A 37-year-old woman presented with an asymptomatic lesion on the scalp of 2–3 years duration which showed a slight increase in size over the last one year. The lesion caused much discomfort while combing hair and also “cancer” anxiety in the patient. On inquiry, the patient did not have any significant medical or surgical history in the past. Local examination revealed a skin-colored, smooth-surfaced, broad-based pedunculated nodule of an approximate size of 6 × 5 ×10 mm. Surrounding scalp skin appeared normal. On palpation, it was non-tender and firm in consistency. The lesion was excised and sent for histopathological evaluation [Figure 1]. The histology of the excised specimen revealed an epithelial neoplasm which was symmetrical with rounded outlines in the dermis. The neoplasm was composed of multiple tumor islands separated by intervening stromal connective tissue with only a focal connection with overlying epidermis [Figure 2]. The tumor islands were composed of an admixture of immature basaloid cells and mature sebocytes in varying proportions. Basaloid cells showed monomorphic round to oval nuclei with scanty cytoplasm. Scattered mature cells had abundant pale, bubbly cytoplasm and small scalloped nuclei suggestive of sebaceous differentiation [Figure 3]. Cysts and ductal structures were present [Figure 4]. The labyrinthine or sinusoidal pattern in the basaloid component was seen [Figure 5]. Occasional mitotic figures were present within the neoplasm.

Figure 1:: Broad-based pedunculated skin-colored nodular lesion
Export to PPT
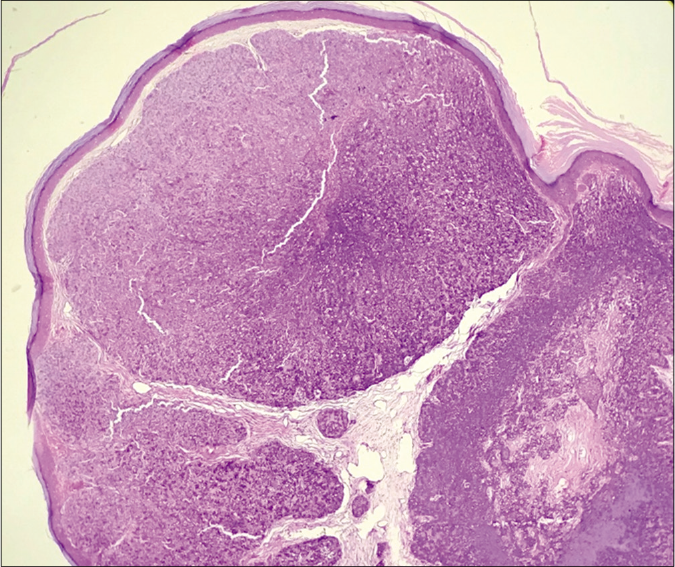
Figure 2:: Multiple tumor islands with intervening stroma in the dermis (H and E × 40) scanner view
Export to PPT

Figure 3:: Admixture of basaloid cells (green arrows) and scattered mature sebocytes (red arrows) within tumor islands (H and E ×400)
Export to PPT
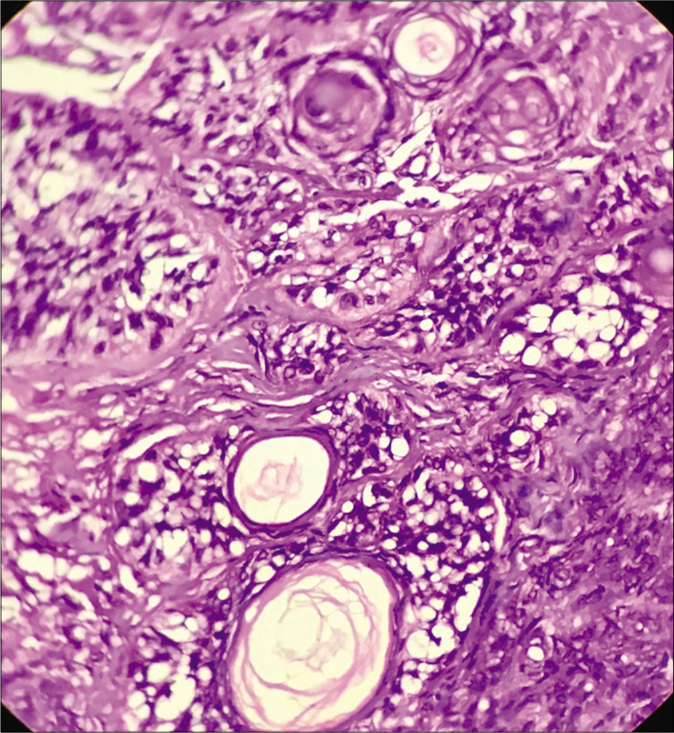
Figure 4:: Ducts and cystic structures with mature sebocytes (H and E ×400)
Export to PPT
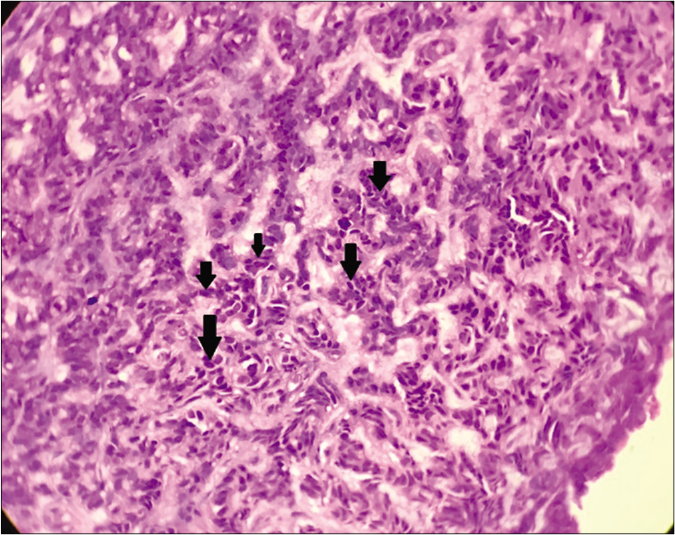
Figure 5:: Labyrinthine/sinusoidal pattern of basaloid cells (black arrows) (H and E ×400)
Export to PPT
QuestionWhat is your diagnosis?
AnswerSebaceoma
DiscussionSebaceoma was first described by Troy and Ackerman in 1984 as a benign neoplasm with sebaceous differentiation mostly affecting elderly womenin the head and neck region. It was earlier called sebomatrixoma or sebaceous epithelioma, erroneously indicating malignancy, hence best avoided.1
Classically, these tumors present as yellow or skin-colored nodules of varying sizes either solitary or multiple. They may even occur within the nevus sebaceous. Histologically, the tumor is composed of variable proportions of mature sebocytes and immature sebaceous germinative cells within multiple tumor nodules separated by eosinophilic connective tissue in the dermis. The percentage of immature basaloid cells is usually quite high compared to fewer and mostly scattered mature sebocytes. The connection of tumor nodules with overlying epidermis may or may not be present. Sebaceous ductal structures with holocrine secretions areusually seen within the nodules. Infundibulo cystic structures, areas with apocrine differentiation, squamous metaplasia and keratoacanthoma like architecture are other uncommon features. A few nearly specific organoid patterns which help in the diagnosis of this entity, include rippled pattern, labyrinthine/sinusoidal pattern, carcinoid pattern and petaloid pattern. The rippled pattern is characterized by palisades of neoplastic cells arranged in parallel rows like a ripple, reminiscent of schwannian Verocay bodies. In the labyrinthine or sinusoidal pattern, there is an intricate and tortuous arrangement of various strands and cords of neoplastic cells. Carcinoid pattern comprises trabeculae, ribbons, rosettes and pseudo-rosette-like arrangement of basaloid cells similar to growth patterns in carcinoid tumors. The petaloid pattern shows a flower-like pattern of cells.2
Our provisional clinical diagnosis was cutaneous adnexal neoplasm. Based on clinical features in our case, the important histological differential diagnoses were trichoblastoma or apocrine poroma with sebaceous differentiation. Trichoblastoma with sebaceous differentiation does show large nodular aggregates of basaloid cells and rippled patterns of cells but follicular differentiation and occurrence of germ-papilla arrangement of cells help to differentiate it from sebaceoma. The presence of poroid and cuticular cells with tubular structures and large areas showing apocrine differentiation characterizes apocrine poroma.3
Sebaceous differentiation is usually easily discernible based on mature sebocytes and ducts within the neoplasm. However, in difficult cases, immunohistochemistry marker studies may be done. Mature sebcaeous cells are positive for epithelial membrane antigen and adipophilin.4,5
Dermoscopy serves as an important interface between clinical diagnosis and histological confirmation of skin lesions in current times. Yellowish homogenous ovoid areas correlating with collections of mature sebocytes and arborizing vessels in the periphery of the nodule have been reported which has important clues to the dermoscopic diagnosis of a sebaceoma.6
The occurrence of multiple sebaceous tumors associated with visceral neoplasms, especially gastrointestinal carcinomas characterizes Muir-Torre syndrome which is inherited as an autosomal dominant trait. It is associated with a mutation in genes encoding DNA mismatch repair proteins like MLH1 and MSH2 mainly and less commonly MSH 3, MSH6, MLH3, PMS1 and PMS2.4,5
Herein, we report this case not only for its rarity but also to reinforce the awareness of various histological patterns, differential diagnosis and systemic implications of this unique neoplasm.
留言 (0)