Historically, the placement of percutaneous endoscopic gastrostomy (PEG) tubes in patients with higher body mass indexes (BMIs) has been viewed as a relative contraindication due to challenges related to gastric transillumination and the difficulty in approximating the abdominal and gastric wall.[1,2] Providing long-term care for these individuals requires specialized expertise in performing common invasive procedures.[2] With the introduction of image-guided procedures, percutaneous radiologic gastrostomy (PRG) has emerged as an effective solution for gastrostomy placement in patients with higher BMI.[3] The PRG technique allows for comprehensive identification and evaluation of all adjacent gastric structures, facilitating meticulous positioning of the feeding tube.[3] Studies have investigated the occurrence of post-operative complications following gastrostomy tube placement.[4,5] However, limited data are available regarding the influence of BMI on complication rates. The objective of this study was to assess whether patients with higher BMI exhibit distinct post-operative outcomes compared to their non-obese counterparts.
MATERIAL AND METHODS Data collectionThe Institutional Review Board has waived the ethical approval for this study. A single-center retrospective review of all radiographically guided percutaneous gastrostomy tube insertions from July 2017 to September 2020 was performed. Two hundred and seventy-three patients were included in this study, with 183 patients and 90 patients in the balloon-assisted gastrostomy (BAG) and dilator groups, respectively. Patients were stratified, based on BMI percentile for age, as being underweight (BMI<18.5), normal weight (BMI 18.5–24.9), overweight (BMI 25–29.9), class I obesity (BMI 30–34.9), class II obesity (BMI 35–39.9), or morbid obesity (BMI>40). Demographic information including indication, type of gastrostomy tube, insertion technique, fluoroscopy time, sedation requirements, and postoperative complications was collected.
Patients were categorized into two groups based on the method of tract dilatation: The BAG group (tract dilatation with an angioplasty balloon) and the dilator group (tract dilatation with Avanos telescoped or sequential dilators). Post-procedural complications following gastrostomy tube placement can be categorized into two distinct groups based on the criteria established by the Cardiovascular and Interventional Radiological Society of Europe (CIRSE): Minor complications and major complications. Minor complications encompass a range of issues such as tube dislodgement, pneumoperitoneum, infection, leakage, and minor bleeding.[6] On the other hand, major complications encompass more severe outcomes, including injury to another hollow viscus, buried bumper syndrome, necrotizing fasciitis, oculocutaneous fistula, and significant bleeding. All analyses were conducted using Chi-square or Kruskal–Wallis testing. Binary logistic regression analysis was performed to estimate the effect of predictors of interest on the presence of minor complications.
Fluoroscopic-guided tube procedureThe percutaneous fluoroscopy-guided gastrostomy tube placement procedure was performed by one of seven highly experienced interventional radiologists, each of whom has served as a faculty member in a tertiary care hospital. The necessary equipment, including a commercially available balloon or dilator gastrostomy kit, was made ready. The skin at the site of tube insertion was thoroughly sterilized using either povidone-iodine or chlorhexidine. The procedure was performed under general anesthesia (fentanyl or midazolam) to ensure patient comfort. The stomach was distended using air through a nasogastric tube. Three gastropexy T-fasteners were inserted into the gastric body and an incision was made at the center. Under fluoroscopy guidance, the gastrostomy tube, either BAG or dilator, was carefully inserted. In the BAG group, the G tube was pre-loaded onto a high-pressure Mustang balloon (Boston Scientific; Washington, D.C., US) for tract dilation. The gastrostomy catheter and balloon catheter were advanced together into the stomach as the balloon was slowly deflated, and the retention balloon of the gastrostomy tube was inflated and anchored to the stomach wall. In the dilator group, a telescoping serial dilator (Avanos Medical; Georgia, US) with a peel-away introducer sheath was used for tract dilation, followed by the insertion of the gastrostomy tube.
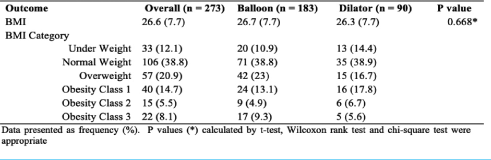
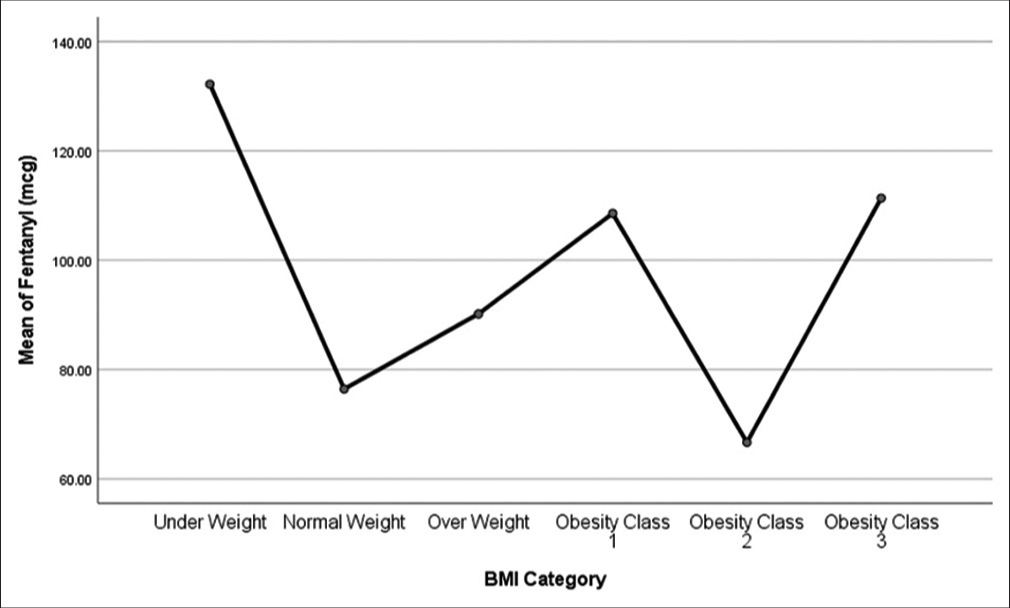
RESULTSThe study analyzed 273 patients who underwent gastrostomy insertion with either a balloon or a dilator. Among eligible patients, 198 (72.5%) were male and 75 (27.5%) were female. The median BMI was 26.6 kg/m2 with a standard deviation of 7.7 [Table 1]. 106 (38.8%) patients were classified in the normal BMI category, 57 (20.9%) were overweight, and 50 (28.3%) were classified as obese [Table 1]. Among the obese patients, 14.7% were in class 1 obesity, 5.5% were in class 2 obesity, and 8.1% were in class 3 obesity [Table 1]. The balloon group had a higher mean BMI compared to the dilator group; however, the difference was not statistically significant (BMI 26.7 balloon vs. 26.3 dilator, P = 0.07) [Table 1]. For pain management, patients in the underweight BMI category required the highest amount of fentanyl (Avg = 132.20, standard deviation [SD] = 179.82), while the lowest dose was given to patients in class 2 obesity (Avg = 66.67, SD = 65.24) [Graph 1].
Table 1: Outcome variables overall and by treatment group.
Export to PPT
Among the indications within the study population, neurological impairment was the most common (n = 152, 55.9%) in both balloon and dilator groups [Table 2]. Head-and-neck cancer was the second most common disease etiology observed in all patients (n = 47, 17.3%), followed by tracheostomy (n = 24, 8.8%), upper GI obstruction (n = 18, 6.6%), and inadequate oral intake (n = 21, 7.7%) [Table 2]. Indications for facial trauma (n = 4, 2.2%) and failure to thrive secondary to congestive heart failure (n = 4, 2.2%) occurred only in the balloon group [Table 2].
Table 2: Major and minor complications by treatment group.
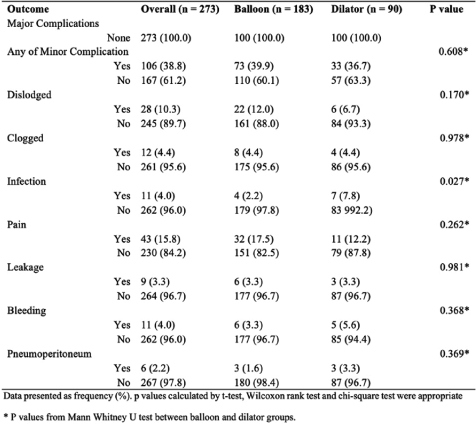
No major complications were reported in either group. Minor complications were reported by 106 patients (38.8%), as per the CIRSE classification system (grades 1 and 2) [Table 3]. The overall rate of minor complications (CIRSE grades 1 and 2) was higher in the balloon group but did not reach statistical significance (39.9% vs. 36.7% in the dilator group) [Table 3]. The most common complication observed across both groups was post-procedural pain, with a higher incidence in the balloon group compared to the dilator group (17.5% vs. 12.2%) [Table 3]. Dislodgement emerged as the second most common complication, occurring more frequently in the balloon group (12%) compared to the dilator group (6.7%) [Table 3].
Table 3: Minor complication overall versus body mass index categories.
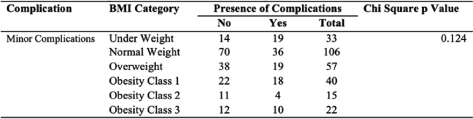
When considering weight categories, the overall rate of minor complications was highest among underweight patients (19/33 = 57.6% P = 0.124) [Table 4]. Class III obesity patients had the second-highest rate of minor complications (10/22 = 45.5%), followed closely by class I obesity patients (18/40 = 45.0%) [Table 4]. Both underweight and normal BMI patients showed a significantly higher incidence of tube dislodgement, compared to other BMI categories (27.2% and 9.4%, respectively, P = 0.015) [Table 5]. Patients in class I and III obesity had a higher incidence of clogged tubes (10% and 9.1%, respectively, P = 0.181) [Table 5]. There was a higher percentage of infection in the underweight BMI categories (9.1%, P =0.565). Underweight and class III obesity group had the highest reported pain complications (18.2%, P = 0.996) [Table 5]. Leakage had a higher reported incidence in the underweight BMI group (6.1%, P = 0.905) [Table 5]. Bleeding was more prevalent in class II and class III obesity groups (6.7% and 14%, respectively), however, did not reach statistical significance [Table 5]. There were six reported cases of pneumoperitoneum with the highest incidence in class I obesity (7.5%, P = 0.124) [Table 5].
Table 4: Minor complication subtypes versus body mass index categories.
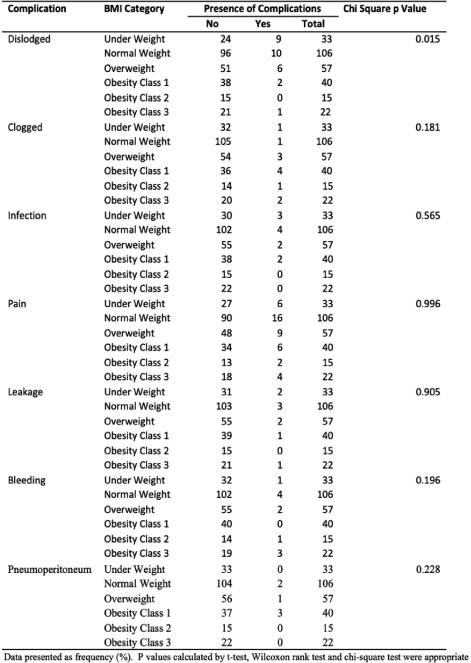
Table 5: Results from unadjusted and adjusted logistic regression models in minor complications (yes/no) as the dependent binary variable. Balloon treatment was used as the reference category. The adjusted model includes body mass index category and age as confounding variables.
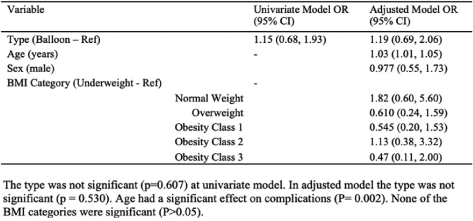
In a multivariable logistic regression, age was associated with an increased risk of minor complications (odds ratio [OR] 1.03, 95% confidence interval [CI] [1.01, 1.05], P = 0.002) [Table 5]. BAG had a greater OR for minor complication rate compared to dilator-assisted gastrostomy, although the difference was not statistically significant (OR 1.19, 95% CI [0.69, 2.06]) [Table 5]. Sex did not show a significant association (OR 0.977, 95% CI [0.55, 1.73], P = 0.94) [Table 5]. BMI classes of overweight, class I obesity, and class III obesity were associated with a higher incidence of minor complications compared to underweight, however, the difference was not statistically significant (P > 0.05) [Table 5].
DISCUSSIONGastrostomy tube placement is a frequently performed intervention aimed at facilitating enteral feeding in patients who are unable to adequately tolerate oral intake. Predicting the outcomes of this procedure has garnered considerable attention, with several factors being explored. Among these factors, BMI has emerged as a predictor for complications arising from percutaneous gastrostomy tube placement.[7] This study examined the relationship between BMI and complications following gastrostomy tube insertion.
The study results indicated that the type of dilator used did not significantly impact the risk of minor complications associated with gastrostomy tubes. Regardless of whether a balloon or dilator gastrostomy tube was used, there was no substantial disparity observed in terms of the overall complication rate. Further analysis comparing specific minor complications between the two types of tubes demonstrated a lack of statistically significant differences in six out of seven complications. Thus, it can be inferred that the choice between balloon and dilator gastrostomy tubes had minimal impact on the overall complication rate, given equal operative conditions within our cohort.
Catheter dislodgement is a common occurrence in percutaneous gastrostomy placement.[2,7] Typically, the gastrostomy tract matures within 1 week; however, this may be delayed in patients who are malnourished.[8] Specific care is required when addressing dislodgement as complications could result in the intraperitoneal spillage of gastric contents, leading to peritonitis and sepsis. Although leakage did not demonstrate statistical significance in the study, it is important to acknowledge that it was a documented complication that could occur following dislodgement. Patients in lower BMI classes exhibited increased rates of g-tube dislodgement, requiring subsequent tube replacement. As previously mentioned, the reduced subcutaneous fat around the g-tube insertion site in lower BMI patients can make the tube more susceptible to movement and discomfort. This discomfort may serve as a catalyst for patients to independently remove the gastrostomy tube, further contributing to the higher rate of dislodgement. One potential solution to address tube dislodgement is the implementation of T-tack placement.[9] This technique involves the use of specialized devices or sutures to secure the gastrostomy tube in place within the abdominal wall. This secure anchoring helps prevent unintentional movement or dislodgement of the tube.
The most common complication reported in the study was pain, though it did not reach statistical significance. This finding is consistent with previous studies that have identified post-procedural pain as one of the most common minor complications following gastrostomy tube insertion.[8,10] Patients categorized in the underweight BMI exhibited an increased incidence of pre-procedural pain management and post-surgical pain complications in contrast to those in higher BMI categories. This phenomenon may be attributed to lower tissue and adipose layers, thus diminishing the cushioning effect on the implanted gastrostomy device and consequently intensifying pressure and discomfort. It is important to note that patients in the class III obesity group also required higher doses of fentanyl, suggesting an increased requirement for pain management during the procedure. Similarly, patients in the class III BMI group showed an increased incidence of reported abdominal pain, though not statistically significant. Patients with higher BMI are associated with a thicker abdominal wall, in turn making access and visualization of the gastric lumen more challenging. The increased adipose tissue may require more strain and manipulation on the abdominal wall, with resultant pain and discomfort for the patient. However, further studies are needed to validate these claims in explaining the varying pain management needs among patients with low and high BMIs. Here, it is worth noting that increased pressure from adipose tissue around the stroma site could lead to clogging of the g-tube. Moreover, although clogged complications did not reach Chi--square significance in our investigation, the gross percentages showed that patients in the class I obesity group had the highest occurrence of clogged g-tubes followed by overweight individuals.
Numerous studies have established a correlation between patients in higher BMI categories and the occurrence of surgical site infections and pneumoperitoneum.[9,11,12] Specifically, higher levels of body fat have been associated with an increased risk of infection at the surgical site. Although the infection rate did not achieve statistical significance, the gross relative percentages indicated that a decrease in BMI increased the odds of surgical site infection. This unexpected finding may be attributed to the proximity of the gastric lumen to the skin surface during the procedure, thus increasing the risk of infection in thinner patients. The presence of increased subcutaneous fat between the gastric lumen and the skin could potentially serve as a protective mechanism from infection.
In our study population, it was observed that age demonstrated a significant association with the risk of minor complications [Table 5]. One explanation for this association is that older patients tend to have a higher prevalence of comorbid conditions. The presence of multiple comorbid conditions in older patients can significantly impact their overall health status and physiological resilience. These findings suggest that age should be regarded as a critical factor when evaluating the likelihood of minor complications arising after the insertion of a gastrostomy tube insertion. It is worth noting that while age is an important factor, it should be considered in conjunction with other factors such as frailty, nutritional status, and functional abilities. These additional factors may also contribute to the increased risk of procedural complications in older patients.
When compared to a widely adopted gastrostomy method such as PEG, the PRG method offers an alternative approach to delivering enteral nutrition.[7,12] Several studies have demonstrated that fluoroscopic techniques exhibit higher success rates and lower rates of major complications compared to endoscopic techniques.[6,13-16] Despite this, a notable vulnerability in radiologically-inserted gastrostomy (RIG) is the necessity for smaller gastrostomy tube sizes, rendering them more susceptible to blockages and necessitating additional interventions.[13,17]
The retrospective nature of this study and its evaluation from a single institution’s perspective imposes several limitations. The sample size was relatively small, which might have resulted in an increased likelihood of random variation, reducing the statistical power. Although this investigation provided valuable insights into the outcomes and complications associated with PRG, it recognizes the absence of specific patient data related to endoscopically placed tubes in the current study. In future studies, a prospective randomized clinical trial between PRG and PEG methods would offer clinician’s valuable information for selecting the most suitable method based on BMI. Furthermore, this comparison would contribute to the development of evidence-based guidelines for percutaneous gastrostomy tube insertion, considering the diverse patient population and their varying anatomical and physiological characteristics.
CONCLUSIONPRG tube placement serves as a crucial intervention in interventional radiology, offering not only sustained enteral access for patients with compromised nutrition but also effective gut decompression. Our results showed patients in lower BMI classes exhibited increased rates of gastrostomy tube dislodgment and procedural pain management. Age demonstrated a significant association with the risk of minor complications. This study provides valuable insight into predicting and preventing complications in gastrostomy tube placement following gastrostomy tube insertion and highlights areas where more attention is needed to improve patient outcomes.
留言 (0)