Since December 2019, the coronavirus outbreak and its variants have spread worldwide (1–3). Coronavirus Disease 2019 (COVID-19) patients report significant psychiatric and psychological sequelae, including anxiety, stress, depression, posttraumatic stress disorder, cognitive deficits, loneliness, and sleep disturbances (4–8). However, patients’ mental problems varied according to their perception of social support (9). Perceived social support (PSS), which describes how people evaluate and believe about the capacity of their social network and resources against stress and crisis, has recently been considered as a protective factor during the COVID-19 period (10, 11). PSS refers to the extent to which people find family members, friends, and other significant people in their lives available for support (12). The more these people are present in times of need and provide emotional, practical support and practical solutions, the more empowered a person feels to face problems. However, in the absence of social support, people feel lonely and isolated (13). Lack of PSS is associated with some psychological problems and difficulties in effectively coping with crises. PSS is essential among COVID-19 patients who were faced with social restrictions such as preventing them from meeting their relatives. Previous evidence has shown that lack of social support can predict high levels of stress (14) and sleep problems (15), which play a significant role in immune system weakness and lack of recovery (16).
Coping with stress and its psychological consequences is difficult without PSS (17). Evidence has shown that having social support during the COVID-19 crisis was effective in facilitating the management of related stress (18). PSS can reduce stress levels (19), enhance coping strategies in response to stressful conditions (20), and protect individuals against the physical and psychological consequences of adverse life events (21). However, when the patients feel lower level of PSS, they are more prone to non-adherence to medication (22).
PSS is associated with several aspects of sleep quality (23). During the COVID-19 pandemic, people with less PSS reported significantly more sleep problems than others (10). When people feel they have social support, they experience a greater sense of security, belonging, and relaxation, which affects their sleep quality (24). However, the lack of PSS is associated with loneliness, anxiety and depression, aggravating sleep problems (10, 25).
Mixed evidence has been reported on the difference in perceived social support across genders. Some studies have shown that perceived social support does not differ by gender (26, 27). In contrast, some research has revealed that gender affects the quality and quantity of perceived social support (28, 29). For example, depressed males received more social support from their friends, while depressed females received more support from significant others in their lives (30). Additionally, among cancer patients, males perceived less social support than female peers (31).
Similarly, mixed evidence was drawn from previous studies regarding the age differences in perceived social support. Some studies have shown that age does not create differences in the level of perceived social support and its components (32, 33), while F Li, S Luo, W Mu, et al. (34) examined the social support that individuals receive from different sources during COVID-19, and indicated the association between getting older and high perceived social support from sources outside of the family. On the contrary, a psychometric study of MSPSS reported a significant opposite trend that younger patients (56-65 years) perceived more outstanding social support from significant others than older patients (above 66 years).
The Multidimensional Scale of Perceived Social Support (MSPSS) is a valid instrument that assesses PSS in all three domains of family, friends, and significant others. The factor structure and psychometric properties of the MSPSS have been analyzed in different populations (Table 1). For example, investigations of the MSPSS among general populations have indicated that MSPSS three-factor structure is reliable (58). In a clinical population of cancer patients in Spain, it is shown that the original three-factor structure has a good model fit and substantial measurement invariance in gender and age (40). Similar results were also reported among Korean non-metastatic breast cancer survivors (aged 31–73) (35). However, the MSPSS’s factor structure and construct validity are not yet well known among COVID -19 patients.
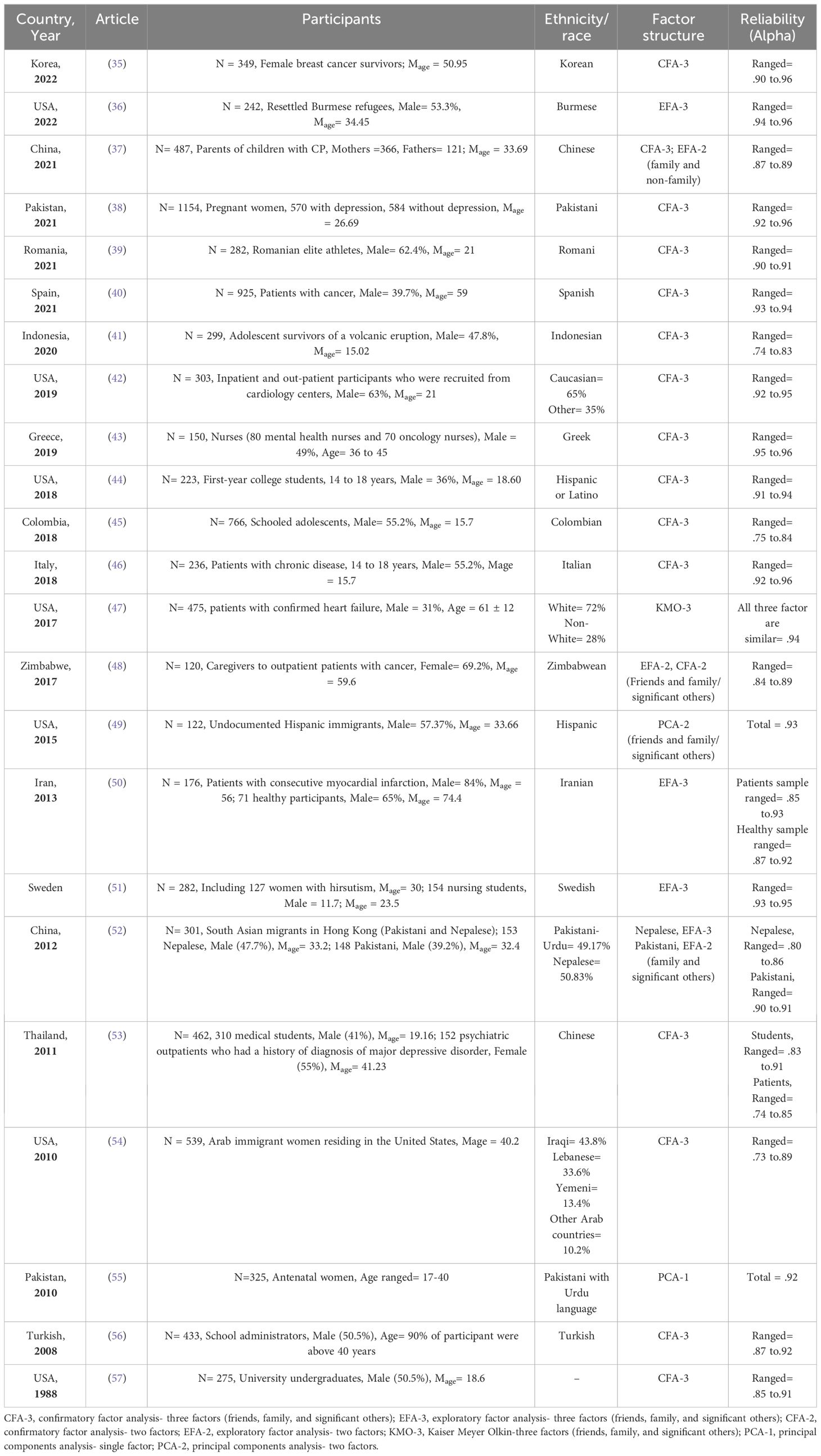
Table 1 Studies validating psychometric properties of the MSPSS in different countries and populations.
As a developing country in the Middle East, Iran has made significant progress in its healthcare system. However, it was severely affected by the outbreak of the Covid-19 pandemic. Culturally, Iranian people have a collective culture, and family relationships are still the main focus of social support for individuals. However, in critical situations, including illness, individuals receive various social supports from other sources. Even if the COVID-19 pandemic terminates, we risk an outbreak of coronaviruses (59) or other potential pandemics (60). Therefore, examining the three-factor model and measurement invariance of PSS in COVID-19 patients and the relationship of its factors with stress and sleep quality as two highly correlated factors can expand our knowledge about the reliability and validity of the PSS model. It can also show which of the PSS sources are more related to stress and reduced sleep quality in patients so that related interventions can be considered. Evidence related to it can help the medical service system to improve the quality of patient care and treatment during hospitalization and recovery. Consequently, the present study was conducted to investigate the three-factor structure of the MSPSS, test for gender and age invariance, and estimate psychometric properties such as internal consistency and concurrent validity among COVID-19 patients. Therefore, we identified the following hypotheses based on previous evidence:
● The MSSS among COVID-19 patients will follow the same three-factor structure (family, friends, and significant others) as the original version.
● Gender invariance in the MSPSS factor structure will be equal in the configural, metric, and scalar invariance.
● Age invariance in the MSPSS factor structure will be equal in the configural, metric, and scalar invariance.
● The invariance of latent factor means will be similar by gender and age groups on MSPSS scores from friends, family, and significant other.
● The MSPSS will have acceptable internal consistency based on Cronbach’s alpha.
● The MSSS will have acceptable concurrent validity based on its negative correlation with sleep problems.
● The MSSS will have acceptable concurrent validity based on its negative correlation with perceived stress.
2 Methods2.1 ParticipantsThe 328 hospitalized COVID-19 patients (54.9% male) aged 21 to 92 (M = 50.77, SD = 15.32) were selected from two general hospitals (Baharloo and Ziaeian Hospitals) with a hospitalization duration of 7 days, on average. The inclusion criteria consist a history of hospitalization due to COVID-19 and the exclusion criteria include a) lack of interest in participating in the study, b) insufficient ability to answer questions, and c) the patient’s death after discharge from the hospital. Most participants had diploma education (78, 23.2%) and were housewives (n= 119, 36.3%). In addition, patients mostly lived with their spouses and children (n= 209, 63.7%) and had no smoking history (n= 284, 86.6%). The demographic characteristic of the sample is presented in Table 2.

Table 2 The description of the sample characteristics (n = 328).
2.2 Recruiting, assessing, and conducting procedureThe current cross-sectional study conducted between March and October 2020, on patients hospitalized due to Coronavirus infection at Baharloo and Ziaeian Hospitals in Tehran, Iran. After confirming the positive diagnosis of coronavirus, demographic information of patients, including gender, age, educational and occupational status, and their contact numbers, were collected in a registration form.
Participants read and assented to the informed consent form before starting the study. Then, three psychology experts collected data (the MSPSS, the PSS-10, and the PSQI) via telephonic interview from those who filled in the consent form. The implementation of the measurement phase was carried out by measurement experts familiar with the tools. Before starting the assessment, participants received instructions on how to answer the questions. It was also explained to them that if any of the items were unclear, they should discuss it with their evaluator. If the person had a wrong understanding of the items, the necessary explanations were provided. This study was approved by the ethical board of Tehran University of Medical Sciences (Ethic Code: IR.TUMS.VCR.REC.1399.156).
2.3 Measurements2.3.1 The multidimensional scale of perceived social support – Persian versionThe MSPSS (57) has a 12-item, developed to measure how people think about their social support assets (including friends, family, and significant others). In addition, it has a 7-point Likert scale, ranging from 1 (strongly disagree) to 7 (strongly agree), scored between 12 to 84, where higher scores on this scale mean greater perceived social support. Psychometric studies examining the MSPSS in different populations supported the original three-factor solution (39, 43, 52, 57). Furthermore, some studies that examined MSPSS in the patient population while confirming its three-factor structure have shown good psychometric properties (61).
2.3.2 Perceived stress scale – Persian versionThe PSS (14 items-version) was presented to evaluate patients’ appraisal of stressful conditions in their life (62). Subsequently, the developers endorsed a 10-item version of the tool (63). This 10-item unidimensional scale comprised four positively and six negatively worded items. Items were scored through a 5-point Likert scale, between 0 (never) to 4 (very often), where positively worded items were reversely coded. The original study of PSS-10 reported good internal consistency (α= .78) (63). Moreover, the Persian version of PSS-10 also demonstrated high internal consistency reliability (α= .93) (64).
2.3.3 Pittsburgh sleep quality index – Persian versionThe PSQI (65) is a self-administered 19-item tool for a brief assessment of sleep disturbances that influence sleep quality within the prior month. The seven components of PSQI include sleep latency, subjective sleep quality, habitual sleep efficiency, sleep duration, use of sleep medication, daytime dysfunction, and sleep disturbances). PSQI is scored on a 4-point Likert scale, and the components’ scores are counted together to obtain the total sleep quality score. The total PSQI score ranged between 0 and 21, with high scores showing poor quality of sleep and the cut-off point of higher than 5 for identifying poor sleepers. A good internal consistency was reported for the original PSQI (Cronbach’s α= .83) in the preliminary study (65), as well as the internal consistency of PSQI (α= .81) was acceptable among the Iranian sample (66).
2.4 Statistical strategyThe Confirmatory factor analysis (CFA) with less bias and a more robust maximum likelihood (MLR) estimator was adopted to examine a priori models of the factor structure by HN Cheung and MJ Power (67). Statistical strategies were as follows: First, as it is recommended for ordinal Likert-type scales, the internal consistency was examined using Cronbach’s alpha, mean inter-item correlation, and the equivalent of Cronbach’s alpha coefficients (Theta and Omega), which are based on the polychoric correlation, rather than the Pearson correlation (68, 69) and was conducted in R version 4.1.2 (70, 71). According to a rule of thumb, a correlation coefficient of.70 or higher was considered an acceptable level of internal consistency of the items (72).
Second, we used the following statistical tests and indices (73–78) to evaluate the fitness the models (parenthesis indicate acceptable values): the chi-square (χ2; p >.05), the Tucker–Lewis index (TLI >.95), the comparative fit index (CFI >.95), the normal chi-square (3 > χ2/df < 2), the standardized root mean square residual (SRMR <.05), the root mean square error of approximation (RMSEA <.05), and the confidence interval of 90%. A low Bayesian information criterion (BIC) points to a good model fit. The comparison of competing models was carried out using a chi-square difference test. A nested model is more restrictive than a baseline model since it has more degrees of freedom (79).
Third, having selected the most appropriate model, we tested its measurement of gender equality. Invariance of factorial structure/pattern (configural invariance), corresponding factor loadings (metric invariance), and finally, corresponding indicator means (scalar invariance) were evaluated. We tested the differences in RMSEA, SRMR, and CFI of nested models for invariance (80–82).
Finally, the concurrent validity was determined by examining the correlation between the MSPSS and PSQI, as well as PSS-10, using Kendall’s coefficient (τb) for non-normal data. Correlations in this study were interpreted as having effect sizes of small (.10), medium (.30), large (.50), and very large (.70) (83).
3 Results3.1 Factor structureThe Mplus 8.7 version was utilized to ascertain the MSPSS factorial validity (84), and the goodness of fit was tested for four models. The first model (M1) examined a general solution in which items were loaded over a general social support component to test the unidimensional model of assumed latent factor and included just random measurement error and indicator-specific variance (85). If the general factor model fitted well with the data, the assumption of the multidimensionality of the measurement tool was violated. In other words, it could be interpreted as the lack of discrimination validity for subscales of psychological tools. Model 2 (M2) consisted of a three-factor orthogonal model containing three uncorrelated latent factors. According to the literature, model 3 (M3) examined a three-factor oblique model resembling the exploratory factor analysis (67). Eventually, model 4 (M4) encompassed a three-factor first-order loaded on the one-factor second-order. In the higher-order model, more than one orthogonal first-order subordinate factors mediate the relationship between observed indicators and superordinate second-order latent factor (86). Based upon the largely standardized covariances among the latent factors in M3, a second-order model may be needed to account for the estimated variances and covariances of three perceived social support subscales (Figure 1).
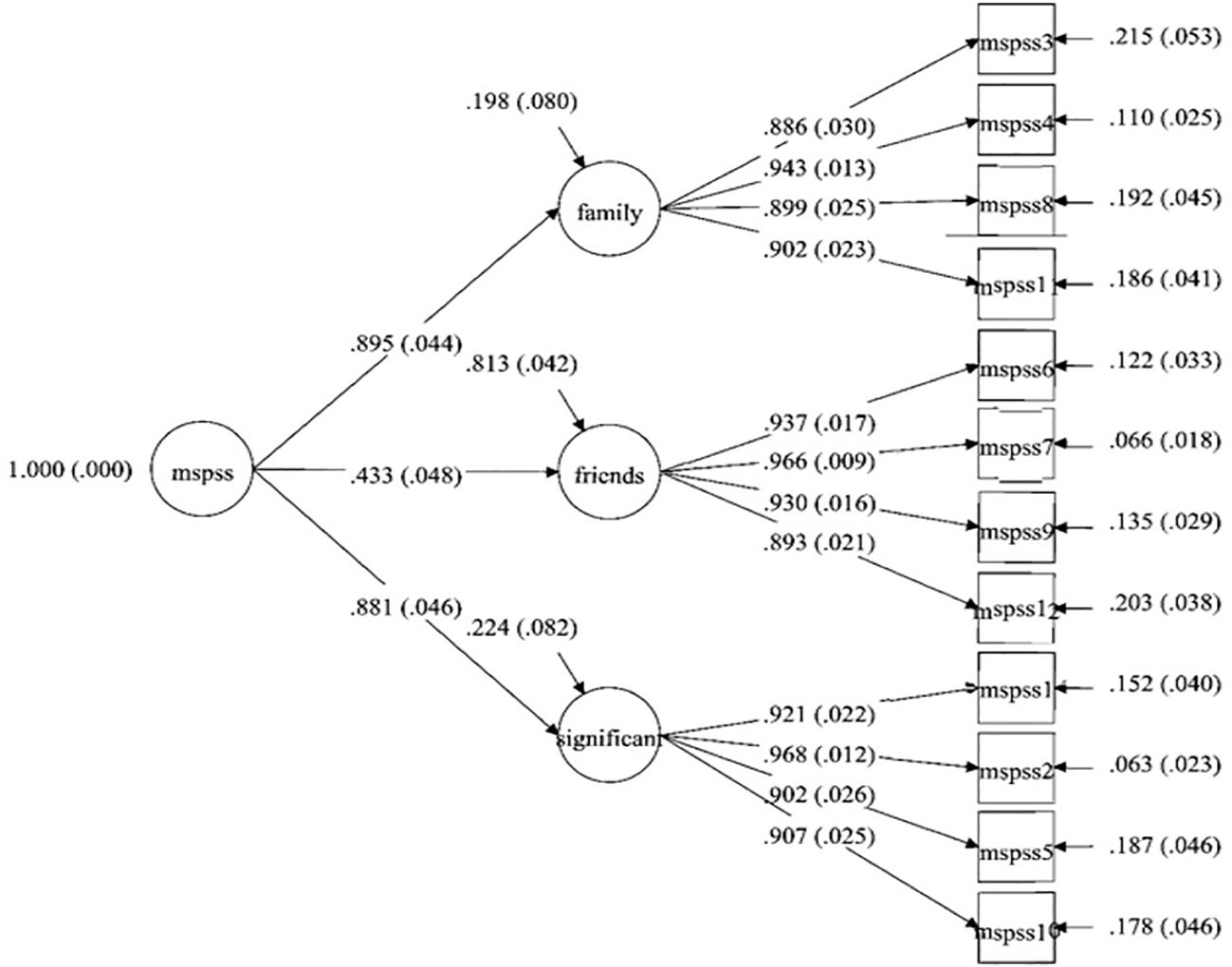
Figure 1 The three first-order and one second-order confirmatory factor analysis of the MSPSS.
3.2 Model selectionAs indicated in Table 3, oblique three-factor model (M3) and the three-factor first-order and one-factor second-order model’s fit indices (M4) met most of the specified criteria. They also yielded better model fit, compared to nested models (M1 and M2). Then, the parsimonious principle (87) was used to compare the M4 fit indices with those of the M3 as competitive models. The results indicate that based on the fitness indices, neither of these independent models has any distinct advantages (see Table 3), although the three-factor first-order and the one-factor second-order model can be optimized/parsimonious based on the theory-derived model.
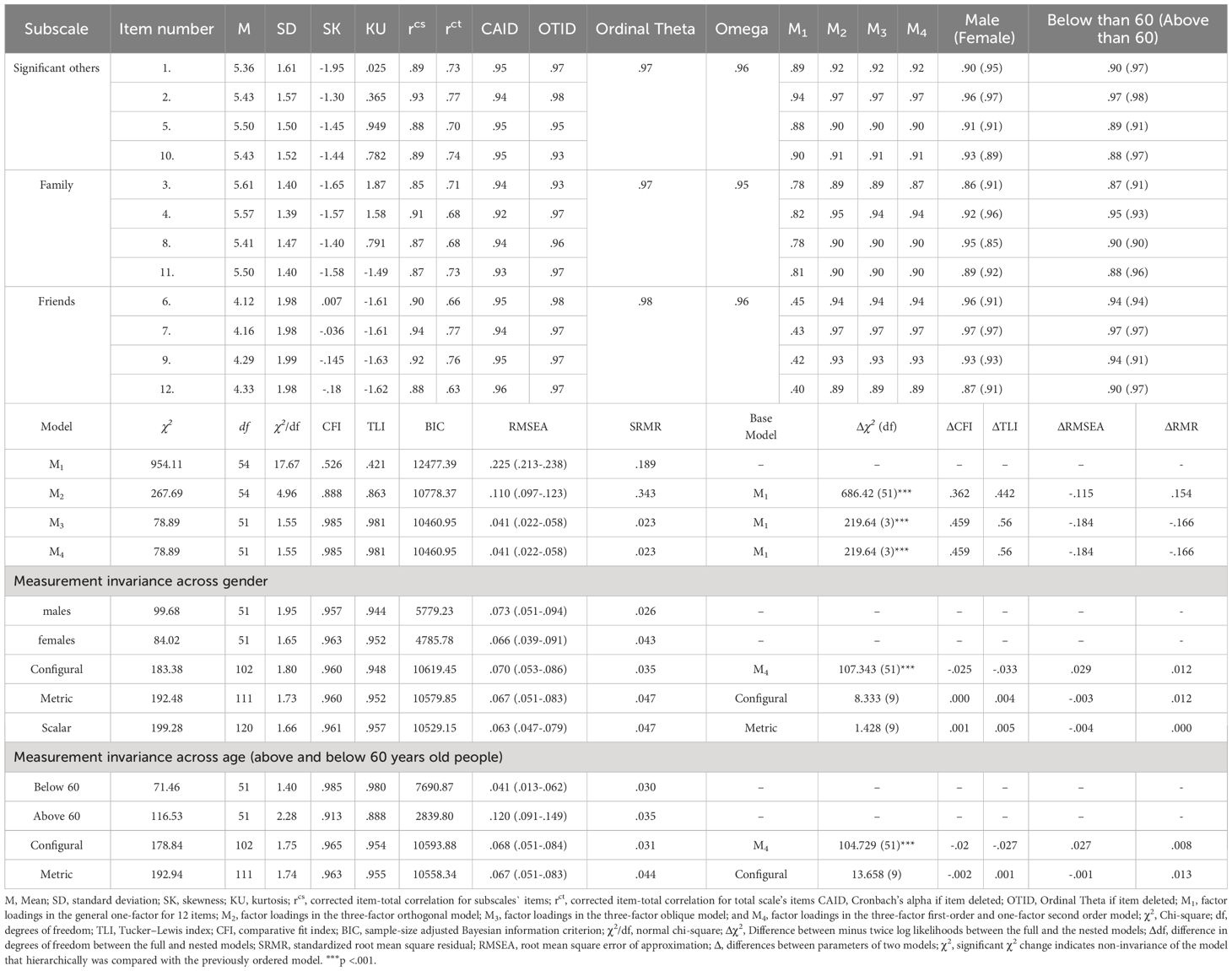
Table 3 Means, standard deviations, internal consistency coefficients, fit indices for CFA of MSPSS.
In examining gender invariance (males and females) and age invariance (above 60 years old (older patients) vs. below 60 years old (non- older patients)), a multi-group CFA analysis was performed in the total sample, males and females groups, and also in older and non-older groups to obtain a satisfactory fitness for the baseline model in each one, under the parsimony and meaningfulness principle (88). Then, configural, weak, and strong measurement invariance were evaluated (Table 3) (81, 89, 90).
Given that changes in the model fit index were minimal, configural invariance was established for the M4 across gender (male vs. female) and age groups (older vs. non-older patients). Comparison of metric model with configural model (ΔCFI = .000, ΔTLI = .005, ΔRMSEA = .003, ΔRMR = .0012), scalar model with metric model (ΔCFI = .001, ΔTLI = .005, ΔRMSEA = .004, ΔRMR = .000), as alternative models indicated that three-factor oblique model (Table 3) was invariant across gender.
Similarly across age groups, comparison of metric model with configural model (ΔCFI = .002, ΔTLI = .003, ΔRMSEA = .003, ΔRMR = .0012), scalar model with metric model (ΔCFI = .001, ΔTLI = .005, ΔRMSEA = .002, ΔRMR = .001), as alternative models indicated that three-factor oblique model was invariant across age (Table 3).
3.3 Internal consistencyThe descriptives, Cronbach’s alpha, Theta (ordinal alpha), Omega reliability coefficients, and corrected item-total correlation for the MSPSS subscales are presented in Table 3. The MSPSS Cronbach’s α was.94, and for friends, family, and significant others was from.92 to.96, suggesting an excellent internal consistency. Almost all the items within the three subscales had a moderate positive relationship with each other-with values ranging from.85 to.94 (according to a corrected item-total correlation for items in each subscale), and from.63 to.77 (using item-total correlation corrected for the scale’s items). Finally, the means of inter-item correlation were.55,.86,.82, and.87 for the total score, significant others, family, and friends’ subscales, respectively.
3.4 Latent factor mean differences social support across gender and ageA testing invariance of latent factor means showed significant group similarity by gender and age on perceived social support scores from friends, family, and significant other (p >.05, Table 4). Nevertheless, the older patients scored significantly lower on the latent factor mean level of the friends’ subscale of perceived social support (mean differences = .47, z = 2.03, p <.05) than the non-older patients.
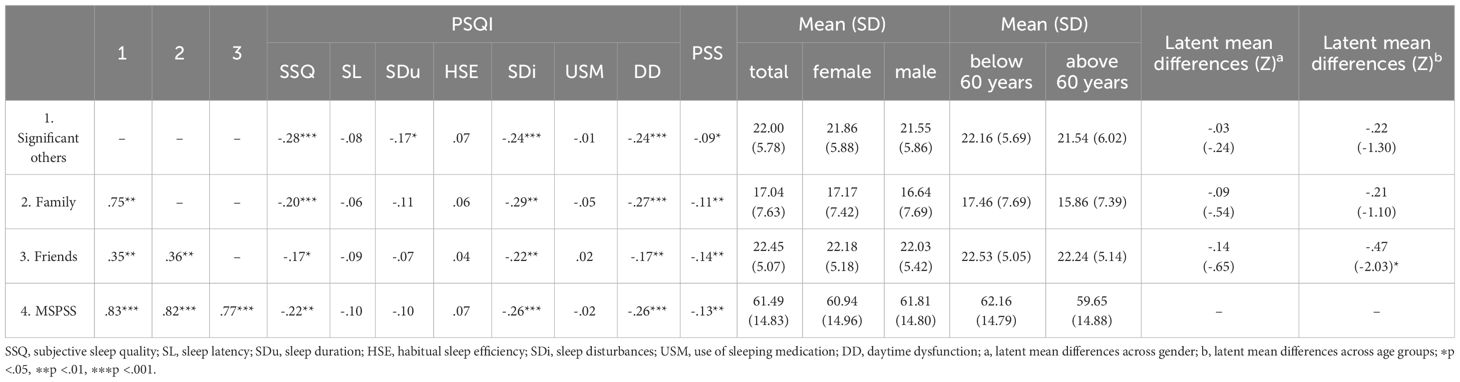
Table 4 The correlation coefficients of MSPSS, PSQI subscales and PSS, Means, Standard Deviations and Latent mean differences.
3.5 Concurrent validity of MSPSSTable 4 showed the inter-correlation between MSPSS subscales. Correlation coefficients ranged from.35 to.83. Concurrent validity was estimated by the testing correlation of total MSPSS and its subscales with PSQI components and PSS-10 (Table 4). Kendall’s correlation coefficients showed total MSPSS has a negative significant correlation with subjective sleep quality (τb = -.22, p <.01), sleep disturbances (τb = -.26, p <.001) and daytime dysfunction (τb = -.26, p <.001). Furthermore, MSPSS has significant negative correlations with PSS-10 (τb = -.13, p <.01).
4 DiscussionThis study aimed to evaluate the MSPSS measurement model, its equivalence in terms of gender and age, and concurrent validity in patients discharged from COVID-19 inpatient care. Both the three-factor first-order and one-factor second-order models had adequate fit indices to the data. All items were loaded on corresponding factors according to the three-factor first-order and one-factor second-order models. These results signify that the most acceptable model to expound on the MSPSS would be considering the three-factor (family, friends, and significant other). In this regard, the results of the present study are consistent with previous literature (35, 57) concerning the three-factor structure of MSPSS among COVID-19 patients, rather than the one-factor model (55).
Due to the test for gender and age invariance in the MSPSS factor structure, results illustrated equalities in the configural, metric, and scalar invariance (81, 91). In other words, the structure of the MSPSS measures the same construct by gender and age groups, which is in line with former studies in other samples (40, 92). Based on the latent factor mean differences, it can be concluded that males and females with COVID-19 perceive the social support of their resources similarly. From these data, it can be concluded that females and males probably have similar needs for social support due to the history of hospitalization due to COVID-19, and they interpret and understand it in the same way. Likewise, older and non-older patients perceive social support from two sources, family and significant others. However, when it comes to social support for friends, older patients perceive less social support than non-older patients. Probably, during the period of the disease, due to the need for quarantine and isolation, patients have less contact with friends than family and important people in life, and older patients are more likely than younger people to comply with social restrictions (93, 94).
Another principal aim of the study involved testing associations between perceived social support, sleep quality, and perceived stress. Perceived social support has been shown to correlate negatively with perceived stress among university students (95). In addition, it moderates the stress impact on mothers of sick children (96), and alleviates pain by reducing the stress of irritable bowel syndrome (IBS) patients, which refers to the social support stress-buffering role (28, 97). The results showed that perceived social support and perceived stress are negatively associated. These findings support the assumption that higher levels of social support can act as a protective factor against stress and highlight the importance of social relationships in modulating the stress of patients’ lives.
More specifically, as predicted, a significant negative relationship was found between perceived social support and sleep quality (subjective sleep quality, sleep disturbances, daytime dysfunction), in line with earlier evidence (98). The association between perceived social support and sleep quality is more influenced by its protective and moderating role on sleep quality risk factors. For instance, I Grey, et al. (10), demonstrated the association of perceived social support with better sleep quality during the COVID-19 pandemic, possibly due to the association of perceived social support with depression, irritability, and loneliness. In addition, R Xu, Y Lin and B Zhang (99) have shown that perceived social support can moderate the sleep quality’s relationship with the subjective well-being of older patients by buffering the effect of negative emotions. Overall, the perceived social support relationship with sleep quality seems to be affected by the impact of social support on feelings of loneliness, reduced adverse psychological reactions, and improved health status.
4.1 limitations, and future directionsAlthough the present study added considerable evidence to the literature, there were still limitations. Due to the unique circumstances of the outbreak of COVID-19, the voluntary sampling method was chosen for the present study. However, this method may make it difficult to access a complete representative sample of the community, which in turn can hinder the ability to generalize the results widely. This study included only COVID-19 patients over 21 years old. Therefore, caution should be exerted to generalize these findings to other populations and the age group under 21 years, as this study was conducted with people above 21 years old. In addition, only self-report data were contained in the present study; hence, associations between the variables may have been affected by shared method variance. Further, as this was a cross-sectional study, the causal relationship between perceived social support and other variables was not considered. Consequently, the results of the study may have been affected by some external factors such as seasons, the peak of the pandemic, and quarantine measures.
Despite that no difference was found in the factor structure of MSPSS based on gender and age in the present study, future investigations need to investigate these discrepancies in various groups more because the evidence for age and gender differences is relatively contradictory. Eventually, the Persian version of the MSPSS will be widely used in various clinical settings. Given Iran’s ethnic and cultural diversity, it is suggested that future studies examine the psychometric properties and effectiveness of this tool among Iranian different ethnic groups and cultures. Also, since coronaviruses and their various variants have been around in the past and are likely to reappear in the future and affect people’s lives, longitudinal research, multiple methods, and more specific disciplines are ought.
5 ConclusionThe MSPSS has an acceptable and promising factor structure, validity, reliability, and measurement invariance across gender and age among COVID-19 patients. This study provided support for the clinical utility of MSPSS in various populations. Given the high importance of perceived social for COVID-19 patients and people experiencing stressful events, MSPSS can be applied support to their perceived social support to look into the associations between sleep quality and perceived stress.
Data availability statementThe raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statementThe studies involving humans were approved by Ethics Committee of Tehran University of Medical Sciences. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributionsMHA: Writing – review & editing, Writing – original draft, Supervision, Software, Methodology, Funding acquisition, Formal analysis, Conceptualization. ZV: Writing – review & editing, Validation, Resources, Investigation, Data curation. HNC: Writing – review & editing. RA: Writing – review & editing, Writing – original draft, Visualization. SA: Writing – review & editing, Validation, Investigation, Data curation. MHS: Writing – review & editing, Visualization, Validation, Investigation. FE: Writing – review & editing, Writing – original draft, Resources, Project administration, Methodology, Funding acquisition, Conceptualization.
FundingThe author(s) declare financial support was received for the research, authorship, and/or publication of this article. This research was supported by grant number 99-1-101-47,395 from the Tehran University of Medical Sciences. Open-access funding is provided by the Norwegian University of Science and Technology.
Conflict of interestThe authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s noteAll claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References1. Lupia T, Scabini S, Mornese Pinna S, Di Perri G, De Rosa FG, Corcione S. 2019 novel coronavirus (2019-nCoV) outbreak: A new challenge. J Global Antimicrob Resistance. (2020) 21:22–7. doi: 10.1016/j.jgar.2020.02.021
CrossRef Full Text | Google Scholar
2. Bogoch II, Watts A, Thomas-Bachli A, Huber C, Kraemer MUG, Khan K. Pneumonia of unknown etiology in Wuhan, China: potential for international spread via commercial air travel. J Travel Med. (2020) 27. doi: 10.1093/jtm/taaa008
CrossRef Full Text | Google Scholar
3. Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. (2020) 395:497–506. doi: 10.1016/S0140-6736(20)30183-5
PubMed Abstract | CrossRef Full Text | Google Scholar
4. Deng J, Zhou F, Hou W, Silver Z, Wong CY, Chang O, et al. The prevalence of depression, anxiety, and sleep disturbances in COVID-19 patients: a meta-analysis. Ann New York Acad Sci. (2021) 1486:90–111. doi: 10.1111/nyas.14506
CrossRef Full Text | Google Scholar
5. Zandifar A, Badrfam R, Yazdani S, Arzaghi SM, Rahimi F, Ghasemi S, et al. Prevalence and severity of depression, anxiety, stress and perceived stress in hospitalized patients with COVID-19. J Diabetes Metab Disord. (2020) 19:1431–8. doi: 10.1007/s40200-020-00667-1
PubMed Abstract | CrossRef Full Text | Google Scholar
6. Schou TM, Joca S, Wegener G, Bay-Richter C. Psychiatric and neuropsychiatric sequelae of COVID-19 – A systematic review. Brain Behav Immun. (2021) 97:328–48. doi: 10.1016/j.bbi.2021.07.018
PubMed Abstract | CrossRef Full Text | Google Scholar
7. Spencer-Segal JL, Smith CA, Slavin A, Sampang L, DiGiovine D, Spencer AE, et al. Mental health outcomes after hospitalization with or without COVID-19. Gen Hosp Psychiatry. (2021) 72:152–3. doi: 10.1016/j.genhosppsych.2021.07.004
PubMed Abstract | CrossRef Full Text | Google Scholar
8. de Filippis R, El Hayek S, Shalbafan M. Editorial: Mental illness, culture, and society: Dealing with the COVID-19 pandemic. Front Psychiatry. (2022) 13:1073768. doi: 10.3389/fpsyt.2022.1073768
PubMed Abstract | CrossRef Full Text | Google Scholar
9. Kandeğer A, Aydın M, Altınbaş K, Cansız A, Tan Ö, Tomar Bozkurt H, et al. Evaluation of the relationship between perceived social support, coping strategies, anxiety, and depression symptoms among hospitalized COVID-19 patients. Int J Psychiatry Med. (2021) 56:240–54. doi: 10.1177/0091217420982085
PubMed Abstract | CrossRef Full Text | Google Scholar
10. Grey I, Arora T, Thomas J, Saneh A, Tohme P, Abi-Habib R. The role of perceived social support on depression and sleep during the COVID-19 pandemic. Psychiatry Res. (2020) 293:113452. doi: 10.1016/j.psychres.2020.113452
PubMed Abstract | CrossRef Full Text | Google Scholar
12. Xu J, Ou J, Luo S, Wang Z, Chang E, Novak C, et al. Perceived social support protects lonely people against COVID-19 anxiety: A three-wave longitudinal study in China. Front Psychol. (2020) 11:566965. doi: 10.3389/fpsyg.2020.566965
PubMed Abstract | CrossRef Full Text | Google Scholar
13. Wang J, Mann F, Lloyd-Evans B, Ma R, Johnson S. Associations between loneliness and perceived social support and outcomes of mental health problems: a systematic review. BMC Psychiatry. (2018) 18:156. doi: 10.1186/s12888-018-1736-5
PubMed Abstract | CrossRef Full Text | Google Scholar
14. Özer Ö, Özkan O, Budak F, Özmen S. Does social support affect perceived stress? A research during the COVID-19 pandemic in Turkey Vol. 31. . United Kingdom: Taylor & Francis (2021) p. 134–44.
16. Prather AA. Chapter 24 - Sleep, stress, and immunity. In: Grandner MA, editor. Sleep and health. London, UK: Academic Press (2019). p. 319–30. doi: 10.1016/B978-0-12-815373-4.00024-1
CrossRef Full Text | Google Scholar
17. Wang F, Huang L, Zhang H, Jiang H, Chang X, Chu Y. The mediating role of perceived stress on the relationship between perceived social support and self-care ability among Chinese enterostomy patients. Supportive Care Cancer. (2021) 29:3155–62. doi: 10.1007/s00520-020-05829-8
CrossRef Full Text | Google Scholar
18. Tindle R, Hemi A, Moustafa AA. Social support, psychological flexibility and coping mediate the association between COVID-19 related stress exposure and psychological distress. Sci Rep. (2022) 12:8688. doi: 10.1038/s41598-022-12262-w
PubMed Abstract | CrossRef Full Text | Google Scholar
19. Ross AM, Steketee G, Emmert-Aronson BO, Brown TA, Muroff J, DeVoe ER. Stress-buffering versus support erosion: Comparison of causal models of the relationship between social support and psychological distress in military spouses. Am J Orthopsychiatry. (2020) 90:361–73. doi: 10.1037/ort0000438
PubMed Abstract | CrossRef Full Text | Google Scholar
20. Zabalegui A, Cabrera E, Navarro M, Cebria MI. Perceived social support and coping strategies in advanced cancer patients. J Res Nurs. (2011) 18:409–20. doi: 10.1177/2F1744987111424560
CrossRef Full Text | Google Scholar
21. Cohen S, Underwoo LG, Gottlieb BH. Social support measurement and intervention: A guide for health and social scientists. New York, NY, US: Oxford University Press (2000). doi: 10.1093/med:psych/9780195126709.001.0001
CrossRef Full Text | Google Scholar
22. Semahegn A, Torpey K, Manu A, Assefa N, Tesfaye G, Ankomah A. Psychotropic medication non-adherence and its associated factors among patients with major psychiatric disorders: a systematic review and meta-analysis. Systematic Rev. (2020) 9:17. doi: 10.1186/s13643-020-1274-3
CrossRef Full Text | Google Scholar
23. Rambod M, Ghodsbin F, Beheshtipour N, Raieyatpishe A, Mohebi Noubandegani Z, Mohammadi-Nezhad A. The relationship between perceived social support and quality of sleep in nursing students. Iran J Nurs. (2013) 25. Available at: https://www.sid.ir/paper/114061/en.
24. Troxel WM, Buysse DJ, Monk TH, Begley A, Hall M. Does social support differentially affect sleep in older adults with versus without insomnia? J Psychosom Res. (2010) 69:459–66. doi: 10.1016/j.jpsychores.2010.04.003
PubMed Abstract | CrossRef Full Text | Google Scholar
25. Al Maqbali M. Anxiety and depression During the COVID-19 Pandemic and Their Impact on Sleep. In: BaHammam A, Pandi-Perumal SR, Jahrami H, editors. COVID-19 and Sleep: A Global Outlook. Springer Nature Singapore, Singapore (2023). p. 41–59. doi: 10.1007/978-981-99-0240-8_3
CrossRef Full Text | Google Scholar
27. Bucholz EM, Strait KM, Dreyer RP, Geda M, Spatz ES, Bueno H, et al. Effect of Low Perceived social support on health outcomes in young patients with acute myocardial infarction: results from the variation in recovery: role of gender on outcomes of young AMI patients (VIRGO) study. J Am Heart Assoc. (2014) 3:e001252. doi: 10.1161/jaha.114.001252
PubMed Abstract | CrossRef Full Text | Google Scholar
29. Matud M, Ibáñez I, Bethencourt JM, Marrero R, Carballeira M. Structural gender differences in perceived social support. Pers Individ Dif. (2003) 35:1919–29. doi: 10.1016/S0191-8869(03)00041-2
CrossRef Full Text | Google Scholar
30. Soman S, Bhat SM, Latha KS, Praharaj SK. Gender differences in perceived social support and stressful life events in depressed patients. East Asian Arch Psychiatry: Off J Hong Kong Coll Psychiatrists = Dong Ya Jing Shen Ke Xue Zhi: Xianggang Jing Shen Ke Yi Xue Yuan Qi Kan. (2016) 26:22–9. Available at: https://easap.asia/abstracts/v26n1/1601_V26N1_p22a.html.
31. Eom C-S, Shin DW, Kim SY, Yang HK, Jo HS, Kweon SS, et al. Impact of perceived social support on the mental health and health-related quality of life in cancer patients: results from a nationwide, multicenter survey in South Korea. Psycho-Oncology. (2013) 22:1283–90. doi: 10.1002/pon.3133
PubMed Abstract | CrossRef Full Text | Google Scholar
32. Wang Y, Wan Q, Huang Z, Huang L, Kong F. Psychometric properties of multi-dimensional scale of perceived social support in chinese parents of children with cerebral palsy. Front Psychol. (2017) 8:2020. doi: 10.3389/fpsyg.2017.02020
PubMed Abstract | CrossRef Full Text | Google Scholar
33. Pedersen SS, Spinder H, Erdman RAM, Denollet J. Poor perceived social support in implantable cardioverter defibrillator (ICD) patients and their partners: cross-validation of the multidimensional scale of perceived social support. Psychosomatics. (2009) 50:461–7. doi: 10.1016/S0033-3182(09)70838-2
留言 (0)