Snakebite is a neglected health problem around the globe, causing considerable morbidity and mortality.1 In 2017, the WHO reclassified snakebite as a neglected tropical disease (NTD).2 An estimated 50 000 individuals die in India every year following snakebite and yet there is a paucity of data with regard to snakebite management, hospital course and outcomes.3
Information available about the profile of snakebite victims in Central Kerala, which probably has one of the highest incidence of envenomation in India, is limited.4–7 Electronic medical records and data retrieval systems do not exist in rural hospitals catering to snakebite victims and hence obtaining data is difficult.
We aimed to review the existing clinical case records to understand the clinico-epidemiological profile and to describe the epidemiology, clinical features, complications, the use of anti-snake venom (ASV) and blood products in snakebite cases that presented to one of the high-volume centres catering to envenomation victims in central Kerala.
This was conducted as a pre-pilot single-centre study, with a secondary objective to analyse and identify the dataset to establish a regional snakebite registry. The pilot phase of the registry commenced soon after procurement of the data.
METHODS Study design and settingThis was done as the Phase 1 of a three-phased structured study to establish a regional snakebite registry. The project progressed as follows: Phase 1, a retrospective single-centre record review of snakebite victims (pre-pilot phase); Phase 2, a prospective single-centre clinical cohort study (pilot phase) and Phase 3, establishment of a prospective regional multicentric snakebite registry.
Currently, the project is in Phase 2. Phase 1 was carried out at a single centre, Jubilee Mission Medical College and Research Institute, Thrissur, Kerala, India, over a period of 5 years after approval from the Institutional Review Board (IRB) and Institutional Ethics Committee (IEC number: 04/19/IEC/ JMMC&RI).
Inclusion and exclusion criteriaAll patients aged 18 years and above, who presented with a history of venomous snakebite from January 2010 to January 2015, were included in the study.
For the purpose of the study, a snakebite was defined as ‘venomous snakebite’ if:
The snake brought along was documented as venomous OR
The patient developed signs and symptoms of envenomation as defined by the WHO guidelines.8
All incomplete or destroyed case records were excluded.
Data collection processAdmission registers maintained at the emergency department, medical intensive care unit (ICU), general medicine ward, nephrology ward, dialysis unit, pharmacy and medicolegal department records were collated and cross-verified with the hospital admission registers to avoid duplication of data.
The medical records of all individuals satisfying both the inclusion and exclusion criteria were selected for the study.
Data on the epidemiological factors, pre-hospital care received, clinical features, laboratory investigations, complications, details of the treatment and outcome were recorded.
The geographical location where they were bitten (if recorded) was plotted on Google Maps® and the shortest distance by road to the institute was recorded.
Retrospective regional weather data were procured from the India Meteorological Department.
A detailed proforma was prepared and de-identified data of all individuals were collected from the time of admission to discharge.
No items of information that would enable the identification of any subject was recorded in this study, and no linking list of any sort was kept to protect the identity of the study subjects.
The medical records individually handwritten by the treating physician were reviewed by a single data abstractor over a period of 6 months (SR). The data abstractor was initially trained for one month, and the data were collected on an Excel spreadsheet designed for the study. Data collection was limited to less than 10 entries a day. The data entered were cross-verified by the records department in-charge and members of the investigation team (RJM and SVA) to both avoid endogenous human error and ensure anonymity of the patient. Typographical entry errors flagged by the medical records officer were re-checked and appropriate corrections were made.
For the purpose of this study, information about the following parameters was analysed:
Demographics and clinical details (age, gender, time of bite and admission time, bite to hospital time, clinical features, first aid measures, blood investigations done, bite to needle time, morbidity and mortality)
Morbidity parameters included duration of intensive care admission, total hospital stay, total days on ventilatory support and dialysis requirement
Snakebite characteristics (bite mark, site of bite and species of snake if identified)
ASV usage (time of administration, indication for use of ASV and number of vials of ASV used)
Blood products usage (fresh frozen plasma [FFP], platelets and packed red blood cells [PRBC])
Meteorological data (rainfall [daily, monthly, annually and heavy spells in 24 hours], temperature [daily, monthly, maximum and minimum and extreme values] and relative humidity [daily and monthly]).
Data analysisThe data were tabulated in Microsoft Excel using serial numbers in lieu of patient name. SPSS (International Business Machines Statistical Package for the Social Sciences, IBM Corp., Released 2013, Version 22.0. Armonk, NY, USA: IBM Corp) was used for the analysis of the data. Results on continuous measurements were presented as mean (standard deviation) and minimum– maximum. The results on categorical measurements were presented in number (%). Chi-square/Fisher’s exact test was used to find the significance of study parameters on categorical scale between two or more groups. Kruskal–Wallis test was used to test the association within categories of variables of different sample sizes. Kendall’s tau-b (τb) correlation coefficient was used to measure the strength of association of meteorological parameters with the number of snakebites (p<0.001).
RESULTSBetween January 2010 and January 2015, a total of 3229 individuals were registered with alleged history of snakebite to the institute. Six hundred and sixty-eight (20.7%) records met the inclusion criteria, but complete data were available only from 451 medical case records; 217 charts were either destroyed or there were no meaningful data available.
Demographics and clinical detailsAmong the 451 medical records that satisfied the inclusion and exclusion criteria reviewed, the victims were mostly males (300; 66.5%) with a male:female ratio of 2:1. Forty-five per cent (203/451) of victims were between 41 and 60 years of age, with a mean age of male patients being 41.6 years and that of female patients being 45.4 years.
Of the 451 records reviewed, bite to door time (time taken to reach first medical contact [FMC] following a bite) was available in 424 cases and 262 (58.1%) presented to the emergency department within 2 hours of the bite. The mean (SD) bite to door time was 2.50 (3.06) hours (median 2.5 hours; 95% confidence interval [CI] 2.21–2.79).
The most common presenting symptom was bite site tenderness, discolouration or swelling in 413 (91.6%) followed by limb oedema (71.2%), nausea and vomiting (25.9%) and tender lymphadenopathy (21.3%).
Among the neurotoxic signs, ptosis (12.2%) was the most common manifestation, followed by respiratory distress (8.6%), blurring of vision (7.8%), neck muscle weakness (5.5%) and ophthalmoplegia (2.9%).
The common acute complications noted were acute kidney injury (AKI) in 36.6% of cases, followed by cellulitis in 13.3% and respiratory failure in 4.4%. Of the 165 individuals who developed AKI, 37 (22.4%) required dialysis. Fourteen patients eventually (3%) required ventilator support.
The mean (SD) duration of ventilation was 2.6 (2.4) days (median 4; minimum–maximum 1–8 days; 95% CI 1.34–3.86). The mean (SD) duration of hospital admission was 10.5 (7.4) days (median 6; minimum–maximum 1–90 days; 95% CI 9.8–11.2) and the mean (SD) ICU stay was 5 (7.53) days (median 3; minimum– maximum 1–59 days; 95% CI 4.28–5.72).
Pearson’s correlation showed a strong correlation between need for dialysis with ICU stays (r=743, p<0.001) and with duration of hospital stay (r=713, p<0.001). The presence of AKI also correlated with ICU stay (r=616, p<0.001) and hospital stay (r=587, p<0.001).
Of all the records on snakebites registered in the institute (n=3229), 107/3229 (3.3%) snakebite cases resulted in mortality as per the medicolegal records data. Data sheets were available only for 51 cases, of which complete dataset for meaningful interpretation of results was available for 13 case records. Therefore, only 13 records of mortality could be included (13/451; 2.9%) in this study.
There was no correlation between the length of hospital stay against time delay in presentation or bite to ASV administration time or total ASV dose.
The mean (SD) bite to antivenom administration time was 3.18 (3.3) hours (median 2.25 hours; minimum–maximum 0.25–25 hours; 95% CI 2.87–3.49).
Time delay in presentation and needle time were categorized (<2 hours, 2–5 hours and >5 hours), and Kruskal–Wallis test performed showed no significant difference of length of stay among the categories.
Chi-square test performed revealed a significant association between the delay in presentation and the need for dialysis (p=0.013). A statistically significant difference was noted between clotting time (CT) at admission and need for dialysis (p<0.001) and mortality (p<0.001).
Kruskal–Wallis test showed that there was statistically significant difference of total length of stay (p<0.001) and ICU stay (p<0.001) among the categories of CT (normal or abnormal) at admission.
Snakebite characteristicsDefinitive bite marks were recorded in 404 (89.6%) patients with the lower extremity being the most common site (83.4%). Among the 451 cases, snake species was identified in 170 (37.7%). They were as follows: Russell’s viper 130 (76.5%); cobra 20 (11.8%); hump-nosed and other pit viper species 13 (7.6%); saw-scaled viper 4 (2.3%) and krait 3 (1.8%).
Among cobra bite victims, the mean (SD) hospital stay was 10.45 (14.5) days (minimum–maximum 1–67; median 6; 95% CI 4.095–16.805) and ICU stay was 5 (9.1) days (minimum–maximum 1–43; median 3; 95% CI 1.012–8.988). Six of the 20 (30%) cobra bites required ventilatory support and one required renal replacement therapy.
Russell’s viper bite had a total hospital stay of 7.76 (9.6) days (minimum–maximum 2–90; median 5; 95% CI 6.110–9.410) and ICU stay of 3.5 (3.7) days (minimum–maximum 1–34; median 3; 95% CI 2.864–4.136). Twenty-eight of the 130 (21.5%) Russell’s envenomation developed AKI and 4 required renal replacement therapy.
‘Pit viper’ had a total hospital stay duration of 9.2 (3.2) days (minimum–maximum 5–16; median 6; 95% CI 7.460–10.940) and ICU stay of 3.5 (1.7) days (minimum–maximum 1–7; median 3; 95% CI 2.576–4.424). Two developed renal injury but did not require dialysis.
Krait bite had a total hospital stay of 12.3 (9.3) days (minimum– maximum 7–23; median 7; 95% CI 1.776–22.824) and ICU stay of 7 (4.3) days (minimum–maximum 4–12; median 5; 95% CI 2.134– 11.866). All three krait bite victims required ventilatory support.
Saw-scaled viper bite led to hospitalization of 5.5 (0.58) days (median 5; 95% CI 4.932–6.068) and ICU stay of 2.25 (0.9) days (minimum–maximum 1–3; median 2.5 days; 95% CI 1.368–3.132). None of the saw-scaled and krait bite victims developed AKI.
Anti-snake venom useASV usage data were available in 424 records and 3920 vials of ASV were administered in 424 cases ranging from 2 to 36 vials.
The reason for administering ASV was noted as local signs in 184 (43.4%), haematotoxicity in 165 (38.9%), neurotoxicity in 34 (8.0%), systemic signs in 35 (8.3%) and mixed signs in 6 (1.4%) records.
Of the 451 cases, 213 (47.2%) required ASV within the first 2 hours of admission.
There was a statistically significant association between the total ASV used and need for dialysis (p=0.004), blood transfusion (p<0.001), total length of stay (p=0.046) and ICU stay (p<0.001).
Use of blood productsBlood products were used in 237 (52.5%) cases, of which FFP was used in 44.1%. Platelets alone were administered in 0.7% and PRBC alone in 2.2%; 3.8% (17/237) were administered a combination of FFP and platelets and 1.8% (8/237) required a combination of FFP, platelets and PRBC.
There was a statistically significant association of requiring dialysis and receiving blood products (p<0.001) though there was no significant correlation (r=0.041) between both of them.
There was a statistically significant difference among the categories of platelets administered and need for dialysis (p=0.014), total length of stay (p<0.001) and ICU stay (p<0.001).
Meteorological dataTwo hundred and forty-eight (55%) victims suffered from snakebites between the months of May and September when the average rainfall and humidity was high. There was a statistically significant correlation between number of snakebites with rainfall (τb=0.969, p<0.001) and humidity (τb=0.946, p<0.001).
DISCUSSIONSnakebite is a NTD.9 The burden of the disease is often underestimated. With the exception of a few studies, there has been little effort to quantify the magnitude of the problem in the state, let alone the country.4–6
Jubilee Mission Medical College and Research Institute situated in central Kerala, South India, is a missionary hospital where antivenom is provided free of cost, making it an ideal tertiary care referral institute for snakebite victims.
Describing the demographic profile, clinical features, pre-hospital care, geospatial distribution and treatment with the use of ASV and blood products itself might be the first step towards identifying the magnitude of this neglected disease.
Demographic dataAmong the victims of snakebite, the majority were males in the age group of 41–60 years. State statistics showed that in Thrissur district, 53.57% of the working class are of this peer group, and hence it is not surprising that they are victims of snakebite more commonly.10 Lower extremity was the most common bite site. Unlike other countries where people get bitten when handling snakes, in India the bites are mostly unprovoked. Whether community education, better footwear or interventions such as establishment of better snake rescue and release practices would aid in prevention of snakebite warrants further research.
Bite characteristicsDefinitive bite marks were seen in 89.6% of cases; 10.4% of snakebite cases presented without a bite mark but had signs of envenomation. The absence of bite mark might be an overestimate as it is possible that the bite mark was seen but not recorded in the case sheets. Snakes such as the Bungarus sp. (krait) are notorious to leave no fang marks.11 In addition, bites on thick soles and creases may be missed especially when there is no local pain or swelling.
Although fang marks may help in suspecting a snakebite, an absence of the same should not rule out a snakebite.
Pre-hospital careA tourniquet was applied as per the records of a majority (76%) of the victims. There were two patients with limb-threatening ischaemia noted in the victims of an Indian rock python (Python molurus) bite and in a banded kukri (Oligodon arnensis) bite, both non-venomous snakes, after a tight arterial tourniquet.
The two cases were administered two vials of antivenom each at the FMC before being referred to the snakebite centre.
The rural emergency department physician should record the presence of a tourniquet, especially if it is arterial. Application of herbal remedies such as turmeric, which is widespread in the region, is seldom mentioned in the case records. If intervention such as local incision, wound mutilation or local remedy application has been done, it should also be recorded since it might affect wound management. A prospective enquiry on the treatment sought and existing cultural practices may delineate the reasons for pre-hospital delay that occurs in the management of the bite victims.
The fact that the two aforementioned non-venomous snakes did not warrant antivenom administration highlights the need for assessing if the existing medical education in the region adequately prepares doctors to identify and treat snake envenomation victims using antivenom appropriately.12
Geospatial distribution of bitesPlotting bite locations on Google maps® revealed a higher incidence of bites in human settlements outside forest areas and particularly around paddy fields and local plantations (Fig. 1). In 60% of the individuals, the bite occurred more than 20 km away from their FMC, yet 58% reached within 2 hours of bite.

FIG 1.: Geospatial distribution plot of snakebites: (a) location plot: Green marker: Snakebite treatment centre location, Red Marker: Place of bite recorded; (b) overlaid terrain plot; (c) regional distribution of bites; (d) approximate drainage area
Export to PPT
In this review, we could find no correlation between the length of hospital stay against time delay in presentation or bite to ASV administration time. This could be because most victims arrived early and were administered antivenom.
We would be tempted to interpret that the timing of ASV does not matter in this retrospective review. It is to be kept in mind that this was a unique setting where there was a minimal delay in presentation to the hospital. On the other hand, there was a significant association between time delay in presentation and the need of dialysis and CT at admission. This could mean the more severe the envenomation, the worse the coagulopathy at admission, the worse the prognosis. The delayed the presentation, the higher is the risk of morbidity in terms of renal injury.
Region-specific, prospective snakebite mapping could be a cost-effective strategy that might not only help in vulnerability analysis of the region but also in varied other endeavours such as scientific snake rescue and release, efficient antivenom dispersal, improved ambulance dispatch and public education.
Meteorological dataA majority of snakebites occurred during the monsoon seasons. In Kerala, the monsoon season is divided into Southwest (June to September) and Northeast Monsoon (October to November).13 A peak in snakebite envenomation was found to be in the initial months of Southwest Monsoon (Fig. 2).
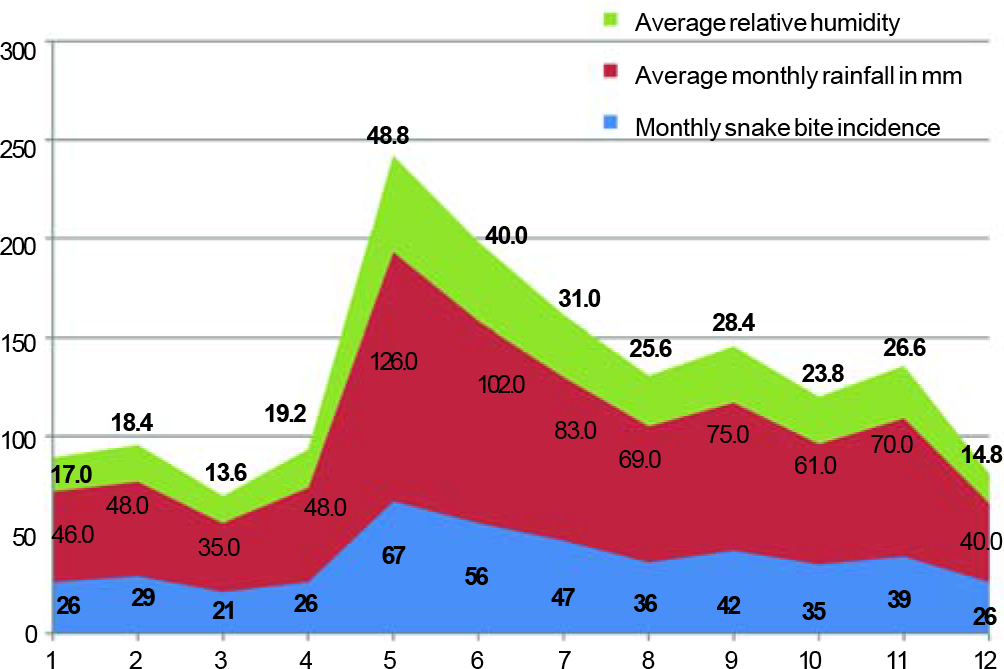
FIG 2.: Stacked plot of rainfall, humidity and snakebite recorded cumulative monthly rainfall in mm, humidity %, snakebite in numbers plotted against the months of the year. X axis: months of the year
Export to PPT
There was a statistically significant increase in the number of bite with rainfall and humidity in the region (Fig. 3). Although it was noted that the number of bites were the most in May when the average daily temperature recorded was the highest, no statistically significant association was found between the number of snakebites and the maximum and minimum daily temperature of the months of the year.
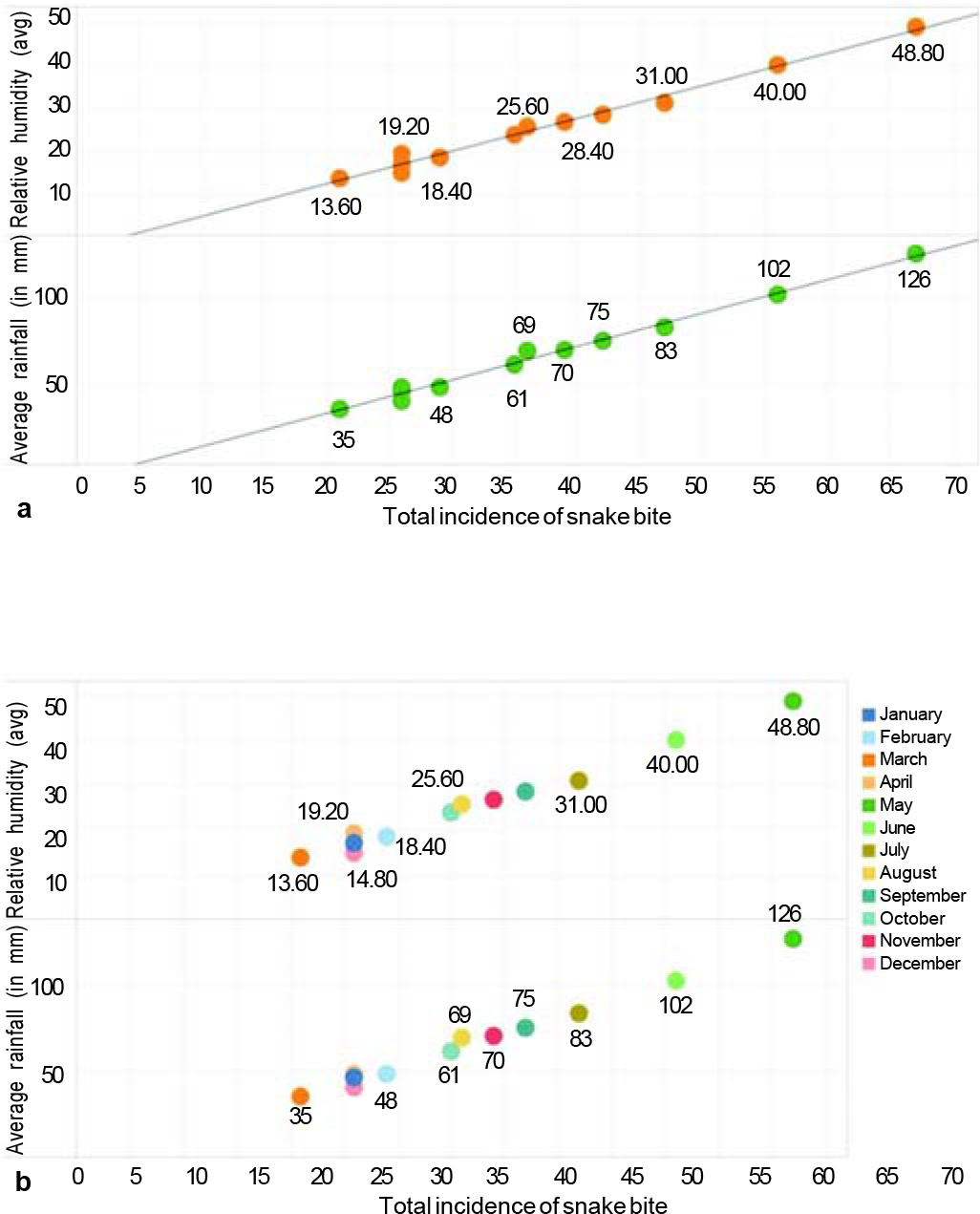
FIG 3.: (a) Incidence of snakebite against average rainfall and humidity (b). and its association in the respective months of the year. Total incidence of snakebite plotted shows an increase when plotted against average rainfall and humidity (a), and also shows an association between the two in the respective months of the year (b)
Export to PPT
Many hypotheses exist as to why the bites increase during the rainy season, ranging from the flooding of the holes, increase in prey during these months and to its association with mating season. Whether the snakes have a humidity forewarning system of the impending climatic change is not known.
Like studies done elsewhere, the meteorological parameters and their association with snakebite need to be explored more extensively and should be included in a prospective registry to get a more accurate picture in this region too.14,15 This information may prove helpful in advising protective clothing for workers when temperatures and humidity exceed certain thresholds.
Temporal dataBites predominantly occurred between 6 p.m. and 6 a.m. (50.7%) though the average surface visibility during the entire study period at 8.30 a.m. and 5.30 p.m. was the same. This dataset can be a bit misleading since meteorological visibility refers to transparency of air: in the dark, meteorological visibility is still the same as in daylight for the same air.
In a prospective registry, questionnaire with regard to the locality details where the bite happened, such as the presence or absence of streetlights or use of portable light sources, may help us in better determining the public intervention to reduce snakebites in the evening.
Antivenom usePolyvalent ASV is the only effective and specific treatment which is available to neutralize the venom of Russell’s viper (Daboia russelii), bispectacled cobra (Naja naja), saw-scaled viper (Echis carinatus) and common krait (Bungarus caeruleus) envenomation in India.8 This therapy is not always available for snakebite cases due to its high cost.16
In this study, an average of 9.2 vials of antivenom were used to treat an individual, with 36 vials being the maximum dose given. In 13 patients who received antivenom, the snake was recorded as a ‘pit viper’. Coagulopathy persisted in all 13 after administration of antivenom.
These data indirectly speak to the multitude of antivenom administration practices existing in the region.17–21 Some physicians advocate low-dose antivenom combined with blood products, whereas some advocate various standard doses of antivenom.17,18,22
Even though guidelines mention paraspecific neutralization of antivenom, we do not have robust data on the degree of neutralization of other species, let alone a genus like Hypnale or Trimeresurus.8,23 Persistent coagulopathy in the ‘pit viper’ bites could mean that there is no effect for the current antivenom for the same.
Clinical featuresLocal signs and symptoms happened to be the earliest trigger for using antivenom. The victims had an average bite to needle time of 120 minutes; 47.2% of cases received the first dose of antivenom in the first 2 hours post-bite.
The admission CT if abnormal was a marker for poor prognosis of morbidity in terms of duration of hospital stay, need for intensive care and requirement for dialysis.
Since Viperidae inflicted the majority of the envenomation in this region, haematotoxicity and renal failure should be the complications anticipated.6 Among the blood parameters studied, platelet count at admission was shown to correlate well with morbidity.5 None of the other blood parameters recommended were done routinely and hence no inference can be drawn on their utility to predict outcome.
Blood product usagePersistent coagulopathy post-antivenom treatment is often managed with blood products.24
In our study, 52.5% of cases were administered blood product transfusions, with FFP being the most common component used.
Utility of blood products in victims of envenomation is debatable.25 FFP has been shown to normalize coagulopathy earlier in certain snakebite victims.26 In Russell’s viper victims, it has been shown to normalize coagulopathy although its ability to confer clinical benefit is controversial.22,27
Whether addition of extra ‘substrate’ in the form of FFP makes things worse or if it aids in early normalization of patients physiology needs to be evaluated.28
LimitationsThis chart review has its limitations in its retrospective design. The information collected was from 668 patients over 5 years, with a rejection rate of 32.5% due to insufficient information and missing data from the total chart pool. A majority of mortality records were not available (88%; 94/107), rendering us incapable of doing reliable mortality data correlations. Poor keeping of medical records leads to a selection bias, which was beyond our control.
These factors highlight the existing deficit in data collection and further advocate the need for the establishment of a prospective registry to quantify this NTD in low-resource settings.
Although there was a training session for data abstractor and cross-verification was ensured by a records supervisor, it is likely that the retrospective aspect may have resulted in information bias or misclassification.
Another major pitfall in the design was in the inclusion criteria. We may have missed a lot of ‘dry bites’ with no symptoms. A dry bite is when a venomous snake bites, but does not inject the venom into the victim. This may not be relevant in the context of establishment of a registry, but it could underestimate the burden of the disease.
External validity of this study is questionable. Records of individuals <18 years of age were not included in this study. Although initially the study was designed to incorporate paediatric cases too, in our setting, a practice of procuring assent for paediatric case records was not in place during the period the case records were reviewed. Hence, the paediatric data were later avoided to comply with the ethical committee norms of the institute.
Well connected by roads, this institute is unique, with regard to accessibility, which might not be the case elsewhere in the country. This might explain the lack of correlation between the length of hospital stay against time delay in presentation or bite to administration time of ASV. A multicentric prospective snakebite registry, which we intent to establish would give a more generalizable picture for the region.
Factors such as the educational status, community awareness, cultural practices, logistic hurdles, socioeconomic status, financial burden of the individual or even individual blood parameters could not be studied in this design.
ConclusionSnakebite is a disease of the poor, and hospitals treating these individuals are often resource-constrained. The study highlights that even though we had a large number of cases, we did not have a data capturing system to give us the actual picture. We need to establish a cost-effective data collection process.
There is a need to establish a prospective comprehensive snakebite registry encompassing not just the clinicoepidemiological characteristics of snakebite victims but also the demographic data, the time factors affecting treatment, the pre-hospital care and practices, ASV, blood product usage, geospatial distribution and meteorological data.
Establishing a multicentric region-specific registry would be the first step towards quantifying the burden of this NTD.
留言 (0)