In early 2020, Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2), also known as COVID-19, was classified as a pandemic by the World Health Organization.1,2 This novel coronavirus can spread from person to person, presents on mucosal surfaces of the digestive tract and in saliva and may cause serious complications.3 Dental professionals are thought to be at increased risk because of aerosol generation during many dental procedures, patient proximity and the dental operating environment.3,4
As part of Canada’s public health response to COVID-19, the provision of dental services was limited to emergent and essential services with the intent to minimize the risk of viral transmission in dental settings during phase 1 of the pandemic.5-7 Oral health plays an integral role in general health.8 True dental emergencies, such as uncontrolled bleeding, severe pain, life-threatening infections of odontogenic origin and orofacial trauma, threaten overall health and patients’ quality of life.8-10 Essential dental care differs from emergent care and relates to the treatment of conditions that require immediate attention to relieve pain or minimize the risk of infection.5 In medically complex patient cohorts, such as oncology and other hospital-based patients, essential dental needs can quickly escalate into emergent issues.11 Therefore, treatment planning and delivery may differ in these settings compared with community-based dental clinics, even during a period of limited community dental treatment.11
True dental emergencies that cannot be resolved via pharmacotherapy or teledentistry require procedural intervention.12 Several recent papers3,12-16 have described an overall reduction in dental emergencies seen during the early pandemic period compared with pre-pandemic periods, but those seen were predominantly odontogenic pain and infection related to pulpal/periapical pathology requiring endodontic or oral surgery interventions. In a sample of over 1500 patients seen during the early pandemic period in England, 63.4% had a diagnosis of symptomatic irreversible pulpitis or apical pathology requiring in-person care, and 50% of patients had their chief complaint resolved with a simple extraction.12 Similar findings were reported in another study investigating dental emergency patterns in 5 hospital departments in England; researchers noted that 83% of these patients were not appropriate for remote consultation and required in-person clinical examination.3 Although many patients avoided hospital settings during the early pandemic period, the proportion of patients admitted to hospital for odontogenic infection rose from 35% to 80%, with a noted increase in severity of orofacial infection.15
Essential dental care forms a significant component of hospital-based dental care. For example, patients undergoing immunosuppression related to solid-organ transplantation, chemotherapy or other reasons are more susceptible to oral infections and their sequelae, including sepsis and death.17,18 Dentistry plays an important role in the management of these patients, as pre-existing oral disease may lead to orofacial infection and, thus, compromise the long-term success of medical therapies.17,18 The goal of dental treatment is to eliminate odontogenic sources of infection and manage oral diseases so that the risk of oral health complications during medical therapy is minimized.17,19 Dental consultation, treatment planning and procedural intervention for medically complex patients is, thus, considered essential dental care.17
Several authors have recommended that the dental profession prepare resources and its workforce for potential future waves of COVID-19 or other pandemics and potential limitations on dental practice.3,15 A preplanned pathway for managing dental emergencies alleviates pressure on emergency services and hospital-based dental services.15 Therefore, this study was designed to describe the types of in-person dental visits occurring during the earliest period of the COVID-19 pandemic and their frequency in academic and hospital-based settings affiliated with the University of British Columbia (UBC) faculty of dentistry. The secondary objective was to compare dental services provided across different academic and hospital-based settings, each of which serves unique patient cohorts. The aim was to amass descriptive data that would help with planning for dental workforce allocation in the potential event of future limitations secondary to COVID-19 or another pandemic.
Materials and MethodsIn British Columbia (BC), Canada, provincial public health bodies took a measured, multi-phase approach in response to the COVID-19 pandemic in early 2020. This approach took place in 4 phases, as described by the Government of British Columbia in collaboration with the BC Ministry of Health.5-7 Phase 1, covered approximately 2 months, 16 March–18 May 2020. During this period, protective measures included declaration of a public health emergency and a provincial state of emergency, postponement of non-urgent surgeries, mandated physical distancing, hand hygiene and cleaning guidelines and other public health measures intended to curtail transmission.5-7 During phase 1 restrictions, the provincial dental college mandated that all elective and non-essential dental services be suspended. In response, community practices, academic institutions and hospital-based dental services significantly curtailed their clinical activities, limiting in-person care.
During phase 1, a limited number of clinics affiliated with UBC’s faculty of dentistry continued to provide emergent and essential dental services, including the UBC Oral Health Centre (OHC), the BC Cancer Agency Department of Oral Oncology (BCCA) and BC Children’s Hospital Department of Dentistry (BCCH). These university and hospital-based clinics have specific mandates and serve unique patient populations. The OHC’s COVID-19 emergency clinic provided clinical services to existing patients of the faculty’s undergraduate and graduate programs. The BCCA provided clinical services at 2 sites to oncology patients with oral health care needs. The BCCH provided clinical services to pediatric patients requiring a hospital setting for the safe provision of dental care.
Data were collected from electronic health records (EHRs) on all in-person dental visits from 16 March to 18 May 2020. Different EHR systems were accessed at each clinical site, including AxiUm (Exan Software, Coquitlam, BC), ClearDent (Burnaby, BC) and the Cancer Agency Information System (CAIS). Information on teledentistry and triage dental consultations via video conferencing during this period was not collected. Data included date of visit, patient demographic information, including age and gender, patient medical comorbidities, reason for the dental visit, treatment rendered during phase 1 restrictions, follow-up appointments and whether emergency treatment was related to incomplete treatment. All patient identifiers were removed. Data were presented using descriptive statistics.
This study was approved by the UBC Behavioural Research Ethics Board and the BC Children’s and Women’s Hospital Research Ethics Board (UBC BREB number: H20-01441).
ResultsDuring phase 1, 396 patients were seen at the 3 academic or hospital-based settings: 263 at the BCCA, 58 at BCCH and 75 at the OHC COVID-19 emergency clinic (Table 1). The average age of patients was 62 years at BCCA, 7.5 years at BCCH and 48 years at OHC (Table 1).
Table 1: Demographic Information for patients seen at 3 dental clinics in British Columbia (BC) during phase 1 of the COVID-19 pandemic.Patient parameter
Clinical site
BCCA
BCCH
OCH
Note: BCCA = BC Cancer Agency Department of Oral Oncology, BCCH = BC Children’s Hospital Department of Dentistry, OHC = UBC Oral Health Centre COVID-19 emergency clinic, SD = standard deviation.
*Behavioural comorbidity includes autism spectrum disorder, attention deficit and hyperactivity disorders, anxiety, developmental delay and others.
†Medical comorbidity includes genetic syndromes, rare diseases, coagulation disorders and others.
‡New medical diagnosis where a physician was requesting dental clearance primarily includes pediatric oncology diagnoses and relapses.
Different patient cohorts are served at these 3 clinical sites and this is reflected in medical comorbidity information (Table 1). At the BCCA, most patients requiring in-person dental consultation or treatment were seen before (27%) or after (22%) head and neck radiation therapy; 15% were seen before bone marrow or stem-cell transplantation and 13% were currently on or imminently starting chemotherapy. In this cohort, the most frequent reason for an in-person dental visit was an essential consultation (i.e., dental clearance) related to their oncology treatment (Figure 1). Less frequent reasons for in-person dental visits included severe pain, prosthodontic emergencies, morbidity related to osteoradionecrosis and odontogenic infection. The most common treatment provided was consultation followed by much lower numbers of oral surgical and prosthodontic procedures (Figure 2). Care was provided in an outpatient ambulatory setting following enhanced infection prevention and control guidelines specific to COVID-19 published by the provincial dental college.5
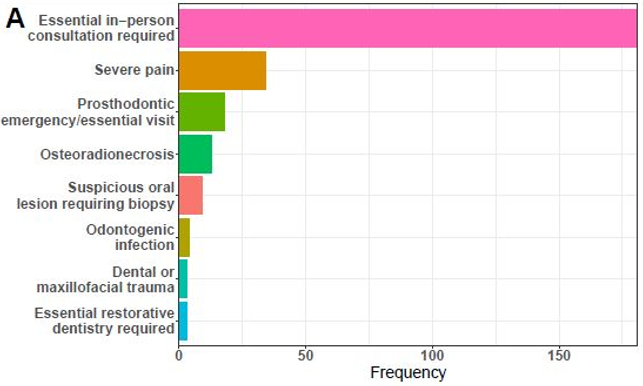
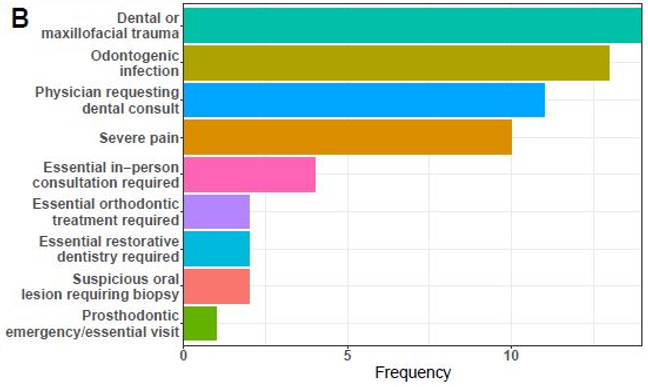
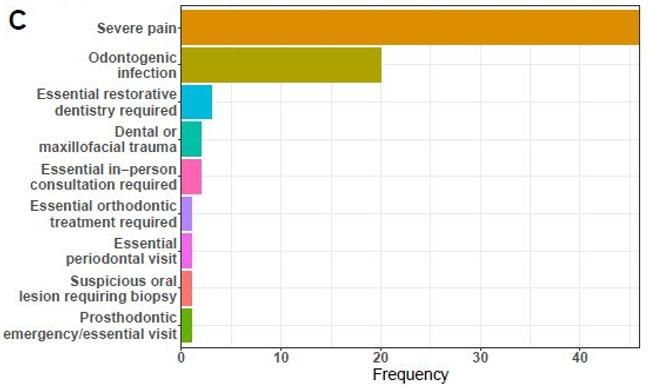
Figure 1: Reasons for in-person dental visits at A.) BC Cancer Agency Department of Oral Oncology, B.) BC Children’s Hospital Department of Dentistry and C.) UBC Oral Health Centre COVID-19 emergency clinic during phase 1 of COVID-19 restrictions.
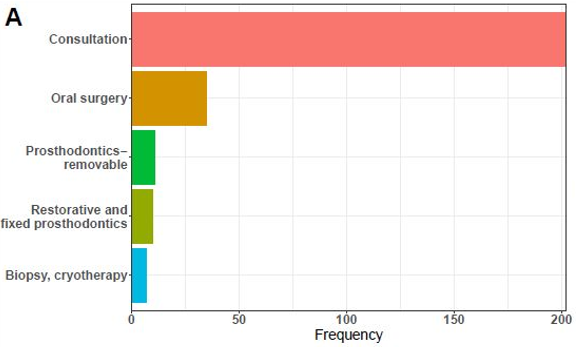
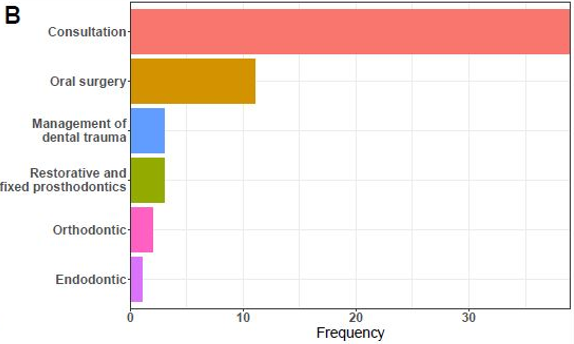
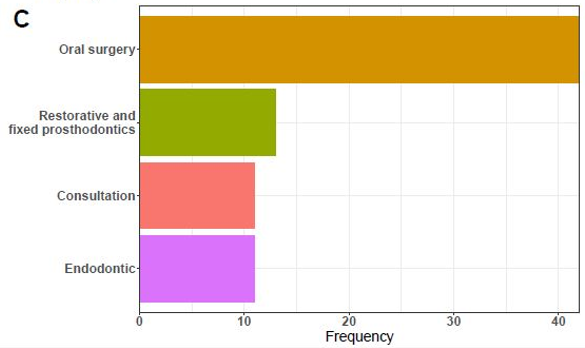
Figure 2: Dental procedures performed at A.) BC Cancer Agency Department of Oral Oncology, B.) BC Children’s Hospital Department of Dentistry and C.) UBC Oral Health Centre COVID-19 emergency clinic during phase 1 of COVID-19 restrictions.
At BCCH, 24% of pediatric patients requiring an in-person visit had a pre-existing diagnosis of behavioural disorder (e.g., autism spectrum disorder, anxiety disorder, developmental delay, attention deficit/hyperactivity disorder). Many (35%) had a significant medical comorbidity (e.g., bleeding disorder, genetic syndrome, rare disease) requiring a hospital setting for the safe provision of their dental care. Some (10%) had a new medical diagnosis, where the physician had recently requested dental clearance for a subsequent medical procedure. This group included pediatric patients with new oncology diagnoses or relapses, severe renal disease and others. Reasons for in-person dental visits and procedures differed from those at other clinical sites: the most common reason was oral/maxillofacial trauma, followed by odontogenic infection, physician request for dental clearance before medical procedures and severe odontogenic pain (Figure 1). The most frequent treatment was consultation, followed by oral surgical procedures, management of dental trauma and restorative treatments (Figure 2). Care was provided in an outpatient ambulatory setting, inpatient wards, emergency room and under general anesthesia in an operating room setting.
At the OHC COVID-19 emergency clinic, most patients seen were physically healthy. However, significant data are missing for this cohort. At this site, the most frequent reason for a dental visit was severe odontogenic pain, followed by odontogenic infection (Figure 1). The procedure provided most often was oral surgery (predominantly dental extractions), followed by dental restorations, consultations and endodontic procedures (Figure 2). Care was provided in an outpatient ambulatory setting.
DiscussionDuring the initial phase of COVID-19 restrictions in BC, emergent and essential dental care was provided out of multiple sites affiliated with the UBC faculty of dentistry. Differences were noted in the reasons for in-person dental visits and procedures performed between clinical sites and can be explained by different patient populations at these sites.
The BCCA provided emergent and essential consultation and treatment to oncology patients undergoing bone marrow transplant/stem-cell transplant, head and neck radiation including management of osteoradionecrosis, bone-modifying agents, head and neck surgery or reconstruction and chemotherapy. The types of treatment provided included predominantly consultation and oral surgical interventions, with relatively low numbers of prosthodontic and restorative services. This dental service is a tertiary level care setting and patients are typically seen after referral from a radiation oncologist, medical oncologist or head and neck surgeon. Attending staff operating in this clinic during the data collection period included oral surgeons, maxillofacial prosthodontists, general dentists and oral medicine specialists. Even during a pandemic, members of the cancer care team aim to minimize disruption and delay of medical treatment (i.e., radiation therapy, chemotherapy, etc.) and dental service is an essential component of this interdisciplinary team, as reflected by our data.
The BCCH provided essential and emergent care to pediatric patients, including timely dental clearance for medical procedures, management of pediatric maxillofacial trauma, orofacial infections and fixed orthodontic appliance removal for urgent medical procedures. Treatment provided was predominantly consultation and oral surgical interventions, with relatively fewer endodontic and restorative services. This hospital dental service is part of a tertiary care pediatric hospital, and patients seen were referred through the hospital emergency department, a pediatrician/family physician or another provider. Attending staff operating in this service during the data collection period were pediatric dentists and oral surgeons.
The OHC COVID-19 emergency clinic provided emergent care to existing patients of the faculty of dentistry and a limited number of patients from the community who were unable to access dental services because of widespread closure of community-based private practices. Most patients presented with uncontrolled pain and orofacial infection. The predominant procedures provided were oral surgery related (i.e., dental extractions) and fewer endodontic and restorative procedures. Attending staff operating in this clinic were full-time faculty members, including oral surgeons, periodontists, prosthodontists, general dentists and endodontists. Results from the OHC clinic are similar to data reported from a recent study from England, where 67% of in-person dental emergencies were extractions.14 Furthermore, the principles for operating a dental service during a pandemic described by these authors, such as the need for deferral of non-emergency patients, identification of true dental emergencies, engineering and administrative controls, reduced interpersonal interactions, conservation of personal protective equipment, prevention of unplanned admissions and staff well-being were identical to those adopted at our clinics in Vancouver.14
During phase 1, almost all community dental practices across BC were closed following guidance from the provincial dental college.5 Patients of record at these community clinics may have had to attend university-based emergency clinics and hospital-based dental departments on an emergent basis, as their regular dentist was not available. Despite the practice closures, community-based dentists are responsible for the essential and emergent dental needs of patients, and these services should be provided via teledentistry when possible.5 Furthermore, community-based dentists should be available to provide information to university-affiliated and hospital-based dentists who may have to provide essential or emergent dental care to their patients.
The experience of the 3 UBC-affiliated clinical sites in this study with regard to COVID-19 nosocomial infection of attending and auxiliary dental staff was similar to that reported from Wuhan University: there were no reported cases during phase 1.2 In the Wuhan study, over 700 patients were treated at the dental school and university-affiliated hospital in the early phase of their pandemic with no COVID-19 nosocomial infections reported among students or staff during that time.2 In our study, no COVID-19 nosocomial infections were reported at the three UBC-affiliated clinics among attending and auxiliary staff during phase 1. This supports the notion that appropriate personal protective equipment, in addition to administrative and engineering controls, is effective.2,4 Examples of administrative and engineering controls employed in the UBC-affiliated clinics include rigorous patient triage, installation of plexiglass barriers in reception areas, significantly reduced patient volume and improved air circulation within operatories.4 Restorative procedures were modified to limit aerosol generation, when possible, and the use of atraumatic restorative techniques, silver diamine fluoride and selective caries removal were selectively employed.20
ConclusionThis descriptive study presents data from dental patients seen during phase 1 of the COVID-19 pandemic in university and hospital-based settings affiliated with the UBC faculty of dentistry. Each clinical site serves a unique patient cohort and the reasons for in-person dental visits and procedures performed differed between sites. At the BCCA, in-person dental visits were mainly for consultations needed by patients related to their oncology treatments. At the BCCH, the most frequent reasons for in-person dental visits were maxillofacial trauma, odontogenic infection, physician request for dental clearance before medical procedures and severe odontogenic pain. At the OHC, the most common reasons were severe odontogenic pain and odontogenic infections. The treatments provided most frequently across all sites were consultations and oral surgical procedures.
THE AUTHORS

Dr. Tong is the program director of the University of British Columbia (UBC) general practice residency program and an assistant professor of teaching in the UBC faculty of dentistry, Vancouver, BC.

Dr. Park is the chief of dentistry at the British Columbia Children’s Hospital and a clinical assistant professor in the Division of Pediatric Dentistry at the UBC faculty of dentistry, Vancouver, BC.

Dr. Carlisle is the regional professional practice leader at the British Columbia Cancer Agency Department of Oral Oncology (Surrey) and a clinical assistant professor at the UBC faculty of dentistry, Vancouver, BC.

Dr. Poh is a professor and acting program director for the oral medicine and oral pathology residency program at the UBC faculty of dentistry, Vancouver, BC; and senior scientist and consulting clinician with the BC Cancer Agency Department of Oral Oncology (Vancouver).
Acknowledgements: The authors thank Drs. Suraj Chavda, Abdullah Alawady and Nicholas Thomas (UBC general practice residents) for their assistance in data collection and Dr. Andrea Esteves for access to UBC Oral Health Centre data. We thank Dr. Chris Wyatt for minor editing and revisions.
Corresponding author: Dr. Nicholas Tong, Faculty of Dentistry, University of British Columbia, 374—2199 Wesbrook Mall, Vancouver BC V6T 1Z3. Email: nicholas.tong@dentistry.ubc.ca
The authors have no declared financial interests.
This article has been peer reviewed.
References World Health Organization. Timeline: WHO’s COCID-19 response. Geneva: World Health Organization: 2020. Available: www.who.int/emergencies/diseases/novel-coronavirus-2019/interactive-timeline (accessed 2021 June 12). Meng L, Hua F, Bian Z. Coronavirus disease 2019 (COVID-19): emerging and future challenges for dental and oral medicine. J Dent Res. 2020;99(5):481‐7. Blackhall KK, Downie IP, Ramchandani P, Kusanale A, Walsh S, Srinivasan B, et al. Provision of emergency maxillofacial service during the COVID-19 pandemic: a collaborative five centre UK study. Br J Oral Maxillofac Surg. 2020;58(6):698-703. Izzetti R, Nisi M, Gabriele M, Graziani F. COVID-19 transmission in dental practice: brief review of preventive measures in Italy. J Dent Res. 2020;99(9):1030-8. Oral health care during phases 2 and 3 fo the COVID-19 response. Vancouver: College of Dental Surgeons of British Columbia; updated 2020 Aug. 18. Available: https://www.cdsbc.org/Documents/covid-19/COVID-19-oral-healthcare-Aug18.pdf (accessed 2021 June 12). Coronavirus disease (COVID-19). Ottawa: Government of Canada; 2020. Available: https://www.canada.ca/en/public-health/services/diseases/coronavirus-disease-covid-19.html (accessed 2021 June 12). Phase I — BC’s restart plan. Victoria: British Columbia Ministry of Health; 2020. Available: https://www2.gov.bc.ca/gov/content/safety/emergency-preparedness-response-recovery/covid-19-provincial-support/phase-1 (accessed December 21, 2021). Zhang W, Wu YY, Wu B. Does oral health predict functional status in late life? Findings from a national sample. J Aging Health. 2018;30(6):924-44. Kassebaum NJ, Bernabé E, Dahiya M, Bhandari B, Murray CJL, Marcenes W. Global burden of untreated caries: a systematic review and metaregression. J Dent Res. 2015;94(5):650-8. Friedman PK, Kaufman LB, Karpas SL. Oral health disparity in older adults: dental decay and tooth loss. Dent Clin North Am. 2014;58(4):757-70. Hong CHL, Hu S, Haverman T, Stokman M, Napeñas JJ, Bos-den Braber J, et al. A systematic review of dental disease management in cancer patients. Support Care Cancer. 2018;26(1):155‐74. Grossman S, Sandhu P, Sproat C, Patel V. Provision of dental services at a single institution in the UK’s epicenter during the COVID-19 pandemic. Br Dent J. 2020;228(12):964-70. Guo H, Zhou Y, Liu X, Tan J. The impact of the COVID-19 epidemic on the utilization of emergency dental services. J Dent Sci. 2020;15(4):564-7. Shah A, Bryant C, Patel J, Tagar H, Akintola D, Obisesan O. COVID-19: establishing an oral surgery-led urgent dental care hub. Br Dent J. 2020;228(12):957-63. Long L, Corsar K. The COVID-19 effect: number of patients presenting to the Mid Yorkshire Hospitals OMFS team with dental infections before and during the COVID-19 outbreak. Br J Oral Maxillofac Surg. 2020;58(6):713-4. Yu J, Zhang T, Zhao D, Haapasalo M, Shen Y. Characteristics of endodontic emergencies during coronavirus disease 2019 outbreak in Wuhan. J Endod. 2020;46(6):730-5. Glassman P, Wong C, Gish R. A review of liver transplantation for the dentist and guidelines for dental management. Spec Care Dentist. 1993;13(2):74-80 1.8 Patients receiving bone marrow transplantation. In Oral & dental care. Vancouver: BC Cancer Agency; 2003. Available: http://www.bccancer.bc.ca/health-professionals/clinical-resources/cancer-management-guidelines/head-neck/oral-dental-care#receiving-bone-marrow (accessed 2021 June 12). Schmalz G, Berisha L, Wendorff H, Widmer F, Marcinkowski A, Teschler H, et al. Association of time under immunosuppression and different immunosuppressive medication on periodontal parameters and selected bacteria of patients after solid organ transplantation. Med Oral Patol Oral Cir Bucal. 2018;23(3):e326-34. Mallineni SK, Innes NP, Raggio DP, Araujo MP, Robertson MD, Jayaraman J. Coronavirus disease (COVID-19): characteristics in children and considerations for dentists providing their care. Int J Paediatr Dent. 2020;30(3):245-50.
留言 (0)