Sir,
Phototherapy is an effective treatment in children with stable vitiligo and is generally quite safe. However, a rarely reported adverse effect is the development of small well-defined depigmented macules in the areas exposed to ultraviolet radiation. These have been described variably as leucoderma punctatum,1 confetti-like hypopigmentation and idiopathic guttate hypomelanosis-like lesions.2 These macules have not been well characterised, and their dermoscopic features have not been described in detail. They have been reported only in a few case reports and series.1
Five children with stable vitiligo receiving photochemotherapy with topical psoralen followed by sun exposure as a source of ultraviolet A (PUVAsol therapy) for the varying duration were noticed to have multiple small well-defined depigmented macules of size 1–5 mm in and around the vitiliginous skin [Table 1 and Figures 1a–e]. These were restricted to the area which was exposed to photochemotherapy. These macules had started after a few months after initiation of PUVAsol therapy and increased in number as the photochemotherapy was continued, although there was mild to good re-pigmentation in the vitiligo lesions. These new depigmented macules were relatively smaller and brighter white, compared to the chalky white hue and larger size of existing vitiligo lesions. When present within vitiligo patches, their boundaries could be delineated due to different hues of depigmentation.
Table 1:: Patients’ profile and duration of photochemotherapy in the form of topical psoralen followed by sun exposure as a source of ultraviolet A (PUVAsol therapy) for vitiligo
No. Age (years) Duration of phototherapy Discontinued since Photo-sclerosis 1 9 6 months 3 years No 2 14 6 months 6 months No 3 6 14 months Continuing Yes 4 10 10 months Continuing Yes 5 12 4 months Continuing Yes
Figure 1:: Idiopathic guttate hypomelanosis-like macules developing after photochemotherapy. (a-e) Clinical pictures of 5 different patients, showing development of these lesions over vitiligo patches (circle) and surrounding hypopigmented (square), hyperpigmented (solid arrowhead), and normal skin (hollow arrowhead). (f-j) Their respective dermatoscopic pictures showing feathery (blue arrow), amoeboid (black arrow), petaloid (red arrow) and nebuloid margins (star). (Heine Delta 20T, magnification 10×)
Export to PPT
On dermoscopy, they had central white structureless areas which lacked a pigmentary network and had multiple convex outpouchings and extensions of their border, suggestive of a petaloid, amoeboid, feathery or nebuloid margin, and a cloudy/popcorn-like appearance [Figures 1f–j].
A biopsy from one lesion located over the hyperpigmented skin of the forearm showed mild papillomatosis and hyperkeratosis, mild flattening of rete ridges, and near absence of basal layer pigmentation in a large section of the slide. The transition between pigmented and non-pigmented basal layer was abrupt and prominent [Figure 2]. No biopsies were performed on other patients.
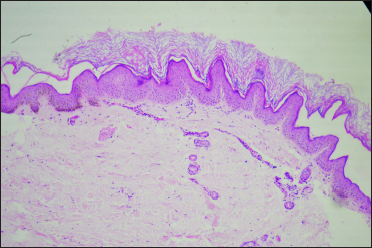
Figure 2:: Histopathology of idiopathic guttate hypomelanosis-like macules over forearm developing after photochemotherapy. Hyperkeratosis, mild papillomatosis and an abrupt transition of normally pigmented basal cell layer to the zone with a near complete absence of melanin in the basal layer. (Haematoxylin and eosin, ×100)
Export to PPT
The presence of lesions exclusively in the distribution of psoralen application and an increasing number of continuing phototherapy supports photochemotherapy as the possible cause for these lesions. Patients three and four had received phototherapy for the maximum duration and had the maximum density of these macules. Patient one had discontinued phototherapy for three years and had the least density.
Small well defined depigmented macules are known to develop after phototherapy in vitiligo,1 psoriasis and mycosis fungoides2 and have been termed as leucoderma punctatum,1 confetti-like hypopigmentation or idiopathic guttate hypomelanosis-like2 (IGH -like) macules. The differential diagnosis of such lesions include punctate vitiligo or vitiligo puncture, also known as confetti vitiligo, and guttate lichen sclerosis [Table 2]. Hypopigmented PUVA keratosis is another differential, which is photo-induced, but the lesions are elevated papules rather than macules.3
Table 2:: Differentials of idiopathic guttate hypomelanosis due to photochemotherapy
Differential Points in favour Points against Confetti vitiligo – Morphology of small depigmented maculesAlthough these lesions have been reported before as IGH-like2 macules, in view of the characteristic dermoscopic features of amoeboid, petaloid, and feathery margins, we opine that these may actually be IGH rather than IGH-like macules.4 The proposed pathogenesis of IGH is multifactorial and implicates photodamage. In fact, IGH has been considered a manifestation of photoaging,5 and occurrence in children in localised areas with long-term intense photo exposure lends credence to the hypothesis that these lesions could be IGH. These IGH-like lesions indicate chronic photodamage and localised premature photoaging in these children. Interestingly, three out of five patients had evidence of chronic phototoxicity in form of photo-sclerosed skin.
Interestingly, even the reported histopathology of these macules is similar to IGH. Both conditions have been reported to show a significant decrease/ near complete absence of melanin and functional melanocytes in the basal and suprabasal layers.1,2,6 A subset of both conditions may show some hyperkeratosis, which when significant may result in clinically raised lesions of hypopigmented keratosis, an entity that probably represents the raised hyperkeratotic variant of IGH.1,3,6 Some patients of both conditions also show epidermal atrophy and flattening of rete ridges.1,6 Interestingly, the focal or patchy presence of melanin, as described by Falabella et al. in leucoderma punctata in 1988, is now a known feature of IGH, described as skip areas.1,7
Although our series is composed of children, IGH-like macules can appear in any age group and is not exclusive to children. Narrow-band ultraviolet B phototherapy can also lead to eruptive IGH-like macules and they are not limited to just psoralen-induced photochemotherapy.2
Photochemotherapy was stopped in all five patients, and they were shifted to mid-potent topical steroids. They were followed for 1–3 months, with no change in either vitiligo patches, IGH-like macules, or extent of re-pigmentation.
In conclusion, it is important to be aware of this rare side effect of phototherapy, as the dyschromia caused by these lesions may offset any benefit of re-pigmentation by phototherapy. As IGH-like macules are dose-dependent and potentially reversible, phototherapy should be discontinued if patients or their guardians perceive a worsening of the appearance of vitiligo lesions due to them.
In this series, we have characterised a rare side effect of photochemotherapy with dermoscopic findings and its putative aetiopathogenesis. We have also highlighted the fact that IGH-like macules following photochemotherapy occur on vitiliginous, re-pigmented and normal skin.
The limitations of this series include a lack of histopathology in all patients and a short follow-up period. There’s a need for further studies with a clinicopathological correlation of lesions at different coloured skin, and with longer follow-up to see the extent of the resolution of these lesions on stopping phototherapy. More robust studies can establish if these IGH-like macules are indeed IGH.
留言 (0)