An 86-year-old man presented with multiple swelling on the left lower leg for the last 2 months, which began as small papular lesions and gradually increased in size and number. There was no history of weight loss or fever. His personal, past and family histories were unremarkable.
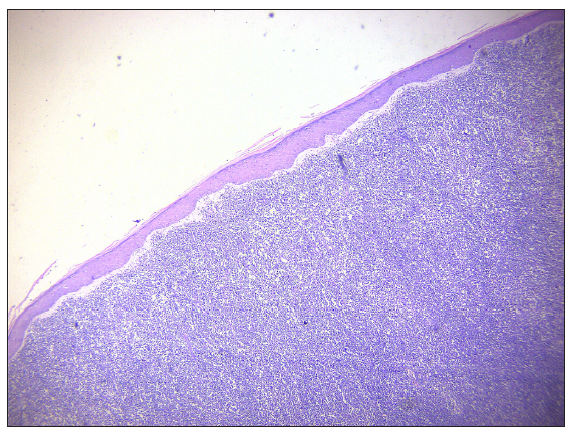
On cutaneous examination, there were seven, linear skin-coloured to erythematous, indurated nodules of 3 × 3 to 8 × 6 cm size with central ulceration and adherent black crusting on the medial aspect of the left leg with bilateral inguinal lymphadenopathy [Figure 1].

Export to PPT
Routine blood tests, peripheral smear, chest X-ray, electrocardiogram (ECG), 2D Echocardiogram (ECHO), ultrasonography (USG) of the abdomen and Computerised tomography (CT) scan of the chest and abdomen were normal. Other tests like lactate dehydrogenase, serum B12, folate, vitamin D3, iron/Total iron-binding capacity (TIBC) were within normal limits, and viral markers were non-reactive.
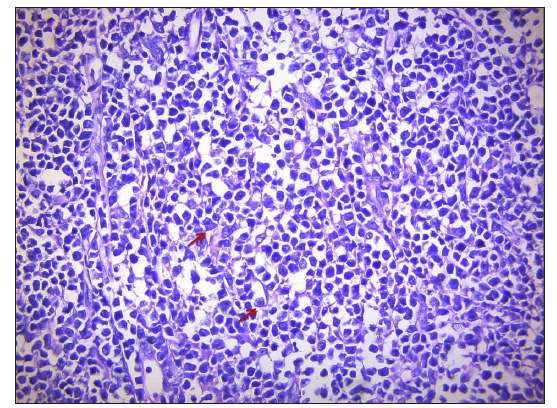
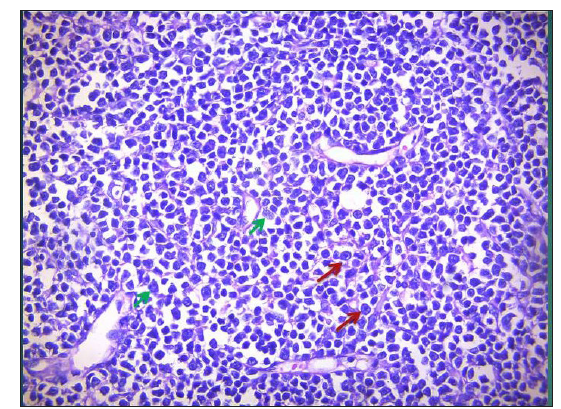
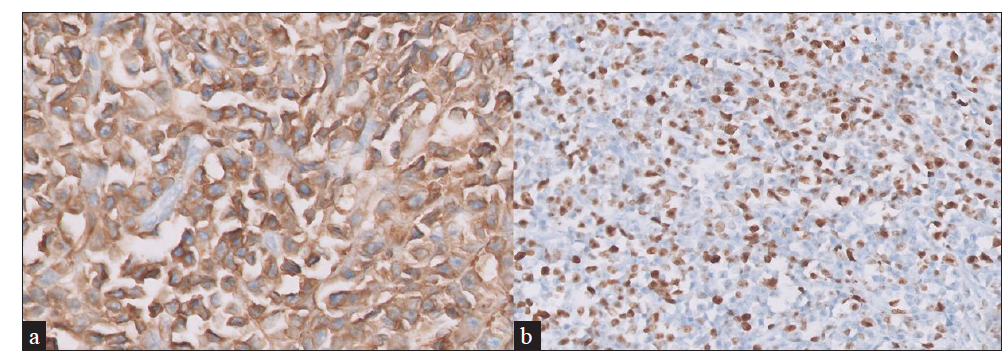
A wedge biopsy was done and sent for histopathological and immunohistochemical (IHC) examination [Figures 2–5].
Export to PPT
Export to PPT
Export to PPT
Export to PPT
Histopathology showed a distinct Grenz zone with diffuse dermal infiltrate of neoplastic lymphoid cells, centroblasts (C- shaped nucleoli) and immunoblasts (i-shaped nucleoli) [Figures 2, 3 and 4]. IHC showed diffusely positive CD20; BCL2, CD10 positivity, focal and weak positivity for MUM1, and MIB1 index 60–70% [Figure 5]. Positron emission tomography (PET) showed hypermetabolic ulcerative lesions up to intermuscular planes of the left distal leg and low-grade F-18 fluorodeoxyglucose (FDG)-avid left popliteal, inguinal and left pelvic nodes.
QuestionWhat is your diagnosis?
DiagnosisPrimary Cutaneous diffuse large B-cell lymphoma, leg type [stage IIE (E-skin), limited to skin, NCCN IPI-4 (H-I Risk), CNS IPI-2 (IR)].
TreatmentThe patient was referred to a higher centre, and started on R-CHOP regimen (single dose 500 mg IV Rituximab along with cyclophosphamide, doxorubicin, vincristine, prednisolone) for 6 cycles.
DiscussionPrimary cutaneous lymphomas are a heterogenous group of extranodal non-Hodgkin lymphomas originating in the skin without evidence of extracutaneous disease. Primary cutaneous B-cell lymphomas (pcBCLs) account for 25% of all cases.1
The incidence of pcBCL has been increasing and is currently about 4 per million persons. It is common in males over 70 years of age.1,2
As per the 2016 revision of the World Health Organisation (WHO), classification of lymphoid neoplasms includes three main types of pcBCL: primary cutaneous marginal zone lymphoma (pcMZL), primary cutaneous follicle centre lymphoma (pcFCL) and primary cutaneous diffuse large B-cell lymphoma (pcDLBCL)-leg-type (LT), as well as intravascular large B-cell lymphoma (IVLBCL).3
Distinct key features of all clinical subtypes of pcBCLS are discussed in Table 1.1
Table 1: Distinct features of three subtypes of Primary cutaneous B-cell lymphomas (pcBCLs)
Marginal zone lymphoma Follicle centre cell lymphoma Diffuse large B-cell lymphoma, leg type Clinical features Solitary or multiple papules,plaques, or nodules Solitary, grouped, or multiple papules, plaques, or nodules Solitary or multiple plaques and tumours Site Trunk and upper extremities Head, neck, and trunk Legs and rarely at other sites Age group Younger patients (median age, 55 years) Elderly patients (median age, 60 years) Elderly patients (median age, 76 years) Relapse Frequent cutaneous relapses (40%), rarely extracutaneousCutaneous relapses in (20%),
Extracutaneous in 5–10%
Frequent relapses and extracutaneous dissemination Histopathology Patchy periadnexal or diffuse infiltrates of small B cells lymphoplasmacytoid cells and plasma cellsFollicular, nodular, or diffuse infiltrates,
Centrocytes and centroblast
Diffuse infiltrates,
Centroblasts and immunoblasts
IHC* BCL2+, BCL6-, CD10- BCL6+, CD20+, BCL2- Ki-67, BCL-2+, MUM1+ 5-year survival rate (%) 99 95 50pcDLBCL-LT affects elderly females and clinically presents as single-to-multiple erythematous to violaceous tumours or nodules on the leg, with 10 to 15% on non-leg locations like the head and trunk.
Other clinical differential diagnoses of leg type could be pseudolymphoma, lymphomatoid granulomatosis, Burkitt’s lymphoma, deep fungal infection, nodular sarcoid, and other types of B-cell lymphoma. Histopathology shows diffuse infiltrates with the presence of centroblasts and immunoblasts. On IHC, the presence of Multiple myeloma oncogene-1 (MUM1) indicates an aggressive course.
The first-line treatment for pcDLBCL-LT with extracutaneous spread is chemotherapy combined with intravenous or intralesional rituximab (R-CHOP), which shows a good response rate with a longer disease-free interval. Other options are lenalidomide and radiotherapy.4
Spontaneous regression of the pcDLBCL-LT tumour after biopsy has been rarely reported.5 The prognosis is unfavourable if multiple lesions are on the legs and the age is more than 75 years. There is a high chance of relapse and extracutaneous spread, and the 5-year survival rate is approximately 50%.1 Hence, early recognition and awareness regarding this subtype are needed.
留言 (0)