Cleft lip and palate (CLP) indeed pose one of the significant challenges in craniofacial anomalies. Approximately 70% of the patients with CLP are non-syndromic, which underscores the importance of treating it as a standalone condition with a notable average incidence of 0.7 cases/1000 births.[1]
CLP is well documented, with sagittal and transverse discrepancies of the maxillary arch contributing to the characteristic facial morphology seen in these individuals. Alongside skeletal discrepancies, dental anomalies such as tooth agenesis, microdontia, and supernumerary teeth are frequently exhibited, thereby requiring specialized dental care to address.[2] Unilateral CLP is indeed the most common presentation, with a noted tendency for the left side of the orofacial structures to be affected. Over and above that, there is a slight predilection for males to be more frequently affected than females.[3]
With many technical aspects being under research, much progress has been obtained, which ameliorates the understanding and addressing of this deformity. From more sophisticated genetic studies elucidating its etiology to less mutilating surgical techniques, these advancements have contributed to boosting prevention and providing appropriate care.
Neonatal maxillary orthopedics entails early orthopedic treatment employing nasoalveolar molding, as introduced by Grayson et al. in 1999[4], which has been employed to treat infants. In older patients, surgical interventions along with orthodontic and prosthetic care are imperative. Managing a large fistula typically proves to be complex and taxing to be achieved solely through traditional local flaps.
Although the roots of modern-day protocols for distraction osteogenesis (DO) can be traced back to the pioneering work of the Russian surgeon Gavril Ilizarov, horizontal alveolar bone transport by DO was disseminated by Liou et al. in 2000.[5] More recently, internal distraction coupled with 3D surgical planning has gained popularity due to its ability to achieve precise surgical movement with superior esthetic outcomes.[6,7] Herein, this case report showcases the successful treatment of a male patient with unilateral CLP using a custom-made appliance for alveolar bone transport by DO.
CASE REPORTThis case report illustrates a 27-year-old male patient who had a history of unilateral CLP and an oroantral fistula measuring approximately 11 mm. His primary concern pertains to the restoration of missing teeth and the enhancement of facial aesthetics. The patient had previously undergone cheiloplasty at around 10 years of age and lip revision surgery at around 26 years of age, both of which were performed before seeking treatment from our team. There is no relevant history of prior palatal closure surgery performed.
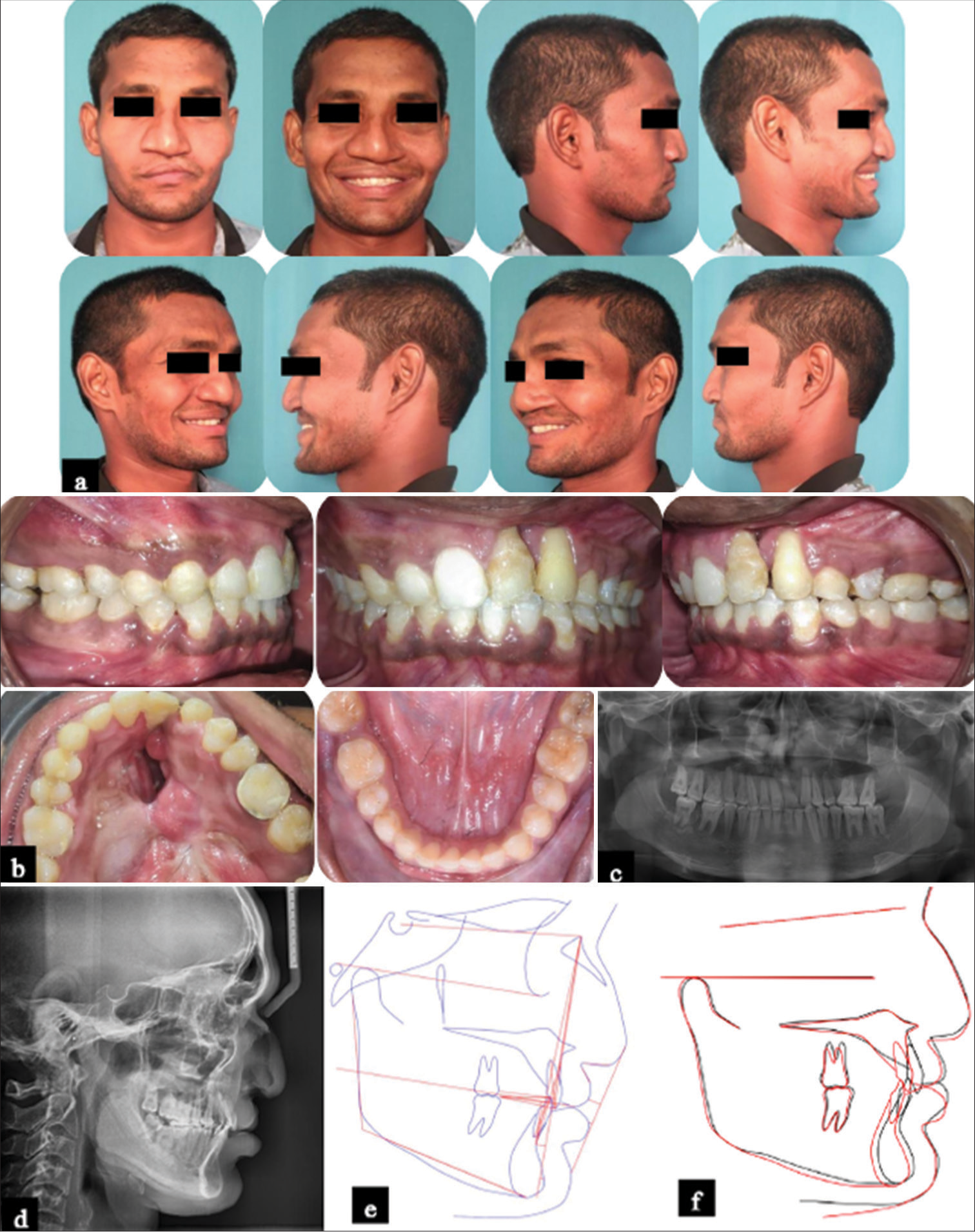
Extraorally, the patient exhibited a mesocephalic head type and mesoprosopic facial form, accompanied by evident asymmetry of the nose and upper lip and contraction scars from previous lip surgeries on the left side [Figure 1a]. A bird’s eye view revealed nasal deviation, with additional observations from a submental view indicating stretched and slumped nasal cartilage, an asymmetrical nostril with a deformed alar complex, a short columella, and an underdeveloped medial crura on the cleft side.
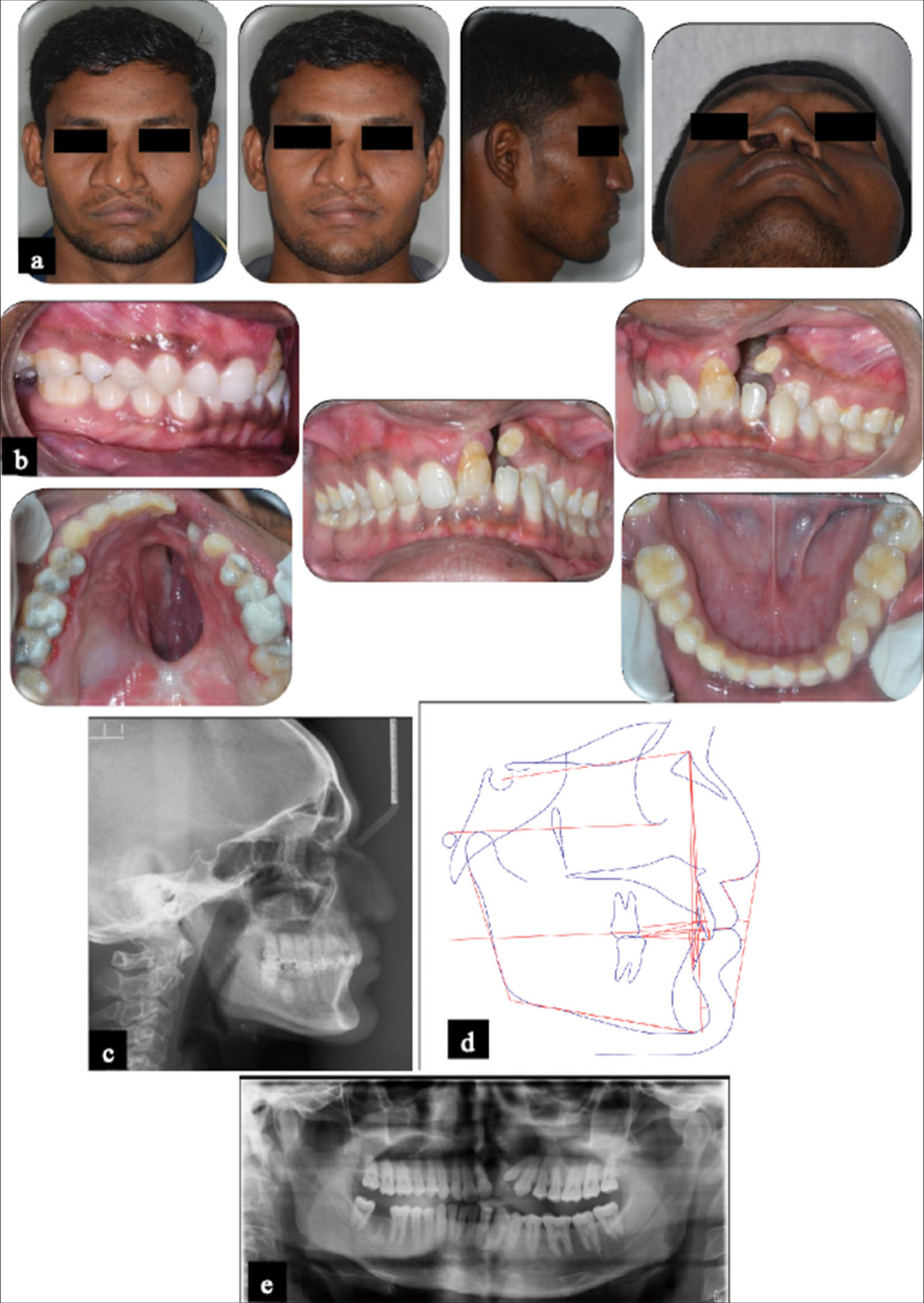
Export to PPT
An intraoral examination revealed a Class I molar relationship on both the right and left sides, with a Class I canine relationship on the right side [Figure 1b]. However, determining the canine relationship on the left side was challenging due to the presence of a cross-bite. Other pronounced findings included a reduced overjet, deep overbite, retruded maxillary incisors, and a peg-shaped maxillary left lateral incisor (22) with Grade II mobility. The mandibular incisors (11, 21, 23) exhibited lingual inclination. In occlusal view photographs, an 11 mm wide cleft was evident on the left side of the maxillary arch, coupled with a deep palatal fistula measuring 4.1 cm × 2 cm. In addition, a missing mandibular right second molar (47) was evident.
On cephalometric evaluation, the patient exhibited a Class I skeletal base (ANB-3°) with a low Frankfurt mandibular plane angle of 14° [Figure 1c and d] with retroclined upper and lower incisors. An orthopantomogram (OPG) revealed a complete unilateral cleft in the left quadrant of the maxillary arch, along with a peg-shaped tooth 22 and a missing tooth 47 [Figure 1e]. Furthermore, teeth 11, 21, and 23 exhibited mesial tipping, and there was evidence of extruded lower incisors with associated marginal bone loss.
DiagnosisIn view of the above findings, the patient was diagnosed with “Angle’s Class I malocclusion on a Class I skeletal base featuring an orthognathic maxilla and an orthognathic mandible, complete unilateral cleft with an oroantral fistula in the maxillary left quadrant accompanied by a cross-bite involving tooth 23. Other notable observations included a missing tooth 47, peg-shaped tooth 22, retroclined upper and lower incisors, and a deviated nasal septum.”
Treatment planA few different treatment alternatives exist for addressing a wide cleft defect. While prosthetic replacement combined with an obturator is one viable approach, given the patient’s age, normal mandibular position, and positive attitude, DO was adopted as the treatment. It is noteworthy that internal distractors are often better tolerated socially and psychologically in comparison to external distractors.[8] As a result, a custom intraoral alveolar distractor was developed to facilitate the transport distraction of the left alveolar segment. The distraction procedure adhered to Ilizarov’s principles, encompassing phases such as the osteotomy phase, latency phase, distraction phase, and consolidation phase.[9] Subsequently, fixed edgewise appliance therapy was initiated with the intention of correcting the remaining malocclusion factors.
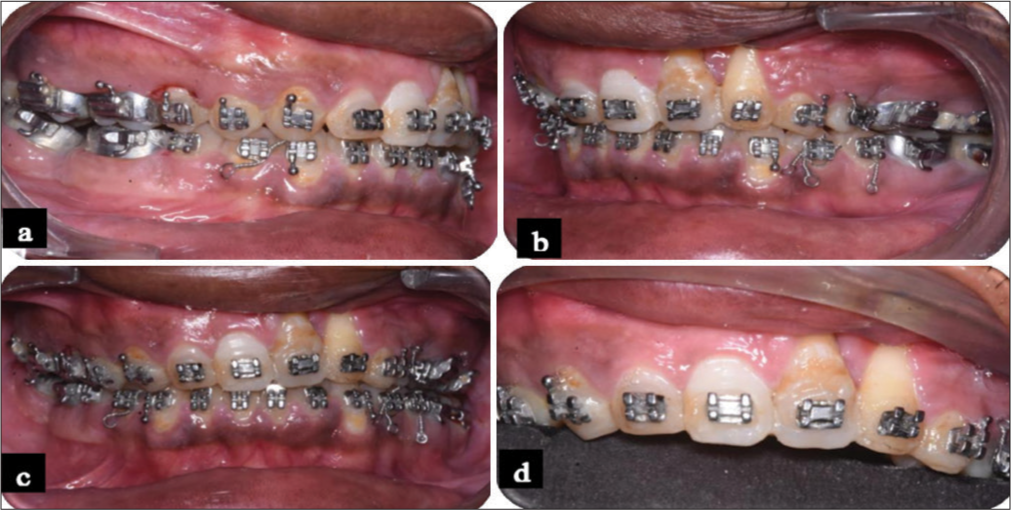
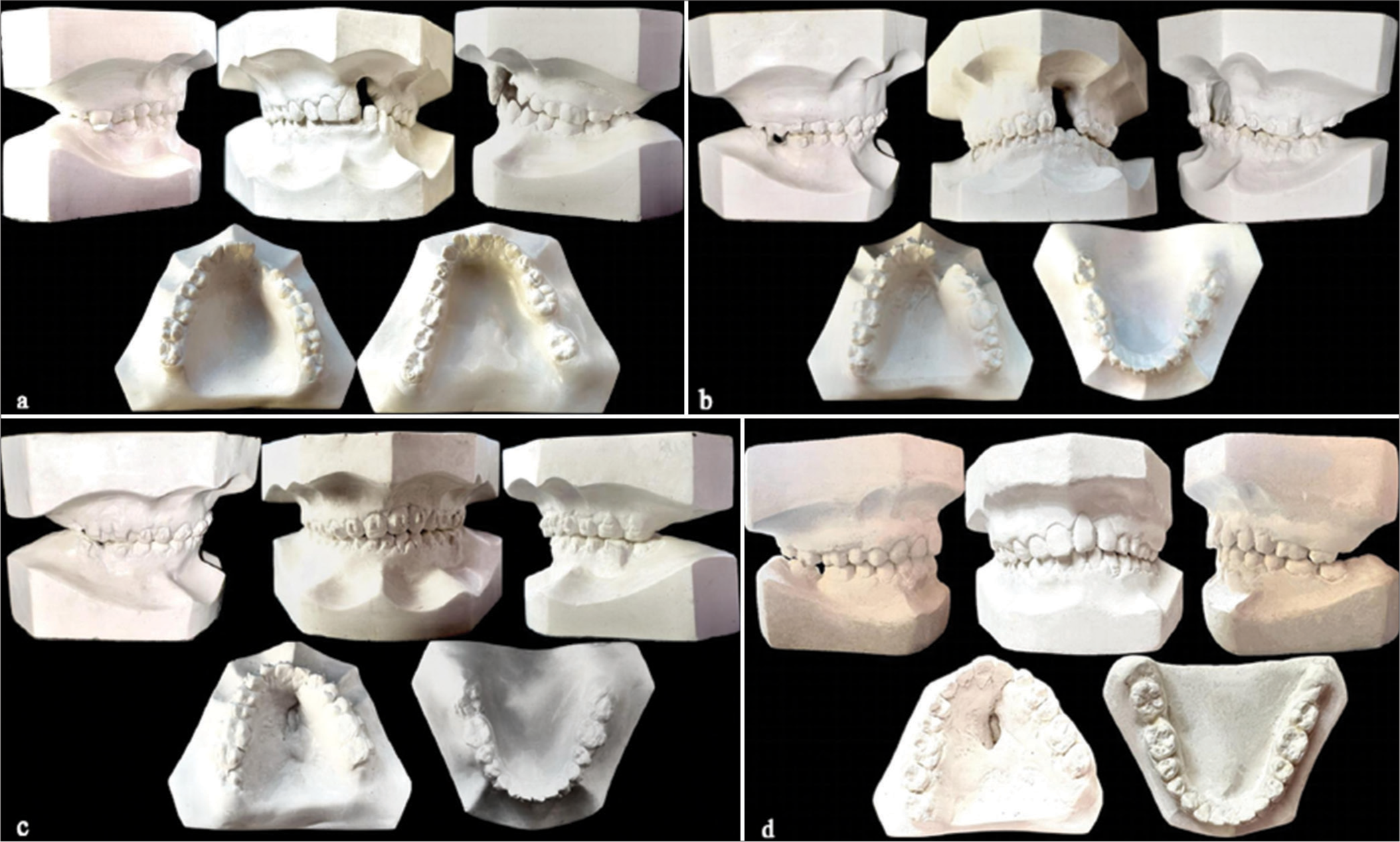
Treatment progressThe orthodontic treatment commenced with placing bands on the maxillary and mandibular first molars. In the maxillary arch, a 0.022-inch slot pre-adjusted edgewise appliance with 0.014-inch nickel-titanium wire was installed to facilitate leveling and aligning. Bite blocks were positioned in the mandibular first molars with the intention of relieving the occlusion, thereby correcting the cross-bite. Concurrently, the peg shaped lateral incisor was extracted due to the presence of Grade II mobility. Following the aligning phase, a custom intraoral distractor was meticulously crafted using a cast model and an 11 mm mini hyrax screw soldered onto custom bands in the premolar and molar to establish an anterior-posterior directed force vector [Figure 2a]. The hyrax screw was strategically installed in such a way that its anterior part was inclined downward to prevent bite opening amidst the distraction. Once the appliance was fabricated, a pre-surgical trial was performed to ensure the proper fit of the appliance [Figure 2b]. At this stage, a rigid 0.022 × 0.028 stainless steel archwire was utilized.
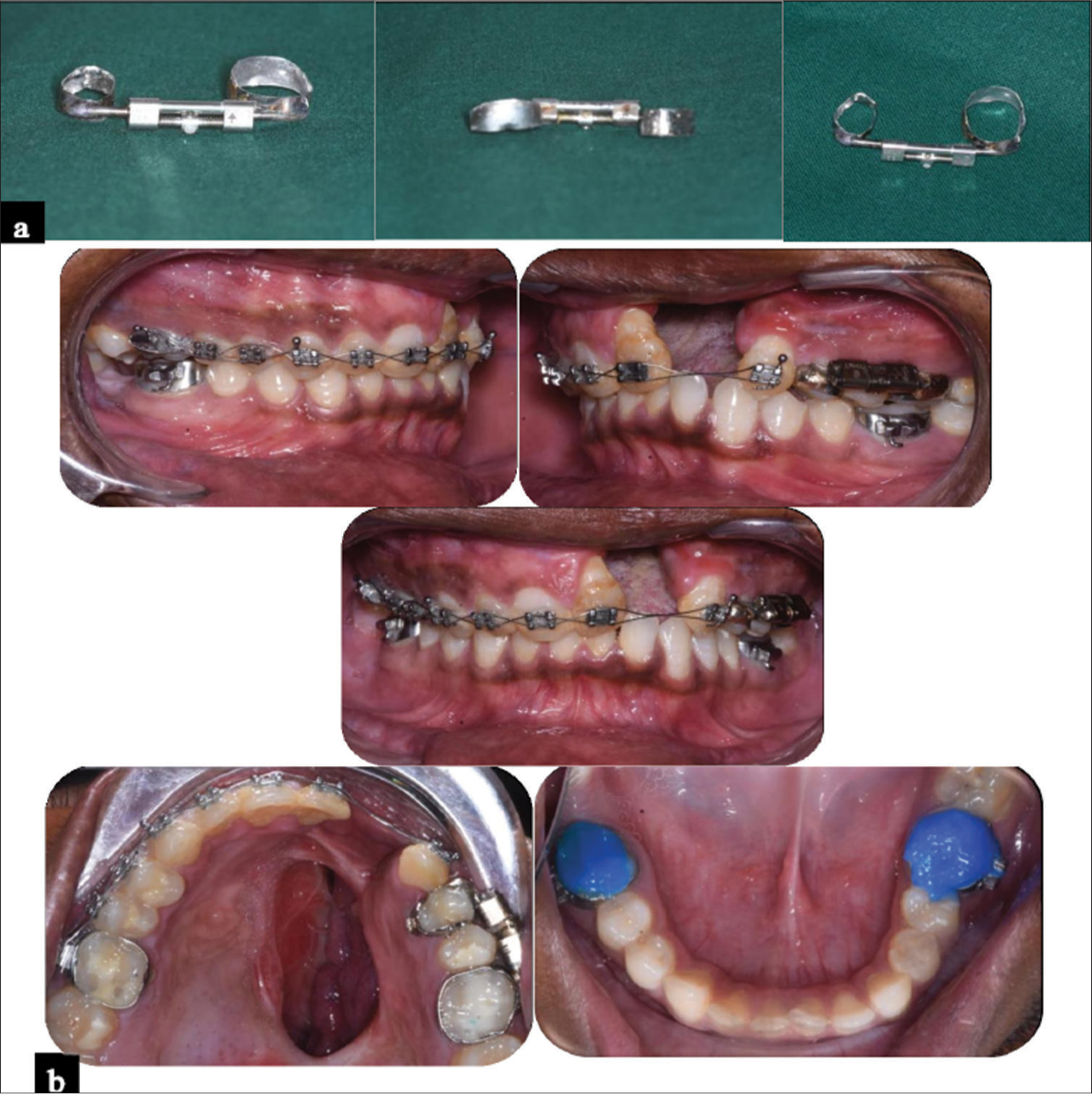
Export to PPT
In the second stage, the osteotomy phase commenced with surgery under general anesthesia. A horizontal incision was made at the level of the mucogingival junction, followed by a horizontal osteotomy extended from the apertura piriformis to the mesial end of the molars. Vertical cuts were then made on both the buccal and palatal sides between the molars and premolars, continuing through the palate to release the anterior part of the maxilla. The final part of the osteotomy preserved the palatal mucosa intact to maintain the vascularization of the anterior segment [Figure 3a]. Immediately following the completion of the osteotomies, the distractor was cemented using Type 1 glass ionomer cement (GIC). The distractor was fully closed, and the teeth in the mobile segment were bound to the posterior teeth for the latency period. Suturing was then performed, and the patient underwent a latency period lasting 5 days. Since the appliance is noninvasive, a secondary surgical procedure to remove the appliance was not warranted.
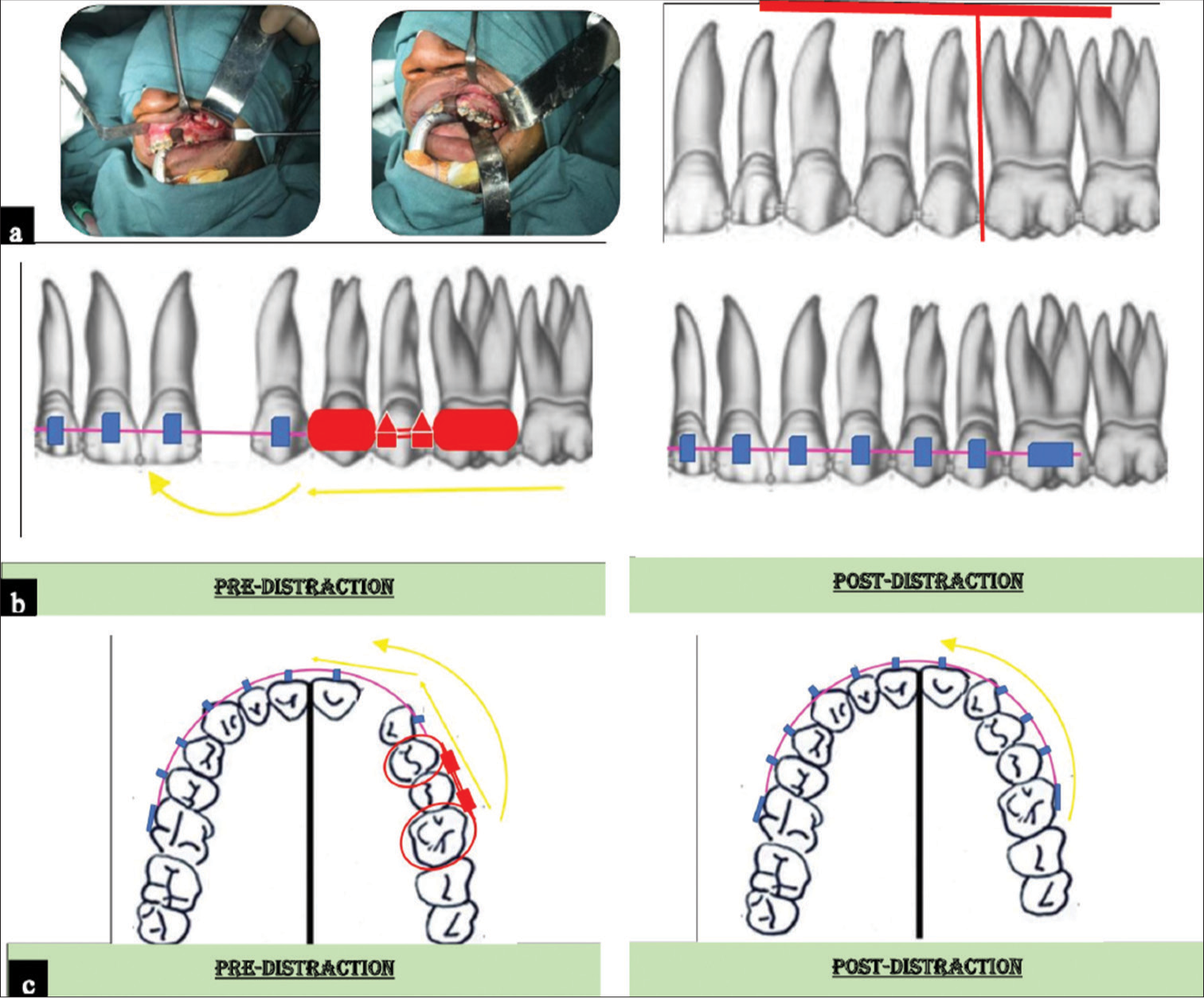
Export to PPT
During the post-latency period, distraction was initiated at a pace of 0.5 mm bidaily using an expander key guided by the rigid stainless-steel wire. Correspondingly, a total of 11 days constituted the distraction phase. The main archwire and device orientation played a crucial role in controlling the force vectors, thereby preventing arch collapse [Figure 3b and c]. The patient was monitored on alternate days, and activation was continued until achieving a normal sagittal maxillary relationship with the mandibular arch. The distraction process was completed on the left alveolar segment, establishing contact with the right segment. Simultaneously, the sagittal position of the canine was adjusted to ensure adequate overjet in the anterior region, and the oroantral fistula was observed to have significantly reduced [Figure 4a-c].
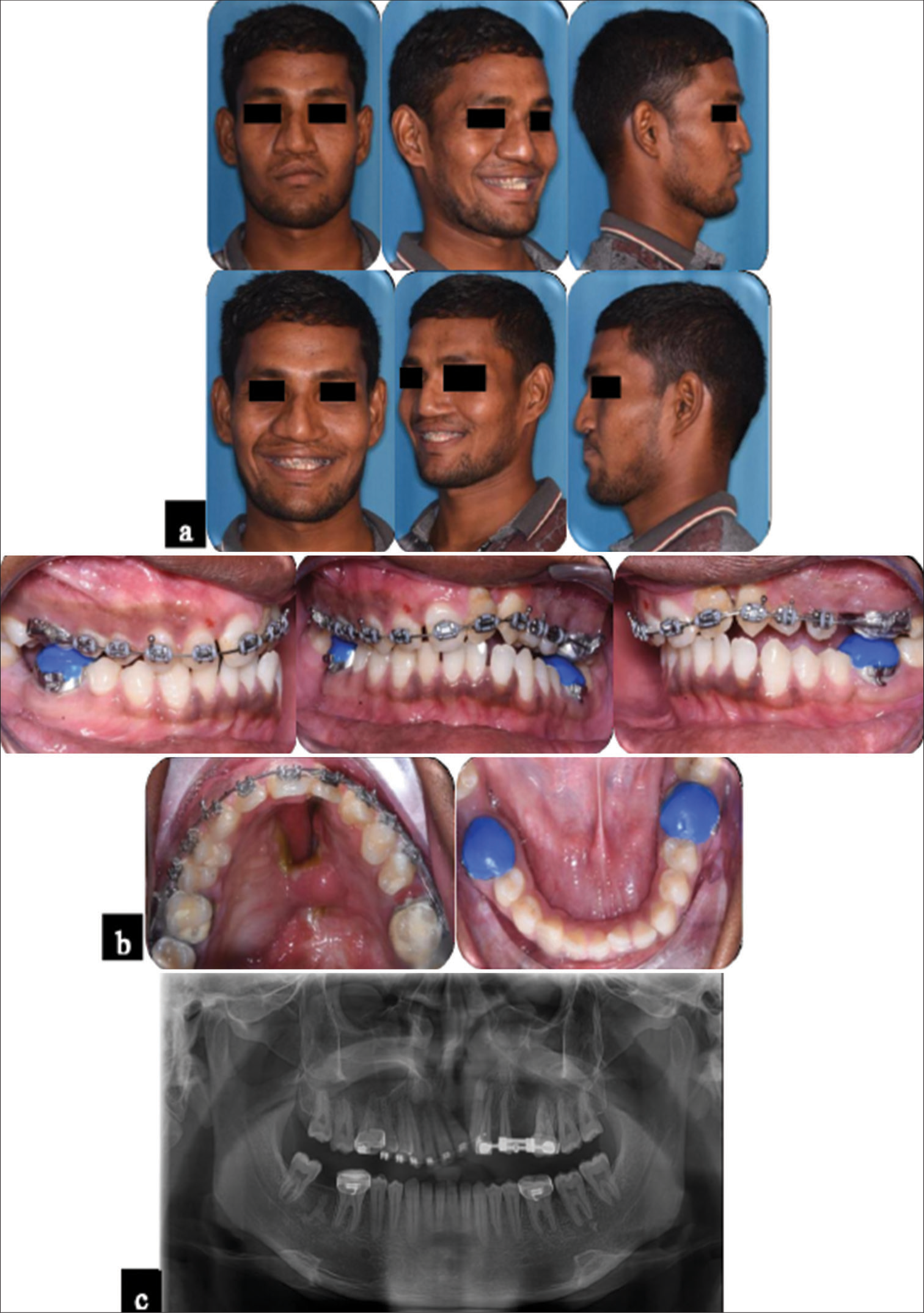
Export to PPT
Following the completion of distraction, the original appliance was left in place to facilitate the consolidation of the regenerated bone. The newly formed soft bone can be molded using elastics, and hence, Class III elastics were enjoined to promote protraction of the molar in the maxillary left quadrant. At the end of this third step, sufficient bone regeneration had occurred to address both the sagittal and transversal issues. Immediately following all the phases of the distraction, orthodontic treatment was resumed. An OPG confirmed the presence of an intact bone bridge at the termination point of the distracted segment [Figure 4c].
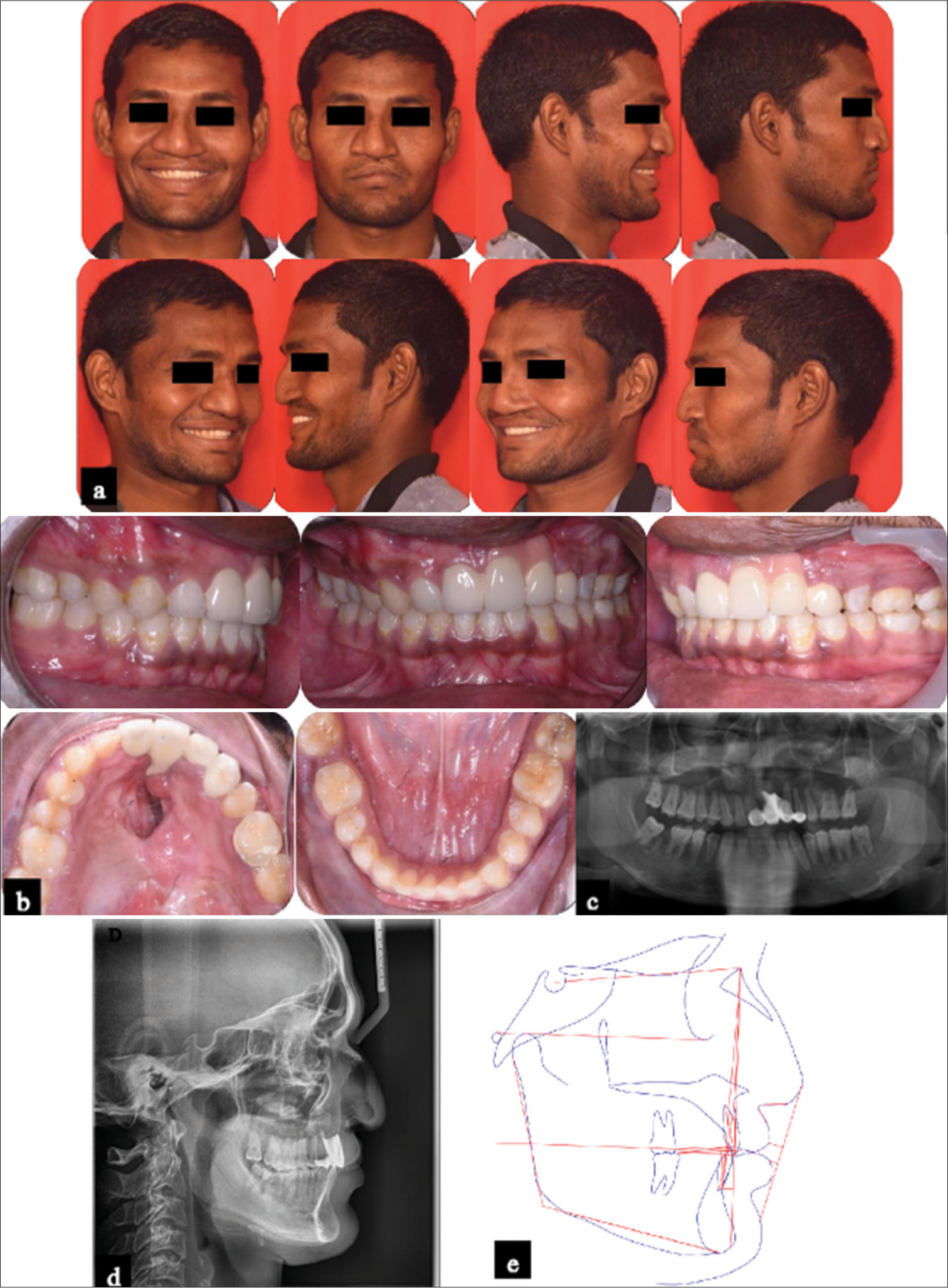
On achieving satisfactory protraction, the maxillary left anterior teeth underwent reshaping, and settling elastics were applied to achieve intercuspation [Figure 5]. On attaining proper intercuspation, orthodontic treatment was concluded, and the patient was referred to a prosthodontist for dental prosthetic intervention. Initially, temporary crowns were placed. Subsequently, a prosthetic replacement was carried out using a 4-unit fixed crown (11, 21, 23 as 22, and 24 as 23) employing ceramic crowns. In addition, full coverage with gingival pigmentation of the prosthetic crown to replicate natural gingival esthetics was employed. Finally, a beggs wrap-around retainer was fitted for both the maxillary and mandibular arches. This would cover the remaining oronasal fistula until the completion of palatal closure surgery.
Export to PPT
RESULTSThe entire treatment spanned over 15 months. At the end of the treatment, Angle’s Class I molar and canine relationships were established on the right side, while a Class II molar and Class I canine relationship was achieved on the left side [Figures 6 and 7]. Ideal overjet, overbite, and torque were attained. An OPG analysis revealed the presence of new bone formation at the osteotomy site along with satisfactory alignment of the roots. Moreover, a significant reduction in the size of the oroantral fistula was noted.
Export to PPT
Export to PPT
DISCUSSIONThe major goal in the treatment of individuals with CLP is to achieve closure of the lip, palate, and velopharynx while achieving a symmetrical profile, esthetically pleasing facial features, and proper dental alignment.[10,11] Patients presenting with wide oroantral fistula conventionally undergo approaches involving the utilization of buccal/labial mucosal flaps as well as tongue flaps.[12,13] Nevertheless, the efficacy of tongue flaps can be inconsistent and may result in complications such as failure of the flap, bleeding, swelling, discomfort, pain, necessitating multi-stage procedures, and partial or complete flap necrosis infrequently.[14] Despite successful surgical interventions, the likelihood of relapse remains high due to these factors.[15,16]
In deliberation, the application of transport DO of the alveolar segment was contemplated to address the aforementioned limitations. DO, initially introduced in craniofacial procedures by McCarthy et al. [17], saw advancements with the introduction of rigid external distraction by Polley and Figueroa.[18] Originally devised for long bone defects, mandibular defects, and temporomandibular joint reconstruction, the concept of transport DO has been adapted for the dentoalveolar region.[19,20] Here, it has been utilized for various purposes, including the reconstruction of vertical alveolar defects and addressing issues such as ankylosed central incisors, anterior maxilla advancement, expediting orthodontic treatment, and resolving dental crowding.[21-25] A transport segment derived from the posterior region of the cleft can be mobilized anteriorly, thereby narrowing the cleft. Both experimental and clinical evidence support the use of tooth-borne devices in DO. [5,26]
In this specific case report, the utilization of archwise interdental DO has been implied to bring together wide alveolar clefts and foster union across the clefts, eliminating the need for bone grafting in both unilateral and bilateral cleft cases.[5] This approach revolves around the process of distracting the dento-osseous segment formed posterior to the cleft site and narrowing the substantial alveolar defect through the medial displacement of this segment.
At the inception of formulating the archwise distraction concept, the distraction procedure was strategized to align with the archwires of the fixed orthodontic appliance. The hypothesis posits that during archwise distraction, the segment bends in accordance with the arch movement, and the newly regenerated bone calcifies in brief segments, which eventually amalgamate to create a curved shape. This produces a curvilinear pattern of distraction rather than a linear distraction.
The DO procedure comprises four sequential stages.[27] Before the osteotomy phase, a personalized tooth-borne distractor was crafted using a hyrax screw and orthodontic bands. The arms of the hyrax screw were shaped on a dental cast to align with the intended distraction vector and subsequently soldered to the bands. Before surgery, the device’s fit was clinically assessed. Following surgery, the distraction device was affixed using GIC. A latency period of 5 days was deemed optimal for the formation of primary bone callus. According to Ilizarov’s concept, the golden standard for optimal rate of distraction was established at 1 mm per day.[9] Accelerated distraction rates could induce local ischemia, potentially delaying ossification in the distraction gap. Conversely, slower rates may prompt premature ossification and consolidation. Accordingly, the distraction phase spanned a total of 11 days.
Following distraction, the device was maintained stable to ensure the successful formation of regenerated bone without cartilaginous intermediates and to prevent delayed osseous remodeling. Henceforth, the consolidation phase persisted with the appliance in place until bone remodeling was completed. Notably, there were no significant alterations in the inclination of the molar tooth or the extent of its distal movement, demonstrating adequate anchorage for transporting a segment.
Both experimental and clinical evidence support the feasibility of dental movements into newly formed bone generated by DO.[5] Hence, the maxillary left molars were readily protracted into the osteotomy site using orthodontic elastic forces. At the end of treatment, settling elastics were employed to ensure proper intercuspation.
On completion, the ultimate restorative plan aimed to employ full coverage restorations or crowns to establish teeth with a morphological shape consistent with the site that they occupied. Henceforth, a decision was made to utilize a 4-unit fixed crown, thereby substituting the canine with a lateral incisor and the first premolar with a canine. The bridge was strategically enhanced with gingiva-colored pigments to emulate the natural gingival esthetics. Subsequent imagery obtained during the 1-year follow-up period demonstrates the sustained stability of the repositioned segments and the structural soundness of the dental arches [Figure 8].
Export to PPT
Iatrogenic effects of the treatment modality to be preventedA tendency for open bite could be developed during the distraction phase. Hence, it is crucial to plan and monitor the force vectors of the distractor precisely
A scissor bite could be developed during molar protraction using elastics, and hence, it is crucial to monitor and employ correct techniques.
CONCLUSIONThe closing remarks of this case report outline the successful treatment of an adult patient presenting with a unilateral CLP alongside a wide oroantral fistula
It can be deduced that transport distraction can be accounted as an effective treatment approach when meticulously planned and diligently followed through
The interdisciplinary collaboration of orthodontic, surgical, and prosthetic procedures aids in attaining the best possible esthetic and functional outcomes
Close fraternization among team members is crucial for achieving a satisfactory outcome in such complex scenarios
A fully integrated cleft team offers lifelong, interdisciplinary, holistic treatment for patients with an oroantral cleft.
留言 (0)