Chronic abdominal pain is currently a challenging clinical problem in modern society. The term “chronic pain” is defined as persistent or recurrent pain lasting 3 months or longer (1, 2). Some studies (3, 4) have demonstrated that abdominal pain represents the most prevalent gastrointestinal symptom observed in clinical practice, with a prevalence rate ranging from 22 to 25%. Abdominal pain, as a symptomatic complaint can be caused by a number of disorders, including both gastrointestinal and extra-intestinal conditions that involve the genitourinary tract, abdominal wall, thorax, and spine. On the other side of the spectrum, it may be caused by organic diseases (Crohn’s disease, intestinal obstruction, chronic appendicitis, chronic pancreatitis, etc.) or functional disorders (functional dyspepsia, irritable bowel syndrome, and centrally mediated abdominal pain syndrome, etc.) (1). The complexity of these conditions necessitates a wide range of differential diagnostic tests and examinations. In some cases, despite extensive and costly investigations, the underlying cause of the abdominal pain may remain undetermined, placing a significant strain on healthcare systems worldwide.
Since its clinical introduction in the early 21st century, SBCE has proven valuable in diagnosing and managing small bowel-related conditions, including unexplained gastrointestinal bleeding, Crohn’s disease, and small bowel tumors (5). However, the effectiveness of this test in patients whose primary complaint is chronic abdominal pain remains a subject of debate. Generally, SBCE is not recommended as a first-line diagnostic tool for patients experiencing chronic abdominal pain. Bardan et al. (6) and Fry et al. (7) concluded that SBCE has no significant clinical value in the diagnosis of patients with chronic abdominal pain, but, May et al. (8) concluded that SBCE has a role in patients with chronic abdominal pain who have some additional symptoms or signs. Therefore, the aim of our study was to determine the factors affecting the efficacy of SBCE examination, thus enhancing the utilization of the capsule in patients with chronic abdominal pain, as well as reducing the waste of healthcare resources.
Methods Patients and study designWe retrospectively included 524 patients who underwent SBCE at our institution from January 2014 to January 2023, all presenting with chronic abdominal pain as their chief complaint. None of these patients exhibited lesions that could explain their symptoms during routine clinical examinations and laboratory tests, which included blood tests, urinalysis, fecal tests, ultrasonography, computed tomography imaging, esophagogastroduodenoscopy, and colonoscopy. We collected demographic characteristics of the patients, including their names, genders, ages, heights, weights, underlying diseases, and specific details from the SBCE examinations, such as hemoglobin levels and inflammatory markers (white blood cell count, platelet count, C-reactive protein, erythrocyte sedimentation rate, and calcitoninogen). The study received approval from the Institutional Review Board of Renji Hospital.
In our study, chronic abdominal pain was defined as recurrent or persistent abdominal pain lasting more than 3 months. Anemia was defined as a hemoglobin level of less than 90 g/L. Small bowel lesions were categorized as clinically significant or not. Clinically significant lesions included mucosal breakdowns such as erosions, ulcers, strictures, or tumors. Lesions that were not considered clinically significant included arteriovenous malformations, red spots, and erythema, etc., and it is possible that these lesions did not account for the patients’ symptoms. The lesion detection rate was defined as the percentage of patients with positive small bowel lesions relative to the total number of patients examined. Delayed upper gastrointestinal transit (DUGT) was defined as the inability of a capsule to pass through the pylorus within 1 h.
After signing the informed consent form for the SBCE examination, all patients received the PillCam SB2/3. They were instructed to fast for 12 h prior to the examination and to adequately prepare their bowels. Approximately 2–3 h after swallowing the capsule, patients were permitted to consume clear liquids and resume their daily activities. At the conclusion of the examination, patients returned the recording system, and the physician downloaded the video images into a computerized system for analysis by a specialized endoscopist. For patients exhibiting signs of delayed transit, conservative treatment or endoscopic intervention to facilitate passage to the duodenum was chosen based on clinical experience.
Statistical analysisStatistical analysis was conducted using SPSS version 26.0. Count data were expressed as % and were compared using the χ2 test. Factors associated with DUGT were identified through logistic regression analysis. Odds ratios (OR) and their corresponding 95% confidence intervals (CI) were calculated. A p-value of less than 0.05 was considered statistically significant.
Results Demographical and clinical characteristicsA total of 524 patients with chronic abdominal pain underwent SBCE, 345 males and 179 females, with a median age of 45 years. Of the cases examined, 113 were delayed, and all patients received conservative, pharmacologic, or endoscopic interventions (Table 1). A total of 509 patients completed the examination, resulting in an examination completion rate of 97.1%.
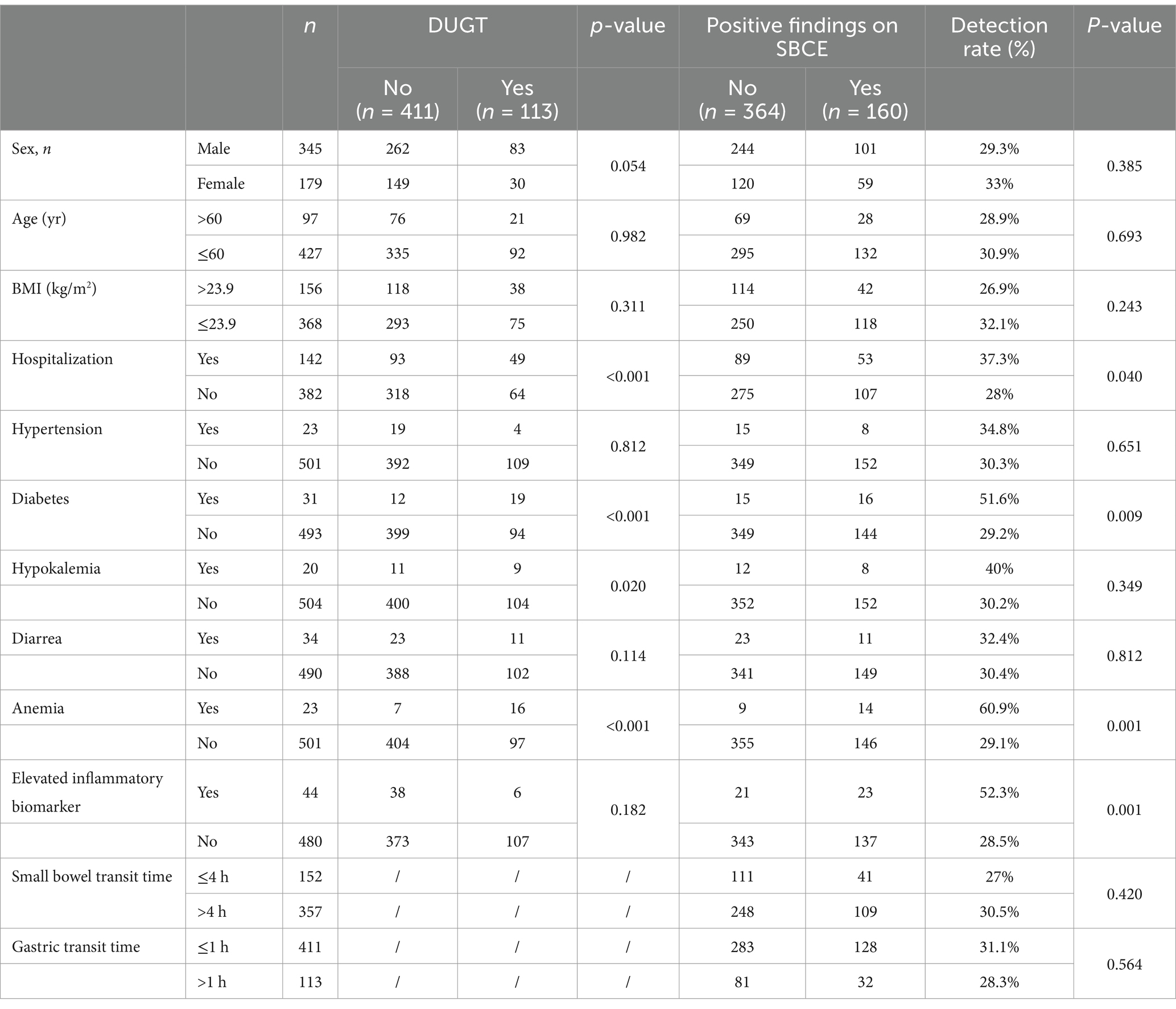
Table 1. Univariate analysis of factors influencing the findings and DUGT of SBCE.
Risk factors for DUGTUnivariate analysis revealed that hospitalization status, diabetes, hypokalemia, and anemia were significantly associated with DUGT in patients presenting with chronic abdominal pain (Table 1). Further multivariate regression analysis indicated a significant association between hospitalization status (OR 1.686, 95% CI: 1.011–2.809, p = 0.045), diabetes (OR 3.463, 95% CI: 1.384–8.666, p = 0.008), and anemia (OR 4.916, 95% CI: 1.798–13.444, p = 0.002) as risk factors for DUGT (Table 2).
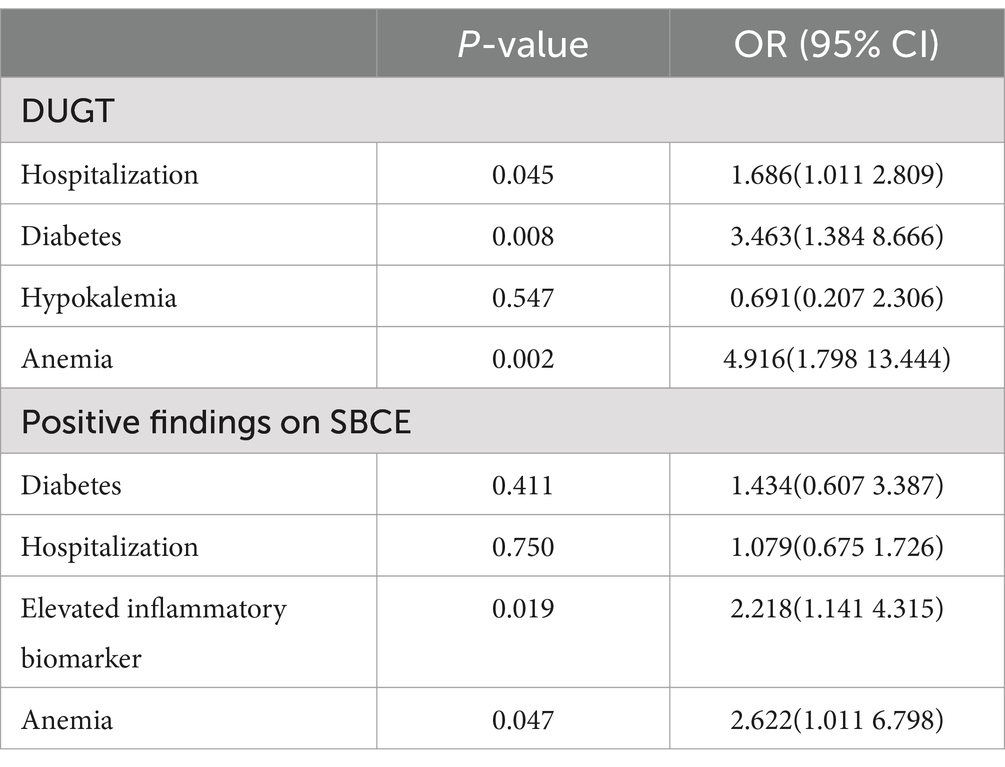
Table 2. Multivariate analysis of factors influencing the findings and DUGT of SBCE.
Factors influencing the positive outcomes of SBCEA total of 160 patients were identified with positive lesions, resulting in an overall lesion detection rate of 30.5%. The specific lesions were categorized as follows: polyps (22 cases), ulcers (108 cases), enterostenosis (10 cases), vascular lesions (17 cases), red spots (18 cases), mucosal congestion and edema (111cases), suspected submucosal lesions (21 cases), diverticula (16 cases), lymphatic dilatations (34 cases), erosions (43 cases), and others (38 cases) (Table 3). Univariate analysis revealed that diabetes, elevated inflammatory markers, and anemia were significantly associated with the lesion detection rate in patients presenting with abdominal pain (Table 1). Further multivariate regression analysis indicated that elevated inflammatory markers (OR 2.218, 95% CI: 1.141–4.315, p = 0.019) and anemia (OR 2.622, 95% CI: 1.011–6.798, p = 0.047) were significant factors influencing the lesion detection rate (Table 2).
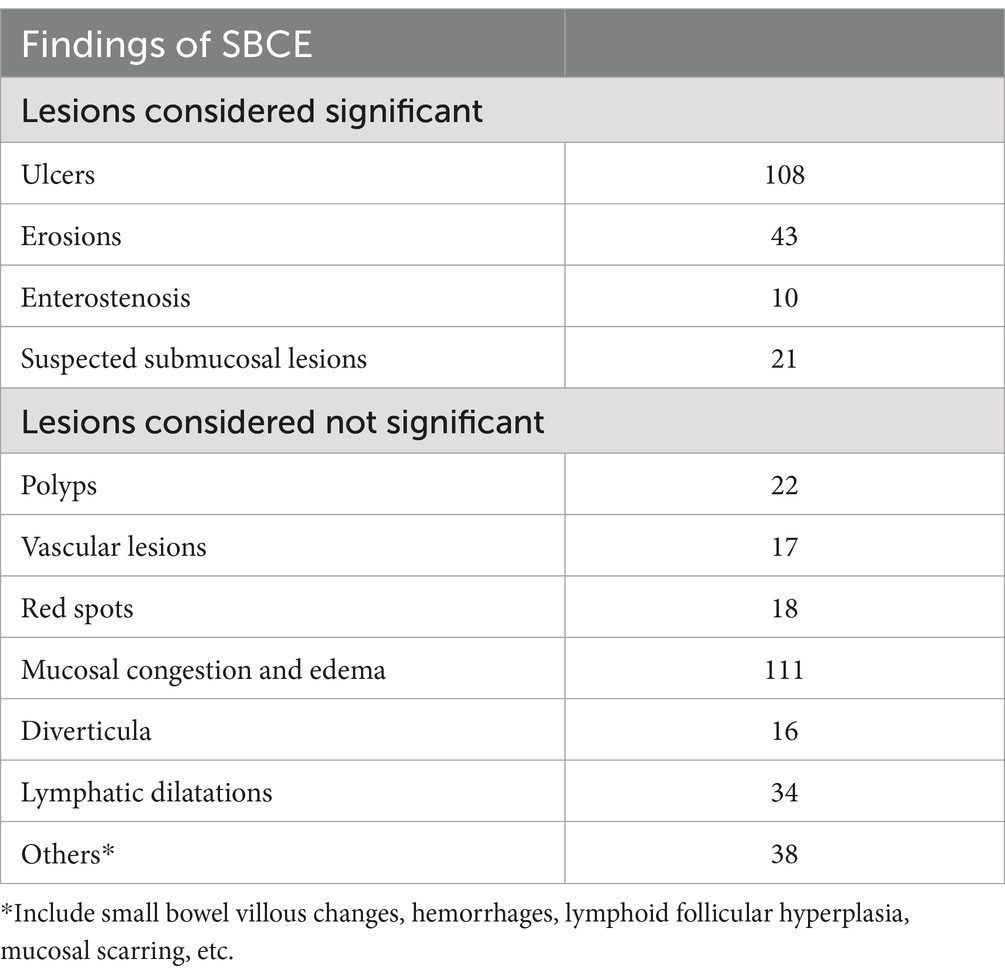
Table 3. Findings of SBCE.
DiscussionOur study identified hospitalization status, diabetes, and anemia as risk factors for DUGT in patients experiencing chronic abdominal pain. Additionally, we found that elevated inflammatory markers and anemia were significantly associated with lesion detection rates. Notably, anemia was both a risk factor for DUGT and significantly correlated with a high lesion detection rate, which may raise concerns during the screening of patients with chronic abdominal pain. Statistically, we observed that the DUGT rate among patients with chronic abdominal pain and anemia was 69.6%. However, the examination completion rate reached 100% when appropriate measures were implemented, and the lesion detection rate approached 60.9%. Therefore, we believe it is worthwhile to conduct SBCE examinations for patients with chronic abdominal pain with anemia after comprehensive consideration.
A retrospective study conducted in Europe involving 190 patients who underwent SBCE found that persistent hospitalization status was linked to an increased risk of gastric retention. This condition occurred in 24.1% of patients during their hospitalization. The study also revealed that persistent hospitalization status was associated with lower rates of completion for whole small bowel examinations (9). In a prior prospective study in Japan (10), 76 patients undergoing SBCE were recruited to evaluate the relationship between physical activity and examination completion rates. The completion rate for SBCE was 100% in the outpatient group, 85.7% in the mild bed rest group, and 72.2% in the strict bed rest group. The investigators concluded that low physical activity was a significant risk factor for failure to reach the cecum during SBCE, and that completion rates increased with higher levels of patient physical activity. Additionally, our previous study with a large sample size also confirmed that hospitalization status was strongly associated with the completion rate of SBCE examinations (11). In our current study, we further confirmed that hospitalization status was a significant risk factor for DUGT in patients with chronic abdominal pain. We believed this was related to extended bed rest and activity limitations experienced by hospitalized patients. Therefore, based on these findings, endoscopists should closely monitor the status of capsule operations when hospitalized patients undergo SBCE examinations. If necessary, they may enhance the efficacy of SBCE by administering prokinetic agents or by placing the capsule directly into the duodenum with the assistance of an endoscope. The European Society of Gastrointestinal Endoscopy recommends that SBCE may be performed on an outpatient basis whenever possible, as completion rates are generally higher in outpatients than in hospitalized patients (12).
In our study, we found that diabetes is a significant risk factor for DUGT. Previous research has demonstrated that gastrointestinal motility dysfunction occurs in approximately one-third of patients who experience capsule retention, with diabetic gastroparesis being one of the most common disorders contributing to gastrointestinal motility dysfunction in this population (13). A retrospective study conducted by Triantafyllou et al. (14) found that diabetic patients exhibited significantly longer capsule gastric transit times and notably lower rates of complete small bowel examinations compared to non-diabetic patients. Additionally, a prospective European study further corroborated the observation of slower gastric emptying in diabetic patients relative to healthy controls (15). Collectively, these findings indicate that diabetes is a significant risk factor for DUGT. Our study also identified anemia as a risk factor for DUGT in chronic abdominal pain. This association may be attributed to the reduced oxygen supply to the gastrointestinal tract in anemic patients, which can lead to decreased gastrointestinal motility, subsequently resulting in DUGT. Typically, we believe that hypokalemia predisposes individuals to muscular weakness, adversely affecting the motility of gastrointestinal smooth muscle. As potassium deficiency persists, motility throughout the gastrointestinal tract progressively diminishes. In a prospective study conducted by Gan et al. (16) prolonged gastric transit time was observed in patients with hypokalemic compared to those with normal potassium levels; however, this finding was not statistically significant, and hypokalemia was not identified as a risk factor for DUGT in our study. The inconsistency of these findings may be related to the varying levels of potassium reduction and the duration of low potassium levels. Therefore, larger, multicenter, prospective studies are necessary to further evaluate the impact of hypokalemia on SBCE.
A previous retrospective study by Fry et al. (7) demonstrated that the detection rate of SBCE in patients with simple chronic abdominal pain not accompanied by additional symptoms, signs, or abnormal laboratory indices was only 6%. Based on the conclusions of this study, it appeared that the use of SBCE in patients with chronic abdominal pain may have limited value. SBCE is an effective technique, and several subsequent studies have further investigated its value in patients with chronic abdominal pain. These studies actively explored factors that can enhance the detection of positive lesions in this patient population. A prospective multicenter study conducted in Europe (8) involving 50 patients with chronic abdominal pain investigated whether the detection rate was higher in patients with chronic abdominal pain who had concomitant symptoms. The study found that the detection rate of lesions in patients with chronic abdominal pain accompanied by other symptoms or signs was 40%, significantly higher than the rate reported in the study by Fry et al. (7). This indicates that rigorous patient selection based on accompanying symptoms or signs is crucial for enhancing the detection rate of SBCE in patients with chronic abdominal pain. Additionally, inflammation appears to be the most valuable additional sign. Elevated inflammatory markers were also found to be significantly associated with detection rate in patients with chronic abdominal pain in our study. In our study, the lesion detection rate of SBCE in patients with chronic abdominal pain was 30.5%. Among patients with chronic abdominal pain and elevated inflammatory markers, the lesion detection rate increased to 52.3%. It is well established that inflammatory bowel disease, a chronic, non-specific intestinal inflammatory disease, is frequently accompanied by recurrent abdominal pain and abnormal elevations of inflammatory markers in laboratory tests. Consequently, patients with chronic abdominal pain and elevated inflammatory markers are more likely to have lesions in the small intestine detected by SBCE, particularly in cases of inflammatory bowel disease.
In a study of patients with iron deficiency anemia, Nahon et al. (17) concluded that hemoglobin levels below 90 g/L were significantly associated with a higher lesion detection rate during SBCE examinations. A Japanese study involving 578 patients who underwent SBCE further validated the correlation between reduced hemoglobin levels and an increased rate of lesion detection (18). In our study, we found that comorbid anemia in patients with chronic abdominal pain was significantly associated with an elevated lesion detection rate. It is well known that certain chronic hemorrhagic diseases of the gastrointestinal tract, such as malignant tumors, intestinal ulcers, and small intestinal vasodilation, often lead to patients presenting with anemia. However, a German study involving 50 patients with chronic abdominal pain found no significant correlation between anemia and the detection rate of lesions in these patients. We speculate that this discrepancy may be attributed to several factors. First, the definitions of anemia vary, in our study, we employed a stricter definition, classifying anemia as hemoglobin levels below 90 g/L. Second, the gastroenterology department of our hospital tends to admit relatively complex and severe cases, which may influence the detection of lesions to some extent. Third, the sample size of patients with anemia included in this study was relatively small. Therefore, we propose that patients with chronic abdominal pain who also have comorbid anemia should be considered for SBCE when other routine tests yield negative results. Several prior studies have demonstrated that the combination of weight loss or hypoalbuminemia in patients with chronic abdominal pain is significantly associated with a high lesion detection rate. However, in the present study, these two factors, weight loss and hypoalbuminemia, were not examined due to the extensive time span of the data and incomplete recording of certain information.
Our study has several limitations. First, it was a retrospective study that may be subject to selection bias. Second, due to the extended time frame, there were variations in the bowel preparation protocols for the included capsules. And we did not incorporate the bowel scores of the patients into our analysis, which could have influenced the lesion detection rate. Additionally, due to the lack of pathological specimens, the nature of suspected submucosal lesions has not been clearly defined. Finally, we utilized only one brand of capsule and did not consider other brands, such as OMOM, in our study.
In conclusion, our study identified hospitalization status, diabetes, and anemia as significant risk factors for DUGT in patients experiencing chronic abdominal pain. Furthermore, it is essential to closely monitor the capsule running status of these patients in clinical settings. Our findings also highlight the considerable value of SBCE in patients with chronic abdominal pain who present with anemia and elevated inflammatory markers.
Data availability statementThe raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statementThe studies involving humans were approved by the Institutional Review Board of Renji Hospital. The studies were conducted in accordance with the local legislation and institutional requirements. The ethics committee/institutional review board waived the requirement of written informed consent for participation from the participants or the participants’ legal guardians/next of kin because this was a retrospective study, so we obtained a waiver of written informed consent from the Institutional Review Board of Renji Hospital.
Author contributionsXH: Conceptualization, Data curation, Methodology, Writing – original draft, Formal analysis. QX: Data curation, Methodology, Writing – review & editing. HX: Conceptualization, Formal analysis, Methodology, Supervision, Validation, Writing – review & editing.
FundingThe author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interestThe authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statementThe authors declare that no Generative AI was used in the creation of this manuscript.
Publisher’s noteAll claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References2. Treede, RD, Rief, W, Barke, A, Aziz, Q, Bennett, MI, Benoliel, R, et al. A classification of chronic pain for ICD-11. Pain. (2015) 156:1003–7. doi: 10.1097/j.pain.0000000000000160
PubMed Abstract | Crossref Full Text | Google Scholar
3. Wallander, MA, Johansson, S, Ruigomez, A, and Garcia Rodriguez, LA. Unspecified abdominal pain in primary care: the role of gastrointestinal morbidity. Int J Clin Pract. (2007) 61:1663–70. doi: 10.1111/j.1742-1241.2007.01529.x
PubMed Abstract | Crossref Full Text | Google Scholar
4. Sandler, RS, Stewart, WF, Liberman, JN, Ricci, JA, and Zorich, NL. Abdominal pain, bloating, and diarrhea in the United States: prevalence and impact. Dig Dis Sci. (2000) 45:1166–71. doi: 10.1023/A:1005554103531
Crossref Full Text | Google Scholar
6. Bardan, E, Nadler, M, Chowers, Y, Fidder, H, and Bar-Meir, S. Capsule endoscopy for the evaluation of patients with chronic abdominal pain. Endoscopy. (2003) 35:688–9. doi: 10.1055/s-2003-41520
PubMed Abstract | Crossref Full Text | Google Scholar
7. Fry, LC, Carey, EJ, Shiff, AD, Heigh, R, Sharma, V, Post, J, et al. The yield of capsule endoscopy in patients with abdominal pain or diarrhea. Endoscopy. (2006) 38:498–502. doi: 10.1055/s-2006-925340
PubMed Abstract | Crossref Full Text | Google Scholar
8. May, A, Manner, H, Schneider, M, Ipsen, A, and Ell, C. Prospective multicenter trial of capsule endoscopy in patients with chronic abdominal pain, diarrhea and other signs and symptoms (CEDAP-plus study). Endoscopy. (2007) 39:606–12. doi: 10.1055/s-2007-966640
PubMed Abstract | Crossref Full Text | Google Scholar
9. Ben-Soussan, E, Savoye, G, Antonietti, M, Ramirez, S, Lerebours, E, and Ducrotté, P. Factors that affect gastric passage of video capsule. Gastrointest Endosc. (2005) 62:785–90. doi: 10.1016/j.gie.2005.07.040
PubMed Abstract | Crossref Full Text | Google Scholar
10. Shibuya, T, Mori, H, Takeda, T, Konishi, M, Fukuo, Y, Matsumoto, K, et al. The relationship between physical activity level and completion rate of small bowel examination in patients undergoing capsule endoscopy. Intern Med. (2012) 51:997–1001. doi: 10.2169/internalmedicine.51.6581
PubMed Abstract | Crossref Full Text | Google Scholar
11. He, XL, Chen, HM, and Xue, HB. Risk factors of delayed upper gastrointestinal transit in capsule endoscopy. Scand J Gastroenterol. (2024) 59:1216–1219. doi: 10.1080/00365521.2024.2399670
Crossref Full Text | Google Scholar
12. Rondonotti, E, Spada, C, Adler, S, May, A, Despott, E, Koulaouzidis, A, et al. Small-bowel capsule endoscopy and device-assisted enteroscopy for diagnosis and treatment of small-bowel disorders: European Society of Gastrointestinal Endoscopy (ESGE) technical review. Endoscopy. (2018) 50:423–46. doi: 10.1055/a-0576-0566
PubMed Abstract | Crossref Full Text | Google Scholar
13. Ormeci, AC, Akyuz, F, Baran, B, Gokturk, S, Ormeci, T, Pinarbasi, B, et al. Retention during capsule endoscopy: is it a real problem in routine practice? J Int Med Res. (2016) 44:968–75. doi: 10.1177/0300060516645420
PubMed Abstract | Crossref Full Text | Google Scholar
14. Triantafyllou, K, Kalantzis, C, Papadopoulos, AA, Apostolopoulos, P, Rokkas, T, Kalantzis, N, et al. Video-capsule endoscopy gastric and small bowel transit time and completeness of the examination in patients with diabetes mellitus. Dig Liver Dis. (2007) 39:575–80. doi: 10.1016/j.dld.2007.01.024
Crossref Full Text | Google Scholar
15. Sangnes, DA, Lundervold, K, Bekkelund, M, von Volkmann, HL, Berentsen, B, Gilja, OH, et al. Gastrointestinal transit and contractility in diabetic constipation: a wireless motility capsule study on diabetes patients and healthy controls. United European Gastroenterol J. (2021) 9:1168–77. doi: 10.1002/ueg2.12169
PubMed Abstract | Crossref Full Text | Google Scholar
16. Gan, HY, Peng, TL, Su, KH, Zhao, LL, Jian, LQ, Yang, RJ, et al. Association between hypokalemia and small bowel capsule endoscopy completion rates in patients in South China: a prospective single-center study. Saudi J Gastroenterol. (2019) 25:40–5. doi: 10.4103/sjg.SJG_77_18
PubMed Abstract | Crossref Full Text | Google Scholar
17. Nahon, S, Lahmek, P, Lesgourgues, B, Nahon-Uzan, K, Tuszynski, T, Traissac, L, et al. Predictive factors of GI lesions in 241 women with iron deficiency anemia. Am J Gastroenterol. (2002) 97:590–3. doi: 10.1111/j.1572-0241.2002.05534.x
PubMed Abstract | Crossref Full Text | Google Scholar
18. Shimada, S, Watanabe, T, Nadatani, Y, Otani, K, Taira, K, Hosomi, S, et al. Clinical factors associated with positive capsule endoscopy findings in patients with obscure gastrointestinal bleeding: a single-center study. Scand J Gastroenterol. (2017) 52:1219–23. doi: 10.1080/00365521.2017.1349174
留言 (0)