Low back pain is the foremost musculoskeletal condition affecting people’s activities of daily living, causing lost wages and workplace disability. The estimated economic costs of low back pain in the United States are upward of $100 billion (Katz, 2006; Vos et al., 2012; Hoy et al., 2014). Low back pain with associated sciatica is commonly caused by mechanical compression from a herniated intervertebral disk on a lumbar spine nerve root (Meng et al., 2022). Sciatica can present with a neurological motor deficit of the lower extremity, manifesting as an inability to dorsiflex the foot (Cox, 2011). A patient diagnosed with discogenic sciatica with a lower extremity motor deficit may require interdisciplinary input, such as a neurosurgical consultation, as a progressive neurological deficit is one of the key indicators for surgical intervention (Sharma et al., 2012; Wielechowski et al., 2020).
The purpose of this case report is to discuss how measuring the forces and movements of a force-based Cox Technic flexion distraction decompression (CTFDD) spinal manipulation along with other modalities may be of clinical benefit. Furthermore, it discusses how CTFDD, along with other modalities, can be an alternative, non-surgical treatment for sciatica originating from an L4–L5 disk herniation.
MethodsForce-based CTFDD is a low-velocity, variable-amplitude form of spinal mobilization. Research documents the biomechanical effects of CTFDD on the lumbar spine, including increased intervertebral disk space heights, decreased intradiscal pressure, and increased vertebral foraminal area (Cox, 2011; Gudavalli et al., 2022, 2023). CTFDD uses the Cox 8 Force Table (C8FT) that can simultaneously flex and distract the lumbar spine while applying equal bi-directional distraction forces. The distraction forces measured by the C8FT are cephalad hand force (HF) and caudalward Long y-Axis Force (LyAF), both displayed in pounds (Cox, 2011). The caudal section movements of the C8FT are lateral flexion and flexion angle, which are measured in degrees. The CTFDD data are collected by force transducers located in the C8FT, then imported to a computer and shown as force and motion graphs. The CTFDD force and motion data can then objectively guide CTFDD treatment parameters by monitoring the bi-directional manipulative forces as noted by patient tolerance and decreasing spinal resistance (Jun et al., 2020; Amjad et al., 2022). CTFDD spinal manipulation has two basic treatment protocols, protocol 1 and protocol 2. Prior to administering any CTFDD treatment protocols, the patient is always tested for tolerance to ensure treatment viability. Tolerance testing prior to CTFDD is important in ensuring a successful clinical outcome. Protocol 1 is for sciatica patients and consists of three sets of five cycles of equal cephalad HF and caudalward LyAF. Protocol 1 is primarily used for disk decompression (Cox, 2011). Upon achieving 50% clinical improvement and a reduction of sciatic leg pain, the patient would be transitioned to protocol 2. Protocol 2 consists of 1 set per spinal movement consisting of 10 cycles of equal distractive HF and LyAF applied in flexion, lateral flexion, and circumduction (Cox, 2011). Protocol 2 is used for disk decompression and spinal mobilization.
Equal-force bi-directional traction (EqFT) used in this treatment plan is a force-based form of traction evolved from the CTFDD treatment protocols. Using a pre-set distractive distance on the C8FT, the objective for the treating doctor is to apply an equal amount of counter HF against the LyAF being generated by the C8FT, thus applying equal bi-directional traction forces. The application of EqFT is dictated by patient tolerance (Figures 1, 2 and Tables 1– 3). EqFT is a prime example of the need for interdisciplinary force-based spinal manipulation research to develop new and innovative treatment protocols, such as EqFT, to improve clinical outcomes for the treatment of low back pain (Reed et al., 2024).
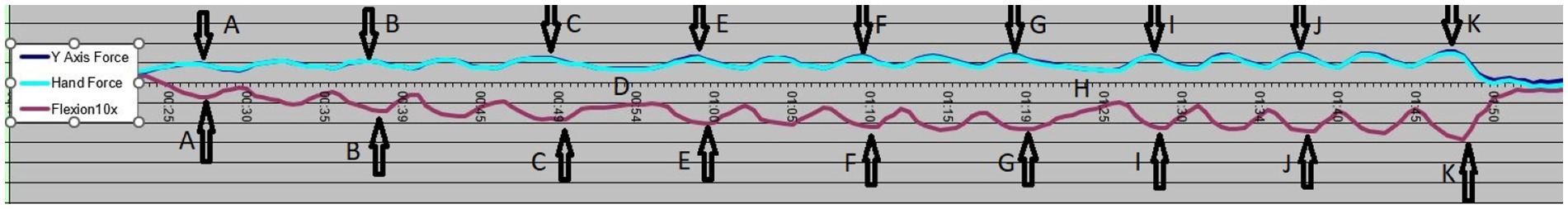
Figure 1. Protocol 1 graph with bi-directional forces and flexion angle values indicated.
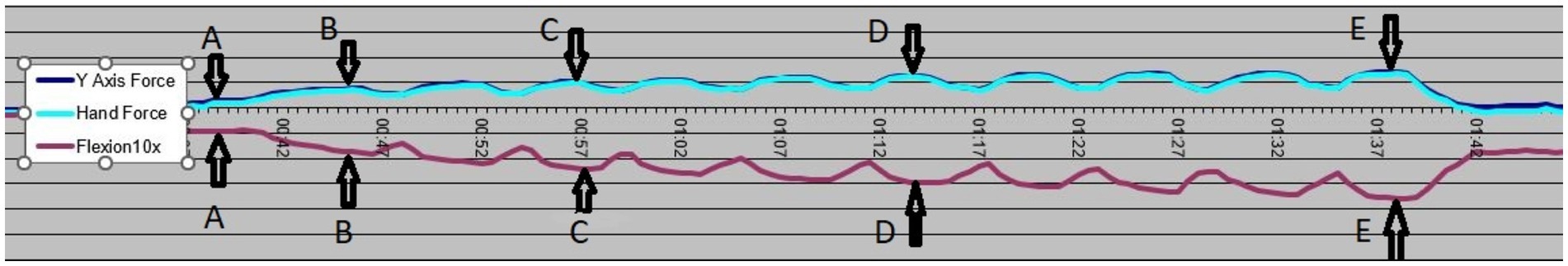
Figure 2. Protocol 2 - flexion graph with bi-directional forces and flexion angle values indicated.
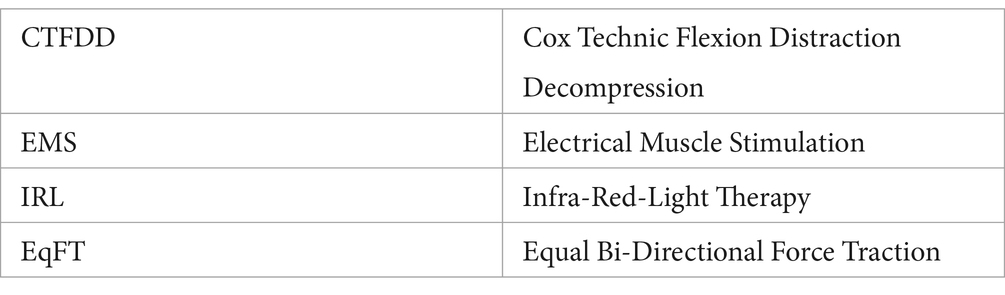
Table 1. Treatment Abbreviations.
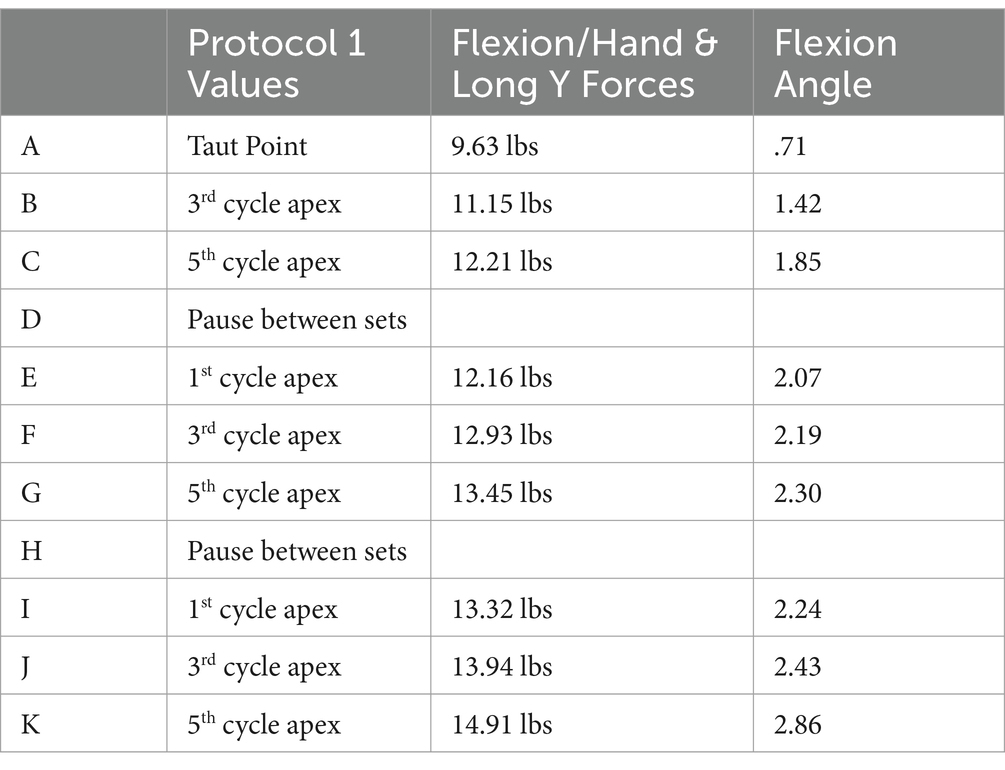
Table 2. Forces and flexion angle at different treatment points for protocol 1.
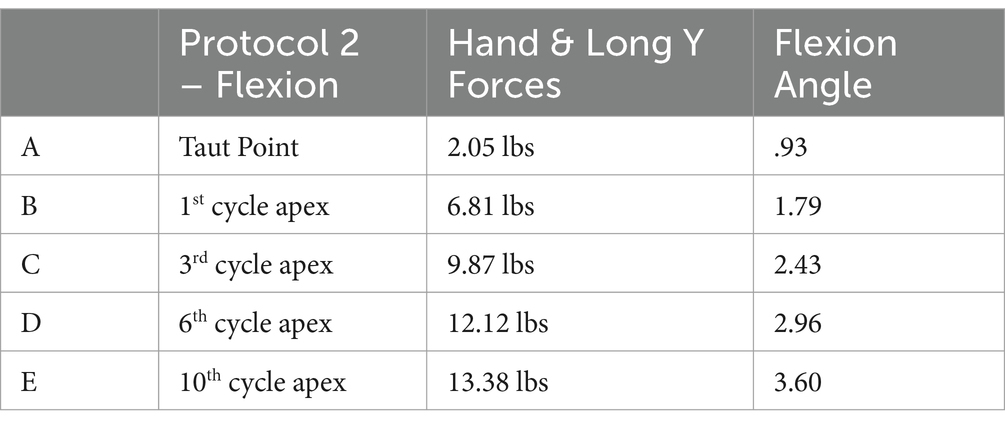
Table 3. Forces and flexion angles at different treatment points for protocol 2.
Patient informationA 59-year-old woman sought chiropractic treatment for the management of sciatica and an inability to dorsiflex the left foot. This condition was described as having a dull, achy, burning pain at the lower left lumbar spine which radiated into the left lateral thigh and then into the left lower extremity and left foot. The left foot was described as having tingling, numbness, and weakness. This sciatica condition began 4 months prior to this initial examination and developed 2 weeks after undergoing right knee joint replacement surgery while performing a post-operative home rehabilitation program. The patient rated the pain as constant 5 of 10 on a numeric pain rating scale, with 0 representing no pain and 10 representing excruciating pain. Initially, the pain was rated at a constant 8 of 10, but it decreased to a constant 5 of 10 following prior treatment. The patient scored 26 on a low back pain (Revised Oswestry) outcome assessment. The patient described the pain as chronic (ongoing for 20 weeks) in duration and without any prior history of the present condition. The patient’s activities of daily living were limited due to low back pain and an inability to feel and dorsiflex the left foot. The patient had difficulty lifting weights, walking, sitting, standing, and traveling. The initial treatment for this sciatica condition was rendered by the orthopedic surgeon who performed the right knee replacement surgery. This treatment consisted of prescribing prednisone and a referral for physical rehabilitation. Physical rehabilitation consisted of stretching, cardiovascular exercise, and a core strengthening program. Subsequently, the patient presented to a pain management physician, who administered a series of epidural injections, and then to a neurosurgeon, who recommended spinal decompression surgery. Chiropractic treatment using HVLA spinal manipulation was also rendered. This form of spinal manipulation showed no improvement, so this chiropractor referred the patient for force-based CTFDD spinal mobilization. The patient’s past health history includes hypothyroidism, type II diabetes, and right knee joint replacement surgery (Tables 1, 4).
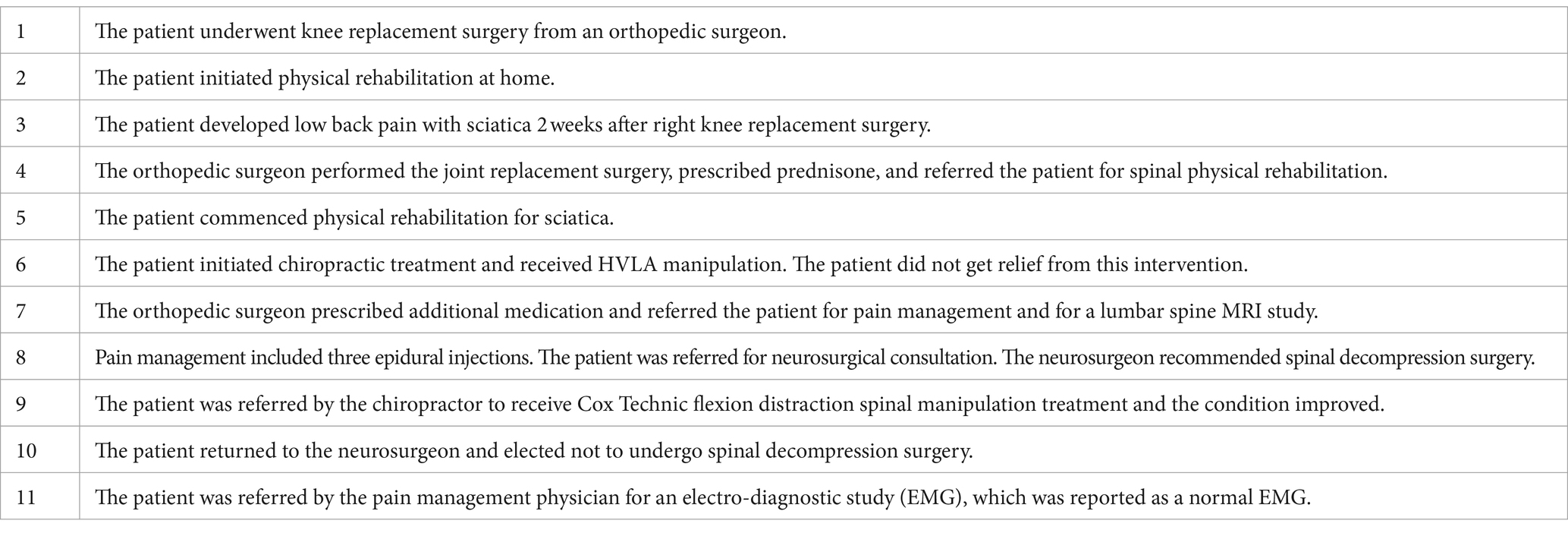
Table 4. Chronological order of prior treatment.
Clinical findingsThe patient is 5′5″ tall, weighs 190 pounds, and demonstrated a limping gait due to numbness and weakness in the left foot. The lumbar spine ranges of motion were measured with a digital goniometer: right lateral bending at 20° with pain, left lateral bending at 20° with pain, and extension at 15° with pain. Flexion measured at 75° with mild pain. An orthopedic examination demonstrated the following positive tests: Bechterew’s test (left leg), SLR test (left leg at 35°), Kemp’s test (bilaterally), Nachlas’ test (left), and prone lumbar flexion (bilateral). These findings suggest a disk lesion, large disk herniation, or nerve root compression. Additionally, Braggard’s test (left leg) and medial hip rotation (left leg) both suggest sciatica. Manual muscle strength testing of the lower extremities, which included plantar flexion, hallux flexion, gluteus maximus, biceps femoris, and quadriceps femoris, were within normal limits and graded at 5/5 bilaterally. Dorsiflexion and hallux extension of the right foot were within normal limits and graded at 5/5. Dorsiflexion and hallux extension of the left foot were reduced and graded at 1/5. Deep tendon reflexes of the lower extremity revealed that the patellar reflexes were rated +2 bilaterally, while the Achilles reflexes were rated +1 bilaterally. Muscle spasms and tenderness were noted upon palpation of the left lumbar para-spinal musculature (L4 and L5 levels), left gluteus maximus, left piriformis muscle, left hamstring musculature, and the left popliteal fossa. The patient’s MRI images (Figure 3) showed no disk bulge or herniation, and no significant central canal or foraminal stenosis was found at the L1-L2, L2-L3, L3-L4, and L5-S1 levels. The L4-L5 level demonstrates disk bulging with a left foraminal disk herniation. A free fragment of disk material is noted at the posterior superior L5 vertebral body. The left ligamentum flavum shows hypertrophy compared to the contralateral side. Mild bilateral facet osteoarthritis is seen, with a trace of effusion at the right facet joint.
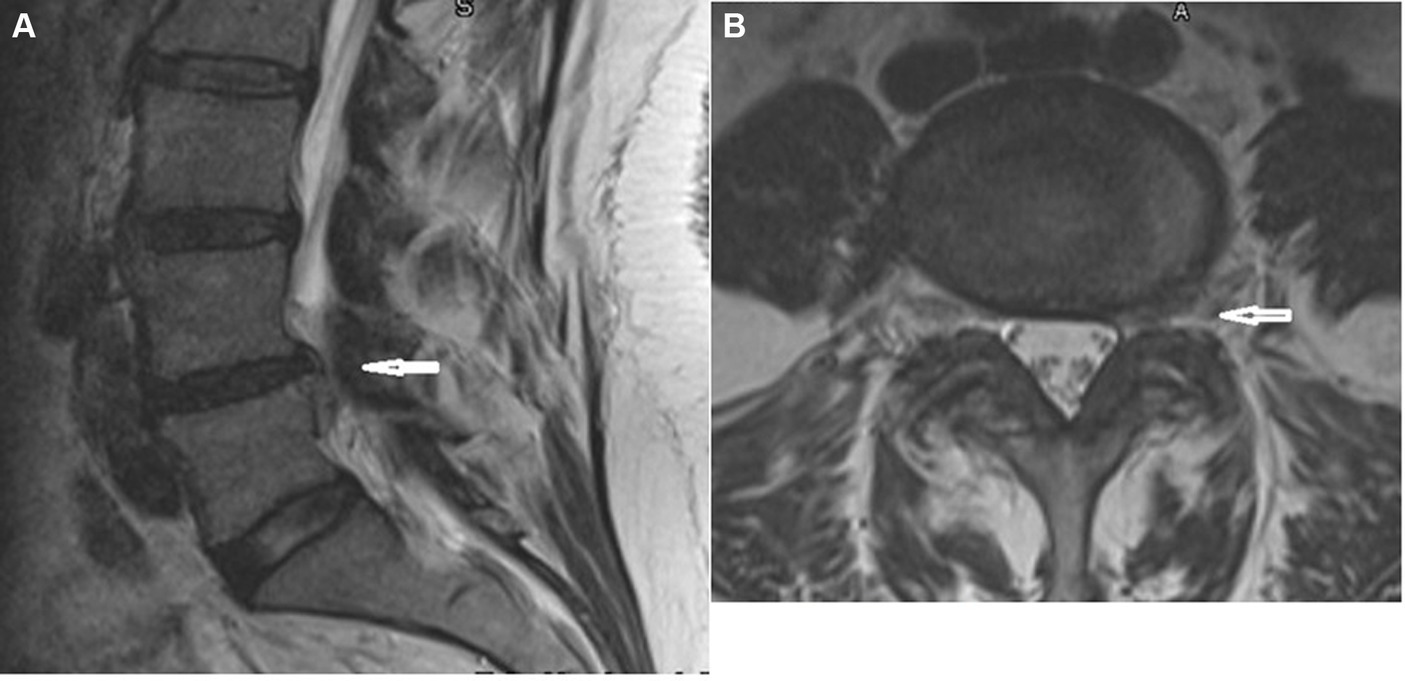
Figure 3. MRI of lumbar spine. (A) Sagittal view. (B) Axial view L4–L5.
Diagnostic assessmentBased on the subjective complaints of this patient, objective clinical findings from the orthopedic and neurological examinations, and a positive lumbar spine MRI study, a diagnosis of discogenic sciatica with a sequestered disk fragment at L5 and a motor deficit in the left lower extremity was rendered.
Therapeutic interventionA treatment plan consisting of force-based CTFDD spinal manipulation and EqFT for 1 min 45 s was used as a per-manipulative treatment to reduce spinal stiffness (Jun et al., 2020) (Figures 1, 2), pre-modulated electrical muscle stimulation (EMS) was applied for 7 min to the affected area to provide temporary pain relief, and 12 joules of infrared light therapy (ILT) were administered at the L4–L5 level to potentially reduce inflammation (Tables 2, 5). A home exercise program consisting of a stretching and strengthening program targeting the lumbar spine and left foot dorsiflexion, ice applications, and lifestyle modifications restricting bending and lifting was also instituted. A treatment schedule of three treatments per week for 4 weeks was initiated with the expectation of achieving 50% subjective and objective clinical improvement. Upon achieving 50% clinical improvement and reduced sciatica pain, the treatment schedule would be reduced until achieving maximum medical improvement. Subjective improvement would be measured by low back pain (Oswestry Revised) outcome assessment form and the numeric pain rating scale. The objective clinical improvement would be measured by an orthopedic/neurological re-examination using measured lumbar ranges of motion, a straight leg raise test, Braggard’s test, Kemp’s test, and manual muscle strength testing of left foot dorsiflexion. Left foot dorsiflexion will be tested at every visit to monitor muscle strength improvement. To apply force-based CTFDD spinal manipulation, a C8FT was used. The C8FT (Model #s – 16201700, 16501702, 16201699, Haven Innovations, Michigan, United States) has sophisticated force cell technology built within its cushions. These force cells are configured to accurately record the treatment forces in pounds applied during a CTFDD spinal manipulation. Additionally, the movements of the caudal (lower) section of the table of flexion and lateral flexion are recorded in degrees. Using the C8FT gives the advantage of acquiring objective treatment forces and motion data ensuring accuracy, consistency, and reproducibility of the CTFDD spinal manipulation (Gudavalli and Cox, 2014). The uniqueness of CTFDD spinal manipulation is the application of equal bi-directional forces of cephalad HF and caudalward long y axial force (LyAF) (Cox, 2011). Initially, the patient was tolerance tested for treatment viability, and then CTFDD protocol 1 was applied to this patient’s lumbar spine to treat sciatica (LyAF) (Cox, 2011) (Figures 1, 2). Upon achieving 50% clinical improvement and a reduction of sciatic leg pain, the patient was transitioned to protocol 2 (Figure 4 and Table 6) (Cox, 2011).
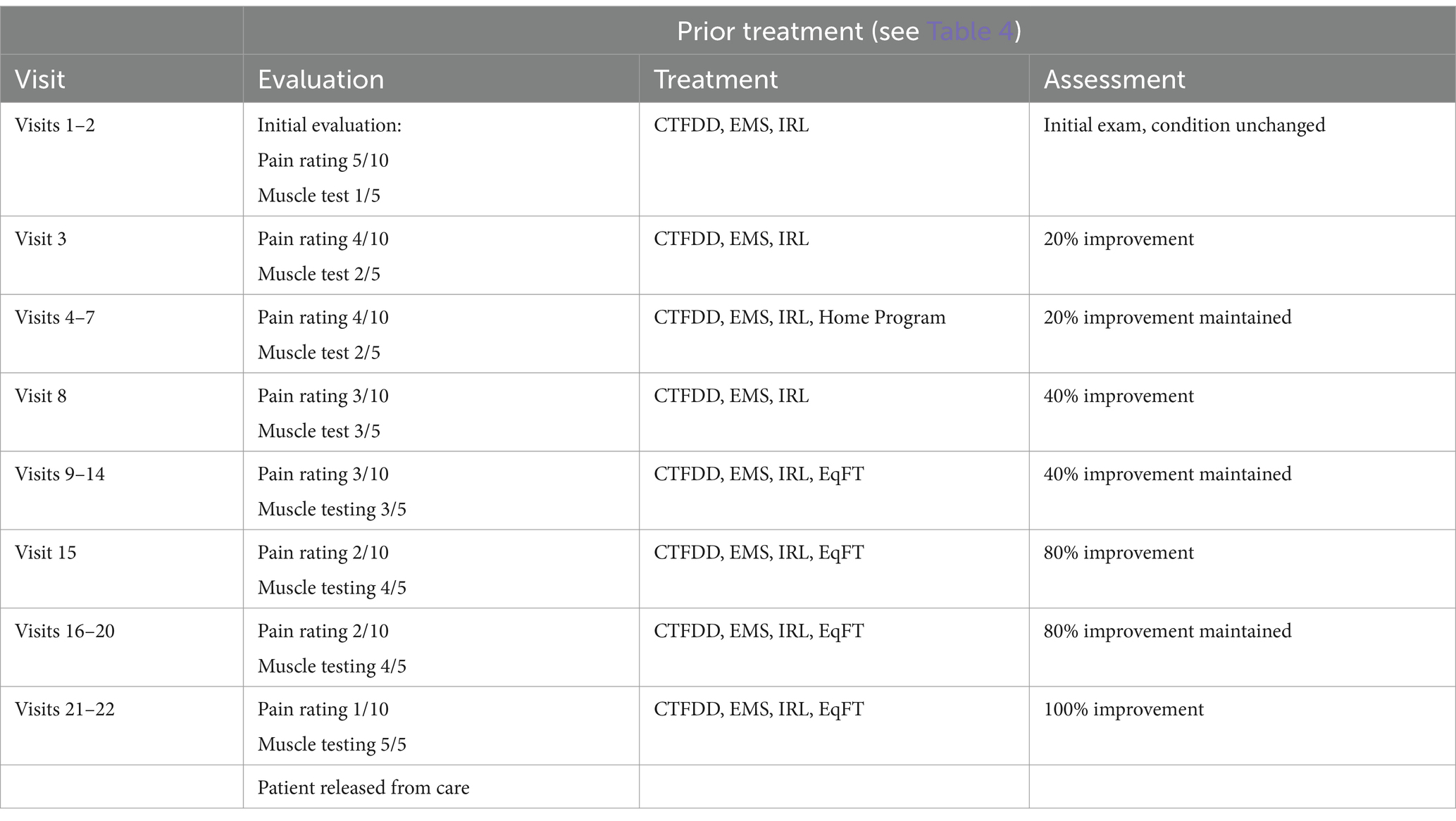
Table 5. Treatment schedule for CTFDD spinal manipulation treatment plan.
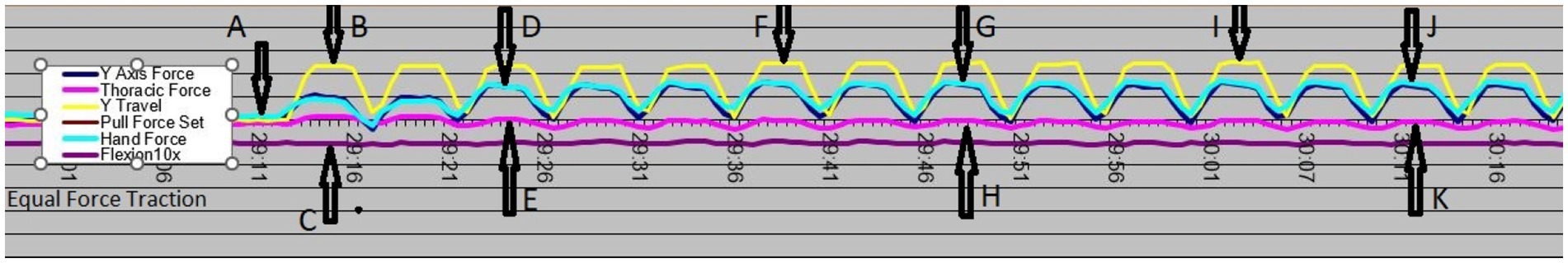
Figure 4. Bi-directional equal force traction graph with bi-directional forces and flexion angle values indicated.
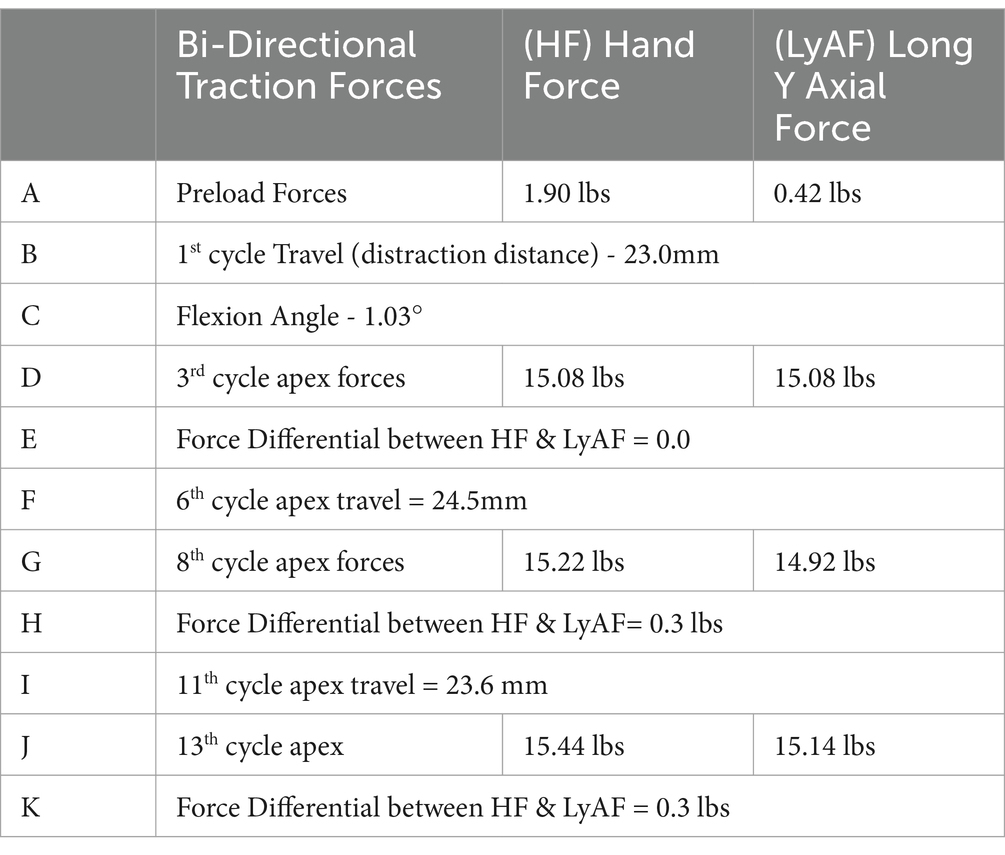
Table 6. Hand and longitudinal forces at different treatment points while delivering equal bi-directional treatment forces.
Follow-up and outcomesThe patient responded well to this treatment plan, and after 7 treatments, the pain was rated at 3/10, and dorsiflexion and hallux extension were rated at 3/5. Lumbar spine ranges of motion had increased by 10% with reduced pain; Kemp’s test was positive on the left side only, and the left leg SLR was positive at 65°. After 22 treatments, the patient rated the pain at 1/10 on a numeric pain rating scale with a low back pain (Revised Oswestry) assessment score of 8. Manuel’s muscle strength testing for dorsiflexion was rated at 5/5 bilaterally, the patient could heel and toe walk normally. The lumbar spine ranges of motion were measured: flexion at 100° without pain, extension at 20° without pain, and right and left lateral bending at 25° without pain, bilaterally. Kemp’s test was negative bilaterally, and SLR was negative at 80°, bilaterally. The patient reported improvements in her ability to lift weight, walk, sit, stand, sleep, and travel and in her social life. Subsequently, the pain management physician referred the patient for an electro-neurodiagnostic study (EMG) after the CTFDD treatment plan was completed. This post-treatment EMG study was reported as normal.
DiscussionDiscogenic sciatica is frequently caused by an L4–L5 herniated disk putting mechanical pressure on the L5 nerve root (Meng et al., 2022). As this condition progresses, weakness of the tibialis anterior, extensor digitorum, halluces longus, and extensor hallucis muscles with dysesthesia of the L5 dermatome can manifest clinically. Peroneus longus and brevis muscle weakness can also occur when an L5-S1 disk herniation compresses the S1 nerve root. Foot and great toe dorsiflexion strengths will depend on the nerve supply of the peroneal nerve to the anterior tibialis and extensor muscles.
Clinically, the straight leg raise test will be positive in proportion to the amount of nerve root compression by the intervertebral disk. Patients with only leg pain and those with a marked predominance of leg pain over back pain have a high probability of harboring an extruded disk fragment (Pople and Griffith, 1994; Cox, 2011; Niazi et al., 2020). A patient with a clinical presentation of acute sciatica in the lower extremity due to a lumbar disk herniation and sequestered fragment is commonly referred for surgical consultation and possible intervention (Wielechowski et al., 2020); however, non-surgical, conservative treatment for radicular pain may be comparable to surgery based on cost, morbidity, and complications (Neault, 1992; Ikeda et al., 1996; Komori, 1996; Memmo et al., 2000; Peul et al., 2007, 2008; Lillie, 2010; Hong and Ball, 2016). Research has shown that non-surgical treatment outcomes are equal to surgery for patients who were surgical candidates with a herniated lumbar disk and radicular pain (Neault, 1992; Ikeda et al., 1996; Komori, 1996; Peul et al., 2007, 2008; Lillie, 2010; Cox, 2011; Hong and Ball, 2016).
Cox flexion distraction spinal manipulation has specific standards of care algorithms for the efficacious management of patients with discogenic sciatica (Cox et al., 1996; Cox, 2011). Randomized clinical studies have demonstrated an increase in lumbar spine ranges of motion in low back pain patients receiving decompression therapy. Our CTFDD treatment data demonstrate a gradual increase in table motion and applied manipulative forces as the number of distraction cycles increases. This increase in manipulative forces and spinal motion post-CTFDD spinal manipulation may indicate increased lumbar spine flexibility and biomechanical improvement. Achieving demonstrable biomechanical improvement graphs from a CTFDD spinal manipulation is a possible direction for force-based spinal manipulation research (Isner-Horobeti et al., 2016; Amjad et al., 2022; Reed et al., 2024).
ConclusionForce-based CTFDD spinal manipulation, along with other modalities consisting of pre-modulated EMS, ILT, and a home stretching and strengthening program, has been found to be an alternative, non-surgical treatment for discogenic sciatica. An interdisciplinary approach to research on the force-based CTFDD spinal manipulation is needed to further evaluate the post-treatment phenomenon of the manipulative forces and motion applied to the lumbar spine using multiple patients and/or a randomized clinical study.
Data availability statementThe raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statementThe studies involving humans were approved by Keiser University Institutional Review Board. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributionsTS: Writing – review & editing, Writing – original draft, Investigation, Conceptualization. MG: Writing – review & editing, Writing – original draft, Methodology, Conceptualization. RK: Writing – review & editing, Writing – original draft.
FundingThe author(s) declare financial support was received for the research, authorship, and/or publication of this article. Several Doctors of Chiropractic donated towards the publication charges.
Conflict of interestThe authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The author(s) declared that they were an editorial board member of Frontiers, at the time of submission. This had no impact on the peer review process and the final decision.
Publisher’s noteAll claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
ReferencesAmjad, F., Mohseni-Bandpei, M. A., Gilani, S. A., Ahmad, A., and Hanif, A. (2022). Effects of non-surgical decompression therapy in addition to routine physical therapy on pain, range of motion, endurance, functional disability, and quality of life versus physical therapy alone in patients with lumbar radiculopathy; a randomized controlled trial. BMC Musculoskeletal Disord. 23:255. doi: 10.1186/s12891-022-05196-x
PubMed Abstract | Crossref Full Text | Google Scholar
Cox, J. M. (2011). Low back pain: mechanism, diagnosis, treatment. 7th Edn. Philadelphia, PA: Lippincott, Williams & Wilkins, 370–375.
Cox, J. M., Feller, J., and Cox-Cid, J. (1996). Distraction chiropractic adjusting: clinical application, treatment algorithms, and clinical outcomes of a 1,000 cases. Top. Clin. Chiropr. 3.
Gudavalli, M., and Cox, J. (2014). Real-time force feedback during flexion-distraction procedure for low Back pain: a pilot study. J. Can. Chiropr. Assoc. 58, 193–200.
Gudavalli, M. R., Cramer, G. D., and Patwardhan, A. G. (2022, 2022). Changes in intradiscal pressure during flexion-distraction type of chiropractic procedure: a pilot cadaveric study. Integr. Med. Rep. 1, 209–214. doi: 10.1089/imr.2022.0002
Crossref Full Text | Google Scholar
Gudavalli, M. R., Cramer, G. D., and Patwardhan, A. G. (2023). Intervertebral movements and changes in intervertebral Foraminal morphology in the lumbar spine during a chiropractic procedure: a cadaveric study. Integr. Med. Rep. 2, 7–13. doi: 10.1089/imr.2022.0022
Crossref Full Text | Google Scholar
Hong, J., and Ball, P. A. (2016). Images in clinical medicine. Resolution of lumbar disk herniation without surgery. N. Engl. J. Med. 374:1564. doi: 10.1056/NEJMicm1511194
Crossref Full Text | Google Scholar
Hoy, D., March, L., Brooks, P., Blyth, F., Woolf, A., and Bain, C. (2014). The global burden of low back pain: estimates from the Global Burden of Disease 2010 study. Ann. Rheum. Dis. 73, 968–974. doi: 10.1136/annrheumdis-2013-204428
Crossref Full Text | Google Scholar
Ikeda, T., Nakamura, T., and Kikuchi, T. (1996). ETAL: Pathomechanism of spontaneous regression of the herniated disc: histologic and Immunohistochemical study. J. Spinal Disord. 9, 136–140. doi: 10.1097/00002517-199604000-00009
PubMed Abstract | Crossref Full Text | Google Scholar
Isner-Horobeti, M. E., Dufour, S. P., Schaeffer, M., Sauleau, E., Vautravers, P., Lecocq, J., et al. (2016). High-force versus low-force lumbar traction in acute lumbar sciatica due to disc herniation: a preliminary randomized trial. J. Manip. Physiol. Ther. 39, 645–654. doi: 10.1016/j.jmpt.2016.09.006
PubMed Abstract | Crossref Full Text | Google Scholar
Jun, P., Pagé, I., Vette, A., and Kawchuk, G. (2020). Potential mechanisms for lumbar spinal stiffness change following spinal manipulative therapy: a scoping review. Therapy 28:15. doi: 10.1186/s12998-020-00304-x
PubMed Abstract | Crossref Full Text | Google Scholar
Katz, J. N. (2006). Lumbar disc disorders and low Back pain: socioeconomic factors and consequences. J. Bone Joint Surg. Am. 88, 21–24. doi: 10.2106/00004623-200604002-00005
Crossref Full Text | Google Scholar
Lillie, G. R. L. (2010). Resolution of low back pain and radicular pain in a 40-year-old male United States navy petty officer after collaborative medical and chiropractic care. J. Chiropr. Med. 9, 17–21. doi: 10.1016/j.jcm.2009.12.006
Crossref Full Text | Google Scholar
Memmo, P. A., Nadler, S., and Malanga, G. (2000). Lumbar disc herniation: a review of surgical indications and outcomes. J. Back Musculoskelet Rehabil. 14, 79–88.
Meng, Z., Zheng, J., Fu, K., Kang, Y., and Wang, L. (2022). Creative effects of Foraminal endoscopic surgery and efficacy of the wearable lumbar spine protection equipment in the treatment of lumbar disc herniation. J Healthc. Eng. 2022:6463863. doi: 10.1155/2022/6463863
Crossref Full Text | Google Scholar
Neault, C. C. (1992). Conservative management of an L4-L5 left nuclear prolapse with a sequestered segment. J. Manip. Physiol. Ther. 5, 318–322.
Niazi, I. K., Kamavuako, E. N., Holt, K., Tam, J., Kuramin, A. I., and Haavik, H. (2020). The effects of spinal manipulation on the electrophysiological and metabolic properties of the tibialis anterior muscle. Healthcare (Basel) 8:548. doi: 10.3390/Healthcare8040548
PubMed Abstract | Crossref Full Text | Google Scholar
Peul, W. C., van den Hout, W. B., Brand, R., Thomeer, R. T., and Koes, B. W.Leiden-the Hague Spine Intervention Prognosis Study Group (2008). Prolonged conservative care versus early surgery in patients with sciatica caused by lumbar disc herniation: two year results of a randomized control trial. BMJ 336, 1355–1358. doi: 10.1136/bmj.a143
Crossref Full Text | Google Scholar
Peul, W. C., van Houwelingen, H., van den Hout, W., Brand, R., Eekhof, J. A., Tans, J. T., et al. (2007). Surgery versus prolonged conservative treatment for sciatica. N. Engl J. Med. Overseas Ed. 356, 2245–2256. doi: 10.1056/NEJMoa064039
PubMed Abstract | Crossref Full Text | Google Scholar
Pople, I., and Griffith, H. (1994). Predication of an extruded fragment in lumbar disc patients from clinical presentations. Spine 19, 156–158. doi: 10.1097/00007632-199401001-00007
PubMed Abstract | Crossref Full Text | Google Scholar
Reed, W. R., Cook, C., Napadow, V., Elliott, D. M., and Kawchuk, G. (2024). The critical need, importance, and value of mechanistic force-based manipulations research. J. Man. Manip. Ther. 32:1-9. doi: 10.1080/10669817.2023.2290782
PubMed Abstract | Crossref Full Text | Google Scholar
Sharma, H., Lee, S. W. J., and Cole, A. A. (2012). The management of weakness caused by lumbar and lumbosacral nerve root compression. J. Bone Joint Surg. Br. 94-B, 1442–1447. doi: 10.1302/0301-620X.94B11.29148
Crossref Full Text | Google Scholar
Vos, T. P., Flaxman, A. D. P., Naghavi, M. P., Lozano, R. P., Michaud, C. M. D., Ezzati, M. P., et al. (2012). Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990-2010: a systematic analysis for the global burden of disease study 2010. Lancet 380, 2163–2196. doi: 10.1016/S0140-6736(12)61729-2
Crossref Full Text | Google Scholar
Wielechowski, A., Keil, A., and Hamstra-Wright, K. (2020). Referral patterns for surgical consult in the management of patients with foot drop due to acute lumbar disc herniation: a survey study of physical therapists in the United States. J. Man. Manip. Ther. 29, 99–106. doi: 10.1080/10669817.2020.1776491
留言 (0)