Sir,
Chronic active Epstein-Barr virus (EBV) infection is a rare lymphoproliferative disorder that presents with prolonged infectious mononucleosis-like symptoms and a sustained EBV deoxyribonucleic acid (DNA) load in the peripheral blood. It is a type of progressive disease that presents with benign, borderline or malignant histologic morphology and varied biological behaviour.1 Patients with chronic active Epstein-Barr virus often presents with fever, hepatosplenomegaly, lymphadenopathy, gastrointestinal damage, pancytopenia, interstitial pneumonia, a variety of rashes, etc. However, chronic active Epstein-Barr virus mimicking dermatomyositis is rare. We herein report such a case report.
A 27-year-old male complained of swelling and redness of the face along with weakness of limbs for two months. High fever was also present during the course of the disease. Physical examination revealed oedema of face including both eyelids, dark erythema, papules, hyperpigmentation and crusting on the limbs and trunk [Figure 1 (a-c)]. Two peanut-size lymph nodes were palpable, one each in the left supraclavicular and left inguinal region. The power of the muscles in the proximal extremities was grade IV.

Figure 1a:: Swelling of both eyelids and face. Oedematous dark erythema, papules, hyperpigmentation and crust were noted on the limbs and trunk
Export to PPT
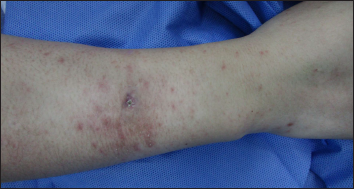
Figure 1b:: Oedematous dark erythema, papules, hyperpigmentation and crust were noted on the right forearm
Export to PPT

Figure 1c:: Oedematous dark erythema, papules and crust were noted on the right thigh
Export to PPT
Laboratory examinations showed the alanine aminotransferase level to be 102 IU/L (Normal <50 IU/L) and the creatine phosphokinase level to be 2342 IU/L (19~226 IU/L). Electromyography revealed myogenic damage of deltoid muscle, biceps brachii muscle and vastus medialis muscle, with spontaneous potential and shortened duration of light force contraction. Correlating the clinical and laboratory findings, a diagnosis of dermatomyositis was made. However, immunologic testing was negative. Biopsy of the necrotic papules on the forearm showed dense lymphoid cell infiltration in the dermis and subcutaneous layer of fat. The infiltrating cells were most positive for Epstein-Barr virus-encoded RNA (EBER)1/2, minority positive for CD3, CD5 and T-cell intracellular antigen (TIA)-1, weakly positive for cluster of differentiation (CD)56 and granzyme B (GrB), but negative for CD2, CD4, CD7, CD8, CD20 and CD30. The Ki-67 proliferative index was approximately 20% [Figure 2 (a-i)]. Biopsy specimens from the right deltoid muscle showed a large amount of focal infiltration of medium-sized atypical lymphocytes with irregularly shaped nuclei, around the muscle fibre. Immunophenotype analysis showed atypical lymphocytes were most positive for CD3 and EBER1/2, partially positive for CD2, CD4, CD5, CD7, CD8 and TIA-1, minority positive for CD20, CD30 and GrB, and weakly positive for CD56. The Ki-67 proliferative index was approximately 10~20% [Figure 3 (a-f)]. Biopsy of the lymph node displayed proliferation of medium-sized lymphocytes, mainly infiltrating the paracortical area [Figure 4 (a-f)]. Immunophenotype analysis showed that the atypical lymphocytes were majority positive for CD3, CD30 and EBER1/2, partially positive for CD2, CD4, CD5, CD7 and TIA-1, minority positive for CD8, CD20 and GrB, weakly positive for CD56, but negative for CD79a and Epetein-Barr virus nuclear antigen (EBNA)2. The Ki-67 proliferative index was approximately 30~40%. T-cell receptor gene rearrangement of the three samples was negative. At the same time, the levels of EBV-associated antibodies were as follows: VCA (virus capsid aantigen)-IgA - 2.55 S/CO and EA-IgG >200 RU/mL. Upon performing a real-time quantitative polymerase chain reaction, 2.31×104 copies of EBV per mL of plasma were observed.
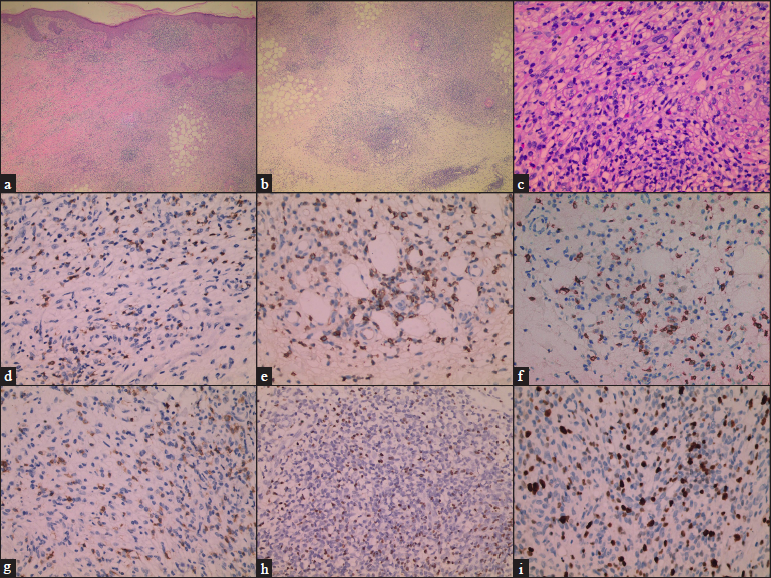
Figure 2a-i:: (a) Large number of inflammatory cells were observed in the whole dermis (H&E,×40), (b) A large number of inflammatory cells were observed in the subcutaneous adipose layer (H&E,×40), (c) Some of the infiltrates were prominently composed of medium-sized atypical lymphocytes that had clear cytoplasm with irregularly shaped nuclei (H&E,×200), (d) CD2 positive (×200), (e) CD3 positive (×200), (f) CD5 positive (×200), (g) CD7 positive (×200), (h) EBER-positive (×200), (i) The Ki-67 proliferative index was approximately 20% (×200).
Export to PPT
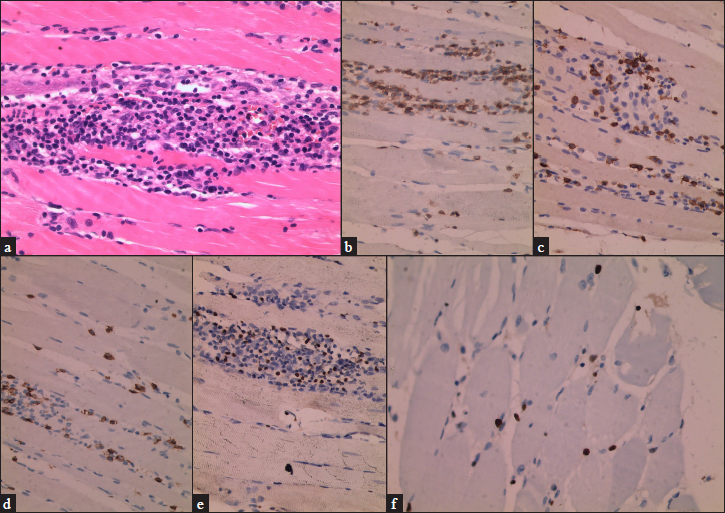
Figure 3a-f:: (a) A large number of medium-sized atypical lymphocytes with irregularly shaped infiltrated muscle fibre (H&E,×400), (b) CD3 positive (×400), (c) CD5 positive (×400), (d) CD8 positive (×400), (e) EBER-positive (×400), (f) The Ki-67 proliferative index was approximately 20% (×400).
Export to PPT
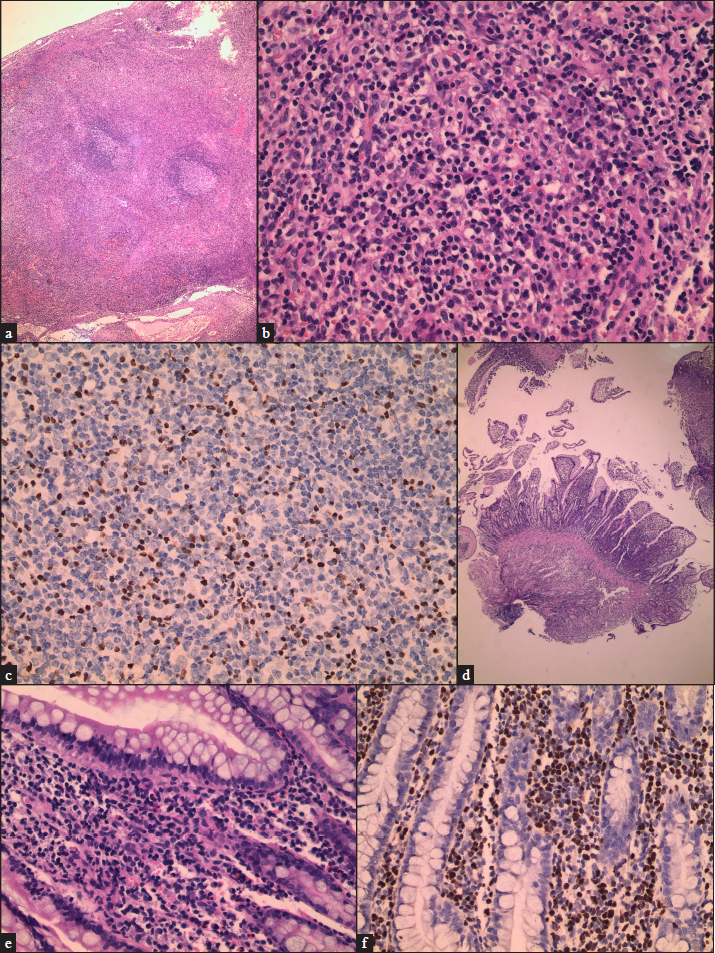
Figure 4a-f:: (a) A large number of lymphocytes infiltrated the paracortical area of lymph node (H&E,×40), (b) A large number of medium-sized atypical lymphocytes with irregularly shaped infiltrated the paracortical area of lymph node (H&E,×100), (c) EBER-positive (×200), (d) A large number of lymphocytes infiltrated the ileum (H&E,×40), (e) A large number of medium-sized atypical lymphocytes with irregularly shaped infiltrated the ileum (H&E,×400), (f) EBER-positive (×200).
Export to PPT
Patient was diagnosed to have chronic active EBV infection and treated with prednisolone. Four months later, he suffered from recurrent ileal bleeding and perforation. Whole-body positron emission tomography/computed tomography, biopsy and immunohistochemical of the ileum confirmed that the disease had transformed from previously inert chronic active EBV to lymphoma and he died five months after confirmation of chronic active EBV infection Figure 4 (a-f).
So far we found only two previous reports of chronic active EBV involving the skin and skeletal muscle mimicking dermatomyositis.2,3 The principal manifestations of the patients were eyelid or facial swelling with EBER-positive T or natural killer (NK) cell infiltration in the muscles mimicking dermatomyositis. However, in our patient, the skin lesions were more varied, and the symptoms of muscle weakness and extensive muscle involvement were more obvious.
Because of the difference in the treatment to be given and the prognosis, it is crucial to distinguish chronic active EBV-related myositis from dermatomyositis. Chronic active EBV-related cutaneous manifestations are variable, including discrete ulcerated papules, papulo-vesicles and nodules, which heal with scarring and pit formation. Some patients also show hydroa vacciniforme - symptoms or hypersensitivity to mosquito bites. On the contrary, highly diagnostic skin lesions of dermatomyositis are heliotrope rash, Gottron’s papules and Gottron’s sign.4
Laboratory test also provides certain clues. Elevated levels of anti-EA-IgG antibody and anti-VCA-IgA antibody contributed to determine EBV infection in our case. More importantly, the EBV DNA load in the peripheral blood by polymerase chain reaction is more than the cut-off value of 10copies/µg DNA, which is a diagnostic criterion of chronic active EBV.1 Besides, it is important and useful to identify EBER1/2 in pathological tissue specimens.
Research has shown that immunosuppressive therapy, including corticosteroids, cyclosporine and azathioprine, may transiently relieve symptoms in some patients but cannot stop the progression of the disease.5 However, most patients with dermatomyositis show a relatively good response to corticosteroids. Therefore, when an atypical rash associated with muscle involvement shows a relatively poor response to corticosteroids, chronic active EBV-associated myositis should be suspected.
Usually, the difference in the clinical picture, laboratory findings and treatment response to corticosteroids may help in distinguishing between dermatomyositis and chronic active EBV-associated myositis. But when chronic active EBV progresses to lymphoma, dermatomyositis-like presentation, chronic active EBV and lymphoma may occur in succession or simultaneously in our case, thereby hindering a complete distinction. Dermatomyositis is the most frequent paraneoplastic syndrome involving muscle in patients with lymphoma. Thus, it is necessary to use whole-body positron emission tomography/computed tomography to search for potential tumours in these patients.
In conclusion, we reported a rare case of chronic active EBV infection mimicking dermatomyositis.
留言 (0)