A 72-year-old woman was referred to a tertiary hospital with a high fever. The complete blood count showed pancytopenia (hemoglobin, 8.0 g/dL; white blood count, 2.97 × 109/L; and platelet count, 30 × 109/L). Her serum level of fibrinogen was normal, but that of triglyceride was 453 mg/dL (reference range 0–200 mg/dL), and ferritin was 904.0 ng/mL (reference range, 13–150 ng/mL). There was no splenomegaly or enlarged lymph nodes in the computed tomography scans. On the peripheral blood (PB) smear, leukoerythroblastosis and circulating neoplastic lymphoid cells (1%) were found (
Fig. 1A). A bone marrow (BM) study was performed, and there was a significant number of neoplastic lymphoid cells (21.6%), which showed large sizes, indented nuclei with a clumped chromatin pattern, and a basophilic cytoplasm with cytoplasmic vacuoles (
Fig. 1B). The number of histiocytes was also increased (3.4%), with the presence of hemophagocytic histiocytes engulfing nucleated cells (
Fig. 1C). The neoplastic lymphoid cells showed strong positivity for CD20 (
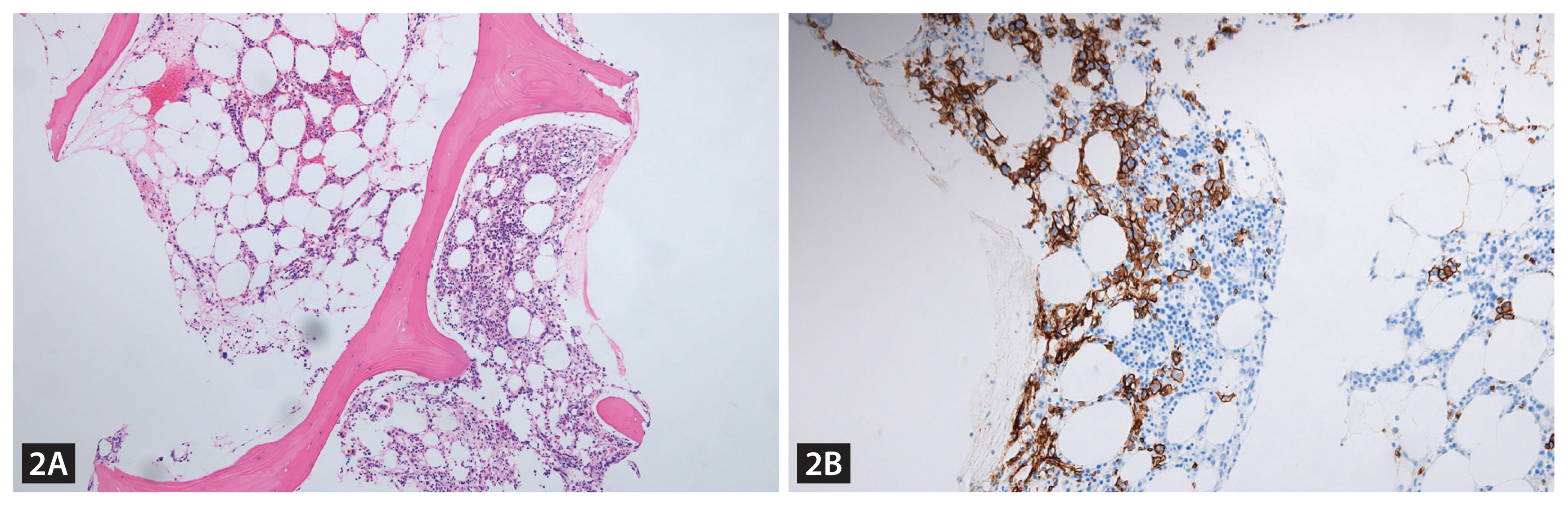
Fig. 2). An additional laboratory workup for hemophagocytic lymphohistiocytosis (HLH) was performed, and the results were as follows: NK-cell activity, 18 pg/mL (reference range ≥ 500 pg/mL), and soluble interleukin-2 receptor level, 7,500 U/mL (reference range, 220–530 U/mL). Based on these findings, she was diagnosed with HLH due to the BM involvement of diffuse large B-cell lymphoma. After one cycle of rituximab, cyclophosphamide, doxorubicin hydrochloride, vincristine and prednisone, the fever was reduced, and pancytopenia was normalized. The follow-up PB smear and BM study showed no evidence of lymphoma involvement. Therefore, the patient reached complete remission status.
The frequent clinical features of HLH are fever, hepatosplenomegaly, and lymphadenopathy. Sometimes an underlying malignancy might be masked by HLH due to the similarity of clinical signs. Therefore, the diagnosis and evaluation of the cause of HLH should be made carefully.
Acknowledgments
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Ethics Committee of Soonchunhyang University (No. 2022-12-060).
NOTES
CRedit authorship contributions
Min-Sun Kim: writing - original draft; Bohyun Kim: conceptualization, data curation, methodology, writing - original draft; Han-Jo Kim: data curation, writing - original draft, writing - review & editing; Sang-Cheol Lee: methodology
Conflict of interest
The authors disclose no conflicts.
NOTES
Funding
This study was supported by the Soonchunhyang University Research Fund.
Figure 1
Peripheral blood smear at diagnosis showed circulating lymphoma cells (Wright-Giemsa stain, ×1,000) (A). Bone marrow aspiration smear showed numerous large neoplastic lymphoid cells, which showed large sizes, indented nuclei with a clumped chromatin pattern, and a small amount of basophilic cytoplasm with cytoplasmic vacuoles (B), and histiocytes with the active hemophagocytosis of hematopoietic cells (C) (B: Wright-Giemsa stain, ×1,000; C: Wright-Giemsa stain, ×1,000).
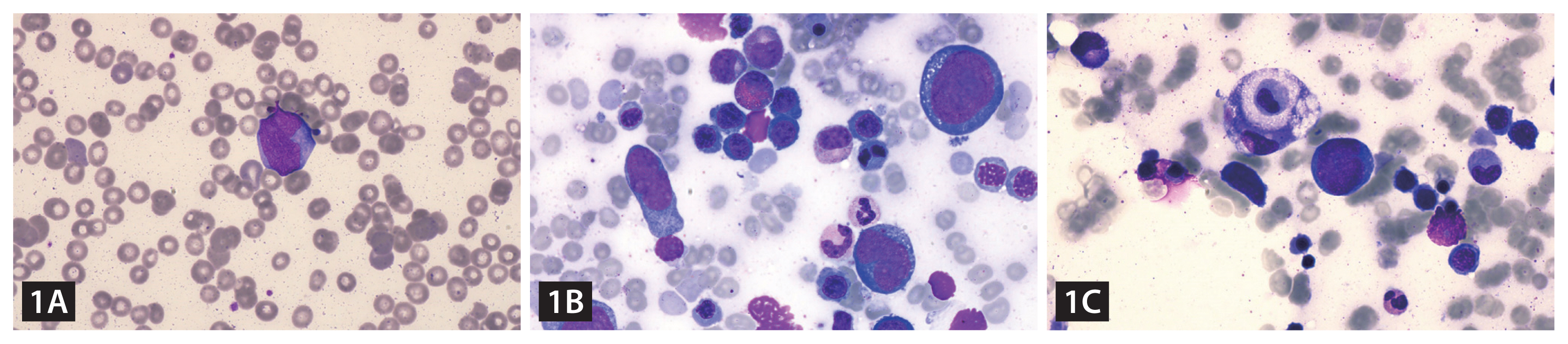
Figure 2
Bone marrow biopsy showed the interstitial infiltration of neoplastic lymphoid cells (Hematoxylin and Eosin stain, ×100) (A). Immunohistochemical staining of the bone marrow biopsy specimen for CD20 (IHC stain for CD20, ×400) (B). The large-sized neoplastic lymphoid cells showed CD20-positivity.
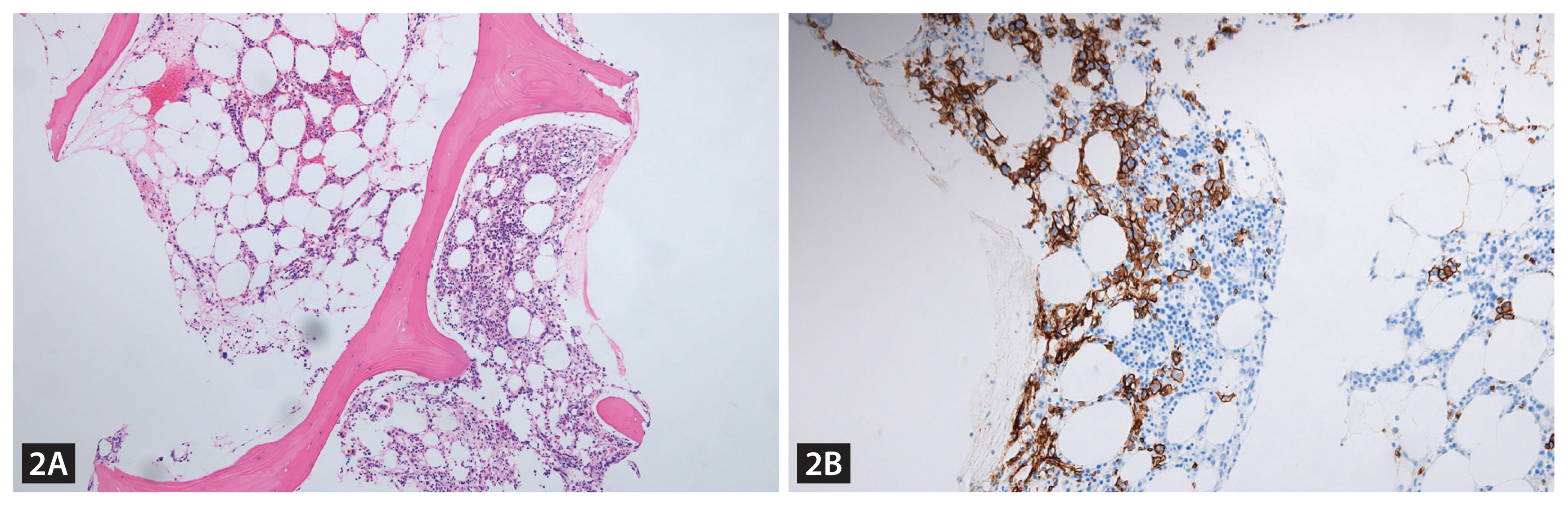
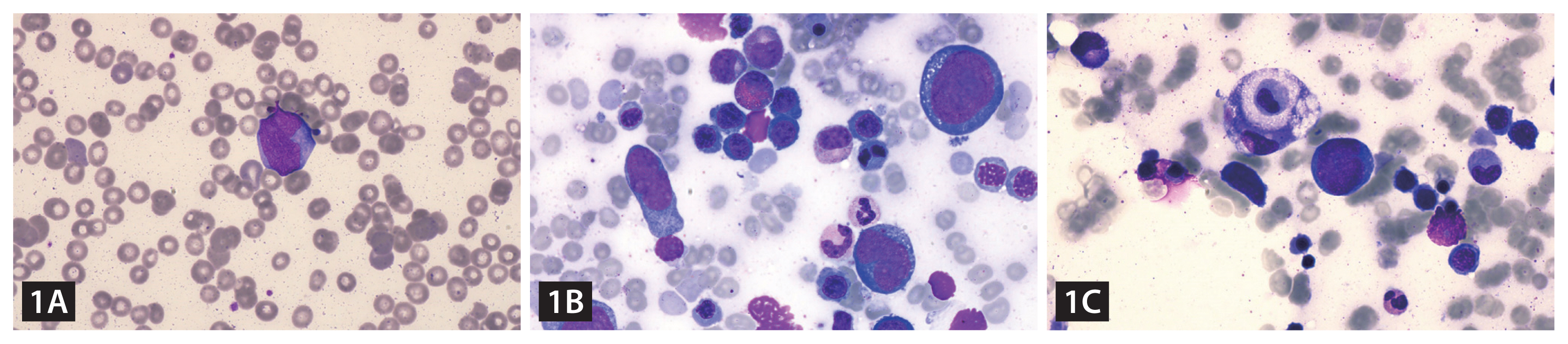 Figure 2
Figure 2
留言 (0)