My5jb20=.
Ethics statementWritten informed consent was obtained from the individual(s), and minor(s)' legal guardian/next of kin, for the publication of any potentially identifiable images or data included in this article.
Author contributionsZJ: Writing – original draft. LS: Conceptualization, Writing – review & editing. WG: Formal Analysis, Resources, Writing – original draft. HL: Writing – review & editing. JZ: Data curation, Methodology, Writing – original draft. WS: Conceptualization, Writing – review & editing. JL: Writing – original draft. JZ: Writing – original draft.
FundingThe author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interestThe authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's noteAll claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References2. Bueno A, Nevado-Sanchez E, Collazo C, De la Fuente-Anuncibay R, González-Bernal J. Functional outcomes in upper limb replantation-a systematic review. J Clin Med. (2024) 13(5). doi: 10.3390/jcm13051289
PubMed Abstract | Crossref Full Text | Google Scholar
3. Hou C, Zhang A, Yu X, Han H. Reconstruction of fully shaped fingers using a free great toe nail flap combined with a second toe tissue flap. Int Wound J. (2022) 19(6):1389–96. doi: 10.1111/iwj.13732
PubMed Abstract | Crossref Full Text | Google Scholar
4. Godina M, Bajec J, Baraga A. Salvage of the mutilated upper extremity with temporary ectopic implantation of the undamaged part. Plast Reconstr Surg. (1986) 78(3):295–9. doi: 10.1097/00006534-198609000-00003
PubMed Abstract | Crossref Full Text | Google Scholar
5. Cavadas PC, Landin L, Navarro-Monzones A, Soler-Nomdedeu S. Salvage of impending replant failure by temporary ectopic replantation: a case report. J Hand Surg Am. (2006) 31(3):463–7. doi: 10.1016/j.jhsa.2005.12.016
PubMed Abstract | Crossref Full Text | Google Scholar
9. Elbeshbeshy B, Paksima N. Post-traumatic thumb reconstruction. Bull Hosp Jt Dis. (2001) 60(3-4):130–3.12102399
PubMed Abstract | Google Scholar
10. Pet MA, Morrison SD, Mack JS, Sears ED, Wright T, Lussiez AD, et al. Comparison of patient-reported outcomes after traumatic upper extremity amputation: replantation versus prosthetic rehabilitation. Injury. (2016) 47(12):2783–8. doi: 10.1016/j.injury.2016.10.004
PubMed Abstract | Crossref Full Text | Google Scholar
11. Wei FC, Chen HC, Chuang CC, Noordhoff MS. Reconstruction of the thumb with a trimmed-toe transfer technique. Plast Reconstr Surg. (1988) 82(3):506–15. doi: 10.1097/00006534-198809000-00025
PubMed Abstract | Crossref Full Text | Google Scholar
12. de Oña I R, Villanueva A G, de Oya A S. An alternative thumb reconstruction by double microsurgical transfer from the great and second toe for a carpometacarpal amputation. J Hand Surg Am. (2018) 43(10):955.e1–.e9. doi: 10.1016/j.jhsa.2018.03.022
Crossref Full Text | Google Scholar
13. Maraccini AM, Slonim AD. Prioritizing the assessment of patient and family experience in the evaluation of healthcare quality. Pediatr Crit Care Med. (2020) 21(10):905–6. doi: 10.1097/PCC.0000000000002551
PubMed Abstract | Crossref Full Text | Google Scholar
15. Contopoulos-Ioannidis DG, Karvouni A, Kouri I, Ioannidis JP. Reporting and interpretation of SF-36 outcomes in randomised trials: systematic review. BMJ. (2009) 338:a3006. doi: 10.1136/bmj.a3006
PubMed Abstract | Crossref Full Text | Google Scholar
17. Barbato B, Salsac AV. Finger and thumb replantation: from biomechanics to practical surgical applications. Hand Surg Rehabil. (2020) 39(2):77–91. doi: 10.1016/j.hansur.2019.10.198
PubMed Abstract | Crossref Full Text | Google Scholar
19. Tuzun HY, Turkkan S, Arsenishvili A, Kurklu M. A new technique for metacarpophalangeal joint replantation after four-finger amputation. Hand Surg Rehabil. (2020) 39(3):235–7. doi: 10.1016/j.hansur.2020.01.007
PubMed Abstract | Crossref Full Text | Google Scholar
21. Yoshida S, Koshima I, Narushima M, Nagamatsu S, Yokota K, Yamashita S, et al. Usefulness of ectopic implantation in multiple finger amputation injury. Clin Case Rep. (2019) 7(3):546–9. doi: 10.1002/ccr3.2040
PubMed Abstract | Crossref Full Text | Google Scholar
22. Bakhach J, Katrana F, Panconi B, Baudet J, Guimberteau JC. Temporary ectopic digital implantation: a clinical series of eight digits. J Hand Surg Eur. (2008) 33(6):717–22. doi: 10.1177/1753193408091429
PubMed Abstract | Crossref Full Text | Google Scholar
23. Yin Y, Tao X, Li Y, Bao B, Ying Y, Bao T, et al. Cosmetic and functional results of a newly reconstructed thumb by combining the phalanx of second toe and the great toenail flap transplantation. J Orthop Surg Res. (2020) 15(1):458. doi: 10.1186/s13018-020-01986-y
PubMed Abstract | Crossref Full Text | Google Scholar
24. Yu F, Xiao F, Peng G, Lin G, Wang W, Xie C, et al. Repair of distal finger soft-tissue defects with free fibular great toe neurovascular flaps. BMC Musculoskelet Disord. (2024) 25(1):479. doi: 10.1186/s12891-024-07563-2
PubMed Abstract | Crossref Full Text | Google Scholar
25. Retrouvey H, Franks A, Dunn T, Novoa K, Ipaktchi K, Lauder A. Management of self-inflicted nonaccidental amputations of the upper extremity: systematic review. J Hand Surg Am. (2023) 48(10):993–1002. doi: 10.1016/j.jhsa.2023.06.011
PubMed Abstract | Crossref Full Text | Google Scholar
AppendixA1. (A) Reconstructive preoperative x-rays; (B–D) functional reconstruction of the left demonstrative and little finger flexion under brachial plexus anesthesia with internal fixation removal; (E,F) postoperative x-rays and dressing changes show good reconstruction.
留言 (0)