The increasing share of the older population necessitates the need for proactive supportive and palliative care.[1] According to the World Health Organization (WHO), one in six people will be more than 60 years old globally by 2030, and by 2050, the population above 60 years of age is estimated to increase to 2.1 billion from 1 billion in 2020.[2] Meanwhile, among those aged 80 years and above, the population size is expected to triple by 2050 from what it was in 2020.[3] The ageing process of older adults results in increased susceptibility to deteriorating physical and mental health, non-communicable and degenerating diseases, falls and injuries leading to disabilities, dependencies and deaths.[4-6] The Lancet Commission reports that, globally, serious health-related suffering (SHS) for older adults who are more than 70 years of age will increase rapidly to up to 183% by 2060 from its estimates of the year 2016.[7] The report also states that the burden of SHS will rise even more rapidly among older adults in low-income countries.[7] The WHO estimates that 58 million people, including 25.7 million in the last year of their lives, will require palliative care every year.[8] However, only 14% of them are receiving palliative care.[8]
India is not exempt from this growth in ageing population and high supportive and palliative care needs.[9,10] According to current estimates, by 2025, India’s older population will reach 158.7 million.[11] This number will more than double to 347 million by 2050, taking a 20% share of the Indian population, accompanied by a high rise in the burden of chronic illnesses, disability and dependence in the country.[11] Consequently, there will be SHS associated with chronic diseases.[7] Palliative care is an approach that aims to reduce serious SHS.[12] However, only <2% of the Indian population has access to palliative care.[13] One of the significant challenges in access to palliative care is identifying patients with palliative care needs.[14] In India, few studies have been carried out to estimate the palliative care needs of the local population.[15-18] These estimates are based on the general population living in the micro-level localities where the older adults are not adequately represented. With the growing older population in India, there is a great need to provide palliative care estimates to develop policies and implement programs to meet their needs.
Among the different conditions that require palliative care, neurological diseases are observed to be more prevalent among the older adult age group.[19] Stroke and other neurological diseases significantly impair functional capacity and are associated with poor quality of life. However, the neuro-palliative care needs of the Indian senior population are largely unknown. This paper aims to provide a national-level estimate for palliative and supportive care needs among Indian older adults with stroke and other neurological diseases based on Longitudinal Ageing Study in India (LASI) data, a nationally representative sample survey of the Indian senior population.
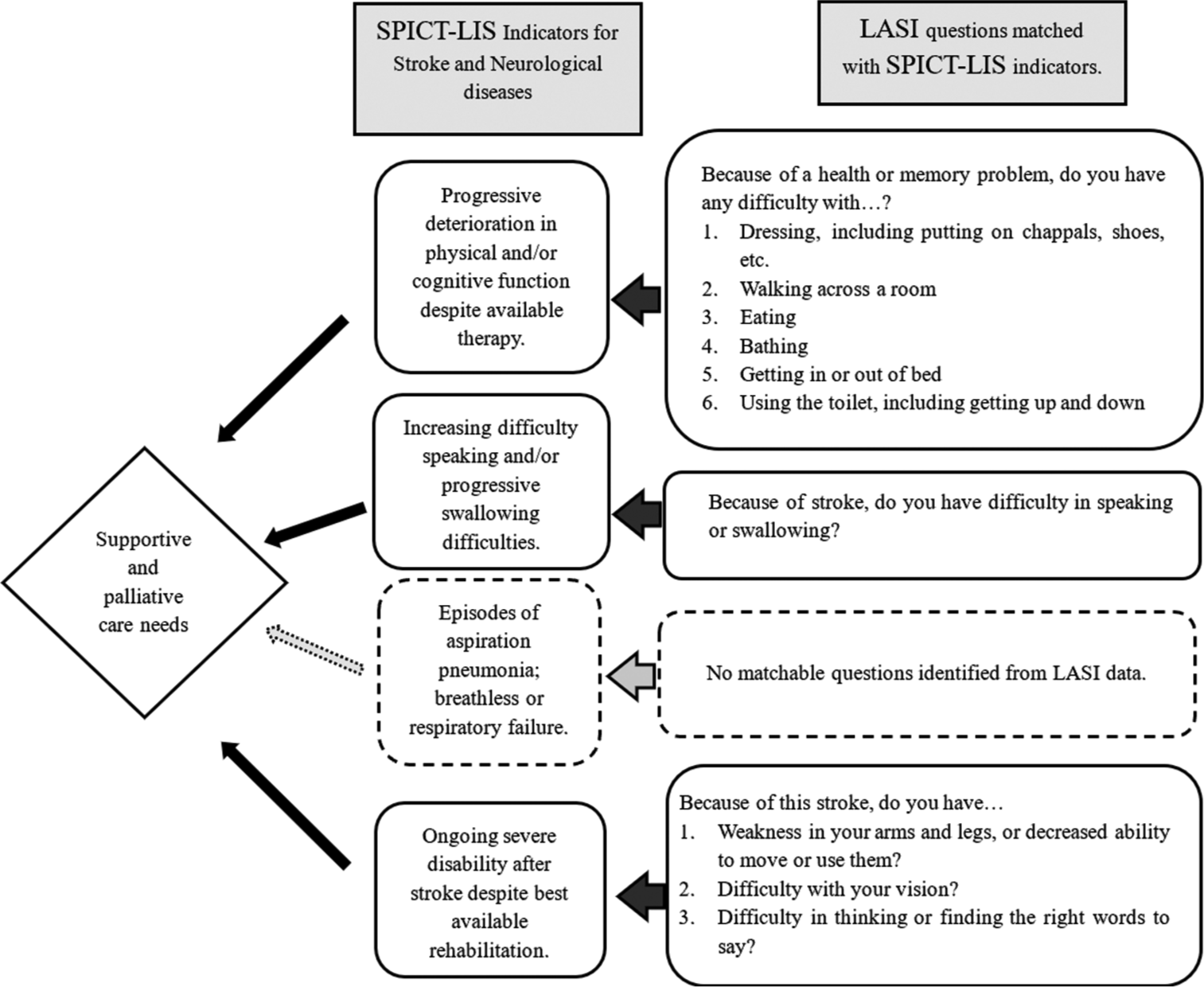
MATERIALS AND METHODSWe used the supportive and palliative care indicator tool low-income setting (SPICT-LIS), a validated instrument to identify patients with palliative care needs. The Primary Palliative Care Research Group, University of Edinburgh, developed the tool in 2010. [20,21] The tool provides general indicators of poor or deteriorating health for all patients and specific indicators for eight different health conditions to identify patients with palliative care needs. In this study, we used the indicators from ‘SPICT-LIS’ to assess the palliative requirement for stroke and other neurological conditions. Subsequently, these indicators were mapped on the survey data from LASI to identify the older adults who required palliative care for stroke and other neurological diseases.
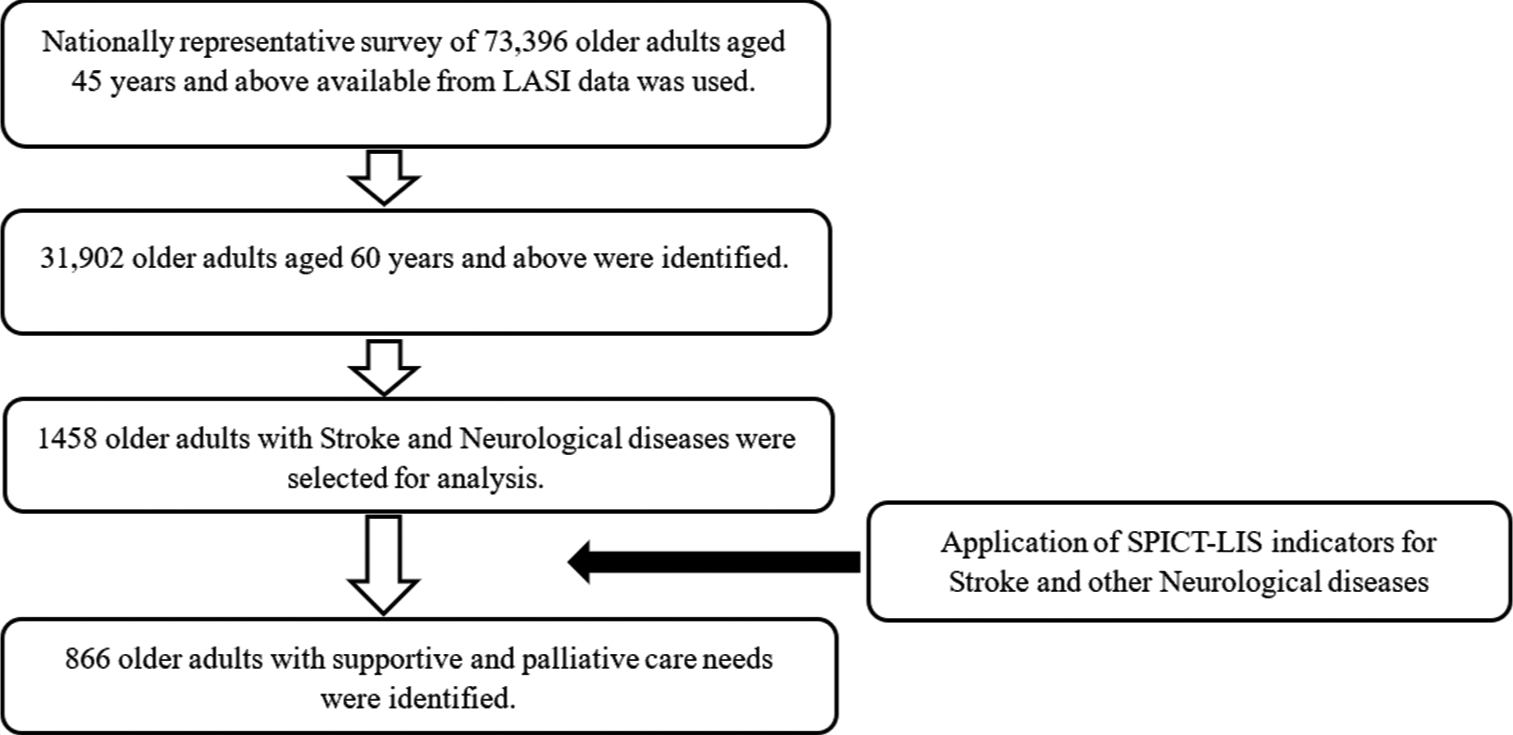
The LASI is a nationally representative survey of 73,396 older adults aged 45 and above across all states and union territories of India.[22] Although the LASI was envisioned to be a longitudinal survey to be conducted every 2 years, the first wave of the LASI survey carried out between April 2017 and December 2018 is cross-sectional in nature.[22] The survey adopted a multistage stratified area probability cluster sampling design to choose its samples. The survey used a standardised tool with quality controls to minimise non-sampling errors. The objective of the LASI was to provide comprehensive information based on demographics, economic status, chronic conditions, experience of medical symptoms, functional status, mental health (cognition and depression), health insurance status, healthcare utilisation and life expectations.[22] This study included older adults who are aged 60 years and above with stroke and other neurological diseases in the estimation process.
Figure 1 depicts the mapping of ‘SPICT-LIS’ indicators about stroke and neurological diseases with that of LASI. According to the ‘SPICT-LIS’ criteria, four indicators must be considered for the palliative requirement. The first indicator is progressive deterioration in physical and cognitive function despite available therapy that was matched in LASI data variables as the inability to perform activities of daily living such as dressing, eating, bathing and toileting due to their physical and memory problems. The second indicator of ‘SPICT-LIS’ is ‘increasing difficulty speaking and progressive swallowing difficulties’, which was mapped with the LASI variable as Having difficulty in speaking and Swallowing. Episodes of aspiration pneumonia, breathlessness or respiratory failure were the third indicator mapped with LASI data. Although shortness of breath while awake and others were available in LASI, these questions were not considered as they may not be relevant in stroke and neurological diseases. The fourth indicator of ‘SPICT-LIS’ was ongoing severe disability after stroke despite the best available rehabilitation, which correlated with persistent weakness in the arms and legs, decreased ability to move, difficulty in vision and thinking and difficulty in finding words due to stroke in LASI.
Export to PPT
From the LASI data, 31,902 older adults aged 60 years and above were identified; among them, 1458 older adults with stroke and other neurological diseases were selected for estimation and further analysis. The SPICT-LIS indicators for stroke and other neurological diseases that were mapped were then compared against the older adults with stroke and other neurological diseases, and the requirement of supportive and palliative care (yes/no) was constructed as the outcome variable [Figure 2]. Subsequently, potential background characteristics that have a determinant impact on the outcome variable were identified as independent variables. It encompassed biological (age, sex and body mass index [BMI]), social (education, income, religion, caste, living status and place of residence), morbidity profile (prevalence of hypertension, diabetes, heart disease and dyslipidaemia) as well as other risk factors (habits of smoking, alcohol and physical activity status).
Export to PPT
Statistical analysisThe study used both descriptive and inferential statistics for statistical analysis. Descriptive statistics were used to estimate the supportive and palliative care needs among older adults with stroke and other neurological diseases. Since LASI followed a multistage stratified area probability cluster sampling design, survey weights were applied during the estimation process, and all the percentages provided in the tables are weighted percentages. Chi-square tests were used to confirm the disparities in these estimates among different sub-group populations. Multivariate logistic regression (odds ratio) was used for inferential statistical analysis to identify the association between the outcome variable and background characteristics. All the statistical analyses were performed using the statistical software package STATA - SE—Standard Edition 17, developed by StataCorp and located in Texas 77845, USA (StataCorp, 2021). Missing data were not included in the analysis.
RESULTS Palliative care need among older adults with stroke and other neurological diseasesTable 1 shows that the overall prevalence of palliative and supportive care needs among older adults with stroke and other neurological diseases in India is 63.6%. In the univariate analysis, a statistically significant higher burden of palliative care needs was observed among older adults aged over 70 years (73.9%), females (67.2%), underweight (66.2%), overweight/obese (60.3%), BMI categories, older adults with primary education and below (66.5%), poorest economic category (76.5%), living alone (70.5%), low social activity (65.2%) and among older adults with hypertension (66.3%) and diabetes (63.6%) when compared against their counterparts. Furthermore, in the univariate analysis, a statistically significant lower burden of palliative care needs was observed among older adults with stroke and other neurological diseases, who engaged in vigorous (37.8%) and moderate physical activity (54.7%) compared to those who did not engage in any physical activity (67.7%).
Table 1: Biological, social, morbidity and risk factor profile of older adults with stroke and other neurological diseases in association with supportive and palliative care needs.
Description Category Sample n(%) Supportive and palliative care needs Chi-square P-value Regression analysis for Supportive and Palliative care needs AOR (CI) P-value Yes No India 1458 866 (63.6) 592 (36.4) Biological profile Age ≤70 years of age 854 (57.3) 464 (55.8) 390 (44.2) 1.00® >70 years of age 604 (42.7) 402 (73.9) 202 (26.1) 0.00 1.26 (0.96–1.66) 0.10 Sex Male 780 (50.6) 444 (60.0) 336 (40) 1.00® Female 678 (49.5) 422 (67.2) 256 (32.8) 0.03 0.91 (0.65–1.25) 0.55 BMI Normal 613 (53.5) 303 (55.5) 310 (44.5) 1.00® Underweight 207 (23.8) 123 (66.2) 84 (33.8) 1.49 (1.02–2.18) 0.04 Overweight/obese 321 (22.7) 186 (60.3) 135 (39.7) 0.01 1.39 (1.01–1.9) 0.04 Social profile Education Primary education and below 1085 (79.0) 664 (66.5) 421 (33.5) 1.00® Middle and secondary education 239 (14.0) 132 (52.9) 107 (47.1) 0.80 (0.55–1.18) 0.27 Higher secondary education and above 134 (7.0) 70 (51.6) 64 (48.4) 0.04 0.69 (0.41–1.16) 0.16 Economic Status (Based on Median Per Capita Expenditure) Poorest 241 (19.4) 164 (76.5) 77 (23.5) 1.00® Poorer 277 (20.2) 172 (66.5) 105 (33.5) 0.77 (0.5–1.2) 0.25 Middle 300 (20.8) 178 (61.2) 122 (38.8) 0.71 (0.46–1.1) 0.13 Richer 287 (20.3) 167 (62.1) 120 (37.9) 0.60 (0.38–0.94) 0.03 Richest 353 (19.3) 185 (51.5) 168 (48.5) 0.01 0.51 (0.33–0.79) 0.00 Religion Hindu 1039 (80.7) 612 (62.8) 427 (37.2) 1.00® Muslim 197 (11.6) 127 (68.2) 70 (31.8) 1.17 (0.75–1.84) 0.48 Other 222 (7.7) 127 (64.5) 95 (35.5) 0.26 0.95 (0.65–1.37) 0.78 Caste SC/ST 422 (29.7) 253 (65.4) 169 (34.6) 1.00® OBC 555 (43.8) 314 (61.7) 241 (38.3) 0.81 (0.57–1.14) 0.22 Other 419 (26.5) 261 (64.3) 158 (35.7) 0.18 1.18 (0.81–1.72) 0.40 Living status Living alone/with others 561 (42.2) 371 (70.5) 190 (29.5) 1.00® Living with spouse 897 (57.8) 495 (58.5) 402 (41.5) 0.00 0.66 (0.48–0.91) 0.01 Residence Urban 582 (29.7) 349 (63.7) 233 (36.3) 1.00® Rural 876 (70.3) 517 (63.5) 359 (36.5) 0.71 1.07 (0.79–1.44) 0.67 Health insurance No 1156 (83.6) 679 (63.5) 477 (36.5) 1.00® Yes 294 (16.4) 183 (63.9) 111 (36.1) 0.27 1.45 (1.06–1.99) 0.02 Welfare schemes Not available 972 (67.8) 588 (63.4) 384 (36.6) 1.00® At least one available 486 (32.2) 278 (63.9) 208 (36.1) 0.22 0.64 (0.49–0.85) 0.01 Social activity Low/Nil social activity 1270 (89) 788 (65.2) 482 (34.8) 1.00® High social activity 188 (11.1) 78 (50.1) 110 (49.9) 0.00 0.5 (0.34–0.74) 0.00 Discrimination No discrimination faced 1393 (96.2) 830 (63.9) 563 (36.1) 1.00® At least one discrimination faced 65 (3.8) 36 (56.3) 29 (43.7) 0.50 0.75 (0.41–1.39) 0.37 Experienced No 1237 (93.3) 688 (61.1) 549 (38.9) 1.00® Ill-treatment Yes 72 (6.8) 50 (60.4) 22 (39.6) 0.02 2.34 (1.29–4.23) 0.01 Morbidity profile Hypertension No 597 (46.4) 332 (60.4) 265 (39.6) 1.00® Yes 861 (53.6) 534 (66.3) 327 (33.7) 0.01 1.41 (1.06–1.87) 0.02 Diabetes No 1107 (79.1) 639 (63.6) 468 (36.4) 1.00® Yes 351 (20.9) 227 (63.6) 124 (36.4) 0.02 1.63 (1.17–2.26) 0.01 Dyslipidaemia No 1339 (94.3) 787 (64.0) 552 (36.0) 1.00® Yes 119 (5.7) 79 (55.9) 40 (44.1) 0.10 1.53 (0.93–2.54) 0.10 Heart disease No 1304 (89.8) 777 (64.1) 527 (35.9) 1.00® Yes 154 (10.2) 89 (58.8) 65 (41.2) 0.66 1.07 (0.7–1.64) 0.74 Feeling depressed No 893 (63.9) 490 (58.1) 403 (41.9) 1.00® Yes 426 (36.2) 253 (65.8) 173 (34.2) 0.12 1.14 (0.86–1.51) 0.38 Risk factors profile Tobacco use No 862 (55.9) 524 (64.7) 338 (35.3) 1.00® Yes 591 (44.1) 339 (62.0) 252 (38.0) 0.19 1.05 (0.78–1.43) 0.74 Alcohol use No 1162 (84.2) 701 (64.8) 461 (35.2) 1.00® Yes 291 (15.8) 162 (56.2) 129 (43.8) 0.14 0.91 (0.64–1.31) 0.63 Physical activity No physical activity 1240 (84.1) 783 (67.7) 457 (32.3) 1.00® Only vigorous 91 (6.9) 27 (37.8) 64 (62.2) 0.34 (0.2–0.58) 0.00 Only moderate 98 (6.9) 49 (54.7) 49 (45.3) 0.77 (0.46–1.29) 0.32 Both vigorous and moderate 21 (2.2) 1 (5.8) 20 (94.2) 0.00 0.03 (0.003–0.29) 0.01In the multivariate logistic regression analysis of older adults with stroke and other neurological diseases, a higher burden of palliative care need was observed among those who belonged to underweight (Adjusted odds ratio [AOR] = 1.49) and overweight/obese BMI categories (AOR = 1.39) when compared with normal weight category and among those who experienced ill-treatment (AOR = 2.34) when compared with those who did not experience ill-treatment. Among the variables in the morbidity profile, a higher burden of palliative care needs was observed among those with hypertension (AOR = 1.41) and diabetes (AOR = 1.63) than their counterparts. Interestingly, older adults with health insurance had a higher burden of palliative care needs (AOR = 1.45) when compared with older adults without health insurance.
Furthermore, in the regression analysis of older adults with stroke and other neurological diseases, a significantly lower burden of palliative care needs was observed among the older adults in the richer (AOR = 0.60) and richest (AOR = 0.51) economic groups when compared with those in the poorest economic group. Older adults who live with their spouse had a lower burden of palliative care needs (AOR = 0.66) when compared with those who live alone or live with others. Similarly, older adults receiving at least one social support scheme had a lower burden of palliative care needs (AOR = 0.64) when compared with those without any social support scheme and older adults with high social activity also had lower palliative care needs (AOR = 0.50) when compared against those with low or no social activity. In the analysis of physical activity, older adults with stroke and other neurological diseases who engaged only in vigorous physical activity and both moderate and vigorous physical activity had a lower burden of palliative care needs (AOR = 0.34 and AOR = 0.03, respectively) when compared with older adults with no physical activity.
DISCUSSIONIn the current analysis of LASI data, 63.5% of older adults with stroke and neurological diseases were identified to have supportive and palliative care needs using SPICT-LIS criteria. Although the tool specifies ‘supportive and palliative care’ in its nomenclature, in practice, both these terms are used interchangeably.[23] The WHO defines palliative care as ‘Palliative care is an approach that improves the quality of life of patients (adults and children) and their families who are facing the problems associated with life-threatening illness, through the prevention and relief of suffering by means of early identification and correct assessment and treatment of pain and other problems, whether physical, psychosocial or spiritual.[8]’ The National Cancer Institute defines supportive care as ‘care given to improve the quality of life of people who have an illness or disease by preventing or treating, as early as possible, the symptoms of the disease and the side effects caused by treatment of the disease. Supportive care includes physical, psychological, social and spiritual support for patients and their families.[24] These definitions show that the goal of supportive care and palliative is to improve the quality of life, and they also follow similar processes to achieve this goal.
In stroke and other neurological diseases, there is a significant loss of function, increased dependence and cognitive impairment in comparison with other chronic diseases, and these reasons contribute to high supportive and palliative care needs in these patients.[25] In the sub-group analysis, several variables in the biological profile, social profile and risk factor profile were found to be associated with supportive and palliative care needs. In the trajectory of neurological diseases, the demand for supportive and palliative care needs increases with advancing disease and age. [25,26] In this current study, 74% of those more than 70 years of age with stroke and other neurological diseases required palliative care. The changes associated with advancing age, such as increasing frailty, cognitive impairment and declining functional status along with progressive neurological disease, cause and accelerate these impairments, resulting in a higher burden of palliative care needs in these individuals.
In the present study, both the underweight and overweight/obese categories had a higher burden of palliative care needs. This was observed in both univariate and multivariate analysis. Studies show that older adults who are underweight have lower life expectancy and lower functional status when compared with older adults who have normal weight,[27] and malnutrition also plays a role in the development of geriatric syndromes.[28] Furthermore, being underweight is an indicator of poor and deteriorating health in the supportive and palliative care indicator tool general criteria. With regard to overweight/obese individuals, the presence of multiple morbidities, functional impairment, malnutrition and accelerated decline in health status could be the possible explanation for higher palliative needs among them.[29] Although the palliative and supportive care need is high in this population, it is essential to note that the actual utilisation of palliative care services is less among obese individuals when compared with normal-weight individuals, and this poor utilisation among obese individuals is associated with adverse outcomes such as higher expenditure and institutional deaths.[30]
In the current study, 6.8% of older adults with stroke and other neurological diseases reported experiencing ill treatment. In the regression analysis, higher palliative care need was observed among the older adults who reported experiencing ill-treatment. Elder abuse is not just a social problem but also a public health problem. Increased vulnerability, dependence and caregiver stress in the context of life-limiting illnesses are crucial factors in abuse.[31,32] As palliative care seeks not only to improve the quality of life of patients with life-limiting illnesses but also to address caregiver burden, anxiety and stress, it can play a major role in addressing this problem.[33,34] Among the morbidity profiles, the presence of hypertension and diabetes was found to be associated with higher supportive and palliative care needs in the regression analysis. Hypertension is known to cause end-organ damage, resulting in stroke, heart failure, renal failure and vascular diseases;[35] Similarly, the complications of diabetes follow a similar disease trajectory.[36] Both hypertension and diabetes are prevalent comorbidities with other chronic conditions and a significant predictor of stroke and may be the reason for their association with supportive and palliative care needs.[37]
The economic category of older adults with stroke and neurological diseases emerged as a significant factor associated with supportive and palliative care needs. The burden of palliative care needs among the richest economic quintile was 51.5%, but among the poorest economic quintile, it was 76.5%. A similar trend was also confirmed in the multivariate analysis. In a study conducted among individuals with palliative care needs in five Asian countries, including India, where individuals from lower socioeconomic categories were observed to experience greater suffering in several domains.[38] The WHO also estimates that 76% of those who need palliative care live in low-middle-income countries, and the highest proportion of need is among low-income countries.[8] These findings suggest that palliative care needs are strongly influenced by economic status.
In the current study, the burden of supportive and palliative care needs was observed to be lower among older adults with stroke and neurological diseases who received support from social welfare schemes and whose social activity levels were high. Several studies show that social support for older adults with palliative care needs produces a better quality of life, health status, satisfaction and mental well-being. [39-43] Like social support, studies also show that social activity among older adults reduces mortality and institutionalisation and improves the health status of older adults. These reasons could explain the lower burden of palliative care needs among them. Furthermore, among older adults with stroke and other neurological diseases, the burden of palliative care needs was observed to be lower among those who engage in vigorous physical activity or both moderate and vigorous physical activity. Among those with stroke or other neurological diseases, physical activity and physical rehabilitation play a significant role in preserving and improving functional ability. [44,45] These findings underscore the importance of improving awareness and access to physical rehabilitation services for older adults affected by stroke and other neurological diseases.
Strengths and limitationsThis is the first study to estimate supportive and palliative care needs in India using a nationally representative sample. SPICT-LIS, a validated instrument in identifying individuals with supportive and palliative care needs, is another merit of this current study. Since the study used a nationally representative sample of the older Indian population, the results have good external validity. Nevertheless, the non-availability of an indicator considered for palliative care needs by SPICT-LIS, like episodes of aspiration pneumonia, breathlessness or respiratory failure in the LASI data, maybe a limitation of this study. The actual palliative estimation, therefore, may be slightly higher than the present estimation. The limitations of the LASI survey apply to the current paper. These include respondent fatigue because of lengthy surveys and local dialect challenges during survey administration.
CONCLUSIONThe supportive and palliative care needs among the older population with stroke and other neurological diseases in India are high. The findings of this study underscore the importance of screening for supportive and palliative care needs among patients with stroke and other neurological diseases to identify these unmet needs. The palliative care needs in this group are influenced by their BMI status, economic category, the experience of ill-treatment, comorbid conditions, social support, social engagement and physical activity. As the proportion of older adults is estimated to double in the next three decades in India, the workforce trained in the provision of generalist and specialist palliative care will be required to meet the growing supportive and palliative care needs of the country.
留言 (0)