As a critical public health issue, childhood sexual abuse (CSA) refers to the involvement of children in sexual activities that they do not fully understand, are unable to give informed consent to, for which they are not developmentally prepared, or that contravene the societal norms (1). CSA is relatively common with prevalence rates of 20%–25% for women and 5%–15% for men (2). Data from published research covering 6,834 Chinese college students reported that the rate of CSA was 20.76%, with men being higher than women (24.23% vs. 18.10%) (3). A survey among Chinese middle school students showed that the prevalence rate of sexual abuse was 25.5% (4).
A multitude of studies have demonstrated that CSA is correlated with a heightened vulnerability to adverse health consequences in later life (5, 6), with sleep disturbance (SD) being among the most notable of these issues (7, 8). Therefore, a more profound comprehension of the relationship between CSA and SD is essential for the prevention, assessment, and treatment of sleep-related issues.
Childhood trauma, particularly CSA, has been consistently linked to sleep problems in adulthood as evidenced by a wealth of research (9–11). Studies have shown that the effects of CSA on sleep can be long-lasting, extending into adulthood (8, 12, 13). CSA survivors are often at a higher risk of experiencing difficulties in falling asleep or maintaining sleep, have lower sleep efficiency, have increased occurrences of nightmares, and have restless sleep (8, 14).—for instance, a longitudinal study involving 533 adult survivors of CSA revealed that the prevalence rate of high insomnia symptoms was as high as 30.6% (13). Additionally, a study focusing on women sexually abused 10 years ago indicated that they reported more SD, identifying such as a long-term consequence of CSA (15). Furthermore, trauma-related psychological problems such as anxiety and depression, which can arise later in life, may then also exacerbate existing SD in CSA survivors (16). However, research confirming the association between CSA and sleep problems among Chinese populations is limited (9). Therefore, it is imperative to further explore the potential pathways linking CSA and SD, especially among Chinese CSA survivors.
Perceived discrimination may indeed serve as a critical link between CSA and SD in adulthood. Perceived discrimination (PD) is defined as people’s beliefs or perceptions of negative attitudes, judgment, or unfair treatment directed toward them as members of a specific group (17, 18). The cognitive model of posttraumatic stress disorder suggests that those who experienced traumatic events may overgeneralize from these events, perceiving a range of activities as more dangerous than they really are (19). Early life trauma can contribute to the development of negative beliefs about the world or the self, increasing the likelihood of feeling discriminated against (20, 21). Compared to those without adverse childhood experiences, adults with such experiences were more likely to experience perceived daily discrimination and lifetime discrimination (17). This heightened perception of discrimination may, in turn, exacerbate sleep disturbances. A growing body of research has consistently shown that discrimination negatively impacts sleep (22, 23). Everyday discrimination is significantly associated with poorer sleep quality and greater disturbances (24). While the existing literature has demonstrated the relationship between adverse childhood experiences and PD in adulthood (21, 25), the specific association between CSA and PD has not been thoroughly explored. There is a need to investigate whether PD plays a significant mediating role in the relationship between CSA and SD. One study has examined PD’s role as a mediator of childhood trauma and psychological distress (26), but the effect of PD on the link between CSA and SD remains understudied. Therefore, further research is necessary to establish whether PD could significantly mediate the association between CSA and SD, which could have important implications for developing targeted interventions to improve sleep quality among survivors of CSA.
Rumination, a maladaptive cognitive processing style or coping strategy in response to trauma (19), is characterized by persistent and negative introspection on one’s suffering, the potential causes, and the consequences of unwanted emotions (27). This pattern often emerges following a traumatic experience and may reinforce problematic interpretations of the trauma (19). According to the cognitive model, rumination can directly amplify feelings of nervous tension, dysphoria, or hopelessness, thereby prolonging and intensifying psychological distress and its associated problems (28, 29). Previous studies have indicated that individuals who have been sexually abused in childhood were more prone to ruminate on their feelings of sadness (30, 31), and this on-going rumination was linked to more severe long-term psychological problems (32), including sleep difficulties (33). Given the relationships between CSA, rumination, and sleep problems, it is hypothesized that CSA can significantly predict SD through the mediating effect of rumination.
Furthermore, rumination and PD have been found to be positively associated with each other (29, 34). A study on racial minorities has indicated that rumination mediated the relationship between PD and depressive symptoms (29). As a maladaptive cognitive strategy, rumination can lead to perseverative thoughts about the feeling of discrimination, which, in turn, can trigger mental health problems (28). However, the extent to which rumination might predict SD through the effect of PD among CSA survivors has not yet been revealed. In consideration of prior studies, we propose the hypothesis that PD and rumination may act as linking factors in the association between CSA and SD.
The present study aimed to extend prior research and further elucidate SD among CSA survivors as well as its associations with PD and rumination. More specifically, we want to know the relationship between CSA and adulthood SD and the extent to which PD and rumination mediated this relationship. Drawing from the extant body of research, it is hypothesized that (1) CSA would have positive relations to SD and (2) PD and rumination would show significant mediating effects on the associations between CSA and SD (Figure 1).
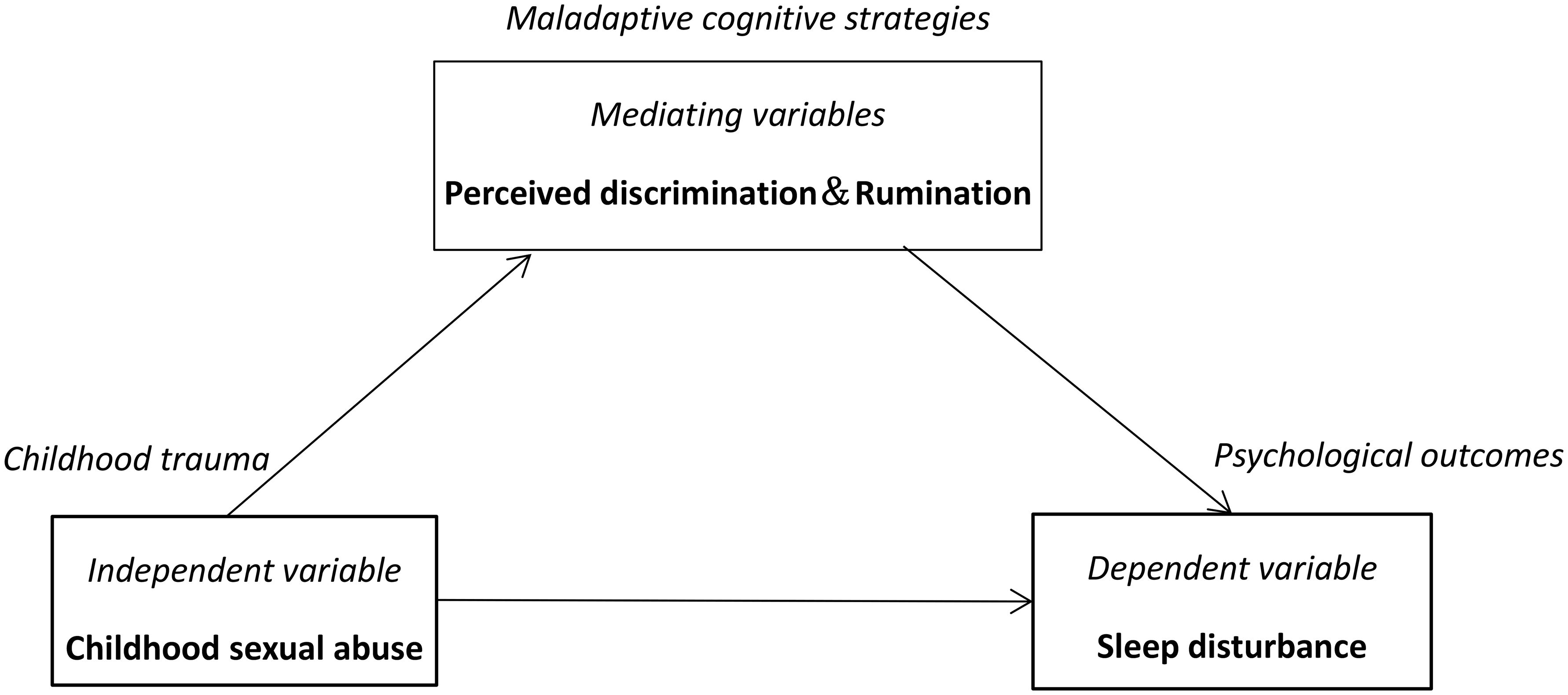
Figure 1. Conceptual framework.
2 Methods2.1 Participants and procedureThe participants were recruited by means of online advertisement, mostly through a web-based platform (https://www.wjx.cn/). After reading the consent form and guidance of the survey, a total of 1,210 respondents (824 men and 386 women) completed this survey. The participants’ ages ranged from 18 to 35 (M = 22.77, SD = 3.14). Among them, there were 565 (46.7%) participants with a history of CSA, 508 (42.0%) participants had a left-behind experience, 702 (58.0%) participants were from the countryside, and 310 (25.6%) participants were from single-parent families. This study was conducted in accordance with the Declaration of Helsinki and received ethical approval by the Ethics Committee for Scientific Research of the Third Affiliated Hospital of Zhengzhou University (grant no. 2022-360-01).
2.2 Measures2.2.1 Childhood Sexual Abuse QuestionnaireSexual abuse history in childhood was assessed using the Childhood Sexual Abuse Questionnaire (CSAQ), a subscale of the Childhood Trauma Questionnaire-Short Form adapted into a Chinese version (35, 36). The CSAQ comprises five items that evaluate the occurrence of sexual abuse during childhood, with each item scored on a five-point scale (1 = never true; 5 = very often true). The participants with a total score of 5 or higher were classified as having a history of CSA. The CSAQ has demonstrated robust psychometric properties in prior studies (5). The Cronbach’s alpha of the CSAQ in the present study was 0.918, indicating high internal consistency.
2.2.2 Inventory of Depressive Symptomatology Self-ReportSD was measured by four sleep-related items derived from the Inventory of Depressive Symptomatology Self Report (IDS-SR): difficulty falling asleep, difficulty maintaining sleep, early awakening, and hypersomnia (37, 38). The participants were asked to rate these items on a four-point Likert scale (0–3) according to their sleep status over the past week. The insomnia total score was calculated as the sum of the scores for the first three items. Based on the scores from these four items, SD can be categorized as insomnia, hypersomnia, and delayed sleep phase. The IDS-SR has been validated by several previous studies (39). The Cronbach’s alpha for the present sample was 0.590.
2.2.3 Perceived Discrimination ScaleThe Perceived Discrimination Scale (PDS) was employed to measure perceived discrimination (25). This scale consists of three items, each rated on a four-point scale ranging from 1 (completely not conform) to 5 (completely conform). The participants were asked to report the frequency with which they experienced discriminatory treatment in their daily lives. The PDS has demonstrated good reliability and validity in Chinese samples (40). In the current study, the Cronbach’s alpha for PDS was 0.923.
2.2.4 Ruminative Response ScaleThe Ruminative Response Scale (RRS), a 22-item self-report measurement, was utilized to evaluate rumination (27). The RRS comprises three factors: symptom rumination, brooding, and reflective pondering (41). The participants were required to respond on a four-point Likert-scale (1 = almost never; 7 = almost always). Numerous studies have demonstrated that the RRS possesses satisfactory properties (42). The Cronbach’s alpha for RRS was 0.970 in the current study.
2.3 Statistical analysisDescriptive analysis, t-test, and bivariate correlations between variables were performed using SPSS 21.0. The mediation effects of PD and rumination on the relationship between CSA and SD were tested using the PROCESS v3.5 (model 6) in SPSS (43). Bias-corrected bootstrap estimates were based on 5,000 samples. The effect was significant when zero was not included in the 95% bootstrap confidence interval.
The structural equation model (SEM) by maximum likelihood estimation (MLE) was conducted using AMOS 23.0. Model fit was estimated based on the following indices: for chi-square (χ2) divided by degrees of freedom (CMIN/DF), goodness-of-fit index (GFI), comparative fit index (CFI), adjusted goodness-of-fit index (AGFI), and root mean square error of approximation (RMSEA). The theoretical model was well fitted with CMIN/DF <2, GFI and CFI >0.95, AGFI >0.90, and RMSEA <0.05 (44).
3 Results3.1 Group comparisonsThe results for group comparisons can be found in Table 1. Participants who experienced CSA exhibited significantly higher scores for SD, PD, and rumination compared to those without such experiences. Specifically, individuals with CSA reported higher rates of insomnia (47.79% vs. 29.30%) and hypersomnia (20.71% vs. 9.46%) than their counterparts without CSA. However, there was no significant difference in the rates of DSP between participants who had experienced CSA and those who had not.
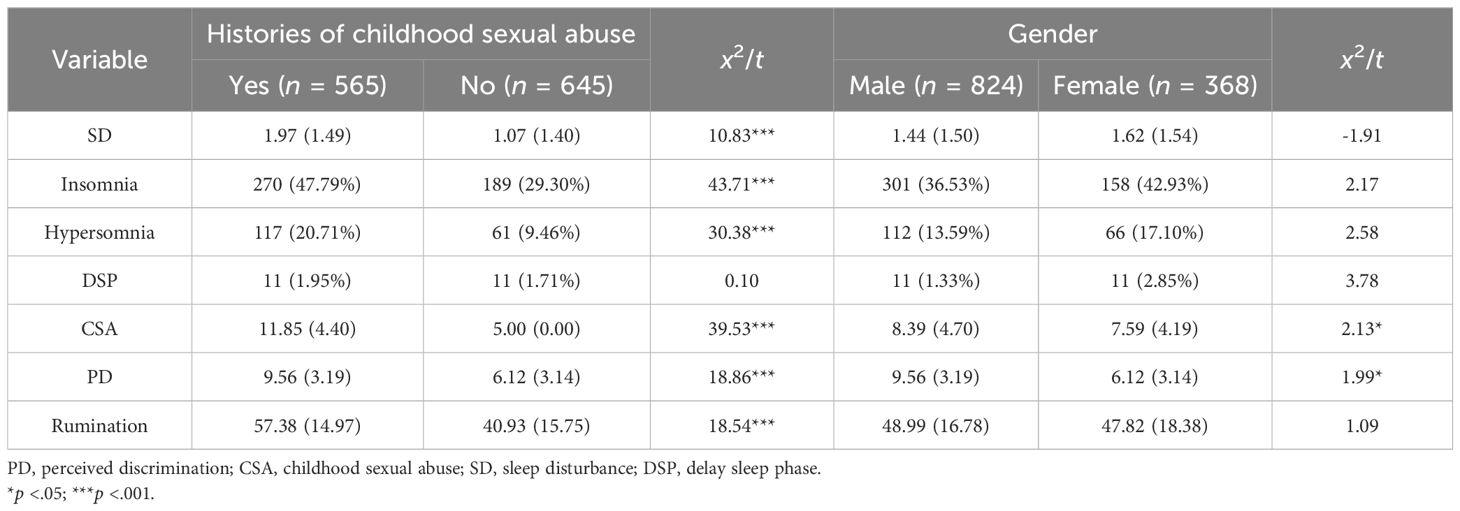
Table 1. Comparison of frequencies or means on variables of interest.
Moreover, male participants reported higher scores of CSA and PD than female participants. However, no significant differences were observed between men and women in terms of SD and rumination as well as the rates of insomnia, hypersomnia, and DSP.
3.2 CorrelationsThe correlations of study variables are presented in Table 2. The results indicated that CSA, SD, PD, and rumination were positively related with each other. Age was positively related to CSA, SD, PD, and rumination. Left-behind experience was negatively related to CSA, SD, PD, and rumination. There was no significant correlation between birth place and CSA, SD, PD, and rumination.
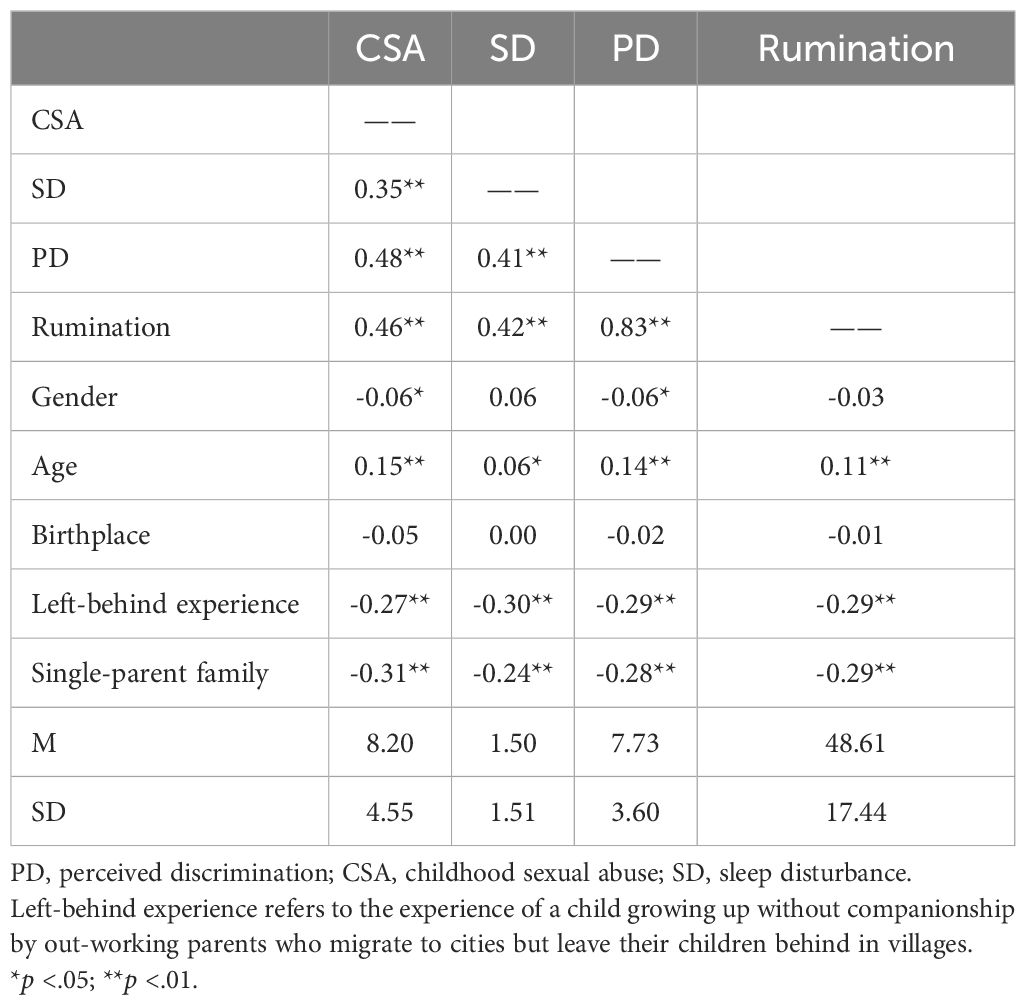
Table 2. Correlations of study variables (n = 1,210).
3.3 Direct and indirect effectsTo clarify the effects of CSA on SD through PD and rumination, after controlling for gender, age, birthplace, left-behind experience, and single-parent family, multiple mediation analysis was conducted. The results can be found in Tables 3, 4. The direct effect of CSA on SD was significant (direct effect = 0.151). There was a significant indirect effect of CSA on SD through PD and rumination. This means that CSA could not only predict SD via PD and rumination, respectively (the indirect effect of SD was 0.050 and the ratio of indirect to total effect was 17.99%; the indirect effect of rumination was 0.014 and the ratio of indirect to total effect was 5.04%) but could also predict SD via the multiple mediating effect of PD and rumination (the indirect effect of PD and rumination was 0.063 and the ratio of indirect to total effect was 22.66%).
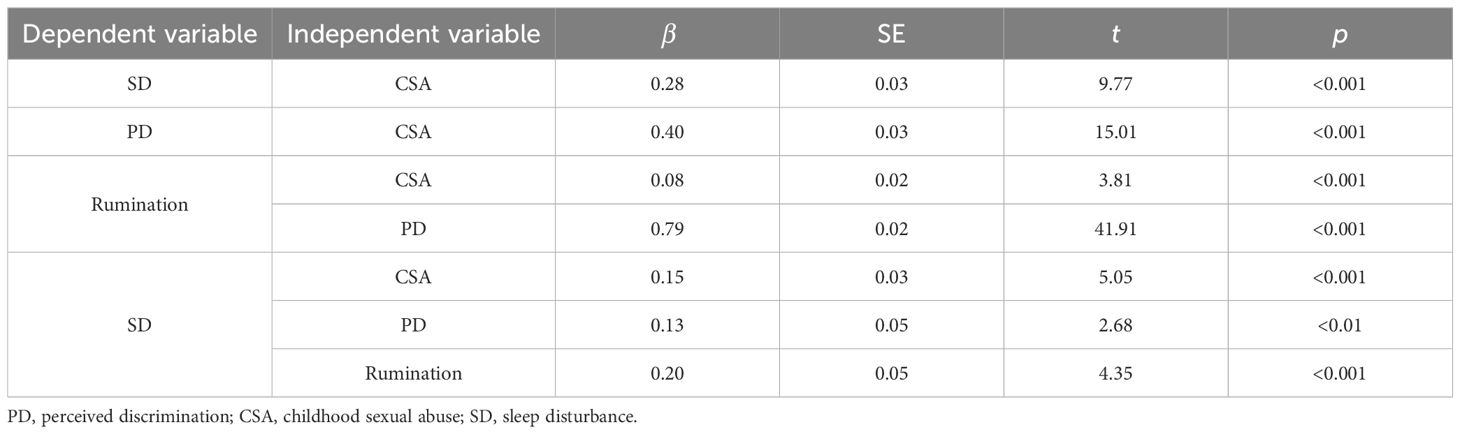
Table 3. Multiple mediation analysis of perceived discrimination and rumination on the relationship between childhood sexual abuse and sleep disturbance.
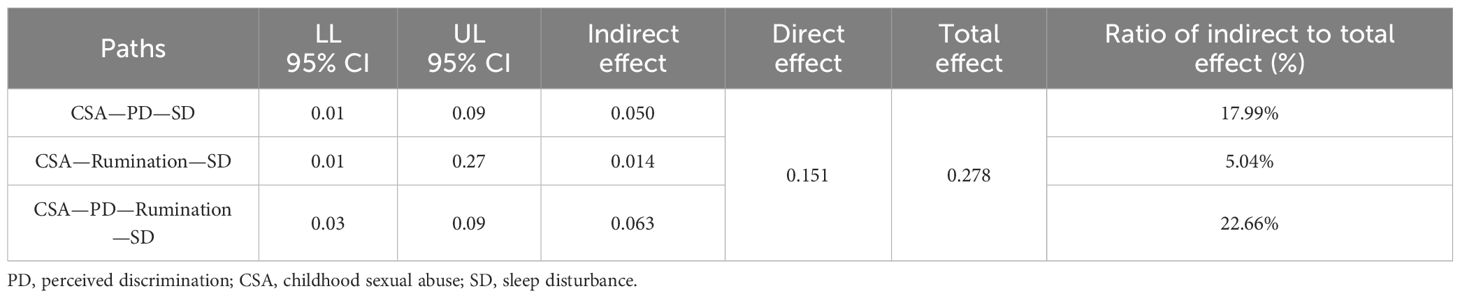
Table 4. Mediation effects of perceived discrimination and rumination between childhood sexual abuse and sleep disturbance.
In order to further visualize the direct effects and indirect effects of CSA on SD through PD and rumination, a total model was performed by using AMOS 21.0. The indices indicated a well fit for the data (CMIN/DF = 3.174, GFI = 0.996, CFI = 0.998, AGFI = 0.982, RMSEA = 0.042). The standardized path coefficients of the total model are displayed in Figure 2.
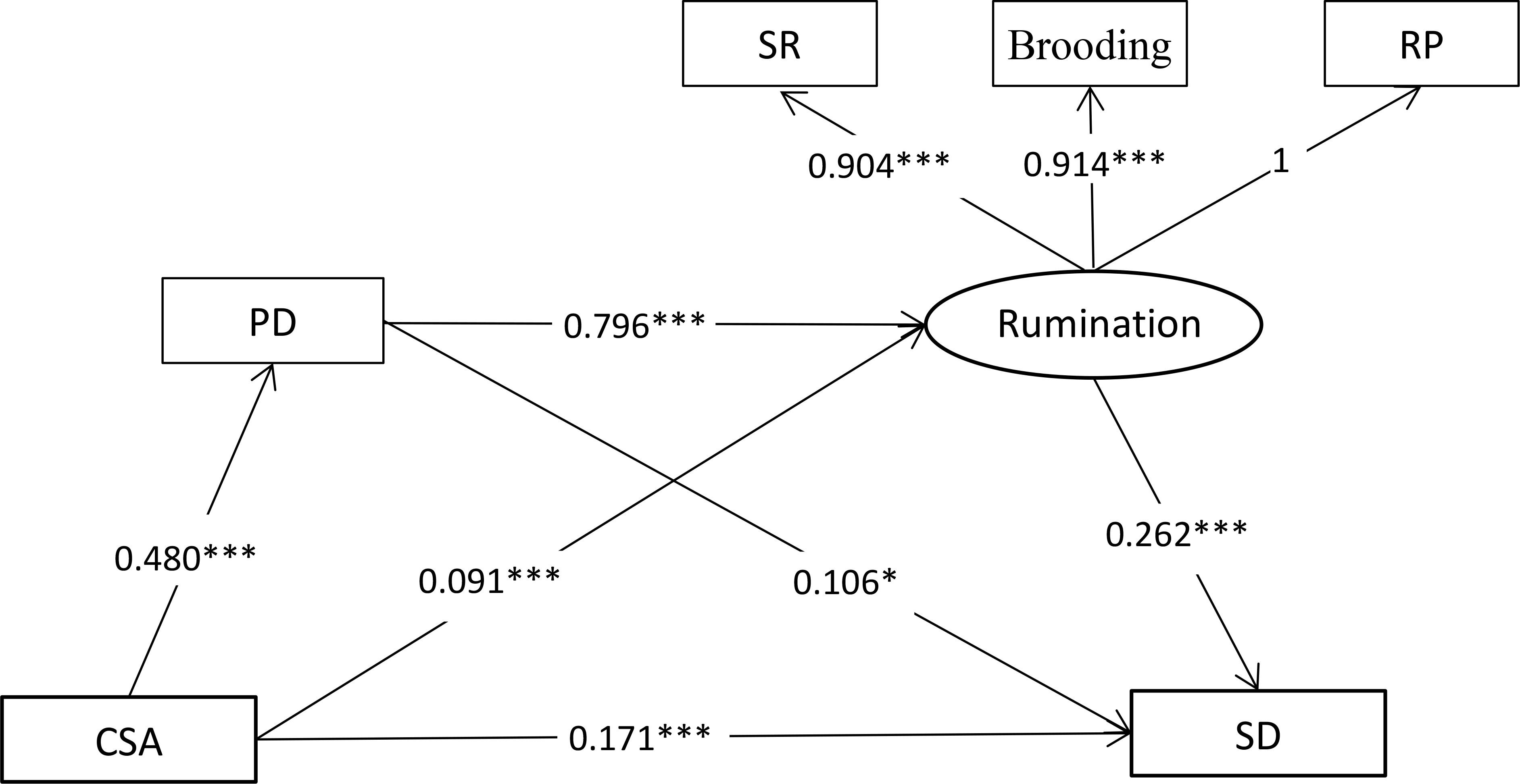
Figure 2. Total model. All coefficients for paths in the structural equation model were standardized. CSA, childhood sexual abuse; SD, sleep disturbance; PD, perceived discrimination; SR, symptom rumination; RP, reflective pondering. *p < .05; ***p < .001.
4 DiscussionBased upon previous literature on the association between adverse childhood experiences and sleep problems, the current study focused on SD among Chinese CSA survivors and further explored its associations with PD and rumination. As hypothesized, a significant relationship was observed between CSA and SD. Additionally, PD and rumination were found to exert significant mediating effects on the association between CSA and SD.
Our study found that participants with CSA experiences reported higher scores of SD and greater rates of insomnia and hypersomnia than those without such experiences. This aligned with previous research indicating that a higher adverse childhood experience score or childhood trauma score was associated with lower sleep efficiency, more insomnia symptoms, and poorer sleep indices (e.g., wake after sleep onset, sleep onset latency, and sleep quality) (16). Steine et al. (13) pointed out that 30.6% CSA survivors experienced severe insomnia symptoms. Our findings, based on a sample of Chinese CSA survivors, extended prior research by reporting an insomnia prevalence rate of 47.79%, which is notably higher than the previously reported figures (8, 13).
Aligning with a growing body of research (13–15), our study confirmed the positive association between CSA history and SD, with CSA directly predicting adulthood SD. This finding supports our first hypothesis that CSA could have positive relations to SD. Individuals who have experienced childhood traumatic events may be at an increased risk of sleep problems. One potential pathway underlying the link between CSA and adulthood SD is the negative association between SD and sleep-related context, as sexual abuse often occurs during bedtime or in a sleep environment (13). Sleep is inherently confined to unthreatening times and places, yet sexual abuse often occurs during sleeping time (15). Individuals who were sexually abused as children may perceive sleep-related context as threatening, developing long-lasting psychological associations between sleep and fear, anxiety, and wakefulness (45, 46), leading to poor sleep quality in adulthood (15). Another plausible explanation is psychophysiological hyperarousal caused by the hyperactivity of the hypothalamus–pituitary–adrenal cortex (HPA) axis (47), a brain system regulating the sleep/wake cycle (13). Disruption to the stress response and circadian timing systems may also contribute to poor sleep quality following exposure to early life stress (16). Furthermore, individuals abused in childhood are more likely to experience trauma or abuse later in life, and sleep problems may be caused by these more recent trauma or abuse (7). Trauma-related psychological problems (e.g., anxiety, depression) that arise later in life may also exacerbate pre-existing SD in survivors of CSA (16). Additionally, individuals with a history of abuse are more prone to engage in health-impairing behaviors, such as smoking and excessive caffeine or alcohol consumption, which can impact sleep quality directly (48).
To our knowledge, this study is the first to shed light on the mediating effects of PD and rumination on the associations between CSA and SD. Firstly, our findings build upon previous research demonstrating that PD played a mediating role in the associations between childhood trauma and psychological distress (26). This study further extends these insights by indicating PD’s role in the link between CSA and SD. Individuals abused during childhood are more likely to experience negative attitudes, judgment, or unfair treatment from others (17). Early adversities might increase biological, neural, and psychological vulnerability to stress by reducing the hippocampal and amygdala volume, which are potential mechanisms of stress sensitization following exposure to violence (21, 49). These adversities might also foster the development of negative beliefs about the world or the self, increasing the likelihood of perceiving discrimination (20, 21). However, discrimination can induce prolonged threat and chronic stress and potentially lead to the sensitization of the mesolimbic dopamine system and the dysregulation of the hypothalamic–pituitary–adrenal axis, both of which are implicated in various mental health issues, including sleep problems (50). PD has been shown to activate people’s feelings of threat, hyperarousal, or vigilance and even cause psychological distress such as anxiety, depression, anger, or cynical hostility (22). These psychological outcomes may, in turn, lead to poor sleep quality (23, 24).
Secondly, while previous research has explored rumination’s mediating role between PD and depressive symptoms among racial minorities (29), our study extends these findings to a sample of Chinese CSA survivors. We found that rumination mediated the relation between PD and SD, suggesting that CSA may predict SD indirectly through both PD and rumination. Rumination often occurs as a consequence of a traumatic experience, and individuals with a history of CSA were likely to ruminate on their feelings of sadness (30, 31). This maladaptive coping strategy can lead to perseverative thoughts about the feeling of discrimination, which, in turn, causes sleep problems (33).
4.1 ImplicationsThe findings of the current study have several notable implications for clinical practice. Firstly, our study lends support to the notion that CSA could have positive relations to SD. As CSA experiences have a detrimental impact on individuals’ mental health, clinicians should be aware that individuals who experienced sexual abuse during childhood may be at an increased risk for sleep problems in adulthood. Secondly, the results of our study provided new evidence to clarify how PD and rumination played mediating effects in associations between CSA experiences and sleep problems. It is noteworthy that these findings supported that the problematic cognitive appraisals and maladaptive coping strategy are critical factors related to SD of CSA survivors. It is crucial for clinicians to consider a wide range of cognitive–behavioral interventions focusing on developing adaptive behavior and positive cognitive strategies. Such interventions may be instrumental in mitigating sleep problems among CSA survivors.
4.2 LimitationsAlthough this study provides new insights into the mediating effects of PD and rumination on the associations between CSA and SD, it is not without limitations. Firstly, our cross-sectional design precludes the establishment of causality between childhood trauma and sleep problems. Therefore, future research employing longitudinal designs is necessary to draw causal conclusions. Secondly, given that different types of childhood trauma may be differently associated with sleep problems, future studies focusing on other types of childhood trauma (e.g., childhood emotional abuse, childhood physical abuse) may enable us to clarify the differences. Thirdly, our study had measurement-specific limitations—for example, because of the retrospective self-assessment style of questionnaires and social desirability of the survey, there might exist recall bias and participants’ bias in the data. This bias can be reduced by maintaining the anonymity of questionnaires in follow-up studies. Lastly, this study did not evaluate any comorbid psychological problems such as anxiety and depression, which may often accompany CSA experiences and may contribute to sleep problems. Therefore, studies in the next step are needed to evaluate and control for such comorbid factors when clarifying the focal associations.
5 ConclusionsIn conclusion, our study, with a sample of Chinese survivors of CSA, confirms the relationship between CSA and adulthood SD. Specifically, the results of this study are among the first, to our knowledge, to show the mediating effects of PD and rumination in this relationship. These results suggest that interventions aimed at reducing feelings of discrimination and developing positive coping strategies might be beneficial in enhancing the sleep quality of individuals with a history of sexual abuse during childhood.
Data availability statementThe raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Author contributionsWW: Funding acquisition, Investigation, Methodology, Writing – original draft, Writing – review & editing. XW: Data curation, Investigation, Writing – review & editing.
FundingThe author(s) declare financial support was received for the research, authorship, and/or publication of this article. This work was supported by PhD research startup foundation of the Third Affiliated Hospital of Zhengzhou University (Grant Number:BS20230106) and and Henan province science and technology research project (Grant Number:242102310106).
Conflict of interestThe authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s noteAll claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References1. World Health Organization. Guidelines for medico-legal care for victims of sexual violence: Childhood sexual abuse. Geneva: World Health Organization (2003).
2. Pereda N, Guilera G, Forns M, Gomez-Benito J. The prevalence of child sexual abuse in community and student samples: a meta-analysis. Clin Psychol Rev. (2009) 29:328–38. doi: 10.1016/j.cpr.2009.02.007
PubMed Abstract | Crossref Full Text | Google Scholar
3. Liu H, Wang W, Qi Y, Zhang L. Suicidal ideation among chinese survivors of childhood sexual abuse: associations with rumination and perceived social support. Child Abuse Neglect. (2022) 123:105420. doi: 10.1016/j.chiabu.2021.105420
PubMed Abstract | Crossref Full Text | Google Scholar
4. Zhao XF, Zhang YL, Li LF. Childhood abuse: An investigation of 435 middle school students. Chin J Clin Psychol. (2004) 04:377–9. doi: 10.1007/BF02911031
Crossref Full Text | Google Scholar
5. Steine IM, Winje D, Skogen JC, Krystal JH, Milde AM, Bjorvatn B, et al. Posttraumatic symptom profiles among adult survivors of childhood sexual abuse: A longitudinal study. Child Abuse Negl. (2017) 67:280–93. doi: 10.1016/j.chiabu.2017.03.002
PubMed Abstract | Crossref Full Text | Google Scholar
6. Zwickl S, Merriman G. The association between childhood sexual abuse and adult female sexual difficulties. Sexual Relationship Ther. (2011) 26:16–32. doi: 10.1080/14681994.2010.530251
Crossref Full Text | Google Scholar
8. Lind MJ, Aggen SH, Kendler KS, York TP, Amstadter AB. An epidemiologic study of childhood sexual abuse and adult sleep disturbances. psychol Trauma: Theory Research Practice Policy. (2016) 8:198–205. doi: 10.1037/tra0000080
PubMed Abstract | Crossref Full Text | Google Scholar
9. Geng F, Zou J, Liang Y, Zhan N, Li S, Wang J. Associations of positive and adverse childhood experiences and adulthood insomnia in a community sample of Chinese adults. Sleep Med. (2021) 80:46–51. doi: 10.1016/j.sleep.2021.01.022
PubMed Abstract | Crossref Full Text | Google Scholar
10. Kajeepeta S, Gelaye B, Jackson CL, Williams MA. Adverse childhood experiences are associated with adult sleep disorders: a systematic review. Sleep Med. (2015) 16:320–30. doi: 10.1016/j.sleep.2014.12.013
PubMed Abstract | Crossref Full Text | Google Scholar
11. Vadukapuram R, Shah K, Ashraf S, Srinivas S, Elshokiry AB, Trivedi C, et al. Adverse childhood experiences and their impact on sleep in adults. J Nervous Ment Dis. (2022) 210:397–410. doi: 10.1097/NMD.0000000000001480
PubMed Abstract | Crossref Full Text | Google Scholar
12. Chapman DP, Wheaton AG, Anda RF, Croft JB, Edwards VJ, Liu Y, et al. Adverse childhood experiences and sleep disturbances in adults. Sleep Med. (2011) 12:773–9. doi: 10.1016/j.sleep.2011.03.013
PubMed Abstract | Crossref Full Text | Google Scholar
13. Steine IM, Skogen JC, Krystal JH, Winje D, Milde AM, Grønli J, et al. Insomnia symptom trajectories among adult survivors of childhood sexual abuse: A longitudinal study. Child Abuse Negl. (2019) 93:263–76. doi: 10.1016/j.chiabu.2019.05.009
PubMed Abstract | Crossref Full Text | Google Scholar
14. Steine IM, Harvey AG, Krystal JH, Milde AM, Gronli J, Bjorvatn B, et al. Sleep disturbances in sexual abuse victims: a systematic review. Sleep Med Rev. (2012) 16:15–25. doi: 10.1016/j.smrv.2011.01.006
PubMed Abstract | Crossref Full Text | Google Scholar
16. Rojo-Wissar DM, Sosnowski DW, Ingram MM, Jackson CL, Maher BS, Alfano CA, et al. Associations of adverse childhood experiences with adolescent total sleep time, social jetlag, and insomnia symptoms. Sleep Med. (2021) 88:104–15. doi: 10.1016/j.sleep.2021.10.019
PubMed Abstract | Crossref Full Text | Google Scholar
17. Campbell JA, Walker RJ, Garacci E, Dawson AZ, Williams JS, Egede LE. Relationship between adverse childhood experiences and perceived discrimination in adulthood. J Affect Disord. (2020) 277:999–1004. doi: 10.1016/j.jad.2020.09.023
PubMed Abstract | Crossref Full Text | Google Scholar
20. Heinonen E, Knekt P, Harkanen T, Virtala E, Lindfors O. Associations of early childhood adversities with mental disorders, psychological functioning, and suitability for psychotherapy in adulthood. Psychiatry Res. (2018) 264:366–73. doi: 10.1016/j.psychres.2018.04.011
PubMed Abstract | Crossref Full Text | Google Scholar
21. Helminen EC, Scheer JR, Edwards KM, Felver JC. Adverse childhood experiences exacerbate the association between day-to-day discrimination and mental health symptomatology in undergraduate students. J Affect Disord. (2022) 297:338–47. doi: 10.1016/j.jad.2021.10.058
PubMed Abstract | Crossref Full Text | Google Scholar
23. Yip T, Xie M, Cham H, El Sheikh M. Linking ethnic/racial discrimination to adolescent mental health: Sleep disturbances as an explanatory pathway. Child Dev. (2022) 93:973–94. doi: 10.1111/cdev.13747
PubMed Abstract | Crossref Full Text | Google Scholar
24. Majeno A, Molina KM, Frisard CF, Lemon SC, Rosal MC. Discrimination and sleep: differential effects by type and coping strategy. Ann Behav medicine: Publ Soc Behav Med. (2023) 57:442–52. doi: 10.1093/abm/kaac071
PubMed Abstract | Crossref Full Text | Google Scholar
25. Shen JL, Hu XY, Liu X. Left-over children's perceived discrimination: its characteristics and relationship with personal well being. J Henan Univ (Social Science). (2009) 49:116–21. doi: 10.15991/j.cnki.411028.2009.06.018
Crossref Full Text | Google Scholar
26. Gangamma R, Tor S, Whitt V, Hollie B, Fish LS. Perceived discrimination as a mediator of ACEs and psychological distress. Am J Family Ther. (2020) 49:282–98. doi: 10.1080/01926187.2020.1813656
Crossref Full Text | Google Scholar
27. Nolen-Hoeksema S, Morrow J. A prospective study of depression and posttraumatic stress symptoms after a natural disaster: the 1989 Loma Prieta Earthquake. J Pers Soc Psychol. (1991) 61:115–21. doi: 10.1037//0022-3514.61.1.115
PubMed Abstract | Crossref Full Text | Google Scholar
28. Borders A, Liang CT. Rumination partially mediates the associations between perceived ethnic discrimination, emotional distress, and aggression. Cultural Diversity Ethnic Minority Psychol. (2011) 17:125–33. doi: 10.1037/a0023357
PubMed Abstract | Crossref Full Text | Google Scholar
29. Miranda R, Polanco-Roman L, Tsypes A, Valderrama J. Perceived discrimination, ruminative subtypes, and risk for depressive symptoms in emerging adulthood. Cultural Diversity Ethnic Minority Psychol. (2013) 19:395–403. doi: 10.1037/a0033504
PubMed Abstract | Crossref Full Text | Google Scholar
30. Conway M, Mendelson M, Giannopoulos C, Csank PAR, Holm SL. Childhood and adult sexual abuse, rumination on sadness, and dysphoria. Child Abuse Negl. (2004) 28:393–410. doi: 10.1016/j.chiabu.2003.05.004
PubMed Abstract | Crossref Full Text | Google Scholar
31. Gu H, Ma P, Xia T. Childhood emotional abuse and adolescent nonsuicidal self-injury: The mediating role of identity confusion and moderating role of rumination. Child Abuse Negl. (2020) 106:104474. doi: 10.1016/j.chiabu.2020.104474
PubMed Abstract | Crossref Full Text | Google Scholar
32. Liu H, Wang W, Qi Y, Zhang L. Suicidal ideation among Chinese survivors of childhood sexual abuse: Associations with rumination and perceived social support. Child Abuse Negl. (2022) 123:105420. doi: 10.1016/j.chiabu.2021.105420
PubMed Abstract | Crossref Full Text | Google Scholar
33. Amaral AP, Soares MJ, Pinto AM, Pereira AT, Madeira N, Bos SC, et al. Sleep difficulties in college students: The role of stress, affect and cognitive processes. Psychiatry Res. (2018) 260:331–7. doi: 10.1016/j.psychres.2017.11.072
PubMed Abstract | Crossref Full Text | Google Scholar
35. Bernstein DP, Stein JA, Newcomb MD, Walker E, Pogge D, Ahluvalia T, et al. Development and validation of a brief screening version of the Childhood Trauma Questionnaire. Child Abuse Negl. (2003) 27:169–90. doi: 10.1016/s0145-2134(02)00541-0
PubMed Abstract | Crossref Full Text | Google Scholar
36. Zhao X, Zhang Y, Li Y, Zhou Y, Li H, Yang S. Reliability and validity of the Chinese version of childhood trauma questionnaire. Chin J Clin Rehabil. (2005) 9:105–7. doi: 10.3321/j.issn:1673-8225.2005.16.037
Crossref Full Text | Google Scholar
37. Rush AJ, Gullion CM, Basco MR, Jarrett RB, Trivedi MH. The Inventory of Depressive Symptomatology (IDS): psychometric properties. psychol Med. (1996) 26:477–86. doi: 10.1017/s0033291700035558
PubMed Abstract | Crossref Full Text | Google Scholar
38. Wu D, Yin H, Xu S, Carmody T, Morris DW. Psychometric properties of the Chinese version of Inventory for Depressive Symptomatology (IDS): Preliminary findings. Asian J Psychiatry. (2010) 3:126–9. doi: 10.1016/j.ajp.2010.08.003
PubMed Abstract | Crossref Full Text | Google Scholar
39. Laskemoen JF, Simonsen C, Büchmann C, Barrett EA, Bjella T, Lagerberg TV, et al. Sleep disturbances in schizophrenia spectrum and bipolar disorders – a transdiagnostic perspective. Compr Psychiatry. (201
留言 (0)